Published online May 15, 2021. doi: 10.4251/wjgo.v13.i5.391
Peer-review started: January 15, 2021
First decision: February 14, 2021
Revised: February 25, 2021
Accepted: March 31, 2021
Article in press: March 31, 2021
Published online: May 15, 2021
Processing time: 112 Days and 0.4 Hours
Colorectal cancers comprise a large percentage of tumors worldwide, and transverse colon cancer (TCC) is defined as tumors located between hepatic and splenic flexures. Due to the anatomy and embryology complexity, and lack of large randomized controlled trials, it is a challenge to standardize TCC surgery. In this study, the current situation of transverse/extended colectomy, robotic/ laparoscopic/open surgery and complete mesocolic excision (CME) concept in TCC operations is discussed and a heatmap is conducted to show the evidence level and gap. In summary, transverse colectomy challenges the dogma of traditional extended colectomy, with similar oncological and prognostic outcomes. Compared with conventional open resection, laparoscopic and robotic surgery plays a more important role in both transverse colectomy and extended colectomy. The CME concept may contribute to the radical resection of TCC and adequate harvested lymph nodes. According to published studies, laparoscopic or robotic transverse colectomy based on the CME concept was the appropriate surgical procedure for TCC patients.
Core Tip: Due to the anatomy and embryology complexity, and the lack of large randomized controlled trials, it is difficult to standardize surgery of transverse colon cancer (TCC). This study discusses the possible appropriate surgical procedures of TCC patients and a heatmap was conducted to show the evidence level and gap. In summary, transverse colectomy challenges the dogma of traditional extended colectomy, with similar oncological and prognostic outcomes.
- Citation: Li C, Wang Q, Jiang KW. What is the best surgical procedure of transverse colon cancer? An evidence map and minireview. World J Gastrointest Oncol 2021; 13(5): 391-399
- URL: https://www.wjgnet.com/1948-5204/full/v13/i5/391.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v13.i5.391
On a global scale, colorectal cancer is the second most common cancer in females and ranks third among males[1]. Generally, transverse colon cancer (TCC) is defined as tumors located between hepatic and splenic flexure[2], and is relatively rare, accounting for 10% of all colon cancers[3,4].
On the one hand, from an embryological standpoint, the proximal two-thirds of the transverse colon are derived from the midgut and the distal one-third is derived from the hindgut, and they are supplied by the middle and left colic artery, respectively[5]. On the other hand, from an anatomical point of view, the transverse colon is in close proximity to upper abdominal vital structures, and is not fixed to the retroperitoneal structures[6,7]. Due to the anatomy and embryology complexity, it is a challenging and daunting mission to mobilize and resect the transverse colon.
In clinical practice, symptoms and signs of TCC are not specific. Abdominal discomfort, which is difficult to locate might be the first complaint and is generally found in an advanced stage. Notably, the transverse colon of some patients has great mobility, and is located at the appendix plane even in the pelvic cavity[5]. Thus, gastritis, appendicitis, oophoritis, and other genitourinary diseases were often confused with TCC.
According to published studies, the 5-year survival rate was 28%-50%, which is obviously poorer than that of other colorectal tumor[8,9]. There are two main reasons: First, lymph node metastasis will occur in TCC patients at both the superior and inferior mesenteric arterial branches, especially the splenic flexure cancers. Second, peripheral important organs might create more surgical danger[8].
Consequently, all these factors contribute to the belief that transverse colic surgery was difficult to standardize and was naturally excluded from several randomized controlled trials (RCTs)[10-13]. The aim of this study was to review the indications, merits and demerits of different surgical procedures for transverse colic via the evidence and gap map.
Excel (2019, Microsoft, Redmond, WA, United States) was used for plotting the heatmap. The following electronic databases were searched: PubMed, EMBASE, and the Cochrane library, and the search was completed on December 12, 2020. All published studies were searched without any language and data restriction. The search items were as follows: TCC, surgical procedures and we also used Medical Subject Headings terms combined with free text terms. We also performed a supplementary literature search using Google Scholar. Endnote software (version 20, Thomson Reuters, Philadelphia, PA, United States) was used for removing duplicate publications and to facilitate the screening progress. Patients were included if: (1) The patients’ tumors strictly followed the definition of TCC (colon cancer located between hepatic and splenic flexure); and (2) Detailed surgical information. And patients were excluded if the study used informal surgical terms, which were hard to be classified.
En-bloc resection of the tumor is the radical therapy of TCC as it is for other colorectal cancers. Because of a low incidence and excluded by RCTs, there is no consensus on the standard transverse colic operation, and the surgical approach for this tumor is frequently based on the surgeon’s preference. The common surgical procedures are extended left or right colectomy and transverse colectomy, by laparoscopy or conventional open resection.
For better oncological outcomes, and according to the tumor location, extended right or left colectomy was the preference of several surgeons[5].
Extended right hemicolectomy was applicable for tumors located less than distal 10 cm of the hepatic flexure, and lymph node dissection, and included ligation of the ileocolic, right colic and middle colic arteries[14]. Correspondingly, extended left hemicolectomy was applied for tumors located less than 10 cm of the splenic flexure proximally, for which lymph node dissection included ligation of the left and middle colic arteries[14].
Identification of the middle colic arteries was important for extended surgery and transverse colectomy[14], including the medial approach described by Fujita et al[15] and Hasegawa et al[16], the “window technique” by Baća et al[17], and rotating transverse mesocolon by Ichihara et al[18]. Due to the specific anatomical position, division of the middle colic vessels and finding the correct surgical plane from complex adjacent organs (such as the duodenum, pancreas or spleen) is challenging in extended colectomy and transverse colectomy[5].
The number of harvested lymph nodes (generally, at least 15) is considered a vital symbol of surgical quality and prognosis[19-21]. Because of the higher number of harvested lymph nodes in extended colectomy, in previous studies, it was believed that patients with advanced TCC who underwent extended colectomy would have a better prognosis[6,22].
Localization of transverse colic carcinoma is especially difficult during surgery, both the attachment to omentum and fixed flexures altogether increases the difficulty. In addition, intraoperative colonoscopy is not applicable because the stimulation may increase hyperinflation of the bowel[5]. Therefore, it has been suggested that four quadrant preoperative tattooing was necessary for transverse colic carcinoma unless the tumor was large enough to be located[23,24].
Transverse colectomy has often been used for tumors located between the hepatic and splenic flexure, and lymph node dissection was performed, including ligation of the middle colic arteries[14]. Transverse colectomy has shown a descending trend from the early 20th century[8]. On the one hand, segmental resection was usually considered a less radical surgical procedures because of low number of harvested lymph nodes. On the other hand, the prevalence of laparoscopy made extended colectomy easier than transverse colectomy.
The most significant technical issue in transverse colectomy was the division of tumor-supplying arteries and drainage veins, especially, the wide variation of middle colic vessels and thorough appreciation of Henle trunk[25-28]. Based on a previous study[29], resection length did not correlate with a better postoperative outcome. Chong et al[8] suggested that appropriate central vessel ligation, a minimum distance of 5 cm from each margin, was more critical than extended bowel length resection. Notably, Stracci et al[30] demonstrated that a length of less than 20 cm was associated with an inadequate lymph node number and unnecessary chemotherapy. Moreover, there is some discussion about lymphadenectomy of the middle colon artery by laparoscopic transverse colectomy, because of the challenging surgical difficul
In previous studies, it was described that less extensive surgeries were safe in TCC patients, but some focused on the distal transverse colon and descending colon[31,33-36]. Chong et al[8] conducted a large cohort study and showed that the disease-free survival and overall survival rate were similar in the transverse colectomy and extended resection group. van Rongen et al[37] and Leijssen et al[6] compared the transverse colectomy and extended colectomy, respectively, and suggested that the former was an appropriate option for patients with TCC.
Laparoscopic colorectal surgery was first applied in benign diseases, such as inflammatory bowel disease. However, last decades have witnessed a trend of increasing laparoscopic surgery, and its application has expanded to colorectal cancer[14]. Laparoscopic resection has been accepted and applied in nearly all types of colorectal cancer, because of the better short outcomes and less surgical trauma[38], and because it played an increasingly important role in TCC patients both in extended resection or transverse colectomy[6].
Although several RCTs demonstrated that laparoscopic resection had an equal safety profile compared with open resection in left and right colic carcinoma, the similar result has not yet been verified for TCC[2,10-12,39-41]. Previous retrospective studies have reported that laparoscopic transverse colon resection showed better short-term outcomes and similar oncological outcomes compared with open surgery[2,14,28,42,43]. Although some studies describe that the surgical time was longer and surgical skills were more difficult, laparoscopic transverse colon resection, including extended colectomy and transverse colectomy did not show a significant trend of higher complications, conversion, or poor long-term prognosis[2,5,44]. Moreover, Yamaguchi et al[42] demonstrated that the laparoscopic group had a lower overall morbidity rate and wound infection rate. Notably, in some studies, it was incorrectly assumed that laparoscopic surgery was related to a low number of harvested lymph nodes, because of a lack of a review of the colorectal cancer literature[43,45,46].
In the field of robotic surgery, left and right colon resections were predominantly performed, and transverse colectomy has rarely been described[47]. Robotic surgery, which showed favorable outcomes in colorectal surgery, had also gained increasing acceptance in transverse surgery[48-52]. In previous studies, it was shown that robotic transverse colon surgery had the same number of harvested lymph nodes, clearer surgical vison, a lower conversion rate, and better short-term outcomes compared with laparoscopic surgery[3].
Regarding the learning curve, surgeons need a longer time compared to open resection and patients need to be selected for laparoscopic or robotic surgery in order to maximize safety and the best oncological outcomes, however, robotic surgery has a shorter learning curve compared to traditional laparoscopy[53,54].
Hohenberger et al[55] introduced the concept of complete mesocolic excision (CME) in radical colic resection. CME, as total mesorectal excision in rectal cancer patients, focuses on achieving en-bloc resection of the entire enveloped mesocolon, has been shown to produce a higher degree of lymphadenectomy, fewer local recurrences, and a better long-term oncological and clinical safety profile compared to non-CME resection[32].
Storli and Eide[7] published the first studies comparing open and laparoscopic CME in TCC patients, and no obvious differences were observed between these two methods. Although previous studies demonstrated that the feasibility of laparoscopic CME for TCC was appropriate[7,32,56,57], the evidence remained limited. Only three published studies demonstrated the safety and feasibility of robotic transverse colectomy, including two studies[3,58] that performed non-CME and only one study[47] that performed CME.
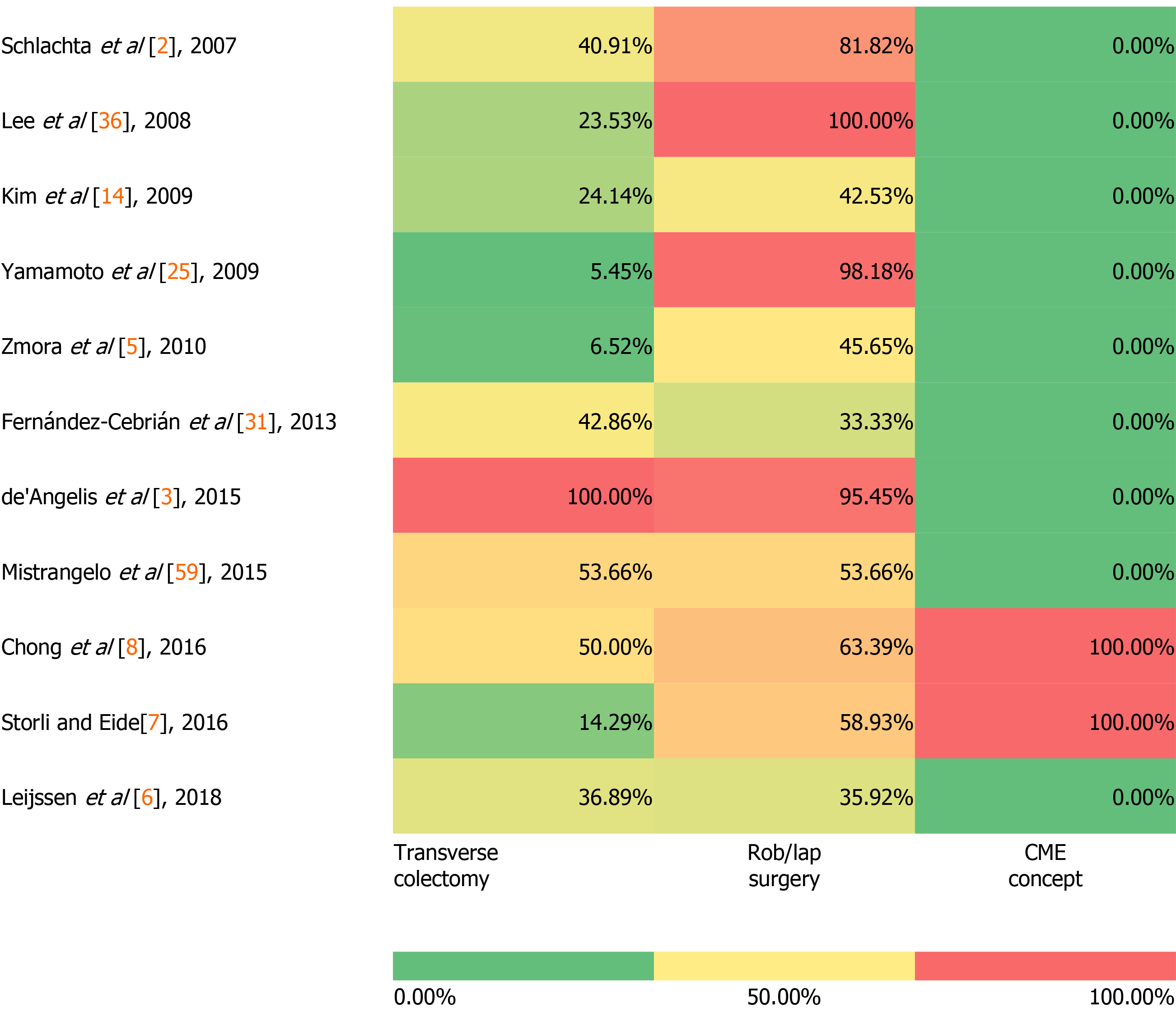
Among the included studies, a heatmap was constructed to demonstrate the current evidence and gap in three aspects: Transverse colectomy vs extended colectomy, robotic vs laparoscopic vs open surgery, and the CME concept in surgery.
As shown in Figure 1, we used the percentage from included studies to show the application of transverse colectomy in total post-operative TCC patients (including transverse colectomy, extended right/left colectomy). From the heatmap, transverse colectomy comprised a lower percentage compared with extended colectomy, in other words, extended colectomy was the preferential choice in the past decades. Compared with traditional open resection, robotic and laparoscopic surgery was applied more frequently because of better short-term outcomes and similar long-term outcomes. Regarding the CME concept in TCC patients, we defined that if the study demonstrated that all surgeries performed followed the concept of CME and we used “100%” to represent the data; if the study demonstrated none of the surgeries followed CME, or no detailed information about this, we used “0%” to present the data. Thus, the CME concept was rarely applied in both the transverse colectomy and extended colectomy, although it was an adequately safe and effective approach.
This study has several limitations. First, it was difficult to draw a convincing conclusion with limited data of TCC patients, such as detailed oncological features, surgical quality, and long-term outcomes. Second, based on published studies and clinical practice, transverse colectomy was a less commonly surgical procedure compared with extended right/ left colectomy. Third, the conclusion does not give robust evidence for standard treatment but reflected the current status of TCC patients.
As the surgical technology drives forward, so do the changes in surgical techniques of transverse cancer resection. Transverse colectomy challenges the dogma of traditional extended colectomy, with similar oncological and prognostic outcomes. Compared with conventional open resection, laparoscopic and robotic surgery plays a more important role in both transverse colectomy and extended colectomy. The CME concept may contribute to the radical resection of TCC and adequate number of harvested lymph nodes. In summary, according to published studies, laparoscopic or robotic transverse colectomy based upon the CME concept was the appropriate surgical procedure for most TCC patients.
However, large, multicenter, and prospective RCTs are needed to standardize surgical procedures of TCC patients. Perioperative management of different tumor stages, resection range, and anastomosis method of different transverse colic length, and long-term outcomes also need to be discussed.
We would like to thank Li Y, Zhang MM, Yu ZL of Peking University People's Hospital for clinical advices, and Zhang RC for providing the help of language supervision. Finally, we showed our respect to all authors of included studies involved in the study.
Manuscript source: Invited manuscript
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bains L, Christodoulou KC S-Editor: Gao CC L-Editor: A P-Editor: Li JH
| 1. | Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H, Dicker DJ, Chimed-Orchir O, Dandona R, Dandona L, Fleming T, Forouzanfar MH, Hancock J, Hay RJ, Hunter-Merrill R, Huynh C, Hosgood HD, Johnson CO, Jonas JB, Khubchandani J, Kumar GA, Kutz M, Lan Q, Larson HJ, Liang X, Lim SS, Lopez AD, MacIntyre MF, Marczak L, Marquez N, Mokdad AH, Pinho C, Pourmalek F, Salomon JA, Sanabria JR, Sandar L, Sartorius B, Schwartz SM, Shackelford KA, Shibuya K, Stanaway J, Steiner C, Sun J, Takahashi K, Vollset SE, Vos T, Wagner JA, Wang H, Westerman R, Zeeb H, Zoeckler L, Abd-Allah F, Ahmed MB, Alabed S, Alam NK, Aldhahri SF, Alem G, Alemayohu MA, Ali R, Al-Raddadi R, Amare A, Amoako Y, Artaman A, Asayesh H, Atnafu N, Awasthi A, Saleem HB, Barac A, Bedi N, Bensenor I, Berhane A, Bernabé E, Betsu B, Binagwaho A, Boneya D, Campos-Nonato I, Castañeda-Orjuela C, Catalá-López F, Chiang P, Chibueze C, Chitheer A, Choi JY, Cowie B, Damtew S, das Neves J, Dey S, Dharmaratne S, Dhillon P, Ding E, Driscoll T, Ekwueme D, Endries AY, Farvid M, Farzadfar F, Fernandes J, Fischer F, G/Hiwot TT, Gebru A, Gopalani S, Hailu A, Horino M, Horita N, Husseini A, Huybrechts I, Inoue M, Islami F, Jakovljevic M, James S, Javanbakht M, Jee SH, Kasaeian A, Kedir MS, Khader YS, Khang YH, Kim D, Leigh J, Linn S, Lunevicius R, El Razek HMA, Malekzadeh R, Malta DC, Marcenes W, Markos D, Melaku YA, Meles KG, Mendoza W, Mengiste DT, Meretoja TJ, Miller TR, Mohammad KA, Mohammadi A, Mohammed S, Moradi-Lakeh M, Nagel G, Nand D, Le Nguyen Q, Nolte S, Ogbo FA, Oladimeji KE, Oren E, Pa M, Park EK, Pereira DM, Plass D, Qorbani M, Radfar A, Rafay A, Rahman M, Rana SM, Søreide K, Satpathy M, Sawhney M, Sepanlou SG, Shaikh MA, She J, Shiue I, Shore HR, Shrime MG, So S, Soneji S, Stathopoulou V, Stroumpoulis K, Sufiyan MB, Sykes BL, Tabarés-Seisdedos R, Tadese F, Tedla BA, Tessema GA, Thakur JS, Tran BX, Ukwaja KN, Uzochukwu BSC, Vlassov VV, Weiderpass E, Wubshet Terefe M, Yebyo HG, Yimam HH, Yonemoto N, Younis MZ, Yu C, Zaidi Z, Zaki MES, Zenebe ZM, Murray CJL, Naghavi M. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2017;3:524-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2838] [Cited by in RCA: 2945] [Article Influence: 368.1] [Reference Citation Analysis (0)] |
| 2. | Schlachta CM, Mamazza J, Poulin EC. Are transverse colon cancers suitable for laparoscopic resection? Surg Endosc. 2007;21:396-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | de'Angelis N, Alghamdi S, Renda A, Azoulay D, Brunetti F. Initial experience of robotic vs laparoscopic colectomy for transverse colon cancer: a matched case-control study. World J Surg Oncol. 2015;13:295. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Wray CM, Ziogas A, Hinojosa MW, Le H, Stamos MJ, Zell JA. Tumor subsite location within the colon is prognostic for survival after colon cancer diagnosis. Dis Colon Rectum. 2009;52:1359-1366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 103] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 5. | Zmora O, Bar-Dayan A, Khaikin M, Lebeydev A, Shabtai M, Ayalon A, Rosin D. Laparoscopic colectomy for transverse colon carcinoma. Tech Coloproctol. 2010;14:25-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Leijssen LGJ, Dinaux AM, Amri R, Kunitake H, Bordeianou LG, Berger DL. A Transverse Colectomy is as Safe as an Extended Right or Left Colectomy for Mid-Transverse Colon Cancer. World J Surg. 2018;42:3381-3389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Storli KE, Eide GE. Laparoscopic Complete Mesocolic Excision vs Open Complete Mesocolic Excision for Transverse Colon Cancer: Long-Term Survival Results of a Prospective Single Centre Non-Randomized Study. Dig Surg. 2016;33:114-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Chong CS, Huh JW, Oh BY, Park YA, Cho YB, Yun SH, Kim HC, Lee WY. Operative Method for Transverse Colon Carcinoma: Transverse Colectomy Versus Extended Colectomy. Dis Colon Rectum. 2016;59:630-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 9. | Sjo OH, Lunde OC, Nygaard K, Sandvik L, Nesbakken A. Tumour location is a prognostic factor for survival in colonic cancer patients. Colorectal Dis. 2008;10:33-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Hazebroek EJ; Color Study Group. COLOR: a randomized clinical trial comparing laparoscopic and open resection for colon cancer. Surg Endosc. 2002;16:949-953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 186] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 11. | Clinical Outcomes of Surgical Therapy Study Group; Nelson H, Sargent DJ, Wieand HS, Fleshman J, Anvari M, Stryker SJ, Beart RW Jr, Hellinger M, Flanagan R Jr, Peters W, Ota D. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350:2050-2059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2606] [Cited by in RCA: 2512] [Article Influence: 119.6] [Reference Citation Analysis (0)] |
| 12. | Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM; MRC CLASICC trial group. Short-term endpoints of conventional vs laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718-1726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2360] [Cited by in RCA: 2292] [Article Influence: 114.6] [Reference Citation Analysis (0)] |
| 13. | Colon Cancer Laparoscopic or Open Resection Study Group; Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, Påhlman L, Cuesta MA, Msika S, Morino M, Lacy A, Bonjer HJ. Survival after laparoscopic surgery vs open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol. 2009;10:44-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 965] [Cited by in RCA: 1052] [Article Influence: 61.9] [Reference Citation Analysis (0)] |
| 14. | Kim HJ, Lee IK, Lee YS, Kang WK, Park JK, Oh ST, Kim JG, Kim YH. A comparative study on the short-term clinicopathologic outcomes of laparoscopic surgery vs conventional open surgery for transverse colon cancer. Surg Endosc. 2009;23:1812-1817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 54] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 15. | Fujita J, Uyama I, Sugioka A, Komori Y, Matsui H, Hasumi A. Laparoscopic right hemicolectomy with radical lymph node dissection using the no-touch isolation technique for advanced colon cancer. Surg Today. 2001;31:93-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Hasegawa S, Kawamura J, Nagayama S, Nomura A, Kondo K, Sakai Y. Medially approached radical lymph node dissection along the surgical trunk for advanced right-sided colon cancers. Surg Endosc. 2007;21:1657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 33] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Baća I, Perko Z, Bokan I, Mimica Z, Petricević A, Druzijanić N, Situm M. Technique and survival after laparoscopically assisted right hemicolectomy. Surg Endosc. 2005;19:650-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Ichihara T, Takada M, Fukumoto S, Kuroda Y. Lymphadenectomy along the middle colic artery in laparoscopic resection of transverse colon. Hepatogastroenterology. 2004;51:454-456. [PubMed] |
| 19. | Gouvas N, Agalianos C, Papaparaskeva K, Perrakis A, Hohenberger W, Xynos E. Surgery along the embryological planes for colon cancer: a systematic review of complete mesocolic excision. Int J Colorectal Dis. 2016;31:1577-1594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 76] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 20. | Le Voyer TE, Sigurdson ER, Hanlon AL, Mayer RJ, Macdonald JS, Catalano PJ, Haller DG. Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J Clin Oncol. 2003;21:2912-2919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 821] [Cited by in RCA: 846] [Article Influence: 38.5] [Reference Citation Analysis (0)] |
| 21. | Chen SL, Bilchik AJ. More extensive nodal dissection improves survival for stages I to III of colon cancer: a population-based study. Ann Surg. 2006;244:602-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 147] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 22. | Chang GJ, Rodriguez-Bigas MA, Skibber JM, Moyer VA. Lymph node evaluation and survival after curative resection of colon cancer: systematic review. J Natl Cancer Inst. 2007;99:433-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 708] [Cited by in RCA: 778] [Article Influence: 43.2] [Reference Citation Analysis (0)] |
| 23. | Zmora O, Dinnewitzer AJ, Pikarsky AJ, Efron JE, Weiss EG, Nogueras JJ, Wexner SD. Intraoperative endoscopy in laparoscopic colectomy. Surg Endosc. 2002;16:808-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 43] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 24. | Feingold DL, Addona T, Forde KA, Arnell TD, Carter JJ, Huang EH, Whelan RL. Safety and reliability of tattooing colorectal neoplasms prior to laparoscopic resection. J Gastrointest Surg. 2004;8:543-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 69] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 25. | Yamamoto S, Fujita S, Akasu T, Yamaguchi T, Moriya Y. Laparoscopic surgery for transverse and descending colon carcinomas has comparable safety to laparoscopic surgery for colon carcinomas at other sites. Dig Surg. 2009;26:487-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Yamaguchi S, Kuroyanagi H, Milsom JW, Sim R, Shimada H. Venous anatomy of the right colon: precise structure of the major veins and gastrocolic trunk in 58 cadavers. Dis Colon Rectum. 2002;45:1337-1340. [PubMed] |
| 27. | Jin G, Tuo H, Sugiyama M, Oki A, Abe N, Mori T, Masaki T, Atomi Y. Anatomic study of the superior right colic vein: its relevance to pancreatic and colonic surgery. Am J Surg. 2006;191:100-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 68] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 28. | Yamamoto M, Okuda J, Tanaka K, Kondo K, Tanigawa N, Uchiyama K. Clinical outcomes of laparoscopic surgery for advanced transverse and descending colon cancer: a single-center experience. Surg Endosc. 2012;26:1566-1572. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 29. | Amri R, Klos CL, Bordeianou L, Berger DL. The prognostic value of lymph node ratio in colon cancer is independent of resection length. Am J Surg. 2016;212:251-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 30. | Stracci F, Bianconi F, Leite S, Liso A, La Rosa F, Lancellotta V, van de Velde CJ, Aristei C. Linking surgical specimen length and examined lymph nodes in colorectal cancer patients. Eur J Surg Oncol. 2016;42:260-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 31. | Fernández-Cebrián JM, Gil Yonte P, Jimenez-Toscano M, Vega L, Ochando F. Laparoscopic colectomy for transverse colon carcinoma: a surgical challenge but oncologically feasible. Colorectal Dis. 2013;15:e79-e83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 32. | Mori S, Kita Y, Baba K, Yanagi M, Tanabe K, Uchikado Y, Kurahara H, Arigami T, Uenosono Y, Mataki Y, Okumura H, Nakajo A, Maemura K, Natsugoe S. Laparoscopic complete mesocolic excision via combined medial and cranial approaches for transverse colon cancer. Surg Today. 2017;47:643-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 33. | Secco GB, Ravera G, Gasparo A, Percoco P, Zoli S. Segmental resection, lymph nodes dissection and survival in patients with left colon cancer. Hepatogastroenterology. 2007;54:422-426. [PubMed] |
| 34. | Gravante G, Elshaer M, Parker R, Mogekwu AC, Drake B, Aboelkassem A, Rahman EU, Sorge R, Alhammali T, Gardiner K, Al-Hamali S, Rashed M, Kelkar A, Agarwal R, El-Rabaa S. Extended right hemicolectomy and left hemicolectomy for colorectal cancers between the distal transverse and proximal descending colon. Ann R Coll Surg Engl. 2016;98:303-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 35. | Beisani M, Vallribera F, García A, Mora L, Biondo S, Lopez-Borao J, Farrés R, Gil J, Espin E. Subtotal colectomy vs left hemicolectomy for the elective treatment of splenic flexure colonic neoplasia. Am J Surg. 2018;216:251-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 36. | Lee YS, Lee IK, Kang WK, Cho HM, Park JK, Oh ST, Kim JG, Kim YH. Surgical and pathological outcomes of laparoscopic surgery for transverse colon cancer. Int J Colorectal Dis. 2008;23:669-673. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 37. | van Rongen I, Damhuis RA, van der Hoeven JA, Plaisier PW. Comparison of extended hemicolectomy vs transverse colectomy in patients with cancer of the transverse colon. Acta Chir Belg. 2013;113:107-111. [PubMed] |
| 38. | Tjandra JJ, Chan MK. Systematic review on the short-term outcome of laparoscopic resection for colon and rectosigmoid cancer. Colorectal Dis. 2006;8:375-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 181] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 39. | Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW Jr, Hellinger M, Flanagan R Jr, Peters W, Nelson H; Clinical Outcomes of Surgical Therapy Study Group. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg. 2007;246:655-62; discussion 662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 789] [Cited by in RCA: 795] [Article Influence: 44.2] [Reference Citation Analysis (0)] |
| 40. | Bonjer HJ, Hop WC, Nelson H, Sargent DJ, Lacy AM, Castells A, Guillou PJ, Thorpe H, Brown J, Delgado S, Kuhrij E, Haglind E, Påhlman L; Transatlantic Laparoscopically Assisted vs Open Colectomy Trials Study Group. Laparoscopically assisted vs open colectomy for colon cancer: a meta analysis. Arch Surg. 2007;142:298-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 397] [Cited by in RCA: 388] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 41. | Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, Heath RM, Brown JM; UK MRC CLASICC Trial Group. Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol. 2007;25:3061-3068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1108] [Cited by in RCA: 1110] [Article Influence: 61.7] [Reference Citation Analysis (0)] |
| 42. | Yamaguchi S, Tashiro J, Araki R, Okuda J, Hanai T, Otsuka K, Saito S, Watanabe M, Sugihara K. Laparoscopic vs open resection for transverse and descending colon cancer: Short-term and long-term outcomes of a multicenter retrospective study of 1830 patients. Asian J Endosc Surg. 2017;10:268-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 43. | Chand M, Siddiqui MR, Rasheed S, Brown G, Tekkis P, Parvaiz A, Qureshi T. A systematic review and meta-analysis evaluating the role of laparoscopic surgical resection of transverse colon tumours. Surg Endosc. 2014;28:3263-3272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 44. | Geis WP, Coletta AV, Verdeja JC, Plasencia G, Ojogho O, Jacobs M. Sequential psychomotor skills development in laparoscopic colon surgery. Arch Surg. 1994;129:206-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 45. | Schwenk W, Haase O, Neudecker J, Müller JM. Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev. 2005;CD003145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 293] [Cited by in RCA: 431] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 46. | Kuhry E, Schwenk WF, Gaupset R, Romild U, Bonjer HJ. Long-term results of laparoscopic colorectal cancer resection. Cochrane Database Syst Rev. 2008;CD003432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 250] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 47. | Ozben V, de Muijnck C, Esen E, Aytac E, Baca B, Karahasanoglu T, Hamzaoglu I. Is Robotic Complete Mesocolic Excision Feasible for Transverse Colon Cancer? J Laparoendosc Adv Surg Tech A. 2018;28:1443-1450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 48. | Trastulli S, Desiderio J, Farinacci F, Ricci F, Listorti C, Cirocchi R, Boselli C, Noya G, Parisi A. Robotic right colectomy for cancer with intracorporeal anastomosis: short-term outcomes from a single institution. Int J Colorectal Dis. 2013;28:807-814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 49. | Kim CW, Kim CH, Baik SH. Outcomes of robotic-assisted colorectal surgery compared with laparoscopic and open surgery: a systematic review. J Gastrointest Surg. 2014;18:816-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 140] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 50. | Fung AK, Aly EH. Robotic colonic surgery: is it advisable to commence a new learning curve? Dis Colon Rectum. 2013;56:786-796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 51. | Buchs NC, Pugin F, Bucher P, Morel P. Totally robotic right colectomy: a preliminary case series and an overview of the literature. Int J Med Robot. 2011;7:348-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 52. | Araujo SE, Seid VE, Klajner S. Robotic surgery for rectal cancer: current immediate clinical and oncological outcomes. World J Gastroenterol. 2014;20:14359-14370. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 55] [Cited by in RCA: 46] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 53. | Antoniou GA, Riga CV, Mayer EK, Cheshire NJ, Bicknell CD. Clinical applications of robotic technology in vascular and endovascular surgery. J Vasc Surg. 2011;53:493-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 74] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 54. | Bokhari MB, Patel CB, Ramos-Valadez DI, Ragupathi M, Haas EM. Learning curve for robotic-assisted laparoscopic colorectal surgery. Surg Endosc. 2011;25:855-860. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 294] [Cited by in RCA: 314] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 55. | Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S. Standardized surgery for colonic cancer: complete mesocolic excision and central ligation--technical notes and outcome. Colorectal Dis. 2009;11:354-64; discussion 364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 990] [Cited by in RCA: 1093] [Article Influence: 68.3] [Reference Citation Analysis (0)] |
| 56. | Wang Y, Zhang C, Feng YF, Fu Z, Sun YM. Comparison of short-term outcomes between laparoscopic-assisted and open complete mesocolic excision (CME) for the treatment of transverse colon cancer. Chin Clin Oncol. 2017;6:6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 57. | Matsuda T, Sumi Y, Yamashita K, Hasegawa H, Yamamoto M, Matsuda Y, Kanaji S, Oshikiri T, Nakamura T, Suzuki S, Kakeji Y. Anatomical and embryological perspectives in laparoscopic complete mesocoloic excision of splenic flexure cancers. Surg Endosc. 2018;32:1202-1208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 58. | Jung KU, Park Y, Lee KY, Sohn SK. Robotic transverse colectomy for mid-transverse colon cancer: surgical techniques and oncologic outcomes. J Robot Surg. 2015;9:131-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 59. | Mistrangelo M, Allaix ME, Cassoni P, Giraudo G, Arolfo S, Morino M. Laparoscopic versus open resection for transverse colon cancer. Surg Endosc. 2015;29:2196-2202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |