Published online Nov 15, 2021. doi: 10.4251/wjgo.v13.i11.1833
Peer-review started: January 14, 2021
First decision: May 3, 2021
Revised: May 8, 2021
Accepted: July 13, 2021
Article in press: July 13, 2021
Published online: November 15, 2021
Processing time: 301 Days and 19.8 Hours
The long-term survival of patients with solitary hepatocellular carcinoma (HCC) following anatomical resection (AR) vs non-anatomical resection (NAR) is still controversial. It is necessary to investigate which approach is better for patients with solitary HCC.
To compare perioperative and long-term survival outcomes of AR and NAR for solitary HCC.
We performed a comprehensive literature search of PubMed, Medline (Ovid), Embase (Ovid), and Cochrane Library. Participants of any age and sex, who underwent liver resection, were considered following the following criteria: (1) Studies reporting AR vs NAR liver resection; (2) Studies focused on primary HCC with a solitary tumor; (3) Studies reporting the long-term survival outcomes (> 5 years); and (4) Studies including patients without history of preoperative treatment. The main results were overall survival (OS) and disease-free survival (DFS). Perioperative outcomes were also compared.
A total of 14 studies, published between 2001 and 2020, were included in our meta-analysis, including 9444 patients who were mainly from China, Japan, and Korea. AR was performed on 4260 (44.8%) patients. The synthetic results showed that the 5-year OS [odds ratio (OR): 1.19; P < 0.001] and DFS (OR: 1.26; P < 0.001) were significantly better in the AR group than in the NAR group. AR was associated with longer operating time [mean difference (MD): 47.08; P < 0.001], more blood loss (MD: 169.29; P = 0.001), and wider surgical margin (MD = 1.35; P = 0.04) compared to NAR. There was no obvious difference in blood transfusion ratio (OR: 1.16; P = 0.65) or postoperative complications (OR: 1.24, P = 0.18).
AR is superior to NAR in terms of long-term outcomes. Thus, AR can be recom
Core Tip: Anatomical hepatectomy is considered an effective way to treat hepatocellular carcinoma (HCC) in theory. However, there is still no consensus about which surgical technique between anatomical and non-anatomical hepatectomy is more suitable for patients with solitary HCC. This study aimed to compare the long-term survival outcomes between anatomical and non-anatomical hepatectomy in HCC patients undergoing curative resection. Patients with a solitary tumor undergoing AR were associated with a better overall survival.
- Citation: Liu H, Hu FJ, Li H, Lan T, Wu H. Anatomical vs nonanatomical liver resection for solitary hepatocellular carcinoma: A systematic review and meta-analysis. World J Gastrointest Oncol 2021; 13(11): 1833-1846
- URL: https://www.wjgnet.com/1948-5204/full/v13/i11/1833.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v13.i11.1833
Hepatocellular carcinoma (HCC) is the sixth most commonly diagnosed cancer and the fourth most common cause of cancer-related death worldwide[1]. It is estimated that there are about 841000 new cases and 782000 deaths annually[2], causing a heavy economic burden on society and government. The main risk factors for HCC are chronic infection with hepatitis B virus (HBV) or hepatitis C virus (HCV), alcohol abuse, aflatoxin, obesity, and type 2 diabetes[3]. China and Eastern Africa are the most high-risk HCC areas globally with a high prevalence of HBV and exposure to aflatoxin. Surgical resection is still considered the first-line treatment for HCC in patients with preserved liver function[4,5], especially for patients who have a solitary HCC. The ideal candidates for surgical resection are patients with a single tumor at an early stage, Child–Pugh class A, no clinically significant portal hypertension, and good performance status[6]. However, the high incidence of postoperative recurrence of HCC remains an unresolved challenge.
Anatomical resection (AR), which was first proposed in the 1980s, was defined as complete removal of one Couinaud’s segment (i.e., segments I-VIII) or a combination of contiguous territories of the third-order subsegmental portal venous branches smaller than one Couinaud’s segment[7]. In theory, AR can produce a better survival outcome by systematic removal of the tumor-bearing portal territories. However, as reported recently, some studies have found that non-anatomical resection (NAR) could achieve a more satisfactory outcome compared with AR[8-10]. Others have concluded that AR can significantly improve the long-term survival results[11,12]. Thus, the superiority of AR for solitary HCC is not clear.
The aim of the present study was to compare the long-term outcomes of AR and NAR for solitary HCC.
This systematic review and meta-analysis is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. The protocol for this review was registered with PROSPERO (number: CRD42020213382).
The electronic databases PubMed, Medline (Ovid), Embase (Ovid), and Cochrane Library were searched for eligible studies from the inception of each database to September 30, 2020. Only studies published in English were included. The following algorithm was applied: (anatomic resection OR anatomical resection OR non-anatomic resection OR non-anatomical resection OR nonanatomic resection OR non-anatomical resection OR limited resection OR systematic resection OR partial resection OR wedged resection) AND (single hepatocellular carcinoma OR solitary hepatocellular carcinoma). Two reviewers (Liu H and Hu FJ) performed the initial literature screening independently. The titles and abstracts were reviewed to identify all potential articles.
The inclusion criteria were as follows: (1) Studies reporting AR vs NAR liver resection; (2) Studies focused on primary HCC with a solitary tumor; (3) Studies reporting the long-term survival outcomes (> 5 years); and (4) Studies including patients without history of preoperative treatment.
The exclusion criteria were as follows: (1) Noncomparative studies; (2) Conference abstracts and case reports; (3) Review articles and editorials; and (4) Studies without data of interest. Duplicated studies by the same authors or centers would be distinguished carefully. The largest patient cohorts were included in this analysis. However, if the patient samples were enrolled at different times, both were included.
Essential information and continuous or dichotomous data for special outcomes of each eligible article were extracted by two independent investigators (Liu H and Hu FJ), using the customized data extraction form that included the following items: Study ID; year of publication; country; sample size; age of participants; number of male patients; HBV and HCV infection; cirrhosis; hepatic function (Child–Pugh class A/B); α-fetoprotein (AFP); des-γ-carboxy prothrombin (DCP); indocyanine green retention rate at 15 min (ICGR-15); tumor characteristics (size and microvascular invasion); perioperative characteristics (operating time, amount of blood loss, blood transfusion, and surgical margin); postoperative complications; duration of hospital stay; duration of follow-up; and long-term outcomes [overall survival (OS) and disease-free survival (DFS)]. If OS and DFS were not summarized in tables or texts directly, they were calculated from the Kaplan–Meier graph using Engauge Digitizer (version 7.2). Disagreements were settled through discussion until reaching a consensus.
Two authors independently assessed the quality of the included studies using the modified Newcastle-Ottawa Scale, which included three broad perspectives: Selection of study groups, comparability of the groups, and ascertainment of exposure or outcome of interest[13,14]. Total score ranged from 0 to 9. Scores > 6 were regarded as high quality[15].
The meta-analysis was performed using Cochrane Collaboration’s Review Manager 5.3 software. The intervention effect was expressed as odds ratios (ORs) for dichotomous outcomes and mean differences (MDs) for continuous outcome measures, with 95% confidence intervals (CIs). Heterogeneity was assessed by χ2 and I2 tests. A random effects model was used routinely only if there was no obvious heterogeneity among the included studies (I2 < 40%)[16].
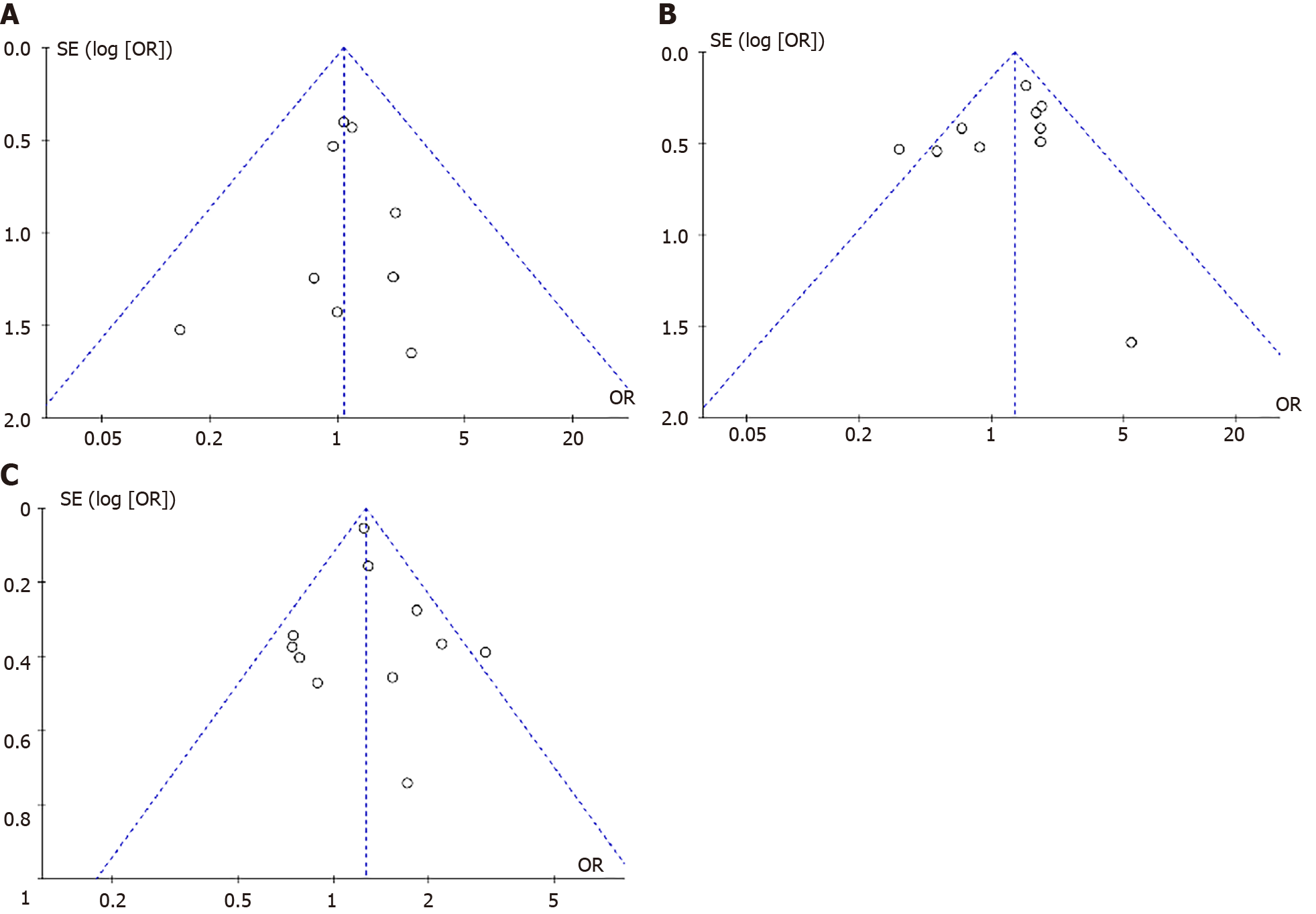
Sensitivity analysis was conducted by deleting the included studies in sequence to recognize the stability of the total effect. Funnel plot was used to assess the publication bias. Begg’s test and Egger’s test were used to evaluate the symmetry of the funnel plot.
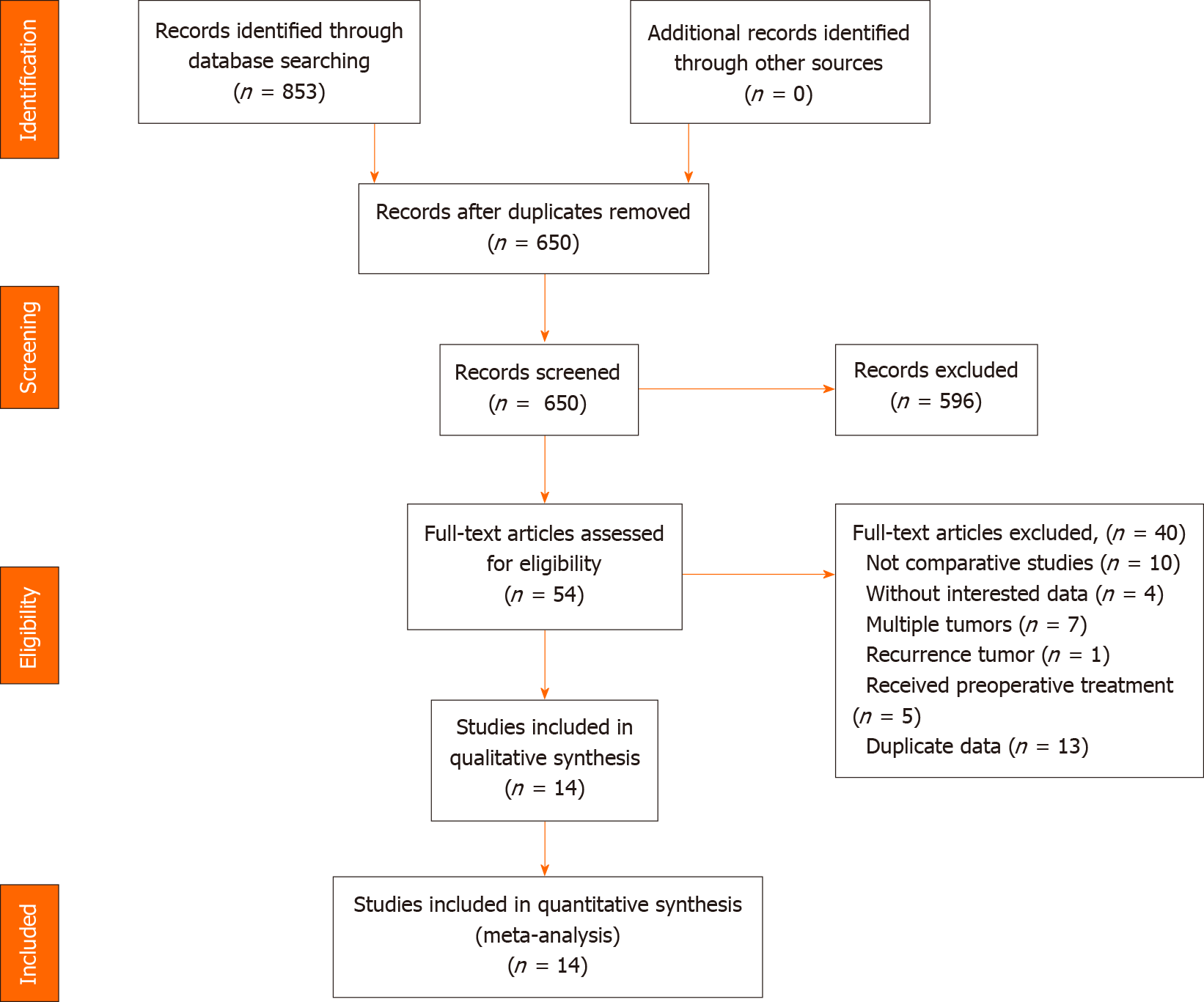
A total of 853 records were retrieved, and 799 records were excluded by reading titles and abstracts because of irrelevance to our theme. By assessing full-text articles of the remaining studies, 14 (with data for 9444 participants) that compared the outcomes between AR and NAR for patients with solitary HCC were included in this meta-analysis[10,12,17-28]. They were published between 2001 and 2020. Eight studies using propensity score matching aimed to reduce the bias and confounding variables[10,12,18,20,21,23,24,26]. All the included studies were from Asia (Table 1), including two from China[18,20], three from Korea[10,19,22], and nine from Japan[11,12,17,21,23-38]. Most studies were marked 7 or 8 stars (Supplementary Table 1). All studies were deemed of high quality. Detailed search steps were described using the PRISMA 2009 flow diagram (Figure 1).
| Ref. | Country | Enrollment of period | Design/center | Patients | Quality score | |
| AR | NAR | |||||
| Cho et al[10], 2019 | Korea | Jan 2008-Sep 2014 | R/Single | 59 | 59 | 8 |
| Eguchi et al[27], 2008 | Japan | 1994-2001 | R/Multiple | 2267 | 3514 | 7 |
| Hirokawa et al[23], 2015 | Japan | Jan 2001-Dec 2005 | R/Multiple | 72 | 72 | 8 |
| Hokuto et al[12], 2018 | Japan | Jan 2007-Dec 2015 | R/Single | 20 | 20 | 8 |
| Ishii et al[26], 2014 | Japan | Jan 2002-Dec 2010 | R/Single | 44 | 44 | 8 |
| Jung et al[18], 2019 | Korea | Jan 2006-Dec 2014 | R/Single | 936 | 388 | 8 |
| Kaibori et al[21], 2017 | Japan | 2003-2007 | R/Multiple | 355 | 355 | 7 |
| Kim et al[22], 2016 | Korea | Jan 2003-Dec 2009 | R/Single | 27 | 72 | 7 |
| Kudo et al[25], 2014 | Japan | Apr 2000-Mar 2012 | R/Single | 121 | 112 | 7 |
| Okamura et al[24], 2014 | Japan | Sep 2002-May 2013 | R/Single | 64 | 64 | 8 |
| Shin et al[19], 2018 | Korea | Jan 2006-Dec 2015 | R/Single | 53 | 63 | 7 |
| Shindoh et al[52], 2020 | Japan | Jan 2011-Oct 2017 | R/Single | 38 | 165 | 7 |
| Yamamoto et al[28], 2001 | Japan | 1990-1994 | R/Single | 90 | 114 | 7 |
| Zhao et al[20], 2017 | China | Jan 2004-Dec 2013 | R/Multiple | 114 | 114 | 8 |
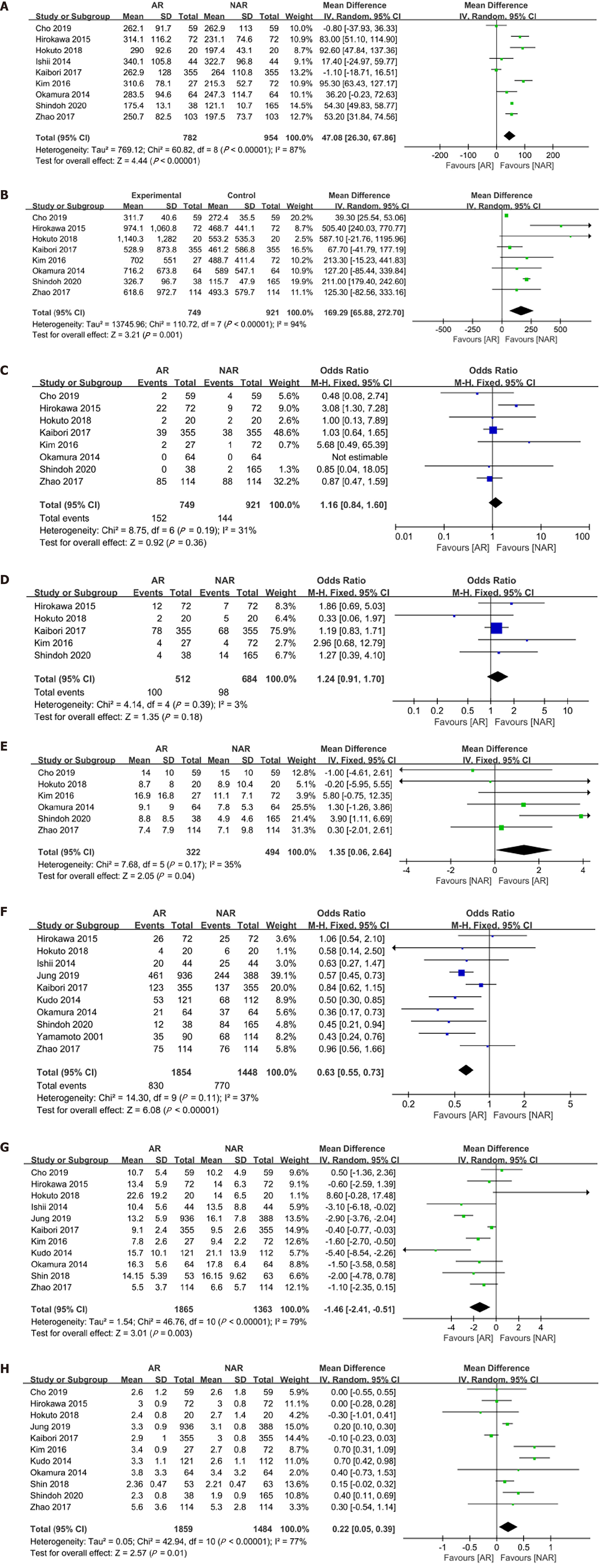
Pooled outcomes showed that the patients in the AR group were characterized by a lower proportion of cirrhosis, smaller tumor size, lower ICG-R15, longer surgical time, and more intraoperative blood loss in comparison with those in the NAR group. The data and the forest plots are displayed in Supplementary Table 2 and Figure 2.
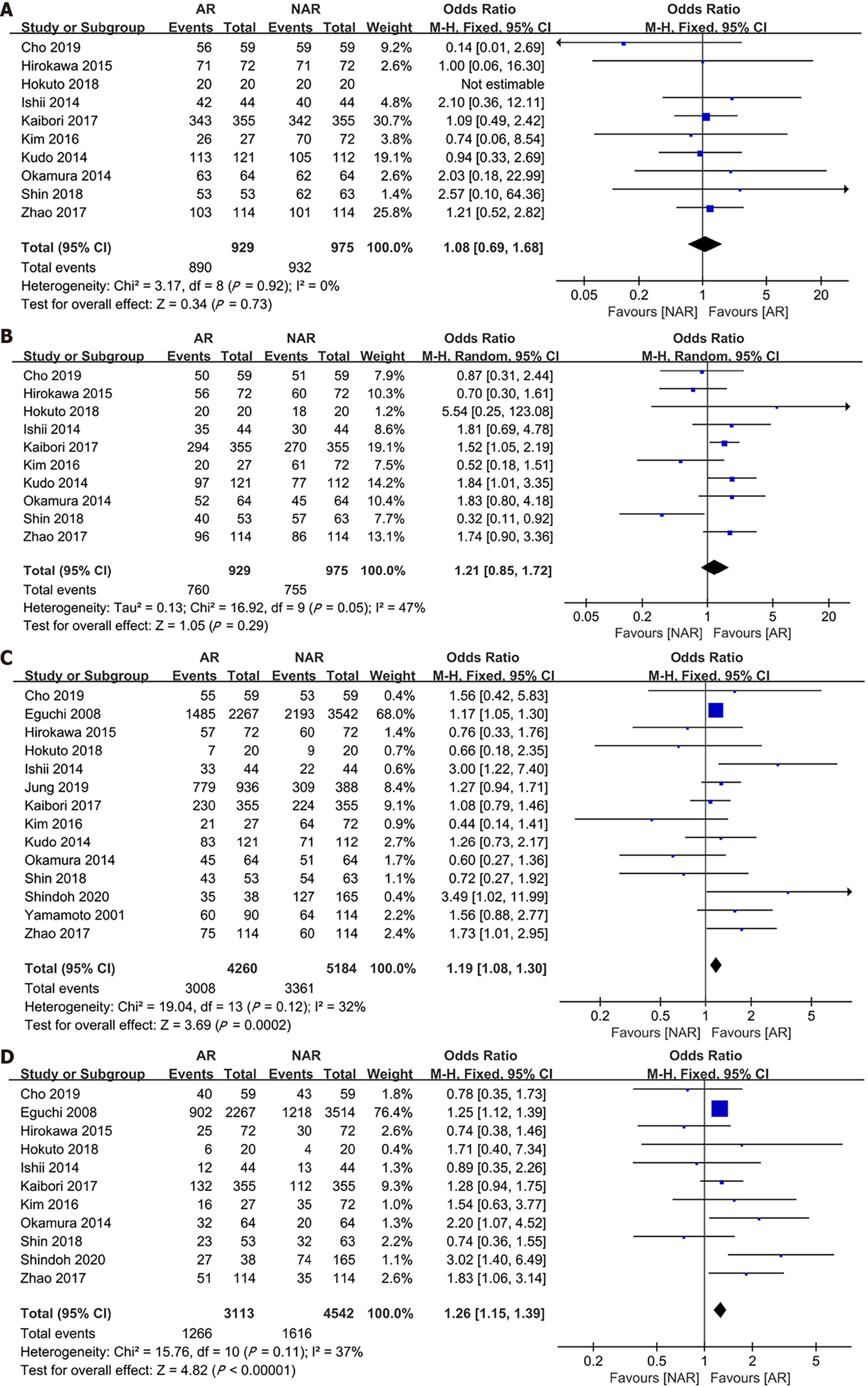
For OS of the two groups, the postoperative 5-year survival rates were 69.8% and 63.7%, respectively (Table 2). All included studies reported 5-year OS, and the pooled outcome showed that the AR group was associated with a better survival (OR: 1.19, fixed model, I2 = 32%, 95%CI: 1.08-1.30, Z = 3.69, P < 0.001)[10,12,17-28]. Concerning 5-year DFS rates, there were 11 studies including 7655 patients. Patients who underwent AR tended to have a better 5-year DFS in comparison with the NAR group (OR: 1.26, fixed model, I2 = 37%, 95%CI: 1.15-1.39, Z = 4.82, P < 0.001)[10,12,17,19-24,26,27]. Ten studies analyzed 1-year DFS of 2110 patients undergoing liver resection, and the pooled result displayed that there was no difference in 1-year DFS (OR: 1.21, random model, I2 = 47%, 95%CI: 0.85-1.72, Z = 1.05, P = 0.29)[10,12,19-26] or 1-year OS (OR: 1.19, fixed model, I2 = 0%, 95%CI: 0.79-1.78, Z = 0.83, P = 0.41)[10,12,19-26]. Details of the data and forest plot are shown in Supplementary Table 3 and Figure 3 respecti
| Studies | Patients | MD/OR (95%CI) | P value | Study heterogeneity | |||||
| AR | NAR | χ2 | df | I2, % | P value | ||||
| Operating time (min) | 9 | 782 | 954 | 47.08 (26.30-67.86) | < 0.001 | 60.82 | 8 | 87 | < 0.001 |
| Blood loss (mL) | 8 | 749 | 921 | 169.29 (65.88-272.70) | 0.001 | 110.72 | 7 | 94 | < 0.001 |
| Blood transfusion | 8 | 749 | 921 | 1.16 (0.84-1.60) | 0.36 | 8.75 | 6 | 31 | 0.19 |
| Surgical margin (mm) | 6 | 322 | 494 | 1.35 (0.06-2.64) | 0.04 | 7.68 | 5 | 35 | 0.17 |
| Complication | 5 | 512 | 684 | 1.24 (0.91-1.70) | 0.18 | 4.14 | 4 | 3 | 0.39 |
| 1-yr OS | 10 | 929 | 975 | 1.08 (0.69-1.68) | 0.73 | 3.17 | 8 | 0 | 0.92 |
| 1-yr DFS | 10 | 929 | 975 | 1.21 (0.85-1.72) | 0.29 | 16.92 | 9 | 47 | 0.05 |
| 5-yr OS | 14 | 4260 | 5184 | 1.19 (1.08-1.30) | < 0.001 | 19.04 | 13 | 32 | 0.12 |
| 5-yr DFS | 11 | 3113 | 4542 | 1.26 (1.15-1.39) | < 0.001 | 15.76 | 10 | 37 | 0.11 |
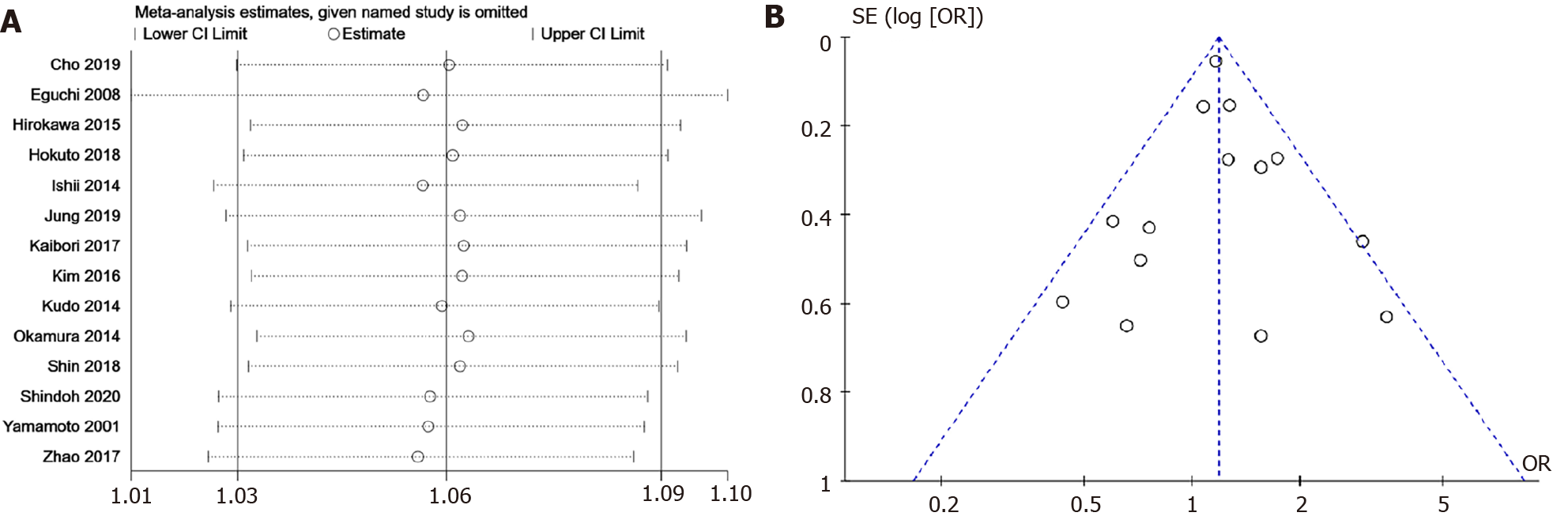
A sensitivity analysis was performed by omitting the included studies in turn to recognize the stability of synthesized 5-year OS. OS was steady as pooled ORs did not alter significantly after eliminating the enrolled studies in sequence (Figure 4A). No evidence of bias was observed in the selected funnel plot (Figure 4B), and other clinical outcomes were also displayed (Figure 5). Similarly, the Begg’s test (Z = 0.22, P = 0.827) and Egger’s test (bias coefficient = 0.026, SE = 0.471, t = 0.05, P = 0.957) were conducted to evaluate funnel plot symmetry. These results demonstrated no obvious evidence of publication bias.
In the management of HCC, the attainment of long-term survival is compromised by the choice of therapeutic method. Although there are various alternative treatment choices, liver resection is still considered the most ideal curative option for HCC, especially for patients with a solitary tumor[6,39]. Whether to perform AR or NAR is a sophisticated decision based on considering the balance between radical resection and avoiding postoperative liver failure from removing too much liver parenchyma, especially in patients with cirrhosis. AR is always related to major liver resection, which may induce a high risk of postoperative liver dysfunction. On the contrary, NAR aims to decrease the incidence of postoperative complications including liver failure. The oncological and long-term benefit of AR is always a debate, and has been studied for many years[40-43]. Due to the high heterogeneity of HCC at both the molecular and clinical levels[44], it is difficult to conduct a high-quality randomized controlled trial (RCT) comparing AR and NAR. A recent meta-analysis using propensity score matching has shown that AR can yield better local control of the disease[45]. Previous studies have suggested that AR provides better long-term outcomes[27,38,46]. Comparable findings have been found by other studies between AR and NAR[9,10,12,19,22-24,31,32,36]. Thus, it remains unclear whether AR has oncological and prognostic superiority as an effective treatment for HCC.
The pooled outcomes showed that, compared with NAR, complete removal of the tumor-bearing third-order portal territories was associated with significantly improved long-term outcomes, including 5-year OS and DFS, with no increase in postoperative complications and transfusion. Our results thus contribute to current knowledge by providing evidence that AR is a satisfactory treatment strategy that can achieve the ideal long-term outcomes in solitary HCC. Several included studies showed that AR is not superior to NAR in terms of long-term outcomes, which disagrees with our pooled outcomes. Shin et al[19] reported that the outcomes of NAR are comparable with those of AR in single HCC < 3 cm. Kim et al[22] found that the long-term survival of NAR for solitary HCC < 5 cm is comparable to that achieved with AR. The reason for this is the different tumor characteristics in that study. Specifically, the tumor size and the proportion of microvascular invasion in the AR group were larger than those in the NAR group. Hirokawa et al[23] also presented similar outcomes by using propensity score matching. This might be because the included patients had no macroscopic vascular invasion, which decreased the advantage of AR. Limited by the reported data, we did not conduct a subgroup analysis in term of tumor size. Further studies are needed to determine the optimal choice for the application of AR for different tumor sizes.
Perioperative outcomes showed that AR was associated with longer operating time, more blood loss, and wider surgical margins when compared to NAR. To our knowledge, AR is always related to major liver resection, and is generally regarded as a more technically demanding operation. Unlike other tumors, underlying liver function plays an important role in patients’ prognosis after initial liver resection[47,48]. As is known to us, impaired liver function is associated with a worse prognosis. Because of the superiority of AR and the preference of surgeons, AR is always conducted in patients with better liver function compared to NAR, and our synthetic results proved this. Although part of included studies used propensity score matching to decrease confounders as much as possible, liver function is still a potential confounder which cannot be bypassed, and we need take it into consideration when interpreting the result. Less remnant liver volume, more intraoperative loss, and longer operating time were related to AR, which theoretically increased the risk of postoperative complications such as liver failure. Although AR is a more challenging procedure than NAR, we did not observe differences in the blood transfusion ratio or postoperative complications. Thus, our results offer powerful support for surgeons to choose AR.
It is estimated that close to 70% of patients with HCC will relapse within 5 years following surgery[49]. HCC has a unique pattern of metastasis via the portal vein. The mechanisms of recurrence can be either intrahepatic metastasis from the initial tumor or a de novo multicentric tumor[50]. Intrahepatic metastasis may be due to residual micrometastases from the HCC spreading through the portal venous system[7,51]. AR can theoretically prevent the progression of HCC by eradicating the primary tumor and microvascular metastasis. Several studies[12,17,18] have demonstrated that OS was significantly better after AR than NAR. The outcomes were in accordance with the outcomes of our meta-analysis. Hence, our finding of a better 5-year DFS after AR than NAR indicated that this procedure is advantageous for improvement of long-term survival.
Our study had several limitations. First, there were no RCTs and most were retrospective. Included samples mainly consisted of Japanese cohorts. Selection bias of enrolled studies might not have been completely negligible, even after the adjustment of propensity scoring. Second, among different medical centers, a standard surgical procedure was not available, and the experience of surgeons may have had an impact on perioperative outcomes, especially operating time, blood loss, and morbidity. Third, the sample size of several included studies was small. Prognosis of HCC is highly dependent on the selection and quality of repeat treatment for recurrence[52], which is another crucial factor that deserves to be further analyzed. There is still a need for a well-designed RCT that is characterized by larger samples and multiple centers to verify the advantage of AR over NAR for patients with solitary HCC.
In conclusion, this meta-analysis indicated that AR improves the 5-year DFS and OS in patients with solitary HCC. Thus, AR should be recommended as the primary option as long as such a surgical maneuver is feasible.
Patients diagnosed with solitary hepatocellular carcinoma (HCC) always receive liver resection. More and more patients are undergoing anatomical hepatectomy which aims to eradicate tumor. Accumulating studies had been performed to compare these two kinds of surgical technique. However, it is still not yet whether anatomical hepatectomy is superior to non-anatomical hepatectomy.
Clarifying the survival benefits of anatomical and non-anatomical hepatectomy is of vital importance for patients with solitary HCC. Furthermore, it will be instructive for doctors to choose better surgical method.
To perform a systematic review and meta-analysis on short- and long-term results of anatomical and non-anatomical hepatectomy in patients with solitary HCC.
PubMed, Medline (Ovid), Embase (Ovid), and Cochrane Library were searched for articles from the inception of each database to 2020 according to the designed extraction scheme, and statistical analysis was performed using Cochrane Collaboration’s Review Manager 5.3 software. The quality of included papers was assessed with the modified Newcastle-Ottawa Scale. The main results of this study included overall survival (OS) and disease-free survival (DFS).
Fourteen studies (9444 patients) comparing anatomical and non-anatomical hepatectomy were included for final analysis with 4260 cases of anatomical resection (AR) and 5184 cases of non-anatomical resection (NAR). Anatomical hepatectomy was associated with a higher 5-year OS [odds ratio (OR): 1.10, 95% confidence interval (CI): 1.08-1.30] and DFS (OR: 1.26, 95%CI: 1.15-1.39). AR was associated with longer operating time [mean difference (MD): 47.08; P < 0.001], more blood loss (MD: 169.29; P = 0.001), and wider surgical margin (MD = 1.35; P = 0.04) compared to NAR. There was no obvious difference in blood transfusion ratio (OR: 1.16; P = 0.65) or postoperative complications between the two groups (OR: 1.24, P = 0.18).
This meta-analysis confirmed that AR is superior to NAR in terms of long-term outcomes. Thus, AR can be recommended as a reasonable surgical approach in patients with solitary HCC.
There are some limitations that should be taken into consideration when interpreting the results. The most vital limitation is that the included studies are non-randomized controlled trial and retrospective. Future studies with large-scale and well-designed randomized controlled trial are needed to further verify the benefits of anatomical hepatectomy for patients with solitary HCC.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tsakatikas S, Vij M S-Editor: Gao CC L-Editor: Wang TQ P-Editor: Guo X
| 1. | Villanueva A. Hepatocellular Carcinoma. N Engl J Med. 2019;380:1450-1462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2066] [Cited by in RCA: 3165] [Article Influence: 527.5] [Reference Citation Analysis (37)] |
| 2. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 55806] [Article Influence: 7972.3] [Reference Citation Analysis (132)] |
| 3. | McGlynn KA. Liver cancer. In: Thun MJ, Linet MS, Cerhan JR, Haiman CA, Schottenfeld D. Cancer Epidemiology and Prevention. 4th ed. New York: Oxford University Press, 2018: 635-660. |
| 4. | Kudo M, Izumi N, Kokudo N, Matsui O, Sakamoto M, Nakashima O, Kojiro M, Makuuchi M; HCC Expert Panel of Japan Society of Hepatology. Management of hepatocellular carcinoma in Japan: Consensus-Based Clinical Practice Guidelines proposed by the Japan Society of Hepatology (JSH) 2010 updated version. Dig Dis. 2011;29:339-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 549] [Cited by in RCA: 664] [Article Influence: 47.4] [Reference Citation Analysis (0)] |
| 5. | Bruix J, Sherman M; American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020-1022. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5972] [Cited by in RCA: 6572] [Article Influence: 469.4] [Reference Citation Analysis (1)] |
| 6. | Roayaie S, Jibara G, Tabrizian P, Park JW, Yang J, Yan L, Schwartz M, Han G, Izzo F, Chen M, Blanc JF, Johnson P, Kudo M, Roberts LR, Sherman M. The role of hepatic resection in the treatment of hepatocellular cancer. Hepatology. 2015;62:440-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 321] [Article Influence: 32.1] [Reference Citation Analysis (0)] |
| 7. | Makuuchi M, Hasegawa H, Yamazaki S. Ultrasonically guided subsegmentectomy. Surg Gynecol Obstet. 1985;161:346-350. [PubMed] |
| 8. | Huang SW, Chu PY, Ariizumi S, Lin CC, Wong HP, Chou DA, Lee MT, Wu HJ, Yamamoto M. Anatomical Versus Non-anatomical Resection for Hepatocellular Carcinoma, a Propensity-matched Analysis Between Taiwanese and Japanese Patients. In Vivo. 2020;34:2607-2612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Shi F, Zhou Z, Huang X, Liu Q, Lin A. Is anatomical resection necessary for early hepatocellular carcinoma? Future Oncol. 2019;15:2041-2051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Cho CW, Choi GS, Kim JM, Kwon CHD, Joh JW. Long-Term Oncological Outcomes of Laparoscopic Liver Resection for Solitary Hepatocellular Carcinoma: Comparison of Anatomical and Nonanatomical Resection Using Propensity Score Matching Analysis. J Laparoendosc Adv Surg Tech A. 2019;29:752-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Kaibori M, Yoshii K, Hasegawa K, Ariizumi S, Kobayashi T, Kamiyama T, Kudo A, Yamaue H, Kokudo N, Yamamoto M. Impact of systematic segmentectomy for small hepatocellular carcinoma. J Hepatobiliary Pancreat Sci. 2020;27:331-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 12. | Hokuto D, Nomi T, Yasuda S, Yoshikawa T, Ishioka K, Yamada T, Takahiro A, Nakagawa K, Nagai M, Nakamura K, Kanehiro H, Sho M. Does anatomic resection improve the postoperative outcomes of solitary hepatocellular carcinomas located on the liver surface? Surgery. 2018;163:285-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in Meta-analyses. Oxford: Ottawa Hospital Research Institute, 2014. |
| 14. | Li H, Zheng J, Cai JY, Li SH, Zhang JB, Wang XM, Chen GH, Yang Y, Wang GS. Laparoscopic VS open hepatectomy for hepatolithiasis: An updated systematic review and meta-analysis. World J Gastroenterol. 2017;23:7791-7806. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 27] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (1)] |
| 15. | Ownby RL, Crocco E, Acevedo A, John V, Loewenstein D. Depression and risk for Alzheimer disease: systematic review, meta-analysis, and metaregression analysis. Arch Gen Psychiatry. 2006;63:530-538. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1104] [Cited by in RCA: 1037] [Article Influence: 54.6] [Reference Citation Analysis (0)] |
| 16. | Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane Handbook for Systematic Reviews of Interventions. 2nd ed. Chichester, United Kingdom: John Wiley & Sons, 2019. |
| 17. | Shindoh J, Kobayashi Y, Umino R, Kojima K, Okubo S, Hashimoto M. Successful Anatomic Resection of Tumor-Bearing Portal Territory Delays Long-Term Stage Progression of Hepatocellular Carcinoma. Ann Surg Oncol. 2021;28:844-853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 18. | Jung DH, Hwang S, Lee YJ, Kim KH, Song GW, Ahn CS, Moon DB, Lee SG. Small Hepatocellular Carcinoma With Low Tumor Marker Expression Benefits More From Anatomical Resection Than Tumors With Aggressive Biology. Ann Surg. 2019;269:511-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 19. | Shin S, Kim TS, Lee JW, Ahn KS, Kim YH, Kang KJ. Is the anatomical resection necessary for single hepatocellular carcinoma smaller than 3 cm? Ann Hepatobiliary Pancreat Surg. 2018;22:326-334. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Zhao H, Chen C, Gu S, Yan X, Jia W, Mao L, Qiu Y. Anatomical vs non-anatomical resection for solitary hepatocellular carcinoma without macroscopic vascular invasion: A propensity score matching analysis. J Gastroenterol Hepatol. 2017;32:870-878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 76] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 21. | Kaibori M, Kon M, Kitawaki T, Kawaura T, Hasegawa K, Kokudo N, Ariizumi S, Beppu T, Ishizu H, Kubo S, Kamiyama T, Takamura H, Kobayashi T, Kim DS, Wang HJ, Kim JM, Han DH, Park SJ, Kang KJ, Hwang S, Roh Y, You YK, Joh JW, Yamamoto M. Comparison of anatomic and non-anatomic hepatic resection for hepatocellular carcinoma. J Hepatobiliary Pancreat Sci. 2017;24:616-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 70] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 22. | Kim JM, Kwon CHD, Joh JW, Na BG, Lee KW, Choi GS, Lee JH. Nonanatomical resection is comparable with anatomical resection in solitary hepatocellular carcinoma <5 cm in the right posterior section. Medicine (Baltimore). 2016;95:e5382. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Hirokawa F, Kubo S, Nagano H, Nakai T, Kaibori M, Hayashi M, Takemura S, Wada H, Nakata Y, Matsui K, Ishizaki M, Uchiyama K. Do patients with small solitary hepatocellular carcinomas without macroscopically vascular invasion require anatomic resection? Surgery. 2015;157:27-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 24. | Okamura Y, Ito T, Sugiura T, Mori K, Uesaka K. Anatomic vs nonanatomic hepatectomy for a solitary hepatocellular carcinoma : a case-controlled study with propensity score matching. J Gastrointest Surg. 2014;18:1994-2002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 74] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 25. | Kudo A, Tanaka S, Ban D, Matsumura S, Irie T, Nakamura N, Arii S. Anatomic resection reduces the recurrence of solitary hepatocellular carcinoma ≤5 cm without macrovascular invasion. Am J Surg. 2014;207:863-869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Ishii M, Mizuguchi T, Kawamoto M, Meguro M, Ota S, Nishidate T, Okita K, Kimura Y, Hui TT, Hirata K. Propensity score analysis demonstrated the prognostic advantage of anatomical liver resection in hepatocellular carcinoma. World J Gastroenterol. 2014;20:3335-3342. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 47] [Cited by in RCA: 51] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 27. | Eguchi S, Kanematsu T, Arii S, Okazaki M, Okita K, Omata M, Ikai I, Kudo M, Kojiro M, Makuuchi M, Monden M, Matsuyama Y, Nakanuma Y, Takayasu K; Liver Cancer Study Group of Japan. Comparison of the outcomes between an anatomical subsegmentectomy and a non-anatomical minor hepatectomy for single hepatocellular carcinomas based on a Japanese nationwide survey. Surgery. 2008;143:469-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 292] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 28. | Yamamoto M, Takasaki K, Ohtsubo T, Katsuragawa H, Fukuda C, Katagiri S. Effectiveness of systematized hepatectomy with Glisson's pedicle transection at the hepatic hilus for small nodular hepatocellular carcinoma: retrospective analysis. Surgery. 2001;130:443-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 98] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 29. | Shindoh J, Makuuchi M, Matsuyama Y, Mise Y, Arita J, Sakamoto Y, Hasegawa K, Kokudo N. Complete removal of the tumor-bearing portal territory decreases local tumor recurrence and improves disease-specific survival of patients with hepatocellular carcinoma. J Hepatol. 2016;64:594-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 166] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 30. | Shindoh J, Hasegawa K, Inoue Y, Ishizawa T, Nagata R, Aoki T, Sakamoto Y, Sugawara Y, Makuuchi M, Kokudo N. Risk factors of post-operative recurrence and adequate surgical approach to improve long-term outcomes of hepatocellular carcinoma. HPB (Oxford). 2013;15:31-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 101] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 31. | Sasaki K, Matsuda M, Ohkura Y, Hashimoto M, Watanabe G. Anatomical vs nonanatomical resection in patients with hepatocellular carcinoma located in the left lateral segment. Am Surg. 2013;79:1163-1170. [PubMed] |
| 32. | Tomimaru Y, Eguchi H, Marubashi S, Wada H, Kobayashi S, Tanemura M, Umeshita K, Doki Y, Mori M, Nagano H. Equivalent outcomes after anatomical and non-anatomical resection of small hepatocellular carcinoma in patients with preserved liver function. Dig Dis Sci. 2012;57:1942-1948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 33. | Yamazaki O, Matsuyama M, Horii K, Kanazawa A, Shimizu S, Uenishi T, Ogawa M, Tamamori Y, Kawai S, Nakazawa K, Otani H, Murase J, Mikami S, Higaki I, Arimoto Y, Hanba H. Comparison of the outcomes between anatomical resection and limited resection for single hepatocellular carcinomas no larger than 5 cm in diameter: a single-center study. J Hepatobiliary Pancreat Sci. 2010;17:349-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 34. | Kamiyama T, Nakanishi K, Yokoo H, Kamachi H, Matsushita M, Todo S. The impact of anatomical resection for hepatocellular carcinoma that meets the Milan criteria. J Surg Oncol. 2010;101:54-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 35. | Tanaka K, Shimada H, Matsumoto C, Matsuo K, Nagano Y, Endo I, Togo S. Anatomic vs limited nonanatomic resection for solitary hepatocellular carcinoma. Surgery. 2008;143:607-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 109] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 36. | Nanashima A, Sumida Y, Abo T, Nagasaki T, Tobinaga S, Fukuoka H, Takeshita H, Hidaka S, Tanaka K, Sawai T, Yasutake T, Nagayasu T. Comparison of survival between anatomic and non-anatomic liver resection in patients with hepatocellular carcinoma: significance of surgical margin in non-anatomic resection. Acta Chir Belg. 2008;108:532-537. [PubMed] |
| 37. | Yamashita Y, Taketomi A, Itoh S, Kitagawa D, Kayashima H, Harimoto N, Tsujita E, Kuroda Y, Maehara Y. Longterm favorable results of limited hepatic resections for patients with hepatocellular carcinoma: 20 years of experience. J Am Coll Surg. 2007;205:19-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 108] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 38. | Hasegawa K, Kokudo N, Imamura H, Matsuyama Y, Aoki T, Minagawa M, Sano K, Sugawara Y, Takayama T, Makuuchi M. Prognostic impact of anatomic resection for hepatocellular carcinoma. Ann Surg. 2005;242:252-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 482] [Cited by in RCA: 503] [Article Influence: 25.2] [Reference Citation Analysis (0)] |
| 39. | Kudo M, Matsui O, Izumi N, Iijima H, Kadoya M, Imai Y, Okusaka T, Miyayama S, Tsuchiya K, Ueshima K, Hiraoka A, Ikeda M, Ogasawara S, Yamashita T, Minami T, Yamakado K; Liver Cancer Study Group of Japan. JSH Consensus-Based Clinical Practice Guidelines for the Management of Hepatocellular Carcinoma: 2014 Update by the Liver Cancer Study Group of Japan. Liver Cancer. 2014;3:458-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 401] [Cited by in RCA: 489] [Article Influence: 44.5] [Reference Citation Analysis (0)] |
| 40. | Kishi Y, Saiura A, Yamamoto J, Koga R, Seki M, Morimura R, Yoshioka R, Kokudo N, Yamaguchi T. Significance of anatomic resection for early and advanced hepatocellular carcinoma. Langenbecks Arch Surg. 2012;397:85-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 41. | Zhou Y, Xu D, Wu L, Li B. Meta-analysis of anatomic resection vs nonanatomic resection for hepatocellular carcinoma. Langenbecks Arch Surg. 2011;396:1109-1117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 84] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 42. | Tanaka S, Mogushi K, Yasen M, Noguchi N, Kudo A, Kurokawa T, Nakamura N, Inazawa J, Tanaka H, Arii S. Surgical contribution to recurrence-free survival in patients with macrovascular-invasion-negative hepatocellular carcinoma. J Am Coll Surg. 2009;208:368-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 43. | Wakai T, Shirai Y, Sakata J, Kaneko K, Cruz PV, Akazawa K, Hatakeyama K. Anatomic resection independently improves long-term survival in patients with T1-T2 hepatocellular carcinoma. Ann Surg Oncol. 2007;14:1356-1365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 141] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 44. | Nault JC, Villanueva A. Intratumor molecular and phenotypic diversity in hepatocellular carcinoma. Clin Cancer Res. 2015;21:1786-1788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 72] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 45. | Famularo S, Ceresoli M, Giani A, Ciulli C, Pinotti E, Romano F, Braga M, De Carlis L, Gianotti L. Is It Just a Matter of Surgical Extension to Achieve the Cure of Hepatocarcinoma? J Gastrointest Surg. 2021;25:94-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 46. | Cucchetti A, Qiao GL, Cescon M, Li J, Xia Y, Ercolani G, Shen F, Pinna AD. Anatomic vs nonanatomic resection in cirrhotic patients with early hepatocellular carcinoma. Surgery. 2014;155:512-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 110] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 47. | Cucchetti A, Cescon M, Ercolani G, Bigonzi E, Torzilli G, Pinna AD. A comprehensive meta-regression analysis on outcome of anatomic resection vs nonanatomic resection for hepatocellular carcinoma. Ann Surg Oncol. 2012;19:3697-3705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 97] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 48. | Portolani N, Coniglio A, Ghidoni S, Giovanelli M, Benetti A, Tiberio GA, Giulini SM. Early and late recurrence after liver resection for hepatocellular carcinoma: prognostic and therapeutic implications. Ann Surg. 2006;243:229-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 706] [Cited by in RCA: 728] [Article Influence: 38.3] [Reference Citation Analysis (0)] |
| 49. | Ishizawa T, Hasegawa K, Aoki T, Takahashi M, Inoue Y, Sano K, Imamura H, Sugawara Y, Kokudo N, Makuuchi M. Neither multiple tumors nor portal hypertension are surgical contraindications for hepatocellular carcinoma. Gastroenterology. 2008;134:1908-1916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 513] [Cited by in RCA: 582] [Article Influence: 34.2] [Reference Citation Analysis (0)] |
| 50. | Poon RT. Differentiating early and late recurrences after resection of HCC in cirrhotic patients: implications on surveillance, prevention, and treatment strategies. Ann Surg Oncol. 2009;16:792-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 106] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 51. | Nakashima T, Kojiro M. Pathologic characteristics of hepatocellular carcinoma. Semin Liver Dis. 1986;6:259-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 102] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 52. | Shindoh J, Kawamura Y, Kobayashi Y, Akuta N, Kobayashi M, Suzuki Y, Ikeda K, Hashimoto M. Time-to-Interventional Failure as a New Surrogate Measure for Survival Outcomes after Resection of Hepatocellular Carcinoma. J Gastrointest Surg. 2020;24:50-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |