Published online Oct 15, 2021. doi: 10.4251/wjgo.v13.i10.1302
Peer-review started: February 21, 2021
First decision: May 8, 2021
Revised: July 17, 2021
Accepted: August 24, 2021
Article in press: August 24, 2021
Published online: October 15, 2021
Processing time: 233 Days and 18.4 Hours
Modern liver ultrasonography (US) has become a “one-stop shop” able to provide not only anatomic and morphologic but also functional information about vascularity, stiffness and other various liver tissue properties. Modern US techniques allow a quantitative assessment of various liver diseases. US scanning is no more limited to the visualized plane, but three-dimensional, volumetric acquisition and consequent post-processing are also possible. Further, US scan can be consistently merged and visualized in real time with Computed Tomography and Magnetic Resonance Imaging examinations. Effective and safe microbubble-based contrast agents allow a real time, dynamic study of contrast kinetic for the detection and characterization of focal liver lesions. Ultrasound can be used to guide loco-regional treatment of liver malignancies and to assess tumoral response either to interventional procedures or medical therapies. Microbubbles may also carry and deliver drugs under ultrasound exposure. US plays a crucial role in diagnosing, treating and monitoring focal and diffuse liver disease. On the basis of personal experience and literature data, this paper is aimed to review the main topics involving recent advances in the field of liver ultrasound.
Core Tip: Modern liver ultrasound has become fully multiparametric able to provide not only anatomic and morphologic but also vascularity, stiffness and dynamic assessment of contrast agent kinetic. Over the years, ultrasound has seen a dramatic increase of its clinical applications in diagnosing, treating and monitoring focal and diffuse liver disease. In this review we will focus on the main topics involving recent advances and modern applications in the field of liver ultrasound.
- Citation: Bartolotta TV, Taibbi A, Randazzo A, Gagliardo C. New frontiers in liver ultrasound: From mono to multi parametricity. World J Gastrointest Oncol 2021; 13(10): 1302-1316
- URL: https://www.wjgnet.com/1948-5204/full/v13/i10/1302.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v13.i10.1302
In 1942 the neurologist Karl Dussik produced a brain “ventriculogram”, paving the way for the use of ultrasound (US) for medical purposes[1]. Since then, the field of medical US has experienced tremendous technical improvement.
In particular liver US has progressively achieved an unprecedented B-mode image quality, being even capable of processing and displaying “harmonic frequencies” which were previously considered “noise” and simply cut off[2]. US is no more a merely bi-dimensional technique but it is also possible to acquire and display in real time entire liver volumes, which can be in turn post-processed for volume calculation or rendering[3].
First (Color) and second (Power) generation Doppler modules have tremendously increased their sensitivity in blood flow detection, yet US is rapidly moving towards third-generation Doppler techniques[4]. Furthermore, the availability of safe and effective contrast agents allows for a real time assessment of the kinetic of contrast enhancement, also providing quantitative parameters about vascularity on a micrometric scale[5].
Analysis of ultrasonic waves propagation allows for objective analysis of tissue properties such as stiffness and fat content, thus providing a useful tool for a non-invasive assessment of various diffuse liver disease[6].
US equipment can consistently fuse and synchronize in a real time and dynamic fashion the US scan of a patient with corresponding computed tomography (CT) or magnetic resonance imaging (MRI) examinations[7].
Also, US can be used to locally deliver drugs or genetic material[8].
On the basis of personal experience and literature data, the main topics involving recent advances in the field of liver US will be presented and discussed.
Introduced in 1997, tissue harmonic imaging (THI) is a nonlinear US image-processing technology aimed at improving conventional gray-scale US image quality.
In B-mode US, the transmitted ultrasounds pulses travel through the tissues in a linear fashion and the frequency of the returning echoes is the same of the transmitted pulses, also known as fundamental frequency. However, when high-pressure ultrasounds waves (> 0.5 MPa) travel through tissues, the transmitted ultrasounds pulse will interact with tissues in a non-linear fashion and from this interaction new frequencies will be generated, which are integer multiples of the fundamental frequency: Harmonic frequencies.
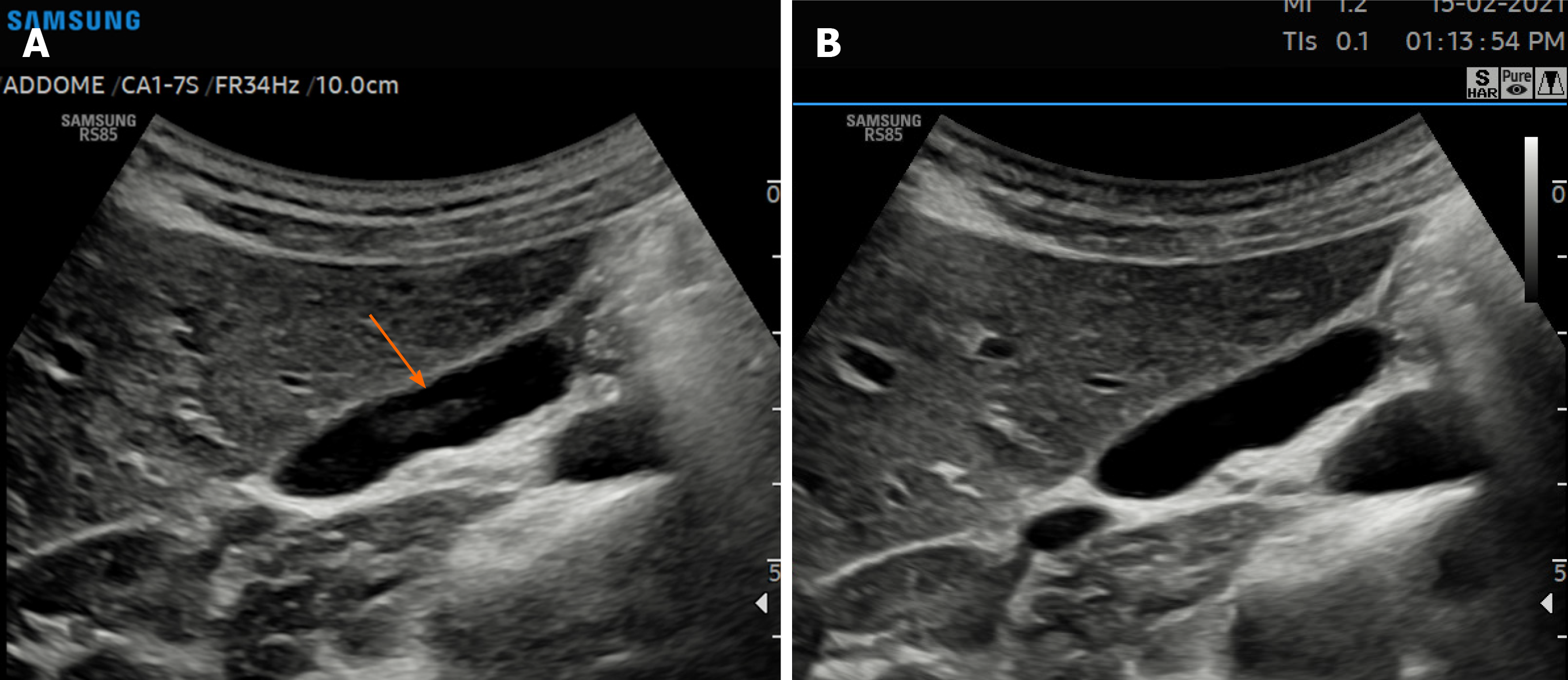
Clinical US systems usually employ second harmonic echoes in order to generate THI images. Among the advantages of THI, a better signal-to-noise ratio and less artifacts deriving from side and grating lobes as well as reverberation are included (Figure 1)[2].
Angiogenesis, the process of formation of new blood vessels, plays an important role in cirrhosis and liver cancer development, invasion, and metastasis[9]. In this regard, first- and second- generation Doppler techniques, namely color Doppler (CD) and power Doppler (PD), have been extensively used to detect the presence of vascularity associated with malignancy in liver masses[10,11]. However, CD and PD adopt wall filters to minimize clutter artifacts. As a consequence, they can detect tumoral vascularization only in larger vessels or when blood flows relatively fast.
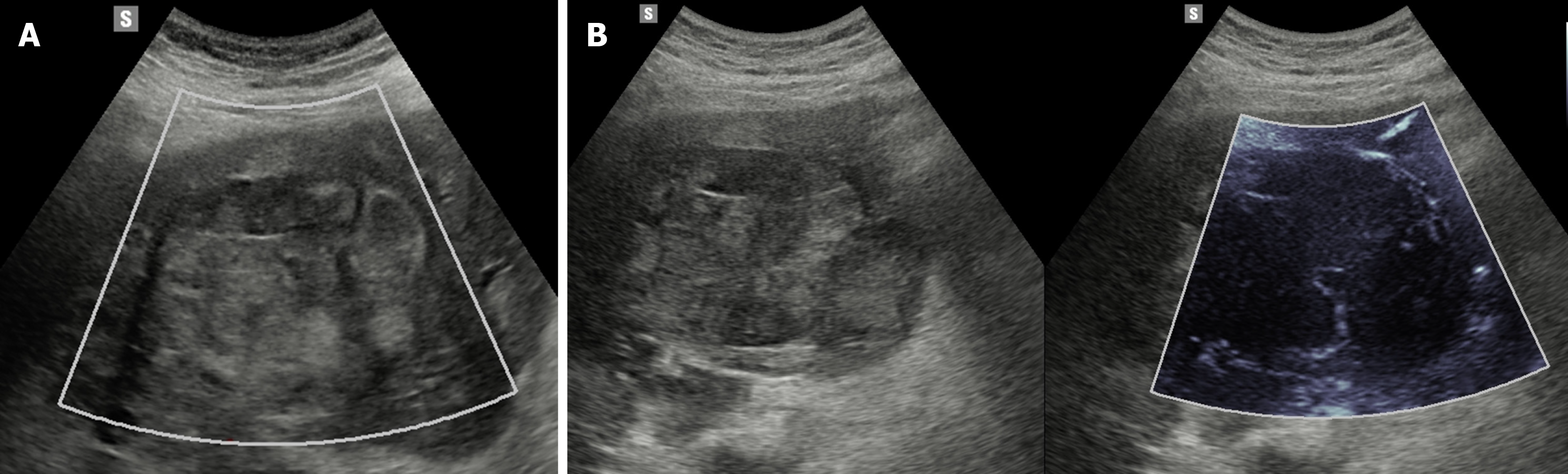
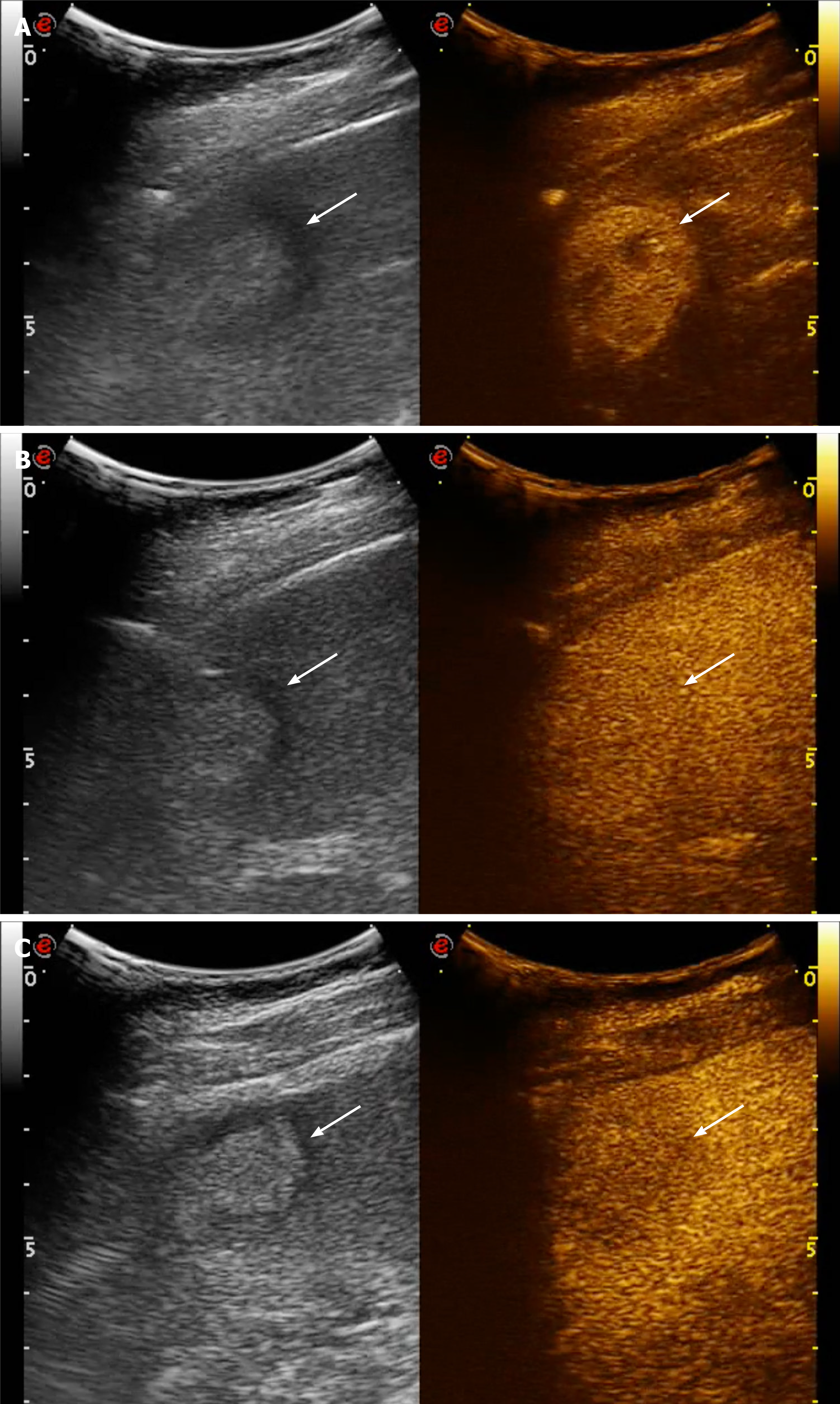
More recently, newer Doppler-based techniques have been introduced which can separate slow or small-vessel flow signals from clutter artifacts, including superb microvascular imaging (SMI), microflow imaging (MFI), and microvascular flow imaging (MVFI, MV-FlowTM)[4].
These new, third-generation Doppler-based techniques enable the depiction of slow flowing blood at very high spatial resolution and frame rate by using advanced clutter suppression, thus improving the sensitivity of Doppler US in the assessment of vascularity in hepatic tumors with a safe, inexpensive and readily available modality (Figure 2)[4].
In a study encompassing 70 focal liver lesions, mainly composed of hepatocellular carcinoma (HCC; n = 43) and aiming to examine the number of vessels present within or at the periphery of each lesion, SMI was able to detect more vessels than Color or Power Doppler (P < 0.001) [11]. Another study focusing on detecting the vascularity of 51 HCC, confirmed the higher sensitivity of MFI (58%) than Color (14%) or power (14%) Doppler (P < 0.001)[12].
MVFI also has been proved to be superior to Color or power Doppler (P < 0.05) for the detection of intratumoral vascularity in 100 HCCs treated by means of transarterial chemoembolization, with excellent intra-observer and good inter-observer agreements[13].
Although a pivotal study evaluating a small series of 29 focal liver lesions (FLLs) has suggested the possibility of differentiating benign from malignant liver masses by detecting different intratumoral vascular patterns at SMI evaluation, to this purpose more powerful and flow-sensitive techniques are available in clinical practice: In particular contrast-enhanced ultrasound[14].
By the late 1990s, the availability of intravenously injected microbubble-based contrast agents and the development of contrast-specific US techniques, has enabled US to depict not only macro-vascularity but also micro-vessels as thin as 40 μm[15].
At the beginning of the 2000s, the development of microbubbles with flexible shells (e.g., phospholipids) and filled with low-solubility gases such as perfluoropropane, perfluorocarbon, or sulfur hexafluoride, has led to a full real time contrast enhanced US (CEUS) examination[16]. CEUS allows to assess liver perfusion non-invasively and in real time, without the need of ionizing radiation, potentially nephrotoxic contrast agents or costly and not widespread equipment, such as CT or MRI. Of note, microbubble-based contrast agents present a radius ranging from 1 to 10 μm, so they can pass through the pulmonary filter but they do not exit the vascular space, acting as purely vascular tracers (blood-pool agents), although one of them exhibits an additional Kupffer phase[17]. CEUS is safe and well tolerated: It can be performed in patients with hepatic or renal failure. Renal obstruction or chronic obstructive pulmonary disease are not a contraindication and laboratory tests of renal function are no necessary in advance. In a study encompassing 23188 patients, the overall reporting rate of serious adverse event was 0.0086%. In the same study no deaths have been reported and the life-threatening anaphylactoid reaction rate was less than 0.002%[18].
Nowadays, CEUS is suggested as useful tool for diagnostic work-up of FLLs, including incidental masses detected in non-oncologic non-cirrhotic patients, suspect metastases in oncologic patients and HCC in cirrhotic patients, aiming at optimizing patient management and at cost-effective therapy delivering[5,19].
A recent meta-analysis focusing on the role of CEUS in the characterization of FLLs showed pooled sensitivity, specificity, diagnostic odds ratio, positive and negative likelihood ratio and area under the curve of 92%, 87%, 104.20, 7.38, 0.09, and 0.9665, respectively[20].
In the clinical setting of a non-oncologic non cirrhotic patient, the pre-test probability of a lesion being benign is high, hence a good specificity is mandatory in order to avoid unnecessary, invasive and unethical treatment.
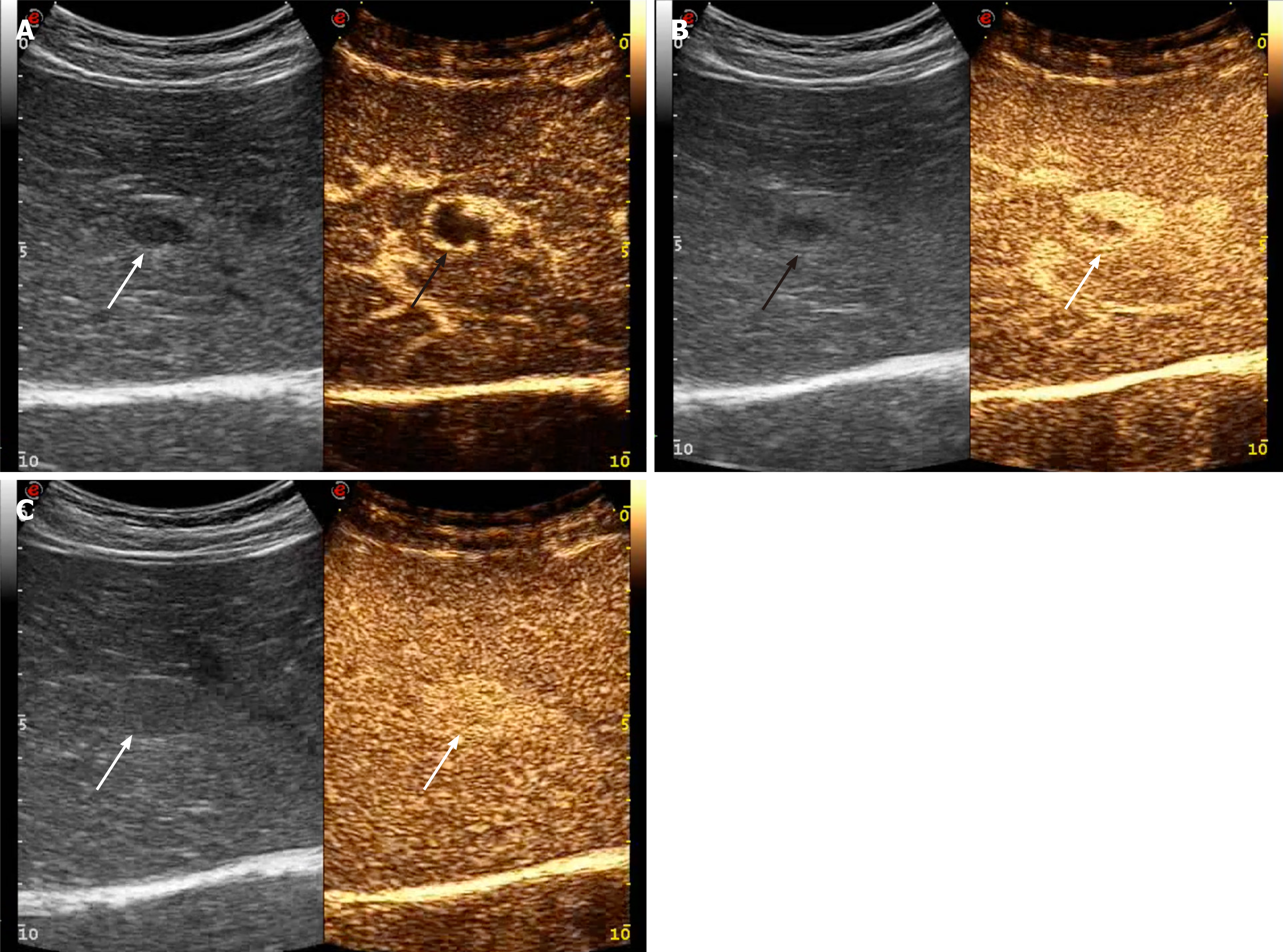
At CEUS, the main feature indicating a benign lesion is a sustained and prolonged contrast-enhancement in the portal-venous (i.e., 30-45 to 120 s after contrast injection) and late phases (i.e., 120 s up to 4-6 min after contrast injection) (Figure 3)[21,22]. The main caveat to this observation is that well differentiated HCC may show prolonged and sustained contrast-enhancement too, although the clinical setting is usually different[23].
However, considering the appropriate clinical setting, further clues to the diagnosis may be obtained by looking at the arterial phase (i.e., 10-45 s after contrast injection)[5]. A peripheral globular contrast-enhancement pattern followed by a centripetal fill-in, either complete or incomplete, is typical of hemangioma (Figure 3)[21]. A centrifugal contrast-enhancement pattern with a spoke-wheel appearance and a central avascular area is typical of Focal nodular hyperplasia[24]. Finally, a peripheral contrast-enhancement without globular appearance followed by a rapid centripetal fill-in may suggest the diagnosis of hepatocellular adenoma (HA)[5]. Nevertheless, as a caveat, HA may appear as hypoechoic lesion in the portal and late phases[25].
In a study of 174 indeterminate FLLs incidentally detected at US, CEUS allowed a correct differentiation of benign from malignant masses in 168 out of 174 (96.5%) cases (P < 0.0001), thus reducing the need for further radiological work-up[21].
In oncologic patients the task of the radiologic work-up of the liver is twofold, aiming first to detect a FLL and second to characterize it: Hence sensitivity also plays a crucial role. US may present equivocal results in liver metastasis detection, with sensitivity values ranging from 40% to 80%, according to the lesion size and the skill and experience of the sonologist[26].
At CEUS, the typical contrast-enhancement pattern of liver metastases is a marked and early wash-out, usually occurring earlier than 60 s after the contrast injection (Figure 4). Wash-out is defined as hypoechoic appearance in comparison to adjacent liver parenchyma in the portal-venous or late phases, irrespective of the appearance in the arterial phase[26].
For the detection of liver metastases, CEUS has been proved to improve sensitivity compared to unenhanced US and to provide a diagnostic performance comparable to that of CT and MRI[27,28].
In particular, in the detection of FLLs CEUS showed sensitivity and specificity values of 77.5%-100% and 76.7%-97.6%, respectively, when compared to CT[17].
CEUS can be very valuable when fatty infiltration of the liver and focal fatty sparing occur in a geographic pattern, in atypical location or shape, thus further worsening US performance both in the detection and the characterization of focal liver lesions[5].
In cirrhotic patients, CEUS allows to detect in real time the typical contrast-enhancement behavior of HCC, without using ionizing radiation and at a higher temporal resolution than CT and MRI[5].
At CEUS, the typical contrast-enhancement pattern of HCC in comparison with liver parenchyma is arterial hyperenhancement followed by late (later than 60 s after contrast injection) and mild washout (Figure 5)[29]. On the other hand, the presence of a marked and early (earlier than 60 s) washout is more typical of non-HCC malignancies, such as intrahepatic cholangiocarcinoma or metastases[30].
Several international guidelines currently recommend CEUS as a useful imaging modality for the radiological work-up of HCC, such as the LI-RADS lexicon of the American College of Radiology[22,30,31].
Compared with CT or MRI, CEUS is real-time dynamic enhancement, every second imaging can be read and tracted, so it’s able to avoid or markedly reduce imaging information losing. But it is not suitable for simultaneous evaluation of several liver focal lesions, and not suitable for large liver focal lesion of diameter > 10 cm.
A systematic comparison of the accuracy of CEUS, CT and MRI in the characterization of FLLs, reported sensitivities values of 88% (95%CI 87% to 90%), 90% (95%CI 88% to 92%) and 86% (95%CI 83% to 88%), respectively, with specificities values of 81% (95%CI 79% to 84%), 77% (95%CI 71% to 82%) and 81% (95%CI 76% to 85%)[32]. CEUS is not deemed to completely replace CT or MRI but, depending on the clinical setting, CEUS could reduce the use of CT and MRI[28].
CEUS may play a role in the guidance, response assessment and detection of complications of interventional procedures[33].
A multi-center study by Lu et al[34], aimed at comparing CEUS with CT or MRI in detecting tumor vascularity after thermal ablation procedure in 151 HCC patients, found out specificity and accuracy values for CEUS of 98.2% and 96.6%, respectively.
CEUS may be performed during or after the interventional procedure[29]. In particular, the use of CEUS during the procedure has been reported to have a significant clinical impact, reducing the need for re-treatments and increasing the cost-effectiveness of the therapy[35].
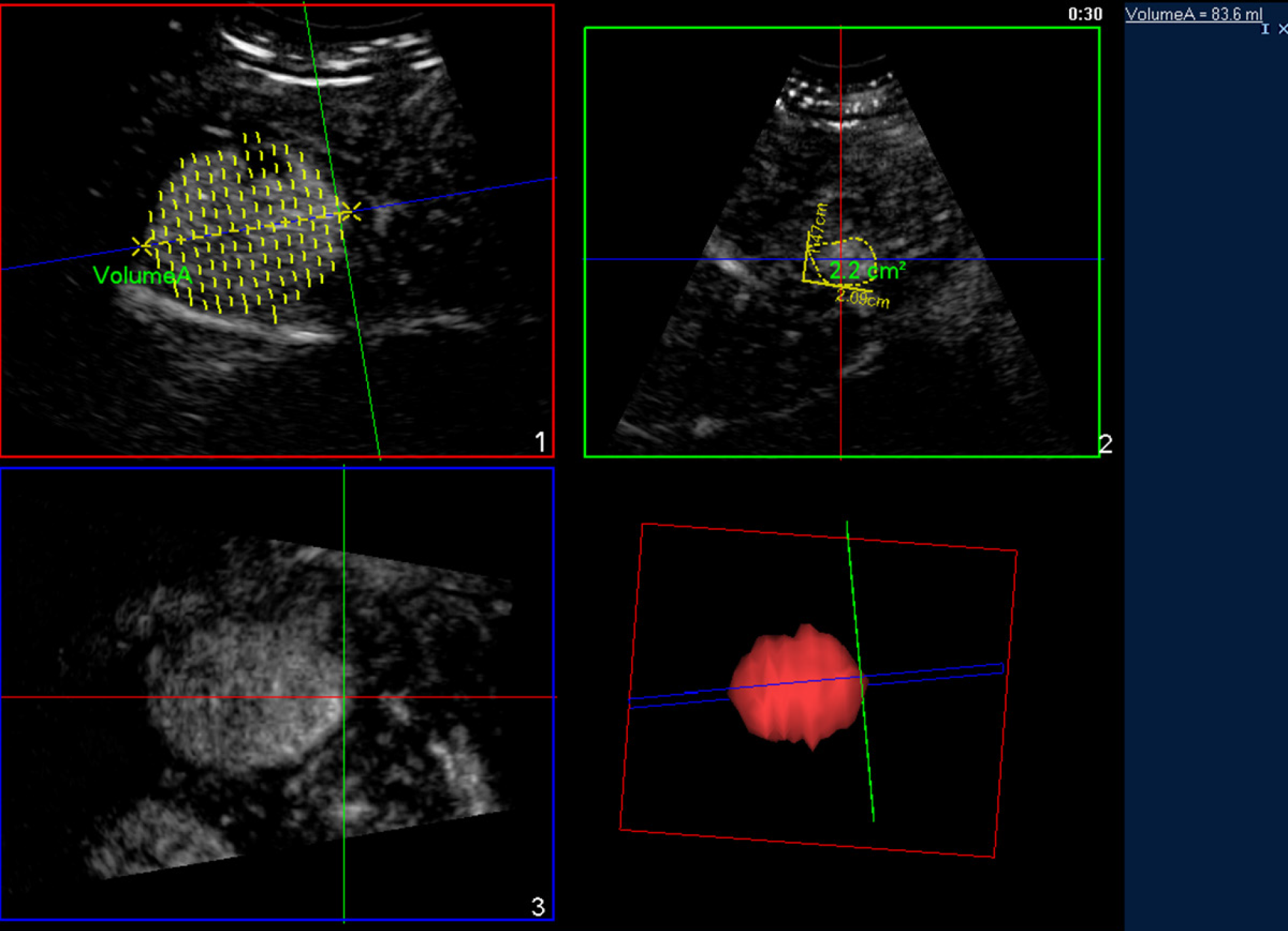
More recent US advances allow a three-dimensional assessment of tumor volume and shape, promising further refinement of CEUS role in planning, treatment and tumor response assessment of HCC treated by means of loco-regional therapies (Figure 6)[3].
An emerging field of clinical utility for dynamic CEUS (D-CEUS) is the monitoring of tumoral response to antiangiogenic drugs. By detecting flow in vessels as tiny as 40 μm, with D-CEUS it is possible to assess in real time tumor contrast kinetycs, to compose time-intensity curves and extract quantitative parameters related to: (1) Blood Volume, such as peak contrast enhancement intensity, Area Under the Curve (AUC), AUC during contrast wash-in, AUC during contrast wash-out; (2) Blood Flow, such as time to peak contrast intensity, slope of the contrast wash-in; and (3) Mean Transit Time. Literature data show encouraging results in the use of D-CEUS to separate the responders from non-responders earlier than CT or MRI by means of AUC or MTT in oncologic patients[36].
In the last decade, new ultrasound-based techniques have been developed which enable a real-time, non-invasive evaluation of liver tissue properties other than echogenicity, such as mechanical characteristics: Elasticity or its counterpart, stiffness.
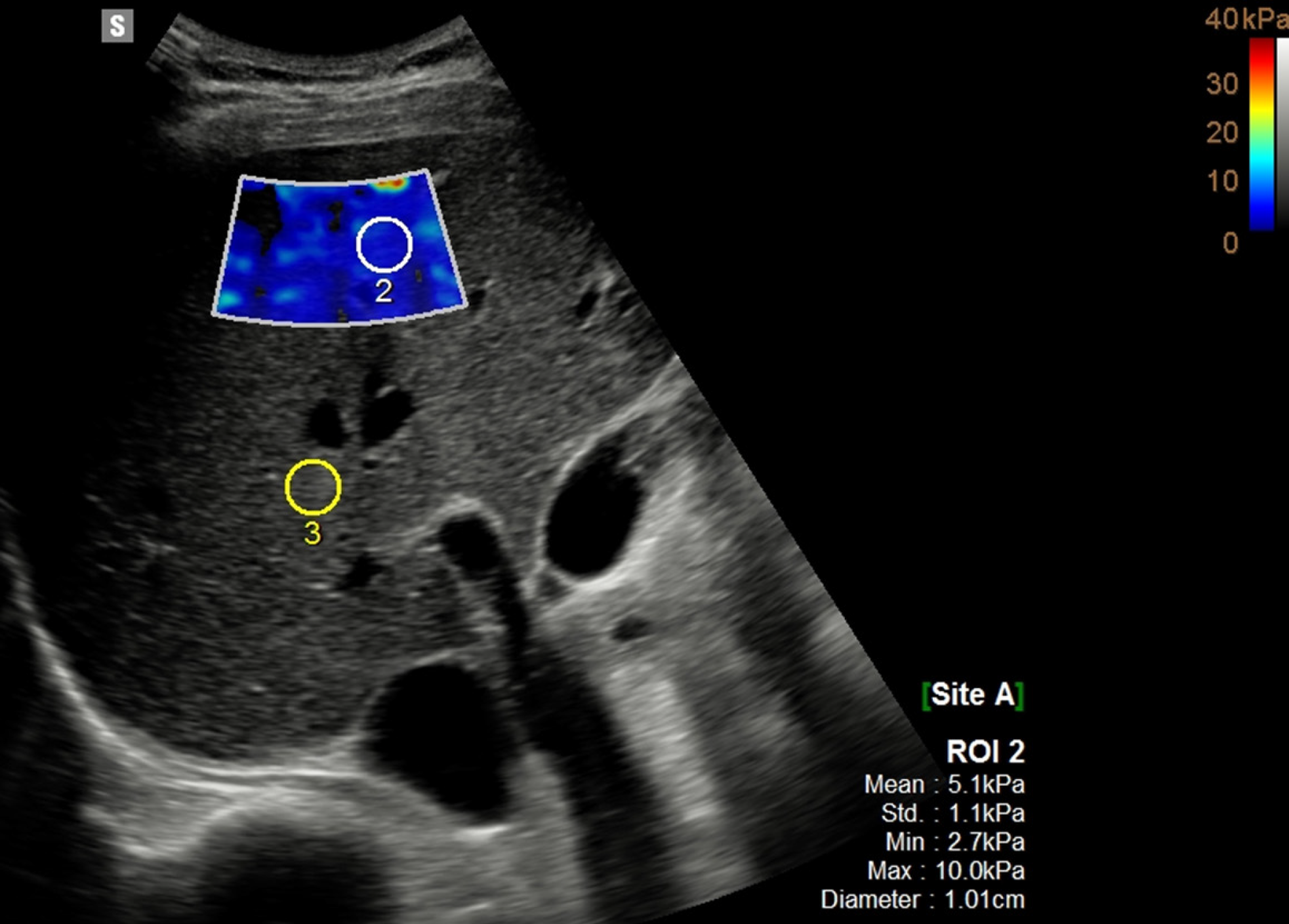
Ultrasound elastography enables quantitative assessment of liver stiffness by applying an external force by means either of a mechanically-induced impulse, as in transient elastography (TE), or ultrasound-induced focused radiation impulse, as in acoustic radiation force impulse (ARFI) and measuring the velocity of propagated ultrasound waves axially (TE) or perpendicularly (ARFI quantification) to the ultrasound beam pathway[37,38]. Since the velocity is directly proportional to the tissue stiffness, the Young modulus (measured in kilopascal, kPa) or wave speed (m/s) can be calculated and usually displayed[39].
TE is widespread and well validated, but limited in terms of size and guidance of liver-sampling area, whereas the more recent ARFI-based techniques, such as shear wave elastography (SWE) allow a better US guidance of the liver-sampling either for small (point SWE: pSWE) or larger (two dimensional SWE: 2D SWE) areas of liver parenchyma[39] (Figure 7). New developments of US Elastography also include a volumetric assessment of liver stiffness (3D SWE) as well as its variations in real time (4D SWE)[40].
Stiffness is strongly related to fibrotic changes which characterize various chronic liver diseases, which ultimately may end in cirrhosis, such as viral infections, alcohol abuse, nonalcoholic fatty liver disease (NAFLD) and biliary disease among others. Hence, accurate staging of liver fibrosis is crucial for patient management, in terms of prognosis, surveillance and treatment[6].
Despite of being operator dependent, prone to technical artifacts and confounding factors which may affect liver stiffness measurements, ultrasound Elastography provides a widespread, noninvasive, low cost, and repeatable method to assess liver fibrosis and several guidelines recommend its use in diagnostic work-up of chronic liver disease[37]. A recent meta-analysis showed that ARFI elastography is accurate and reliable in the diagnosis of liver fibrosis in chronic hepatitis B and C patients and is especially suitable for the evaluation of advanced stages (F ≥ 3 and F = 4)[41].
Another issue related to the clinical use of ultrasound Elastography is the inconsistency of the cut-off values suggested by various manufacturers for the staging of liver fibrosis.
Recently, to overcome this issue, a consensus panel has proposed a manufacturer-neutral “rule of four” with values of 5, 9, 13, 17 kPa for ARFI assessment of liver fibrosis of viral etiologies and NAFLD. Liver stiffness < 5 kPa (1.3 m/s) has high probability of being normal; liver stiffness < 9 kPa (1.7 m/s), without other known clinical signs, rules out compensated advanced chronic liver disease (cACLD); values between 9 kPa (1.7 m/s) and 13 kPa (2.1 m/s) are suggestive of cACLD (further test may be needed for confirmation); and values > 13 kPa (2.1 m/s) are highly suggestive of cACLD[42].
Clinically significant portal hypertension may be present with liver stiffness values > than 17 kPa (2.4 m/s)[42]. More in general, liver stiffness values < 7 kPa (1.5 m/s) (pSWE and 2D SWE) indicate the absence of significant fibrosis[42].
In a recent study, 2D SWE, MRE and TE showed comparable and very good to excellent diagnostic accuracy for advanced fibrosis and comparable but lower accuracy for significant fibrosis in patients with biopsy-proven NAFLD[43].
Steatosis is characterized by an abnormal accumulation of lipids (mainly triglycerides) within the hepatocytes, leading to an overall hepatic-fat content greater than 5% of liver weight or, more practically, when more than 5% of hepatocytes contains fatty droplets[6]. The two most frequent causes of liver steatosis are alcoholic fatty liver disease and NAFLD. This latter may evolve into nonalcoholic steatohepatitis in those 15%-20% of cases with inflammation and fibrosis[6].
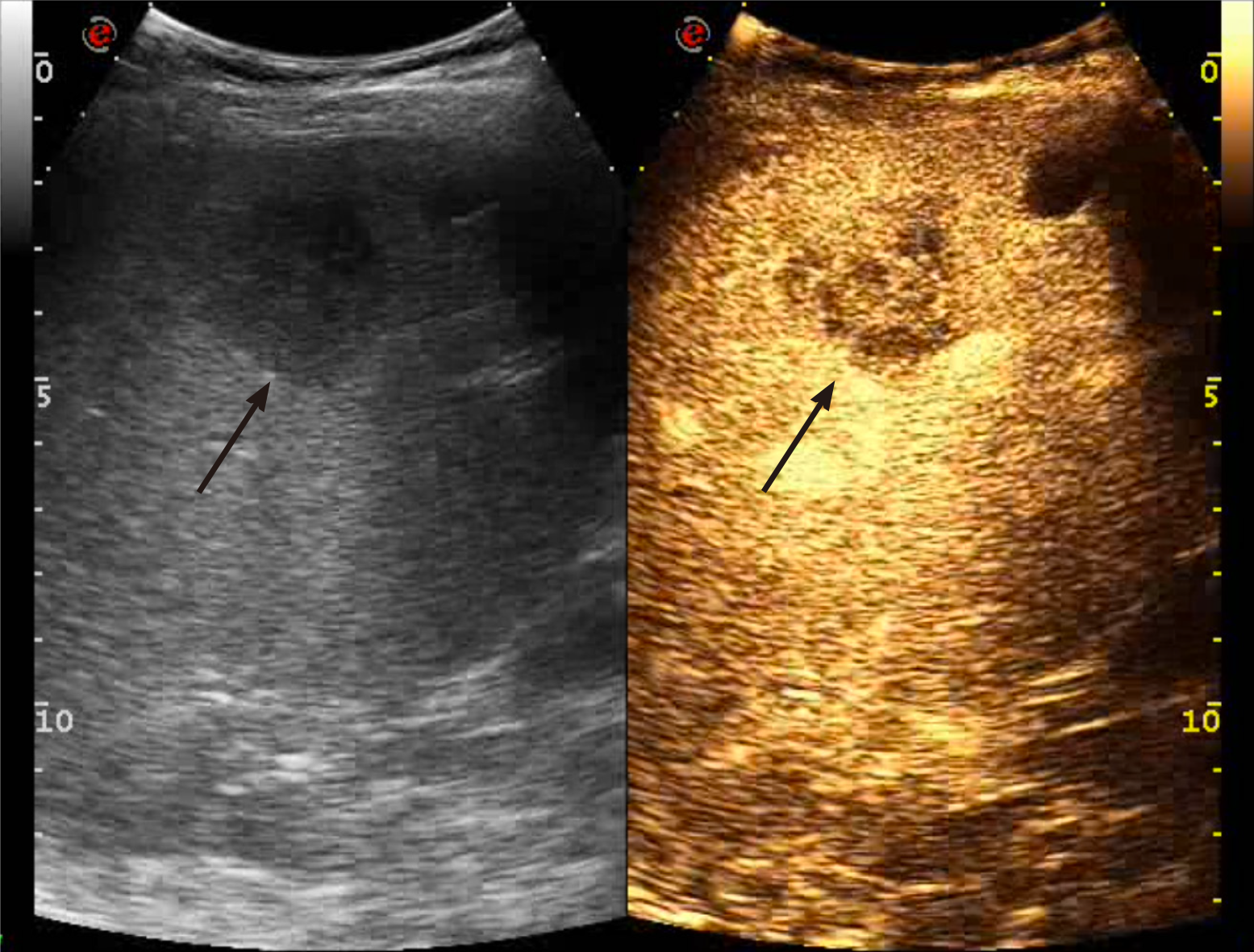
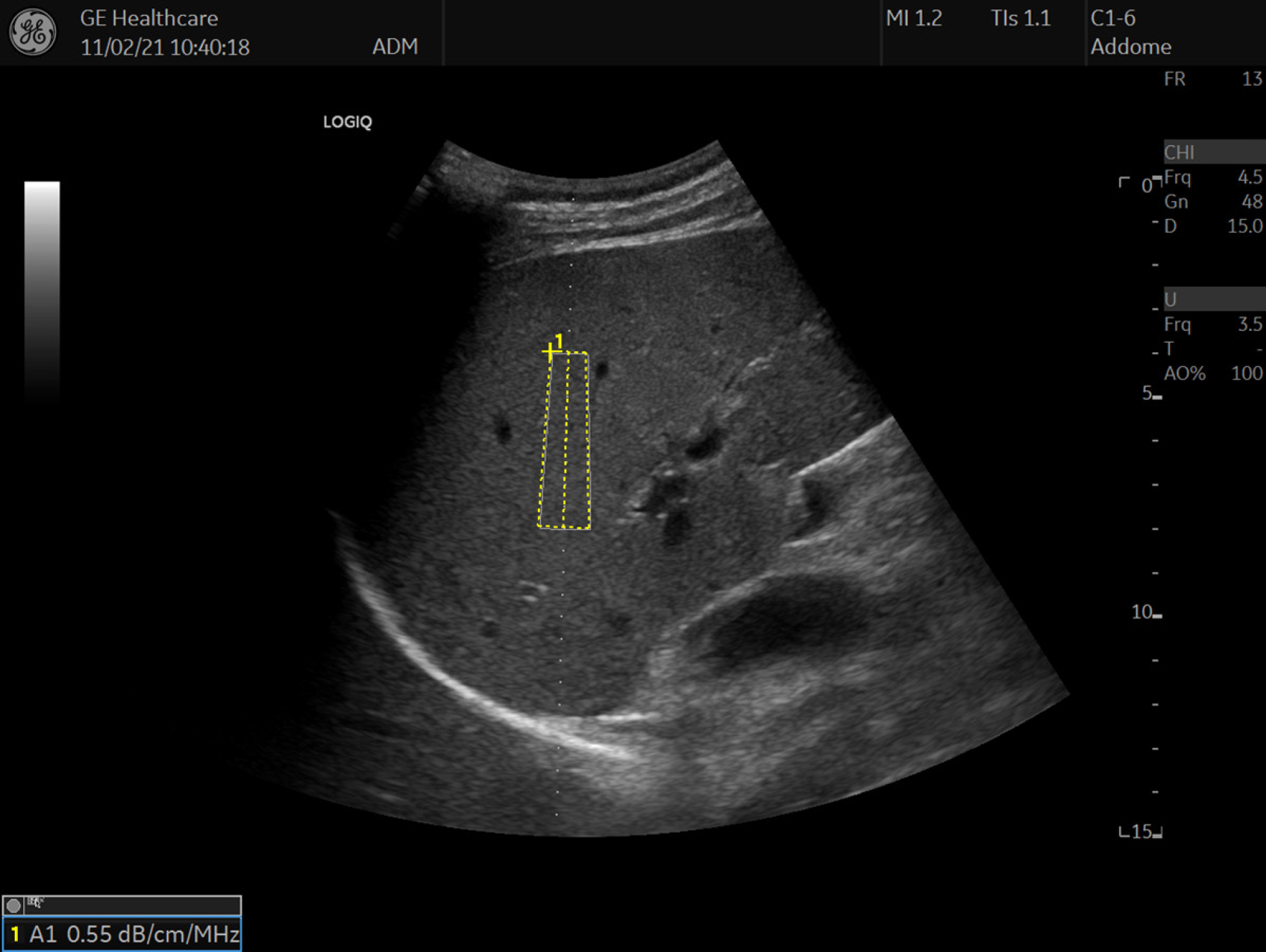
Recently, the controlled attenuation parameter (CAP) has been suggested as a new method for the assessment of liver steatosis. CAP measurements rely on the degree of US beam attenuation through the hepatic parenchyma and the energy attenuation is expressed in decibel/meter (dB/m). In clinical practice, CAP is measured simultaneously to liver stiffness with the transient elastography device (FibroScan, Echosens, France)[44,45]. A recent meta-analysis reported a sensitivity of 68.8%-88.2% and a specificity of 77.6%-82.2% for CAP in monitoring the grade of steatosis in chronic liver disease[46]. One limitation of CAP is the lack of a B-mode guidance for choosing the sampling area. To overcome such a limitation, software for quantifying the attenuation of the ultrsound beam is under development or already available from different vendors. The attenuation coefficient (AC) is expressed in decibel per centimeter per megahertz (dB/cm/MHz) (Figure 8)[47].
In a prospective study encompassing 108 patients the AC values derived from ATI have been shown to present good diagnostic performance in distinguishing the different degrees of hepatic steatosis. Of note, AC values were affected only by the actual degree of steatosis whereas fibrosis and inflammation were not influencing factors[48].
Another recent study conducted on 101 patients found out that an AC of > 0.69 dB/cm/MHz showed sensitivity and specificity values of 76%and 86%, respectively, for diagnosing steatosis (S1–S3), and AC > 0.72 dB/cm/MHz had sensitivity and specificity values of 96% and 74%, respectively, for diagnosing steatosis of grade S2–S3. The concomitant presence of advanced fibrosis (F3–F4) did not influenced the AC values[49]. Hence, the AC is a promising quantitative technique for the noninvasive diagnosis and quantification of liver steatosis. Of note, Magnetic resonance (MRI-PDFF) is another valuable tool to quantify liver steatosis. In a study, MRI-PDFF detected any grade of steatosis with an AUROC of 0.99 (95%CI, 0.98-1.00): A value significantly better than that of CAP (AUROC, 0.85; 95%CI, 0.75-0.96)[44].
Three-dimensional ultrasound (3D-US) has been found useful in obstetrics, gynecology and cardiology[50]. More recently, 3D-US has also gained interest for liver assessment[50]. Of note, 3D-US techniques cast "rays" through the 3D voxel-based volume: The resulting image is projected onto a two-dimensional plane. When the contrast between the examined structure and the adjacent tissues is not wide enough, such as it occurs in liver parenchyma, the results are suboptimal[50]. The administration of microbubble-based contrast agents may overcome this limitation, allowing 3D-CEUS to indicate the way for new applications in hepatic US.
In a study on 83 FLLs, when compared to 2D US, 3D CEUS revealed more details of the boundary and feeding vessels of the mass, as well as distorted features of supply vessels of HCC[51]. 3D-CEUS may also provide volume calculations with almost perfect intrareader agreement which can be used in preoperative planning for loco-regional treatment of focal liver tumors and for effective tumor response assessment after treatment (Figure 6)[3].
New technologic improvements, such as electronic matrix probes, allows real-time 3D volumetric evaluation of FLLs during the entire vascular phase, also providing effective flow quantification[52].
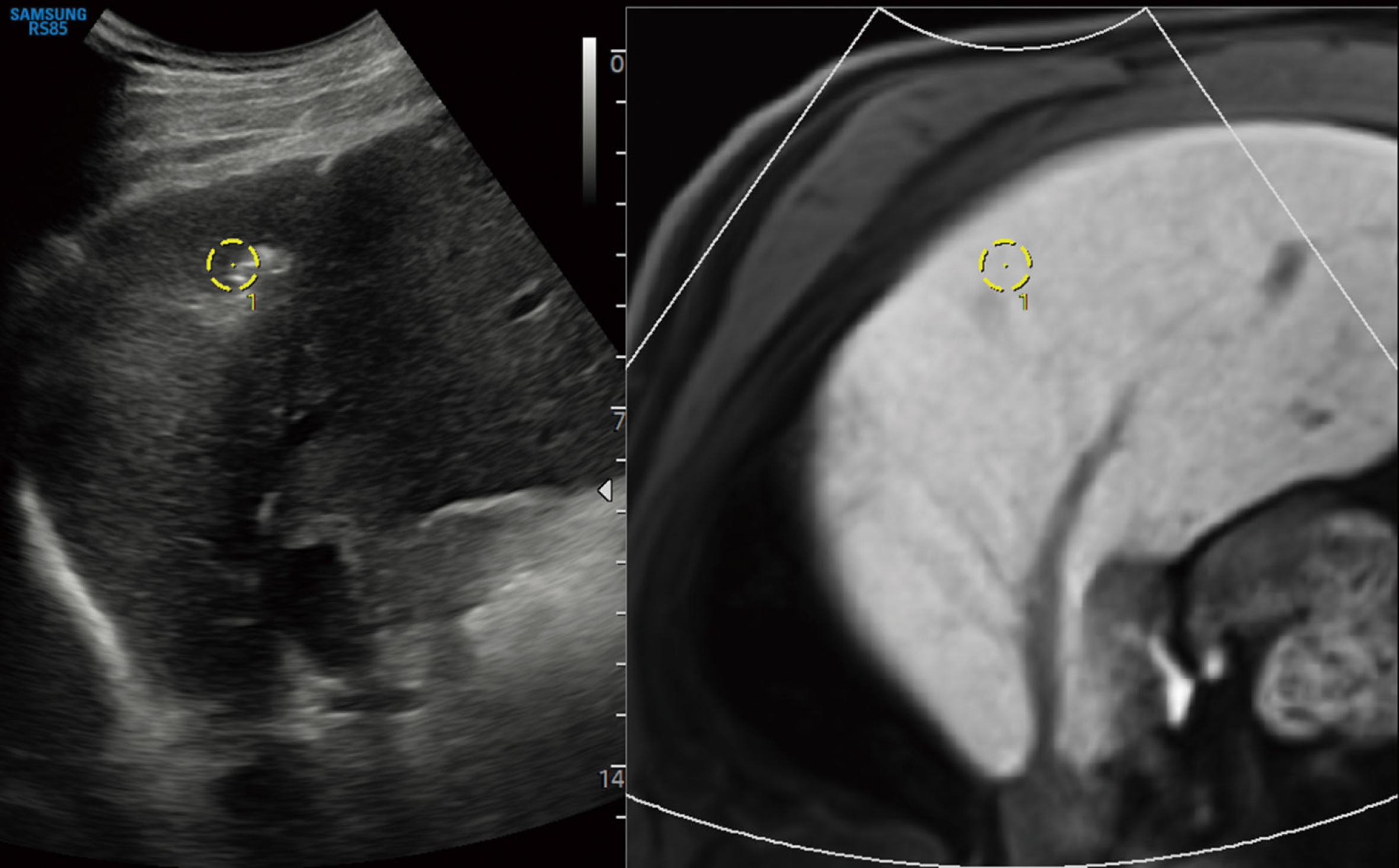
Fusion imaging software provided by different vendors can be embedded in the ultrasound unit in order to synchronize previously acquired CT, MR or PET/CT liver studies with real time US scanning (Figure 9)[53]. Clinical applications of fusion imaging in the liver are mainly related to interventional procedures, including pre-, intra- and post-procedural phases of loco-regional treatment of liver malignancies[53].
Fusion imaging has proved useful for performing effective percutaneous biopsy of FLLs poorly visible at US[54]. The additional use of CEUS may further improve lesion conspicuity allowing a better rate of accurate percutaneous biopsy for FLLs invisible even on fusion imaging[55].
In a study by Song KD et co-workers, 64 of 120 (53.3%) HCCs not visible on conventional ultrasound could be ablated under the guidance of the fusion imaging technique[56]. This is of particular importance for HCC smaller than 2 cm[57]. In order to improve the efficacy of treatment, CEUS can be used if the target HCC lesions have poor conspicuity even on fusion imaging[58].
Fusion imaging has also been suggested as a method to assess tumor response both intra-procedurally and during postoperative follow-up[59]. In a study of 126 HCCs, intraprocedural use of CEUS-CT/MR image fusion was able to accurately evaluate ablative margin and to improve complete ablation rate in 12/55 (21.8%) lesions, which were immediately treated in the same session[60]. The study by Xu et al[61] also confirms that 3D US-CEUS fusion imaging is an useful technique for the intraprocedural evaluation and guidance of supplementary ablation in 76 patients with HCC, liver metastases and cholangiocarcinoma.
In their series, 30 out of 95 tumors have been re-ablated immediately during the same procedure[61].
Ultrasound may play a promising role as tool for delivering therapeutic agents, such as genetic material, proteins, and chemotherapeutic drugs[62].
Currently, microbubbles are studied not only as ultrasound contrast agents but also as tool for delivering drugs locally under ultrasound exposure[63]. More elaborated drug delivery carriers are studied for both simultaneous imaging and focal therapy in the setting of different cancer types, including hepatic malignancies[64].
Radiomics is defined as the process of extraction, analysis, and modeling of a large quantity of features from medical imaging dataset and to correlate this information to prediction parameters, such as clinical end-points, pathological and genomic features[65]. Radiomics is a complex process that can be divided into different phases, including: Acquisition of imaging dataset, tumor segmentation, feature extraction, exploratory analysis, and model building[66].
Radiomics can be applied in liver imaging, including US images. A study by Peng et al[67] has found out that US radiomics models can be useful in distinguishing different histopathological types of primary liver cancer, each of one needing specific treatment. A study by Mao et al[68] showed that US radiomics features allowed to non-invasively distinguish primary from metastatic liver tumors. In another study encompassing 482 HCC patients an US-based radiomics score was found to be an independent predictor of microvascular invasion in HCC[69].
Artificial intelligence, such as deep learning algorithms, is gaining extensive attention in medical imaging and studies applying deep learning to US are being actively conducted, mainly in the field of diffuse liver disease, especially hepatic fibrosis and steatosis evaluation[70,71]. In a recent study of 3446 patients a deep convolutional neural network showed high accuracy in the assessment of METAVIR score using US images and achieved better performance than that of radiologists in the diagnosis of cirrhosis[72].
Modern liver US is no more a simple mono-parametric “B-Mode” technique. US has become fully multiparametric: A “one-stop shop” able to provide not only anatomic and morphologic but also functional information about vascularity, stiffness and other various liver tissue properties, including dynamic assessment of contrast agent kinetic. US plays a crucial role in diagnosing, treating and monitoring focal and diffuse liver disease. Ultrasound beam may be focused to directly ablate tumoral tissue or adequately modulated to deliver drugs and genetic materials locally.
Mastering this complex and multiparametric technique is a cultural challenge. Nevertheless, this challenge needs to be fully taken up in order to provide our patients the best care option in various liver diseases.
Manuscript source: Invited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Karavaş E, Li M, Wu SZ, Wu M S-Editor: Ma YJ L-Editor: A P-Editor: Li JH
| 1. | Kaproth-Joslin KA, Nicola R, Dogra VS. The History of US: From Bats and Boats to the Bedside and Beyond: RSNA Centennial Article. Radiographics. 2015;35:960-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Anvari A, Forsberg F, Samir AE. A Primer on the Physical Principles of Tissue Harmonic Imaging. Radiographics. 2015;35:1955-1964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 3. | Bartolotta TV, Sidoti Pinto A, Cannella R, Porrello G, Taravella R, Randazzo A, Taibbi A. Focal liver lesions: interobserver and intraobserver agreement of three-dimensional contrast-enhanced ultrasound-assisted volume measurements. Ultrasonography. 2021;40:333-341. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | He MN, Lv K, Jiang YX, Jiang TA. Application of superb microvascular imaging in focal liver lesions. World J Gastroenterol. 2017;23:7765-7775. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 36] [Cited by in RCA: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 5. | Bartolotta TV, Vernuccio F, Taibbi A, Lagalla R. Contrast-Enhanced Ultrasound in Focal Liver Lesions: Where Do We Stand? Semin Ultrasound CT MR. 2016;37:573-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Taibbi A, Picone D, Midiri M, La Grutta L, Bartolotta TV. Diffuse Liver Diseases: Role of imaging. Semin Ultrasound CT MR. 2018;39:193-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Schwarze V, Rübenthaler J, Marschner C, Fabritius MP, Rueckel J, Fink N, Puhr-Westerheide D, Gresser E, Froelich MF, Schnitzer ML, Große Hokamp N, Afat S, Staehler M, Geyer T, Clevert DA. Advanced Fusion Imaging and Contrast-Enhanced Imaging (CT/MRI-CEUS) in Oncology. Cancers (Basel). 2020;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 8. | Wang LY, Zheng SS. Advances in low-frequency ultrasound combined with microbubbles in targeted tumor therapy. J Zhejiang Univ Sci B. 2019;20:291-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 9. | Fernández M, Semela D, Bruix J, Colle I, Pinzani M, Bosch J. Angiogenesis in liver disease. J Hepatol. 2009;50:604-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 417] [Cited by in RCA: 445] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 10. | Choi BI, Kim TK, Han JK, Chung JW, Park JH, Han MC. Power vs conventional color Doppler sonography: comparison in the depiction of vasculature in liver tumors. Radiology. 1996;200:55-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 106] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 11. | Dubinsky TJ, Revels J, Wang S, Toia G, Sonneborn R, Hippe DS, Erpelding T. Comparison of Superb Microvascular Imaging With Color Flow and Power Doppler Imaging of Small Hepatocellular Carcinomas. J Ultrasound Med. 2018;37:2915-2924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 12. | Bae JS, Lee JM, Jeon SK, Jang S. Comparison of MicroFlow Imaging with color and power Doppler imaging for detecting and characterizing blood flow signals in hepatocellular carcinoma. Ultrasonography. 2020;39:85-93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 13. | Kang HJ, Lee JM, Jeon SK, Ryu H, Yoo J, Lee JK, Han JK. Microvascular Flow Imaging of Residual or Recurrent Hepatocellular Carcinoma after Transarterial Chemoembolization: Comparison with Color/Power Doppler Imaging. Korean J Radiol. 2019;20:1114-1123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 14. | Lee DH, Lee JY, Han JK. Superb microvascular imaging technology for ultrasound examinations: Initial experiences for hepatic tumors. Eur J Radiol. 2016;85:2090-2095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 82] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 15. | Bartolotta TV, Midiri M, Galia M, Iovane A, Runza G, Carcione A, Lagalla R. Atypical liver hemangiomas: contrast-enhancement patterns with SH U 508A and pulse-inversion US. Radiol Med. 2003;106:320-328. [PubMed] |
| 16. | Quaia E. Microbubble ultrasound contrast agents: an update. Eur Radiol. 2007;17:1995-2008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 245] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 17. | Barr RG, Huang P, Luo Y, Xie X, Zheng R, Yan K, Jing X, Xu H, Fei X, Lee JM. Contrast-enhanced ultrasound imaging of the liver: a review of the clinical evidence for SonoVue and Sonazoid. Abdom Radiol (NY). 2020;45:3779-3788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 49] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 18. | Piscaglia F, Bolondi L; Italian Society for Ultrasound in Medicine and Biology (SIUMB) Study Group on Ultrasound Contrast Agents. The safety of Sonovue in abdominal applications: retrospective analysis of 23188 investigations. Ultrasound Med Biol. 2006;32:1369-1375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 596] [Cited by in RCA: 532] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 19. | Durot I, Wilson SR, Willmann JK. Contrast-enhanced ultrasound of malignant liver lesions. Abdom Radiol (NY). 2018;43:819-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 20. | Wu M, Li L, Wang J, Zhang Y, Guo Q, Li X, Zhang X. Contrast-enhanced US for characterization of focal liver lesions: a comprehensive meta-analysis. Eur Radiol. 2018;28:2077-2088. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (1)] |
| 21. | Zarzour JG, Porter KK, Tchelepi H, Robbin ML. Contrast-enhanced ultrasound of benign liver lesions. Abdom Radiol (NY). 2018;43:848-860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (1)] |
| 22. | Dietrich CF, Nolsøe CP, Barr RG, Berzigotti A, Burns PN, Cantisani V, Chammas MC, Chaubal N, Choi BI, Clevert DA, Cui X, Dong Y, D'Onofrio M, Fowlkes JB, Gilja OH, Huang P, Ignee A, Jenssen C, Kono Y, Kudo M, Lassau N, Lee WJ, Lee JY, Liang P, Lim A, Lyshchik A, Meloni MF, Correas JM, Minami Y, Moriyasu F, Nicolau C, Piscaglia F, Saftoiu A, Sidhu PS, Sporea I, Torzilli G, Xie X, Zheng R. Guidelines and Good Clinical Practice Recommendations for Contrast Enhanced Ultrasound (CEUS) in the Liver - Update 2020 - WFUMB in Cooperation with EFSUMB, AFSUMB, AIUM, and FLAUS. Ultraschall Med. 2020;41:562-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 140] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 23. | Choi JY, Lee JM, Sirlin CB. CT and MR imaging diagnosis and staging of hepatocellular carcinoma: part I. Development, growth, and spread: key pathologic and imaging aspects. Radiology. 2014;272:635-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 371] [Cited by in RCA: 349] [Article Influence: 31.7] [Reference Citation Analysis (1)] |
| 24. | Giambelluca D, Taibbi A, Midiri M, Bartolotta TV. The "spoke wheel" sign in hepatic focal nodular hyperplasia. Abdom Radiol (NY). 2019;44:1183-1184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Garcovich M, Faccia M, Meloni F, Bertolini E, de Sio I, Calabria G, Francica G, Vidili G, Riccardi L, Zocco MA, Ainora ME, Ponziani FR, De Gaetano AM, Gasbarrini A, Rapaccini GL, Pompili M. Contrast-enhanced ultrasound patterns of hepatocellular adenoma: an Italian multicenter experience. J Ultrasound. 2019;22:157-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 26. | Quaia E, D'Onofrio M, Palumbo A, Rossi S, Bruni S, Cova M. Comparison of contrast-enhanced ultrasonography vs baseline ultrasound and contrast-enhanced computed tomography in metastatic disease of the liver: diagnostic performance and confidence. Eur Radiol. 2006;16:1599-1609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 103] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 27. | Larsen LP. Role of contrast enhanced ultrasonography in the assessment of hepatic metastases: A review. World J Hepatol. 2010;2:8-15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 28. | Westwood M, Joore M, Grutters J, Redekop K, Armstrong N, Lee K, Gloy V, Raatz H, Misso K, Severens J, Kleijnen J. Contrast-enhanced ultrasound using SonoVue® (sulphur hexafluoride microbubbles) compared with contrast-enhanced computed tomography and contrast-enhanced magnetic resonance imaging for the characterisation of focal liver lesions and detection of liver metastases: a systematic review and cost-effectiveness analysis. Health Technol Assess. 2013;17:1-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 109] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 29. | Ferraioli G, Meloni MF. Contrast-enhanced ultrasonography of the liver using SonoVue. Ultrasonography. 2018;37:25-35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 30. | Wilson SR, Lyshchik A, Piscaglia F, Cosgrove D, Jang HJ, Sirlin C, Dietrich CF, Kim TK, Willmann JK, Kono Y. CEUS LI-RADS: algorithm, implementation, and key differences from CT/MRI. Abdom Radiol (NY). 2018;43:127-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 150] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 31. | Bartolotta TV, Terranova MC, Gagliardo C, Taibbi A. CEUS LI-RADS: a pictorial review. Insights Imaging. 2020;11:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 32. | Guang Y, Xie L, Ding H, Cai A, Huang Y. Diagnosis value of focal liver lesions with SonoVue®-enhanced ultrasound compared with contrast-enhanced computed tomography and contrast-enhanced MRI: a meta-analysis. J Cancer Res Clin Oncol. 2011;137:1595-1605. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 54] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 33. | Francica G, Meloni MF, Riccardi L, Giangregorio F, Caturelli E, Terracciano F, de Sio I. Role of Contrast-Enhanced Ultrasound in the Detection of Complications After Ultrasound-Guided Liver Interventional Procedures. J Ultrasound Med. 2021;40:1665-1673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 34. | Lu MD, Yu XL, Li AH, Jiang TA, Chen MH, Zhao BZ, Zhou XD, Wang JR. Comparison of contrast enhanced ultrasound and contrast enhanced CT or MRI in monitoring percutaneous thermal ablation procedure in patients with hepatocellular carcinoma: a multi-center study in China. Ultrasound Med Biol. 2007;33:1736-1749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 77] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 35. | Mauri G, Porazzi E, Cova L, Restelli U, Tondolo T, Bonfanti M, Cerri A, Ierace T, Croce D, Solbiati L. Intraprocedural contrast-enhanced ultrasound (CEUS) in liver percutaneous radiofrequency ablation: clinical impact and health technology assessment. Insights Imaging. 2014;5:209-216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 108] [Cited by in RCA: 103] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 36. | Lassau N, Bonastre J, Kind M, Vilgrain V, Lacroix J, Cuinet M, Taieb S, Aziza R, Sarran A, Labbe-Devilliers C, Gallix B, Lucidarme O, Ptak Y, Rocher L, Caquot LM, Chagnon S, Marion D, Luciani A, Feutray S, Uzan-Augui J, Coiffier B, Benastou B, Koscielny S. Validation of dynamic contrast-enhanced ultrasound in predicting outcomes of antiangiogenic therapy for solid tumors: the French multicenter support for innovative and expensive techniques study. Invest Radiol. 2014;49:794-800. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 101] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 37. | Dietrich CF, Bamber J, Berzigotti A, Bota S, Cantisani V, Castera L, Cosgrove D, Ferraioli G, Friedrich-Rust M, Gilja OH, Goertz RS, Karlas T, de Knegt R, de Ledinghen V, Piscaglia F, Procopet B, Saftoiu A, Sidhu PS, Sporea I, Thiele M. EFSUMB Guidelines and Recommendations on the Clinical Use of Liver Ultrasound Elastography, Update 2017 (Long Version). Ultraschall Med. 2017;38:e16-e47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 601] [Cited by in RCA: 582] [Article Influence: 72.8] [Reference Citation Analysis (0)] |
| 38. | Srinivasa Babu A, Wells ML, Teytelboym OM, Mackey JE, Miller FH, Yeh BM, Ehman RL, Venkatesh SK. Elastography in Chronic Liver Disease: Modalities, Techniques, Limitations, and Future Directions. Radiographics. 2016;36:1987-2006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 152] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 39. | Kennedy P, Wagner M, Castéra L, Hong CW, Johnson CL, Sirlin CB, Taouli B. Quantitative Elastography Methods in Liver Disease: Current Evidence and Future Directions. Radiology. 2018;286:738-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 200] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 40. | Gennisson JL, Provost J, Deffieux T, Papadacci C, Imbault M, Pernot M, Tanter M. 4-D ultrafast shear-wave imaging. IEEE Trans Ultrason Ferroelectr Freq Control. 2015;62:1059-1065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 68] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 41. | Hu X, Qiu L, Liu D, Qian L. Acoustic Radiation Force Impulse (ARFI) Elastography for noninvasive evaluation of hepatic fibrosis in chronic hepatitis B and C patients: a systematic review and meta-analysis. Med Ultrason. 2017;19:23-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 42. | Barr RG, Wilson SR, Rubens D, Garcia-Tsao G, Ferraioli G. Update to the Society of Radiologists in Ultrasound Liver Elastography Consensus Statement. Radiology. 2020;296:263-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 319] [Cited by in RCA: 274] [Article Influence: 54.8] [Reference Citation Analysis (1)] |
| 43. | Furlan A, Tublin ME, Yu L, Chopra KB, Lippello A, Behari J. Comparison of 2D Shear Wave Elastography, Transient Elastography, and MR Elastography for the Diagnosis of Fibrosis in Patients With Nonalcoholic Fatty Liver Disease. AJR Am J Roentgenol. 2020;214:W20-W26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 102] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 44. | Park CC, Nguyen P, Hernandez C, Bettencourt R, Ramirez K, Fortney L, Hooker J, Sy E, Savides MT, Alquiraish MH, Valasek MA, Rizo E, Richards L, Brenner D, Sirlin CB, Loomba R. Magnetic Resonance Elastography vs Transient Elastography in Detection of Fibrosis and Noninvasive Measurement of Steatosis in Patients With Biopsy-Proven Nonalcoholic Fatty Liver Disease. Gastroenterology. 2017;152:598-607.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 479] [Cited by in RCA: 542] [Article Influence: 67.8] [Reference Citation Analysis (0)] |
| 45. | Berzigotti A, Ferraioli G, Bota S, Gilja OH, Dietrich CF. Novel ultrasound-based methods to assess liver disease: The game has just begun. Dig Liver Dis. 2018;50:107-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 46. | Karlas T, Petroff D, Sasso M, Fan JG, Mi YQ, de Lédinghen V, Kumar M, Lupsor-Platon M, Han KH, Cardoso AC, Ferraioli G, Chan WK, Wong VW, Myers RP, Chayama K, Friedrich-Rust M, Beaugrand M, Shen F, Hiriart JB, Sarin SK, Badea R, Jung KS, Marcellin P, Filice C, Mahadeva S, Wong GL, Crotty P, Masaki K, Bojunga J, Bedossa P, Keim V, Wiegand J. Individual patient data meta-analysis of controlled attenuation parameter (CAP) technology for assessing steatosis. J Hepatol. 2017;66:1022-1030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 881] [Cited by in RCA: 838] [Article Influence: 104.8] [Reference Citation Analysis (0)] |
| 47. | Ferraioli G, Soares Monteiro LB. Ultrasound-based techniques for the diagnosis of liver steatosis. World J Gastroenterol. 2019;25:6053-6062. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 324] [Cited by in RCA: 299] [Article Influence: 49.8] [Reference Citation Analysis (8)] |
| 48. | Bae JS, Lee DH, Lee JY, Kim H, Yu SJ, Lee JH, Cho EJ, Lee YB, Han JK, Choi BI. Assessment of hepatic steatosis by using attenuation imaging: a quantitative, easy-to-perform ultrasound technique. Eur Radiol. 2019;29:6499-6507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 114] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 49. | Dioguardi Burgio M, Ronot M, Reizine E, Rautou PE, Castera L, Paradis V, Garteiser P, Van Beers B, Vilgrain V. Quantification of hepatic steatosis with ultrasound: promising role of attenuation imaging coefficient in a biopsy-proven cohort. Eur Radiol. 2020;30:2293-2301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 76] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 50. | Downey DB, Fenster A, Williams JC. Clinical utility of three-dimensional US. Radiographics. 2000;20:559-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 137] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 51. | Dong FJ, Xu JF, Du D, Jiao Y, Zhang L, Li M, Liu HY, Xiong Y, Luo H. 3D analysis is superior to 2D analysis for contrast-enhanced ultrasound in revealing vascularity in focal liver lesions - A retrospective analysis of 83 cases. Ultrasonics. 2016;70:221-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 52. | Cao J, Dong Y, Fan P, Mao F, Wang W. Feasibility of dynamic three-dimensional contrast-enhanced ultrasound in focal liver lesions: Image quality evaluation and correlation of quantification with two-dimensional contrast-enhanced ultrasound. Clin Hemorheol Microcirc. 2019;72:305-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 53. | Lee MW. Fusion imaging of real-time ultrasonography with CT or MRI for hepatic intervention. Ultrasonography. 2014;33:227-239. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 116] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 54. | Park HJ, Lee MW, Lee MH, Hwang J, Kang TW, Lim S, Rhim H, Lim HK. Fusion imaging-guided percutaneous biopsy of focal hepatic lesions with poor conspicuity on conventional sonography. J Ultrasound Med. 2013;32:1557-1564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 55. | Kang TW, Lee MW, Song KD, Kim M, Kim SS, Kim SH, Ha SY. Added Value of Contrast-Enhanced Ultrasound on Biopsies of Focal Hepatic Lesions Invisible on Fusion Imaging Guidance. Korean J Radiol. 2017;18:152-161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 56. | Song KD, Lee MW, Rhim H, Cha DI, Chong Y, Lim HK. Fusion imaging-guided radiofrequency ablation for hepatocellular carcinomas not visible on conventional ultrasound. AJR Am J Roentgenol. 2013;201:1141-1147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 83] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 57. | Lee MW, Rhim H, Cha DI, Kim YJ, Lim HK. Planning US for percutaneous radiofrequency ablation of small hepatocellular carcinomas (1-3 cm): value of fusion imaging with conventional US and CT/MR images. J Vasc Interv Radiol. 2013;24:958-965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 67] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 58. | Minami Y, Kudo M. Review of dynamic contrast-enhanced ultrasound guidance in ablation therapy for hepatocellular carcinoma. World J Gastroenterol. 2011;17:4952-4959. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 43] [Cited by in RCA: 49] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 59. | Calandri M, Mauri G, Yevich S, Gazzera C, Basile D, Gatti M, Veltri A, Fonio P. Fusion Imaging and Virtual Navigation to Guide Percutaneous Thermal Ablation of Hepatocellular Carcinoma: A Review of the Literature. Cardiovasc Intervent Radiol. 2019;42:639-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 60. | Li K, Su ZZ, Xu EJ, Ju JX, Meng XC, Zheng RQ. Improvement of ablative margins by the intraoperative use of CEUS-CT/MR image fusion in hepatocellular carcinoma. BMC Cancer. 2016;16:277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 61. | Xu EJ, Lv SM, Li K, Long YL, Zeng QJ, Su ZZ, Zheng RQ. Immediate evaluation and guidance of liver cancer thermal ablation by three-dimensional ultrasound/contrast-enhanced ultrasound fusion imaging. Int J Hyperthermia. 2018;34:870-876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 49] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 62. | Pitt WG, Husseini GA, Staples BJ. Ultrasonic drug delivery--a general review. Expert Opin Drug Deliv. 2004;1:37-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 444] [Cited by in RCA: 391] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 63. | Kim D, Lee JH, Moon H, Seo M, Han H, Yoo H, Seo H, Lee J, Hong S, Kim P, Lee HJ, Chung JW, Kim H. Development and evaluation of an ultrasound-triggered microbubble combined transarterial chemoembolization (TACE) formulation on rabbit VX2 Liver cancer model. Theranostics. 2021;11:79-92. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 64. | Novoselova MV, German SV, Abakumova TO, Perevoschikov SV, Sergeeva OV, Nesterchuk MV, Efimova OI, Petrov KS, Chernyshev VS, Zatsepin TS, Gorin DA. Multifunctional nanostructured drug delivery carriers for cancer therapy: Multimodal imaging and ultrasound-induced drug release. Colloids Surf B Biointerfaces. 2021;200:111576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 65. | Lewis S, Hectors S, Taouli B. Radiomics of hepatocellular carcinoma. Abdom Radiol (NY). 2021;46:111-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 50] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 66. | Cannella R, La Grutta L, Midiri M, Bartolotta TV. New advances in radiomics of gastrointestinal stromal tumors. World J Gastroenterol. 2020;26:4729-4738. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 67. | Peng Y, Lin P, Wu L, Wan D, Zhao Y, Liang L, Ma X, Qin H, Liu Y, Li X, Wang X, He Y, Yang H. Ultrasound-Based Radiomics Analysis for Preoperatively Predicting Different Histopathological Subtypes of Primary Liver Cancer. Front Oncol. 2020;10:1646. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 68. | Mao B, Ma J, Duan S, Xia Y, Tao Y, Zhang L. Preoperative classification of primary and metastatic liver cancer via machine learning-based ultrasound radiomics. Eur Radiol. 2021;31:4576-4586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 63] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 69. | Hu HT, Wang Z, Huang XW, Chen SL, Zheng X, Ruan SM, Xie XY, Lu MD, Yu J, Tian J, Liang P, Wang W, Kuang M. Ultrasound-based radiomics score: a potential biomarker for the prediction of microvascular invasion in hepatocellular carcinoma. Eur Radiol. 2019;29:2890-2901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 141] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 70. | Song KD. Current status of deep learning applications in abdominal ultrasonography. Ultrasonography. 2021;40:177-182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 71. | Zhou LQ, Wang JY, Yu SY, Wu GG, Wei Q, Deng YB, Wu XL, Cui XW, Dietrich CF. Artificial intelligence in medical imaging of the liver. World J Gastroenterol. 2019;25:672-682. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 192] [Cited by in RCA: 138] [Article Influence: 23.0] [Reference Citation Analysis (8)] |
| 72. | Lee JH, Joo I, Kang TW, Paik YH, Sinn DH, Ha SY, Kim K, Choi C, Lee G, Yi J, Bang WC. Deep learning with ultrasonography: automated classification of liver fibrosis using a deep convolutional neural network. Eur Radiol. 2020;30:1264-1273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 85] [Article Influence: 14.2] [Reference Citation Analysis (0)] |