Published online Jan 15, 2020. doi: 10.4251/wjgo.v12.i1.77
Peer-review started: July 3, 2019
First decision: July 31, 2019
Revised: August 24, 2019
Accepted: September 26, 2019
Article in press: September 26, 2019
Published online: January 15, 2020
Processing time: 182 Days and 1 Hours
Diagnosis of lympho-proliferative diseases is sometimes challenging. Excisional lymph node biopsy is the standard of care. Five percent of the patients will present with abdominal or retroperitoneal lymphadenopathy alone. Advancements in endoscopic techniques allow for access to fine needle biopsy in complicated areas, but this often does not meet the standard guidelines for diagnosis.
To investigate the results of laparoscopic excisional biopsy of the hepatic node (LEBHN) through a trans lesser omentum approach.
Data of all patients undergoing LEBHN were collected retrospectively from patients’ electronic charts over a period of 1 year. Data collected included age, gender, suspected disease, number of previous biopsies and biopsy method, surgical approach, intraoperative complications, operative time, post-operative complications, mortality, and final diagnosis.
Six patients were operated in this technique during the time frame of the study, 66.6% (n = 4) were females, and median age was 55 years (range: 25-72 years). We present no conversions from laparoscopy to laparotomy, and mean operating time was 51.2 min. Mean length of hospital stay was 1 d, and morbidity and mortality were nil. Most importantly, this technique offered definite diagnosis and appropriate treatment in all patients. Final diagnosis included two patients with lymphoma (Hodgkin and Follicular), two patients with sarcoidosis, and two patients with reactive lymph nodes with no evidence of malignancy.
In conclusion, this technique seems to be feasible and safe and may offer a simple approach for a definite diagnosis for what seems to be a complicated anatomical area.
Core tip: Diagnosis of lympho-proliferative diseases is sometimes challenging, and laparoscopy is an essential tool. Laparoscopic excisional biopsy of the hepatic node seems to be feasible and safe and may offer a simple approach for a definite diagnosis for what seems to be a complicated anatomical area.
- Citation: Ben-Ishay O. Laparoscopic dissection of the hepatic node: The trans lesser omentum approach. World J Gastrointest Oncol 2020; 12(1): 77-82
- URL: https://www.wjgnet.com/1948-5204/full/v12/i1/77.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v12.i1.77
Diagnosis of lympho-proliferative diseases is sometimes challenging. Based upon the current international guidelines[1,2], a surgically excised tissue biopsy is widely accepted as the gold standard for the diagnosis of lymphoma. An excisional biopsy of a lymph node (LN) allows assessment of the micro-architecture and provides adequate material for immunocytochemistry, flow cytometry, fluorescence in situ hybridization studies, and extraction of DNA and RNA for molecular diagnostics. The major disadvantages of surgical biopsies are the probable need for general anesthesia and deferrals due to the need of a surgical consult and operating room time. These issues are addressed through percutaneous and endoscopic core needle biopsies or fine needle aspiration with cellblock techniques.
When possible, a superficial LN, most often from the groin or axilla, should be excised, and this can be done simply under local anesthesia in day care setup. Often though this is not possible, and an intra-abdominal LN must be obtained.
The intra-abdominal lymphatic system is complex, and lymphadenopathy is often retroperitoneal, along the celiac axis and in the pelvis. Traditionally, laparoscopic biopsies of retroperitoneal or celiac nodes are considered complicated. Lymph nodes that are distributed along the celiac trunk include the root of the left gastric (station 7), the proper hepatic artery (station 8), and the splenic artery (station 9).
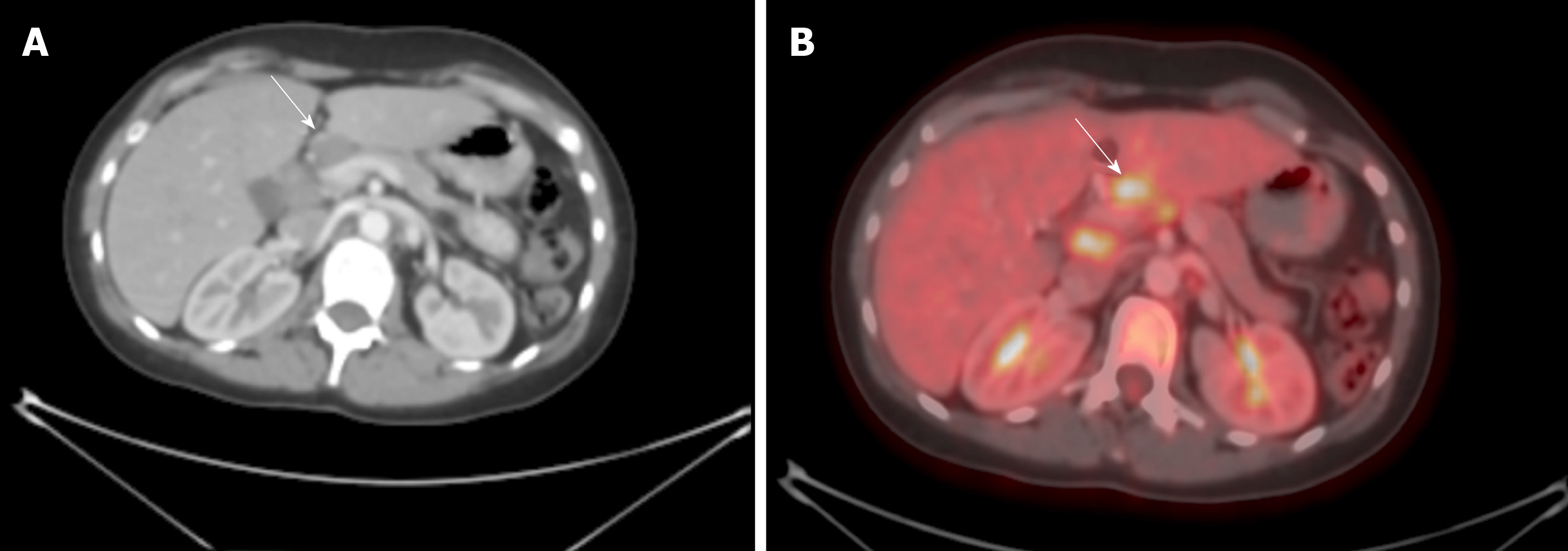
The hepatic node is the lymph node lying on the proper hepatic artery right above the neck of the pancreas. This node is quite often enlarged and has an abnormal fluorodeoxyglucose uptake on positron emission tomography (Figure 1).
Approach to the supra-pancreatic area is complex; the current study presents our experience with six patients who underwent laparoscopic excision of the hepatic node (LEBHN) through a trans lesser omentum approach.
After general anesthesia was induced, the patient was placed in a lithotomy position, and the operating table was maintained in 20° into the reverse Trendelenburg position. The surgeon was located between the legs of the patient, while the first assistant and the camera operator were placed to the left and the right side of the patient respectively.
After insufflation of the abdomen with CO2 through a veres needle, a 10 mm trocar was placed above the umbilicus. The camera was than inserted, and an exploration of the abdomen was performed. A second 10 mm trocar was placed in mid left abdomen, and three 5 mm trocars were placed sub-xifoide, mid right quadrant, and left upper quadrant.
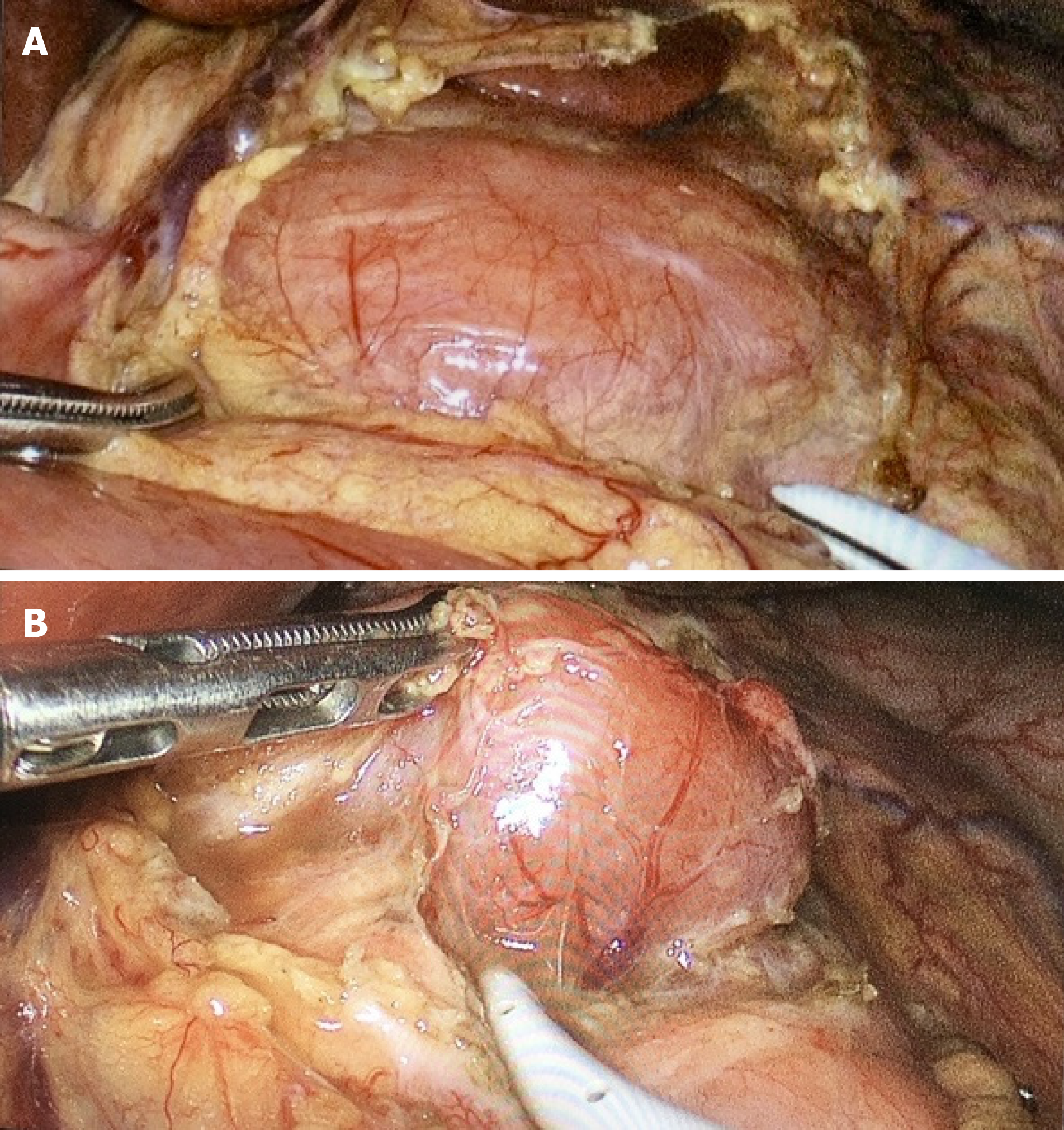
The left lobe of the liver was retracted upwards towards the diaphragm, and the lesser omentum with its pars flaccida was exposed. The pars flaccida was excised, the supra-pancreatic area was exposed, and the hepatic node was then observed (Figure 2A). The peritoneal layer above the hepatic node was carefully dissected with an electric cautery, and the node was than dissected carefully with bipolar energy (Figure 2B).
Data of all patients undergoing LEBHN over a period of 1 year were collected retrospectively within the array of the surgical oncology service of the Department of general surgery at the Rambam Health Care Campus. Data included demographics, preoperative data including number of previous biopsies, previous biopsy methods used, and operative and post-operative data. Operative and postoperative complications were recorded.
Six patients were operated in this technique during the time frame of the study, 66.6% (n = 4) were females, and the median age was 55 years (25-72). Two patients had a suspected recurrence of a previously treated lymphoma. Three patients had one previous attempt for tissue diagnosis, and one had three of them. One patient had percutaneous attempt for biopsy, four had endoscopic biopsies trough endoscopic ultrasound, and one patient had a mediastinoscopy with mediastinal biopsy. Table 1 depicts the demographic operative and post-operative characteristics of the entire cohort. All patients were operated in a laparoscopic approach with no conversions to laparotomy. All patients had an uneventful operation with no operative or post-operative complications. Mean length of hospital stay was 1 d, and morbidity and mortality were nil.
| Age | Gender | No of Biopsies | FNA | FNB | ORT | LOS | Complications | Diagnosis |
| 72 | F | 1 | Yes | No | 71 | 1 | No | Follicular LY |
| 39 | F | 1 | No | No | 53 | 1 | No | Hodgkin LY |
| 25 | M | 0 | No | No | 49 | 1 | No | Sarcoidosis |
| 60 | F | 0 | No | No | 65 | 1 | No | Reactive LN |
| 69 | F | 3 | Yes | Yes | 47 | 1 | No | Sarcoidosis |
| 51 | M | 1 | No | No | 22 | 1 | No | Reactive LN |
Retroperitoneal lymphadenopathy occurs in various hematologic and granulomatous diseases. Approximately 5% of patients will have abdominal lymphadenopathy without enlargement of LN in superficial areas[4]. Advancements in percutaneous and endoscopic techniques allow diagnosis through minor ambulatory procedures. Laparoscopic abdominal and retroperitoneal lymph node biopsy was previously proven to be feasible and safe in the diagnosis of lympho-proliferative diseases[3-13]. Biopsy of celiac nodes or hepatic nodes though has been described occasionally in the literature. The current study describes six patients that underwent a laparoscopic celiac node biopsy in a trans lesser omentum approach. The advantages of this technique over other endoscopic approaches are the high chances for a definitive diagnosis, a better diagnostic yield, and early instigation of treatment.
The approach to the supra-pancreatic area is possible through dissection of the gastro-colic ligament and entrance to the lesser sac, this technique allows full exposure of the pancreas, splenic artery, and hepatic artery. Pisano et al[4] used this approach in four cases. This technique carried some disadvantages as mobilization of the large curvature of the stomach increases the rate of complications, such as intraoperative hemorrhage and injury to the stomach, and significant increases the operating time.
In our small case series, there were no conversions to laparotomy. The outcomes of operative time, blood loss, and complications were acceptable. All patients received an accurate diagnosis without any false-negative results.
Although the results of this current patient series are good, the small sample size does not permit firm conclusions.
In conclusion, LEBHN seems to be feasible and safe, and surgeons may use this simple approach to a fairly complicated anatomical area to patients who do not have access to superficial lymph nodes.
Diagnosis of lympho-proliferative diseases is challenging. Although an excisional biopsy of a complete lymph node is the gold standard for diagnosis, endoscopic or percutaneous techniques are often used due to the surgical challenge the location of the lymph node imposes.
The current study describes a small case series of laparoscopic dissection of the hepatic node through a trans lesser omentum approach. This approach is rarely discussed in the English literature.
The study describes the clinical and surgical results of this novel technique.
A single center, retrospective evaluation of patients undergoing laparoscopic dissection and excisional biopsy of the hepatic node.
During the time frame of the study, six patients were operated using this novel technique, with no conversions to laparotomy, no intra and post-operative complications and acceptable operating time. Most importantly, surgery yielded a definite diagnosis in all patients, and there was no need for further investigation.
Laparoscopic dissection of the hepatic node seems to be feasible and safe, and surgeons may use this simple approach to a fairly complicated anatomical area in highly selected patients who do not have access to superficial lymph nodes.
This study suggests that approach to the hepatic node and the celiac axis is easily and safely performed through a trans lesser omentum approach. This may facilitate future discussion on how to achieve the diagnosis of lympho-proliferative disease in patients who do not have enlarged and pathological superficial lymph nodes.
Manuscript source: Unsolicited manuscript
Specialty type: Oncology
Country of origin: Israel
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Isik A, Sergi CM S-Editor: Ma YJ L-Editor: Filipodia E-Editor: Qi LL
| 1. | Cheson BD, Fisher RI, Barrington SF, Cavalli F, Schwartz LH, Zucca E, Lister TA; Alliance, Australasian Leukaemia and Lymphoma Group; Eastern Cooperative Oncology Group; European Mantle Cell Lymphoma Consortium; Italian Lymphoma Foundation; European Organisation for Research; Treatment of Cancer/Dutch Hemato-Oncology Group; Grupo Español de Médula Ósea; German High-Grade Lymphoma Study Group; German Hodgkin's Study Group; Japanese Lymphorra Study Group; Lymphoma Study Association; NCIC Clinical Trials Group; Nordic Lymphoma Study Group; Southwest Oncology Group; United Kingdom National Cancer Research Institute. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol. 2014;32:3059-3068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2850] [Cited by in RCA: 3842] [Article Influence: 349.3] [Reference Citation Analysis (0)] |
| 2. | Tilly H, Gomes da Silva M, Vitolo U, Jack A, Meignan M, Lopez-Guillermo A, Walewski J, André M, Johnson PW, Pfreundschuh M, Ladetto M; ESMO Guidelines Committee. Diffuse large B-cell lymphoma (DLBCL): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26 Suppl 5:v116-v125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 524] [Cited by in RCA: 584] [Article Influence: 58.4] [Reference Citation Analysis (0)] |
| 3. | Durai R, Mir N, Ng PC. Laparoscopic retroperitoneal/mesenteric lymph node sampling: a safe and effective technique. Singapore Med J. 2011;52:758-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Pisano G, Calò PG, Piras S, Sanna S, Manca A, Tatti A, Nicolosi A. Laparoscopic lymph node biopsy in the diagnosis of lymphoma. Indications and results. Ann Ital Chir. 2012;83:469-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Cowles RA, Yahanda AM. Laparoscopic biopsy of abdominal retroperitoneal lymphadenopathy for the diagnosis of lymphoma. J Am Coll Surg. 2000;191:108-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Gossot D, de Kerviler E, Brice P, Mariette X, Meignin V, Cazals-Hatem D, Frija J, Célérier M. Surgical endoscopic techniques in the diagnosis and follow-up of patients with lymphoma. Br J Surg. 1998;85:1107-1110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Strickler JG, Donohue JH, Porter LE, Habermann TM. Laparoscopic biopsy for suspected abdominal lymphoma. Mod Pathol. 1998;11:831-836. [PubMed] |
| 8. | Walsh RM, Heniford BT. Role of laparoscopy for Hodgkin's and non-Hodgkin's lymphoma. Semin Surg Oncol. 1999;16:284-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Silecchia G, Fantini A, Raparelli L, De Leo A, Vitolo D, Monarca B, Bezzi M, Rosato P, Basso N. Management of abdominal lymphoproliferative diseases in the era of laparoscopy. Am J Surg. 1999;177:325-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Silecchia G, Raparelli L, Perrotta N, Fantini A, Fabiano P, Monarca B, Basso N. Accuracy of laparoscopy in the diagnosis and staging of lymphoproliferative diseases. World J Surg. 2003;27:653-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Asoglu O, Porter L, Donohue JH, Cha SS. Laparoscopy for the definitive diagnosis of intra-abdominal lymphoma. Mayo Clin Proc. 2005;80:625-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Casaccia M, Torelli P, Cavaliere D, Panaro F, Nardi I, Rossi E, Spriano M, Bacigalupo A, Gentile R, Valente U. Laparoscopic lymph node biopsy in intra-abdominal lymphoma: high diagnostic accuracy achieved with a minimally invasive procedure. Surg Laparosc Endosc Percutan Tech. 2007;17:175-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Daly SC, Klairmont M, Arslan B, Vigneswaran Y, Roggin KF, Ujiki MB, Denham W, Millikan KW, Luu MB, Deziel DJ, Myers JA. Laparoscopy has a superior diagnostic yield than percutaneous image-guided biopsy for suspected intra-abdominal lymphoma. Surg Endosc. 2015;29:2496-2499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |