Published online Dec 15, 2018. doi: 10.4251/wjgo.v10.i12.516
Peer-review started: September 18, 2018
First decision: October 15, 2018
Revised: October 24, 2018
Accepted: November 7, 2018
Article in press: November 7, 2018
Published online: December 15, 2018
Processing time: 87 Days and 9.4 Hours
Hemangioma of the small intestine is a rare vascular malformation. Before the advent of capsule endoscopy (CE) and balloon-assisted enteroscopy (BAE), preoperative diagnosis of this disease was extremely difficult.
In this study, we report a 24-year-old female with a large transmural small bowel cavernous hemangioma, which was diagnosed with CE and BAE preoperatively and removed successfully using minimally invasive surgery. Meanwhile, we perform a literature review of the studies about intestinal hemangiomas published after 2000. Literature review revealed that 91.9% of the lesions were diagnosed preoperatively by CE and/or BAE and 45.9% of them were treated endoscopically, which is a marked improvement compared to before 2000. Therefore, CE and BAE are useful modalities for the preoperative diagnosis of hemangiomas in the small intestine.
Endoscopic treatment of intestinal hemangioma is generally prudent and might be suitable for multiple, relatively small lesions.
Core tip: Hemangioma of the small intestine is a rare disease and mostly presents as gastrointestinal bleeding. With the advent of capsule endoscopy and balloon-assisted enteroscopy, the preoperative diagnosis of this disease has been considerably improved. Surgical resection is the conventional treatment modality. With the improvement of endoscopic therapeutic interventions, less invasive procedures are becoming possible. However, potential risks of endoscopic treatment include bleeding and intestinal perforation. Since intestinal hemangiomas originate from the submucosal layer and some of them are transmural, endoscopic treatment might sometimes result in uncontrolled bleeding or perforation.
- Citation: Hu PF, Chen H, Wang XH, Wang WJ, Su N, Shi B. Small intestinal hemangioma: Endoscopic or surgical intervention? A case report and review of literature. World J Gastrointest Oncol 2018; 10(12): 516-521
- URL: https://www.wjgnet.com/1948-5204/full/v10/i12/516.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v10.i12.516
Hemangioma of the small intestine is a rare disease, accounting for 7%-10% of all benign tumors of the small intestine[1,2]. It may be solitary or multiple, with the jejunum being the most common site of involvement[3]. The main presenting symptoms include hemorrhage, abdominal pain, obstruction, intussusceptions, or rarely, perforation[4,5]. It originates from the submucosal vascular plexuses and may extend into the muscular layer or beyond[6]. Histologically, hemangiomas are congenital benign vascular lesions that can be classified as capillary, cavernous, or mixed-type according to the size of the vascular channels[2]. With the advent of capsule endoscopy (CE) and balloon-assisted enteroscopy (BAE), complete investigation of the small bowel is possible[7]. The preoperative diagnosis of this disease has been considerably improved. Recent advances in endoscopic techniques have led to successful endoscopic intervention, but most large lesions have been treated surgically. Here, we present a case with solitary small bowel hemangioma, which was diagnosed preoperatively by CE and BAE and removed successfully using minimally invasive surgery.
A 24-year-old female suffered from recurrent melena and fatigue for 1 year.
Over the past year, the patient experienced repeated black stool, accompanied by fatigue, without hematemesis, hematochezia, abdominal pain or fever. The lowest level of hemoglobin was 42 g/L.
Past and family medical history was unremarkable.
Physical examination showed moderate anemia. Detailed dermatological evaluation did not show any cutaneous lesions.
Laboratory studies revealed moderated microcytic and hypochromic anemia (hemoglobin, 7.5 g/dL). Fecal occult blood test was positive.
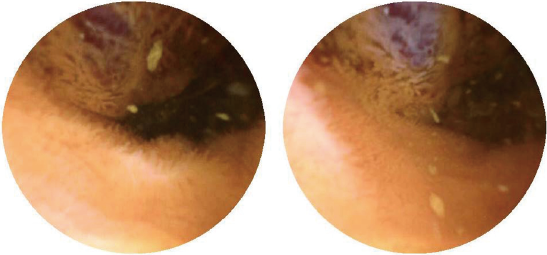
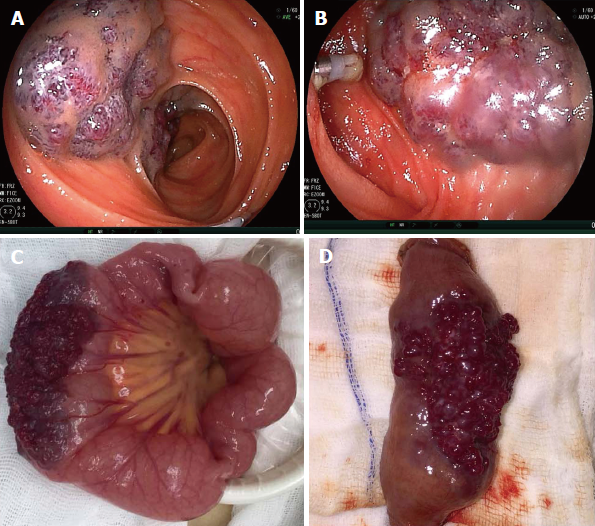
Gastroscopy and colonoscopy were normal. CE was performed, showing a prominent polypoid lesion in the ileum with no sign of active bleeding (Figure 1). Transanal double-balloon enteroscopy (DBE) revealed a reddish purple lesion in the ileum about 80 cm proximal to the ileocecal valve (Figure 2A). A titanium clip was used to mark the limit reached. Transoral DBE was performed to assess the remainder of small bowel, which revealed no additional lesions (Figure 2B).
From the endoscopic appearance of the lesion, it was most likely a hemangioma. Considering that the lesion was large and diffuse, endoscopic interventions such as endoscopic mucosal resection (EMR) and endoscopic sclerotherapy might lead to uncontrolled bleeding or perforation. Therefore, laparoscopic surgery was deemed the best choice.
The patient had repeated bleeding and a large amount of bleeding every time. Since the lesion was large and diffuse, surgery would be better for the patient.
The patient suffered from recurrent melena in the past year. From the results of the CE and BAE, the cause is likely the small intestinal hemangioma. The surgical indication was explicit.
The diagnosis is relatively clear. Since biopsy might lead to uncontrolled bleeding, we could not verify the diagnosis preoperatively.
Imaging examination including ultrasound and CT scan did not find any abnormalities. From the endoscopic appearance of the lesion, it was most likely a hemangioma. The patient was a young female with a good health status. We could consider resecting the lesion laparoscopically.
Small bowel bleeding and small intestinal hemangioma.
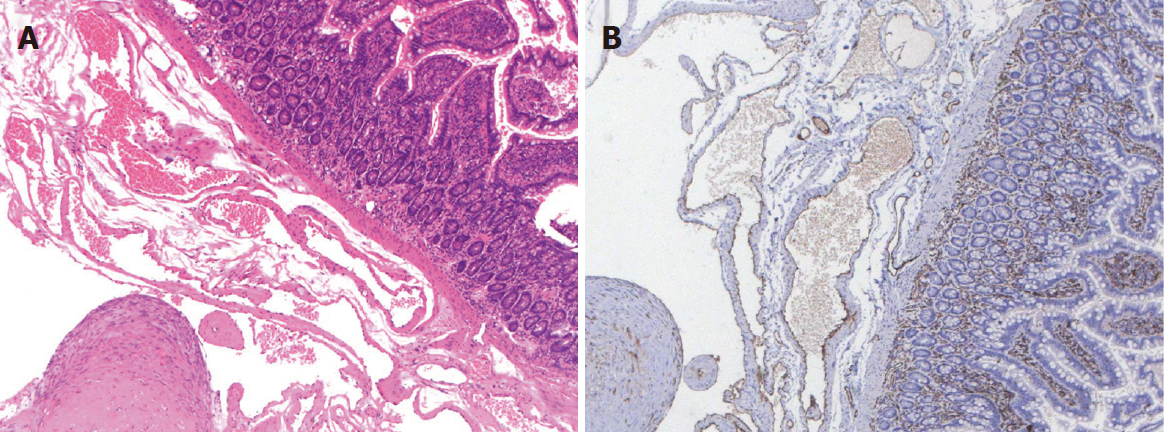
The patient was sent to laparoscopy, and a 5 cm × 3 cm × 3 cm purple-colored, raspberry-like lesion was found spreading diffusely along the serosal surface of the ileum (Figure 2C). The lesion was completely resected (Figure 2D). Hematoxylin-eosin staining (Figure 3A) and CD31 immunohistochemistry (Figure 3B) indicated a transmural cavernous hemangioma.
The patient recovered quickly and had no further episodes of bleeding since the operation. The hemoglobin value increased to normal (12.4 g/dL) and was stable.
Hemangioma accounts for only 0.05% of all gastrointestinal (GI) neoplasms. They mostly present with occult GI bleeding and iron deficiency anemia. Because of its rarity, it is not considered a common cause of GI bleeding. Previously, the preoperative diagnosis of this disease was difficult, and almost all cases were diagnosed during or after the operation[1]. With the introduction of CE and BAE over the past decades, the small intestine has now become an area that can be targeted[8]. We searched the PubMed database for studies about intestinal hemangiomas published after 2000 utilizing the following search terms: “hemangioma”, “vascular malformation”, “small intestine” and “small bowel”. A manual search was also performed using the references of eligible articles. The language was limited to English. A total of 37 cases (16 women, 21 men, mean age 39 years) were retrieved and reviewed (Table 1). The most common manifestation included GI bleeding and anemia. A total of 75.7% (28/37) of the cases were single, and the common location of the small intestine was the jejunum (60.9%). Thirty-four of the 37 lesions (91.9%) were diagnosed before operation by CE and/or BAE. Of these cases, 11 were detected with CE alone, and 22 were diagnosed with both CE and BAE. Compared with the cases reported before 2000, a markedly increased proportion of cases were preoperatively diagnosed[1]. As in our case, CE was used to initially examine the GI tract, which was based on the algorithms for the diagnosis and treatment of obscure GI bleeding[7]. Both transanal DBE and transoral DBE were then performed to complete total enteroscopy, which was useful to localize the lesion and rule out other lesions.
| Ref. | Country | Case | Sex/age | Complaint | Diagnosis | Location | Single/multiple | Treatment | Pathology |
| Easler et al[9] | United States | 1 | M/71 | Anemia, melena | BAE | Jejunum | Single | EMR | Cavernous |
| Ng et al[10] | China | 1 | F/20 | Anemia | Small bowel enema | Terminal ileum | Multiple | APC | - |
| Wardi et al[11] | Israel | 1 | M/77 | Anemia, melena | CE | Ileum | Single | Laparoscopy | Capillary |
| Ersoy et al[6] | Turkey | 1 | F/50 | Melena, hematemesis | CE + BAE | Proximal jejunum | Single | Laparoscopy | Cavernous |
| Fernandes et al[12] | Portugal | 1 | F/56 | Hematochezia, syncope | CE | Ileum | Single | Laparoscopy | Cavernous |
| Law[13] | China | 1 | F/31 | Melena | CE + BAE | Jejunum | Single | Laparoscopy | Cavernous |
| Ning et al[14] | China | 1 | M/10 | Melena | BAE | Jejunum/ileum | Multiple | Polidocanol injection | - |
| Elias et al[15] | United States | 1 | M/30 | Anemia | CE + BAE | Jejunum | Multiple | Surgery | Cavernous |
| Shibuya et al[16] | Japan | 1 | M/74 | Melena | CE + BAE | jejunum | Single | EMR | Capillary |
| Willert et al[8] | Australia | 1 | M/19 | Anemia | CE + BAE | Jejunum/ileum | Multiple | EMR | Cavernous |
| Igawa et al[17] | Japan | 12 | 6M/6F | Gastrointestinal bleeding | CE + BAE | Jejunum/ileum | 7 single/5 multiple | Polidocanol injection | - |
| Takase et al[18] | Japan | 2 | F-62/M-52 | Melena | CE + BAE | Jejunum/ileum | Single | Laparoscopy | Cavernous/capillary |
| Akazawa et al[19] | Japan | 1 | F/56 | Melena | CE + BAE | Jejunum | Single | Laparoscopy | Cavernous |
| Chen et al[20] | United States | 1 | M/23 | Fatigue | CE | Ileum | Single | Laparoscopy | Cavernous |
| Dhumane et al[21] | France | 1 | M/60 | Anemia | CE + BAE | Jejunum | Single | Laparoscopy | Cavernous |
| Bae et al[22] | South Korea | 1 | M/13 | Dizziness, fatigue | CE | Jejunum | Single | Laparoscopy | Cavernous |
| Huber et al[23] | Germany | 1 | M/23 | Weakness, dizziness | CE + BAE | Jejunum | Single | Laparoscopy | Cavernous |
| Quentin et al[3] | France | 1 | F/32 | Hematochezia | CE | Jejunum | Single | Laparoscopy | Cavernous |
| Khurana et al[24] | United States | 1 | M/62 | Melena | BAE | Jejunum | Single | Surgery | Cavernous |
| Pera et al[25] | Spain | 1 | M/16 | Fatigue | CE | Jejunum | Single | Laparoscopy | - |
| Pinho et al[26] | Portugal | 1 | F/9 | Melena, anemia | CE | Ileum | Single | Surgery | Cavernous |
| Magnano et al[27] | Italy | 1 | M/13 | Fatigue, malaise | CE | Ileum | Single | Laparoscopy | Cavernous |
| Kuo et al[28] | China | 1 | F/20 | Abdominal pain | - | Jejunum | Single | Laparoscopy | Cavernous |
| Guardiola et al[29] | Spain | 1 | M/19 | Anemia | CE | Ileum | Single | Laparoscopy | Cavernous |
| Purdy-Payne et al[30] | United States | 1 | F/20 | Abdominal pain | - | Terminal ileum | Single | Laparoscopy | Cavernous |
Surgical resection, which is relatively more invasive, is the conventional treatment modality for intestinal hemangiomas. With the improvement of endoscopic therapeutic interventions, less invasive procedures are becoming more widely employed. Of the 37 cases of intestinal hemangiomas published after 2000 (Table 1), 17 cases (45.9%) were treated endoscopically. Among them, 3 cases were removed by EMR, one case was treated by argon plasma coagulation, and 13 cases were subjected to sclerotherapy. Most of these lesions were multiple (14/17, 82.4%), and the lesions were relatively small. As suggested by the guideline on the management of small bowel bleeding, the patient should be managed with endoscopic therapy if a source of bleeding is found. Surgical treatment is generally regarded as a last resort[7]. Compared with surgery, endoscopic treatments including sclerotherapy and EMR are less invasive. However, they increase the potential risks of GI bleeding and intestinal perforation. Since intestinal hemangiomas originate from the submucosal layer, endoscopic treatment such as EMR is dangerous because of the risk of perforation. Endoscopic treatment might lead to perforation because some intestinal hemangiomas were transmural, as in our case. Considering that the hemangioma was large in the current case, uncontrolled bleeding would probably occur after endoscopic intervention. After discussion with a multidisciplinary team, which included gastroenterologists, endoscopists and surgeons, we decided to remove the lesion by laparoscopy. It turned out that a laparoscopic approach was likely the best choice for our case, as the lesion was relatively large and most importantly, transmural. Thus, endoscopic treatment of intestinal hemangioma should be prudent. It is likely suitable for multiple, relatively small lesions.
In conclusion, we present a case of small bowel hemangioma that was preoperatively diagnosed by CE and BAE and treated by laparoscopy. We believe it is important for both the endoscopist and surgeons to recognize this somewhat unusual lesion. It is recommended that careful consideration of the indications for endoscopic treatment. As in our case, hemangiomas may sometimes involve the entire wall of the intestine. Endoscopic intervention may lead to uncontrolled bleeding or perforation. For the large and diffuse lesions, a laparoscopic excision might be a better approach.
Hemangioma of the small intestine is a rare disease, which mostly presented as occult GI bleeding and iron deficiency anemia. With the advent of CE and BAE, the diagnosis of lesions in the small intestine has been considerably improved. Endoscopic treatment of intestinal hemangioma should be prudent, and it might be suitable for multiple and relatively small lesions.
Conflict of interest statement: The authors have no conflict of interest to declare.
Manuscript source: Unsolicited manuscript
Specialty type: Oncology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Cao ZF, Sawaki A, Yarema RR S- Editor: Ji FF L- Editor: Filipodia E- Editor: Song H
| 1. | Ramanujam PS, Venkatesh KS, Bettinger L, Hayashi JT, Rothman MC, Fietz MJ. Hemangioma of the small intestine: case report and literature review. Am J Gastroenterol. 1995;90:2063-2064. [PubMed] |
| 2. | Kumar N, Adam SZ, Goodhartz LA, Hoff FL, Lo AA, Miller FH. Beyond hepatic hemangiomas: the diverse appearances of gastrointestinal and genitourinary hemangiomas. Abdom Imaging. 2015;40:3313-3329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Quentin V, Lermite E, Lebigot J, Marinnes MZ, Arnaud JP, Boyer J. Small bowel cavernous hemangioma: wireless capsule endoscopy diagnosis of a surgical case. Gastrointest Endosc. 2007;65:550-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Rao AB, Pence J, Mirkin DL. Diffuse infantile hemangiomatosis of the ileum presenting with multiple perforations: a case report and review of the literature. J Pediatr Surg. 2010;45:1890-1892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Ruiz AR Jr, Ginsberg AL. Giant mesenteric hemangioma with small intestinal involvement: an unusual cause of recurrent gastrointestinal bleed and review of gastrointestinal hemangiomas. Dig Dis Sci. 1999;44:2545-2551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Ersoy O, Akin E, Demirezer A, Koseoglu H, Balci S, Kiyak G. Cavernous haemangioma of small intestine mimicking gastrointestinal stromal tumour. Arab J Gastroenterol. 2013;14:139-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Gerson LB, Fidler JL, Cave DR, Leighton JA. ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding. Am J Gastroenterol. 2015;110:1265-1287; quiz 1288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 368] [Cited by in RCA: 448] [Article Influence: 44.8] [Reference Citation Analysis (1)] |
| 8. | Willert RP, Chong AK. Multiple cavernous hemangiomas with iron deficiency anemia successfully treated with double-balloon enteroscopy. Gastrointest Endosc. 2008;67:765-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Easler JJ, Papachristou GI. A case of obscure gastrointestinal bleeding. Gastroenterology. 2012;142:700, 1044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Ng EK, Cheung FK, Chiu PW. Blue rubber bleb nevus syndrome: treatment of multiple gastrointestinal hemangiomas with argon plasma coagulator. Dig Endosc. 2009;21:40-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 11. | Wardi J, Shahmurov M, Czerniak A, Avni Y. Clinical challenges and images in GI. Capillary hemangioma of small intestine. Gastroenterology. 2007;132:1656, 2084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Fernandes D, Dionísio I, Neves S, Duarte P. Cavernous hemangioma of small bowel: a rare cause of digestive hemorrhage. Rev Esp Enferm Dig. 2014;106:214-215. [PubMed] |
| 13. | Law WL. Cavernous hemangioma: uncommon cause of obscure gastrointestinal bleeding. J Am Coll Surg. 2007;205:511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Ning S, Zhang Y, Zu Z, Mao X, Mao G. Enteroscopic sclerotherapy in blue rubber bleb nevus syndrome. Pak J Med Sci. 2015;31:226-228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Elias G, Toubia N. Hemangioma of the small intestine presenting with recurrent overt, obscure gastrointestinal bleeding. Clin Gastroenterol Hepatol. 2010;8:A18, A18.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Shibuya T, Osada T, Mitomi H, Takeda T, Nomura O, Nakayama H, Hidaka Y, Mori H, Beppu K, Sakamoto N. Jejunal capillary hemangioma treated by using double-balloon endoscopy (with video). Gastrointest Endosc. 2010;72:660-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Igawa A, Oka S, Tanaka S, Kunihara S, Nakano M, Chayama K. Polidocanol injection therapy for small-bowel hemangioma by using double-balloon endoscopy. Gastrointest Endosc. 2016;84:163-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 18. | Takase N, Fukui K, Tani T, Nishimura T, Tanaka T, Harada N, Ueno K, Takamatsu M, Nishizawa A, Okamura A. Preoperative detection and localization of small bowel hemangioma: Two case reports. World J Gastroenterol. 2017;23:3752-3757. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Akazawa Y, Hiramatsu K, Nosaka T, Saito Y, Ozaki Y, Takahashi K, Naito T, Ofuji K, Matsuda H, Ohtani M. Preoperative diagnosis of cavernous hemangioma presenting with melena using wireless capsule endoscopy of the small intestine. Endosc Int Open. 2016;4:E249-E251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Chen CH, Jones J, McGowan P. Profound iron deficiency anemia caused by a small-intestinal cavernous hemangioma. Gastrointest Endosc. 2009;69:1392-1393; discussion 1393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Dhumane P, Mutter D, D’Agostino J, Mavrogenis G, Leroy J, Marescaux J. Small bowel exploration and resection using single-port surgery: a safe and feasible approach. Colorectal Dis. 2013;15:109-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Bae SJ, Hwang G, Kang HS, Song HJ, Chang WY, Maeng YH, Kang KS. Single Cavernous Hemangioma of the Small Bowel Diagnosed by Using Capsule Endoscopy in a Child with Chronic Iron-Deficiency Anemia. Clin Endosc. 2015;48:340-344. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Huber A, Abdel Samie A, Kychenko D, Theilmann L. A rare cause of recurrent iron-deficiency anemia: cavernous hemangioma of the small intestine. J Gastrointestin Liver Dis. 2012;21:343. [PubMed] |
| 24. | Khurana V, Dala R, Barkin JS. Small bowel cavernous hemangioma. Gastrointest Endosc. 2004;60:96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Pera M, Márquez L, Dedeu JM, Sánchez J, Garcia M, Ramón JM, Puigvehí M. Solitary cavernous hemangioma of the small intestine as the cause of long-standing iron deficiency anemia. J Gastrointest Surg. 2012;16:2288-2290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 26. | Pinho R, Rodrigues A, Proença L, Silva AP, Fernandes S, Leite S, Amaral I, de Sousa P, Fraga J. Solitary hemangioma of the small bowel disclosed by wireless capsule endoscopy. Gastroenterol Clin Biol. 2008;32:15-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Magnano A, Privitera A, Calogero G, Nanfito’ L, Basile G, Sanfilippo G. Solitary hemangioma of the small intestine: an unusual cause of bleeding diagnosed at capsule endoscopy. J Pediatr Surg. 2005;40:e25-e27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 28. | Kuo LW, Chuang HW, Chen YC. Small bowel cavernous hemangioma complicated with intussusception: report of an extremely rare case and review of literature. Indian J Surg. 2015;77:123-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 29. | Guardiola A, Navajas J, Valle J, López-Pardo R, Rodríguez-Merlo R, Lombera Mdel M, Alcántara M. Small bowel giant cavernous hemangioma diagnosed by capsule endoscopy. Rev Esp Enferm Dig. 2012;104:277-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Purdy-Payne EK, Miner JF, Foles B, Tran TA. The “Endothelialized Muscularis Mucosae”: A Case Report Describing a Large Cavernous Hemangioma at the Terminal Ileum and a New Histologic Clue for Preoperative Diagnosis from Endoscopic Biopsy. Case Rep Gastrointest Med. 2015;2015:454836. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |