Published online Nov 15, 2018. doi: 10.4251/wjgo.v10.i11.449
Peer-review started: April 17, 2018
First decision: May 17, 2018
Revised: June 25, 2018
Accepted: June 28, 2018
Article in press: June 29, 2018
Published online: November 15, 2018
Processing time: 213 Days and 3.7 Hours
To compare outcomes in patients undergoing rectal resection by robotic total meso-rectal excision (RTME) vs laparoscopic total meso-rectal excision (LTME).
Standard medical electronic databases such as PubMed, MEDLINE, EMBASE and Scopus were searched to find relevant articles. The data retrieved from all types of included published comparative trials in patients undergoing RTME vs LTME was analysed using the principles of meta-analysis. The operative, post-operative and oncological outcomes were evaluated to assess the effectiveness of both techniques of TME. The summated outcome of continuous variables was expressed as standardized mean difference (SMD) and dichotomous data was presented in odds ratio (OR).
One RCT (ROLARR trial) and 27 other comparative studies reporting the non-oncological and oncological outcomes following RTME vs LTME were included in this review. In the random effects model analysis using the statistical software Review Manager 5.3, the RTME was associated with longer operation time (SMD, 0.46; 95%CI: 0.25, 0.67; z = 4.33; P = 0.0001), early passage of first flatus (P = 0.002), lower risk of conversion (P = 0.00001) and shorter hospitalization (P = 0.01). The statistical equivalence was seen between RTME and LTME for non-oncological variables like blood loss, morbidity, mortality and re-operation risk. The oncological variables such as recurrence (P = 0.96), number of harvested nodes (P = 0.49) and positive circumferential resection margin risk (P = 0.53) were also comparable in both groups. The length of distal resection margins was similar in both groups.
RTME is feasible and oncologically safe but failed to demonstrate any superiority over LTME for many surgical outcomes except early passage of flatus, lower risk of conversion and shorter hospitalization.
Core tip: The findings of this meta-analysis of one RCT and 27 case control studies on 5547 patients are consistent with the recently published ROLARR trial validating the feasibility and oncological safety of robotic total meso-rectal excision (RTME). However, RTME failed to demonstrate any superiority over laparoscopic total meso-rectal excision except reduced conversion rate.
- Citation: Jones K, Qassem MG, Sains P, Baig MK, Sajid MS. Robotic total meso-rectal excision for rectal cancer: A systematic review following the publication of the ROLARR trial. World J Gastrointest Oncol 2018; 10(11): 449-464
- URL: https://www.wjgnet.com/1948-5204/full/v10/i11/449.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v10.i11.449
Colorectal cancer has higher prevalence rate in the developed world and almost one third of cancers are diagnosed in the rectum[1-4]. Total mesorectal excision (TME) performed either by open or laparoscopic technique is an accepted gold standard treatment of rectal cancer worldwide. Laparoscopic TME (LTME) has apparent advantages and considered a preferred mode of surgery due to less tissue trauma[5-11]. Due to precision in dissection, stable base unit and better visualization in difficult areas like lower pelvis, the robotic TME (RTME) is also considered a possible alternative to LTME[12,13]. RTME may potentially offer same advantages which LTME offers as reported in some studies. There have been several previous systematic reviews[14-21] on LTME vs RTME; however, none since the ROLARR trial, a multi-centre randomised controlled trial comparing RTME to LTME, has published its results. In addition, several new comparative studies have also been reported which require combined statistical evaluation to generate up to date and better evidence.
Our study is an up to date meta-analysis of studies comparing RTME vs LTME including recently published ROLARR trial to be able to distinguish the potential advantages or disadvantages that robotics may play in the treatment of rectal cancer.
Following are features of individual publications needed to qualify for inclusion in this systematic review as depicted in the following PICOS style: (1) Participants: Adult patients with histologically proven and MDT recommended resectable rectal cancer; (2) Intervention (Exposure): RTME; (3) Control: Patients with rectal cancer undergoing TME or rectal resection by laparoscopic approach; (4) Outcomes: Length of stay, operation time, blood loss, post-operative complications, mortality, positive circumferential resection margins, length of distal resection margins, lymph node harvesting, surgical site infections, time till first flatus, conversion rate, tumour recurrence and re-operation rate; (5) Study design: No restrictions were placed in study design. However, published studies should have reported comparison between two arms, those are RTME vs LTME. No studies were excluded based on the year of publication, publication centre, age or gender of the participants or publication language.
Four databases: PubMed, Ovid EMBASE, SCOPUS, and Cochrane Library were searched to find target studies. Four trial registries: ClinicalTrials.gov, European Clinical Trials Register, ISRCTN Register, and the International Clinical Trials Registry were examined. The literature exploration was performed until March 2018.
For PubMed, the search was run by means of using MeSH words and by utilizing advanced search choice. The MeSH words “rectal cancer”, AND (“laparoscopic resection OR minimal invasive surgery resection OR robotic surgery resection OR total meso-rectal excision”) were used. Furthermore, an advanced study exploration was done using the terms “rectal resection”. Ovid, EMBASE and SCOPUS were searched with the same search terms as the PubMed advanced search. The Cochrane Library was searched using the term “rectal cancer”. Trial registries were all examined using the word “rectal cancer”.
Two authors evaluated and studied initially titles and then abstracts, adding any curtained references into the Excel spreadsheet. The duplicate articles were excluded. Based upon the information given in the published abstracts, the initial decision of study inclusion or exclusion was made. The published article of the potentially includable studies was then evaluated. The conflicts about data, its accuracy and variability among extracting authors was sorted by agreement or by intercession of an experienced supervising consultant surgeon with had vast clinical and publication experience.
Data was independently collected by two reviewers into the electronic data collection forms of the Microsoft Excel spread sheet. The data items were agreed by the authors prior to commencing study selection. The data pertaining to the analysable outcomes was extracted in addition to the study citation, ethics committee approval, study registration and study quality indicators for all types of comparative studies. Once each author had completed data extraction, the data files were electronically compared and discrepancies in data entry were investigated and resolved.
The comparative efficacy of robotic surgery and conventional laparoscopic surgery for rectal resection was directly matched and pooled for each outcome of interest if there were at least two studies for each comparison. The odds ratio (OR) was estimated and pooled across studies using a random-effect model. Heterogeneity was assessed using Cochrane Q test and I2 statistic. The statistical analysis of the data was conducted according to the guidelines provided by the Cochrane Collaboration including the use of RevMan 5.3® statistical software, and the use of forest plots for the graphical display of the combined outcomes[22-28].
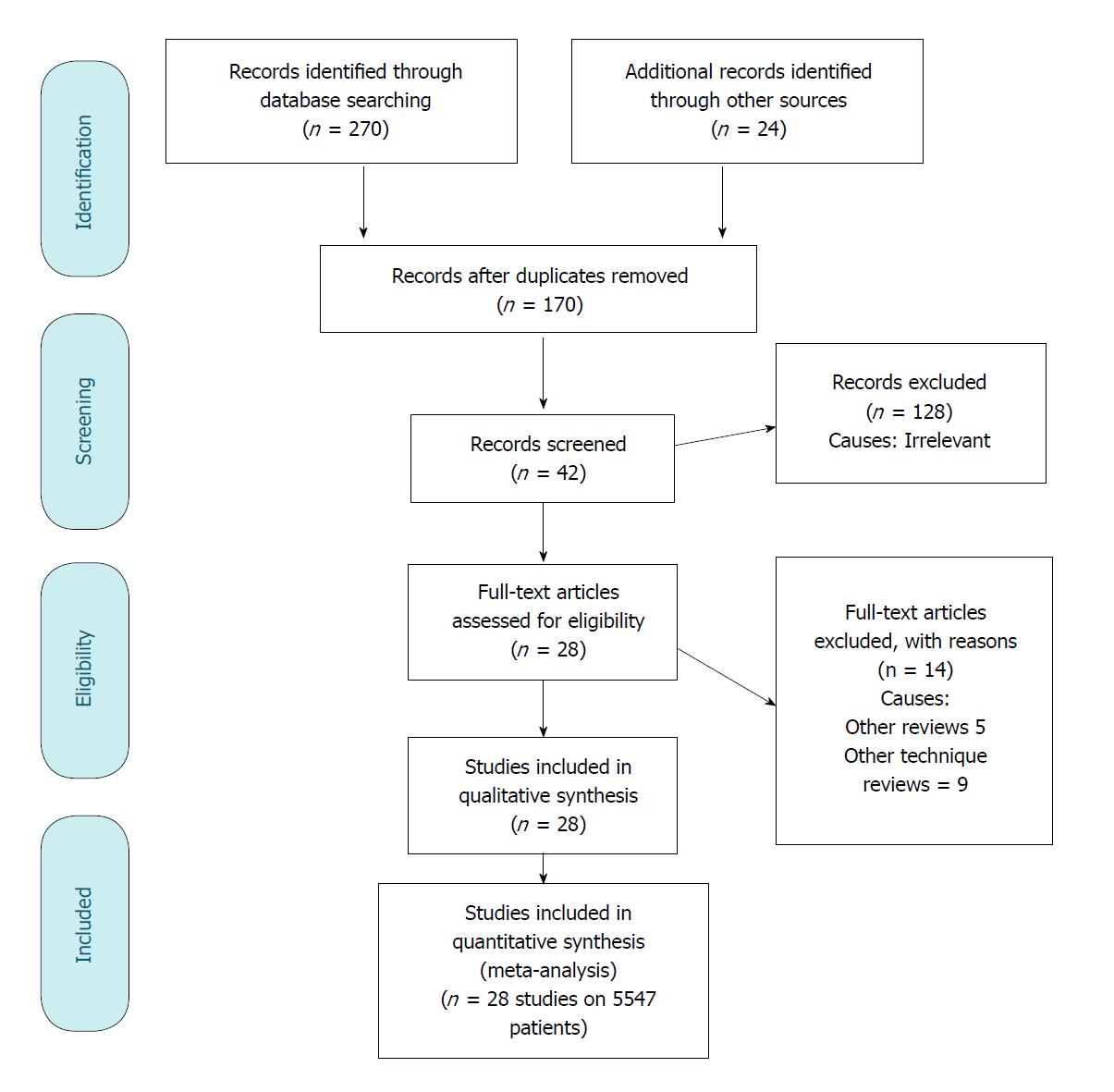
A total of 294 studies were identified from Scopus and MEDLINE and other standard medical electronic databases. Among them, 1 RCT and 27 non-randomized comparative (both retrospective and prospective case control) studies[29-56] published until March 2018, were eligible for inclusion. The inclusion and exclusion pathway is described in PRISMA flow chart Figure 1.
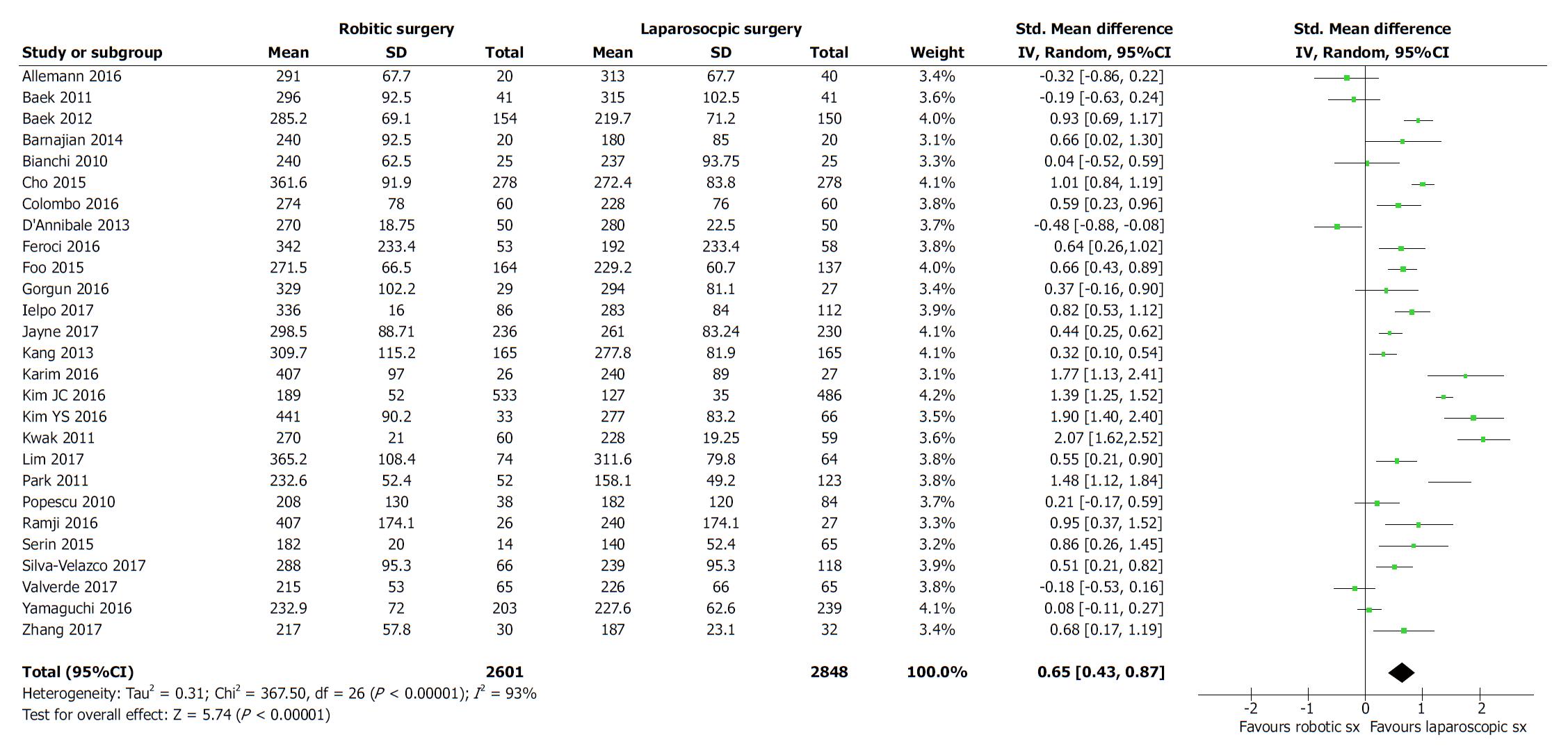
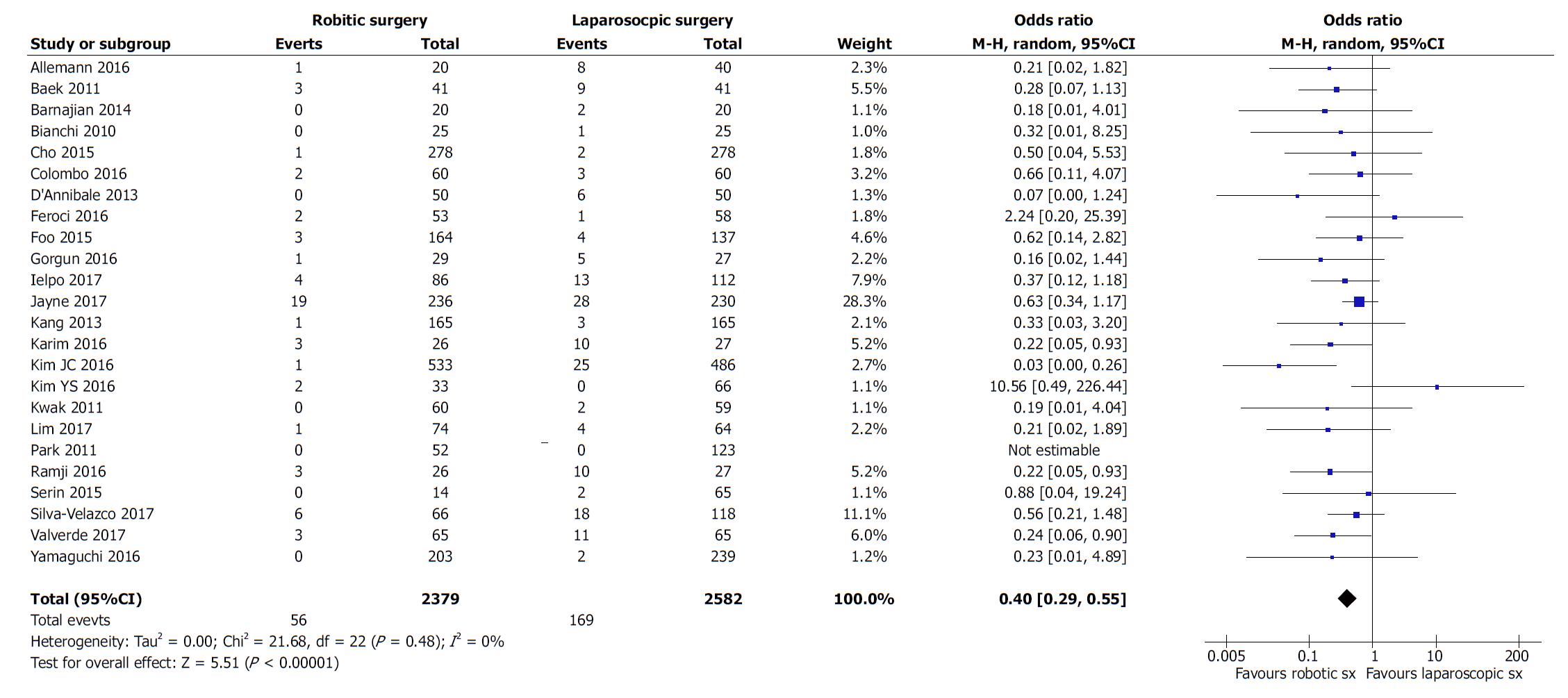
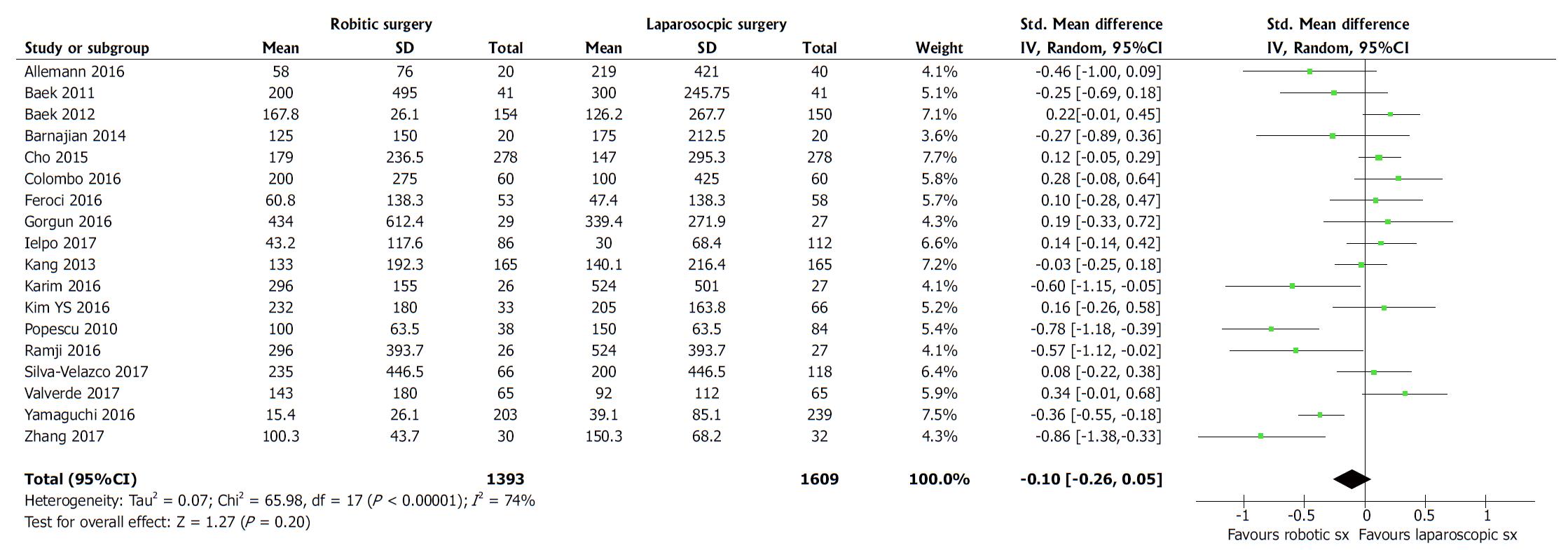
All studies evaluated and reported the outcome of duration of operation. The duration of operation was longer (SMD, 0.20; 95%CI: -0.11, 0.52; z = 1.28; P = 0.20; Figure 2) in robotic surgery group, but with the clinical advantage of the reduced rate of conversion (OR, 0.40; 95%CI: 0.29, 0.55; z = 5.51; P = 0.00001; Figure 3) to open surgery. The reduced risk of conversion to laparotomy following RTME seems to be significantly advantageous in terms of the intensity of surgical trauma posed by laparotomy. There was similar risk of blood loss (SMD, 0.09; 95%CI: -0.14, 0.33; z = 0.76; P = 0.45; Figure 4) following both approaches of TME. Clinical and methodological heterogeneity [Tau2 = 0.31, χ2 = 367.50, df = 26, (P < 0.00001); I2 = 93%] was noted in trials which was the basis for the random effects model analysis leading to the above outcomes.
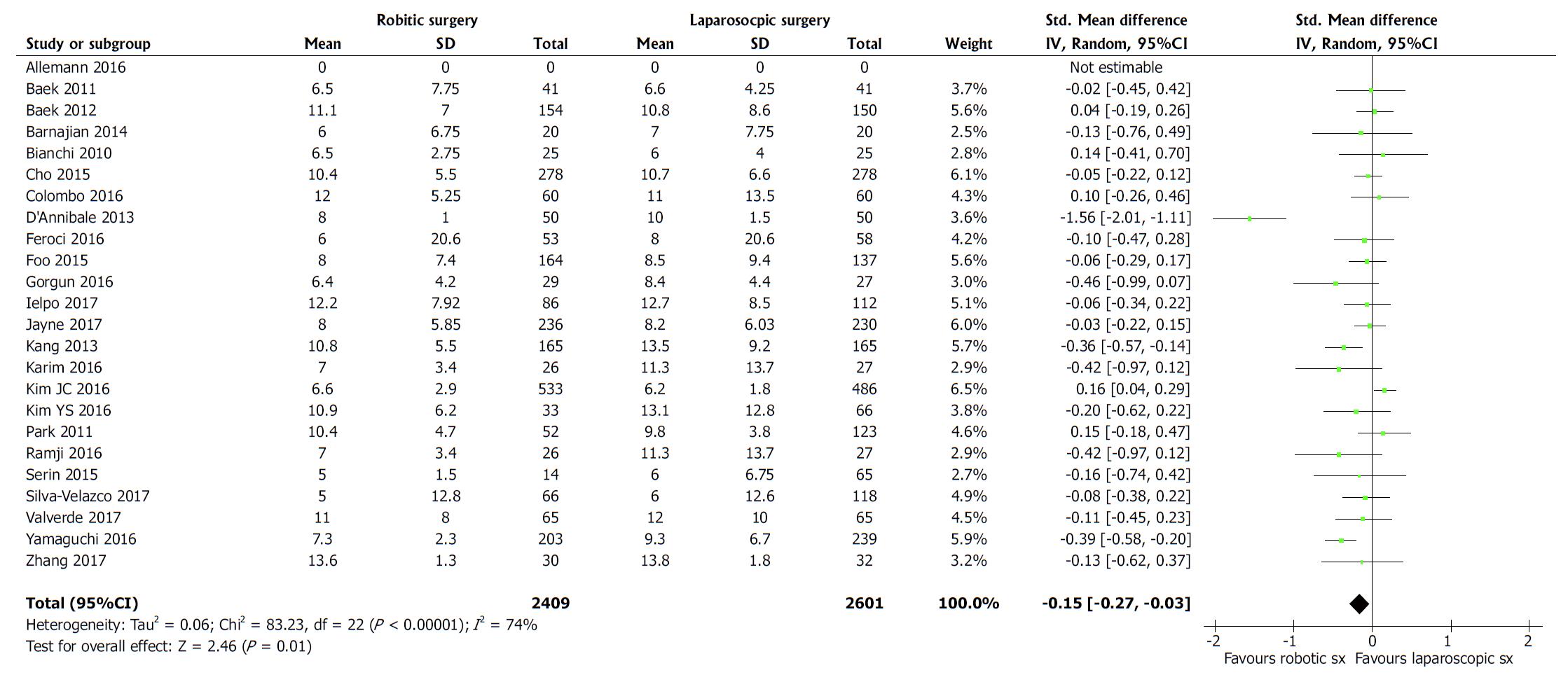
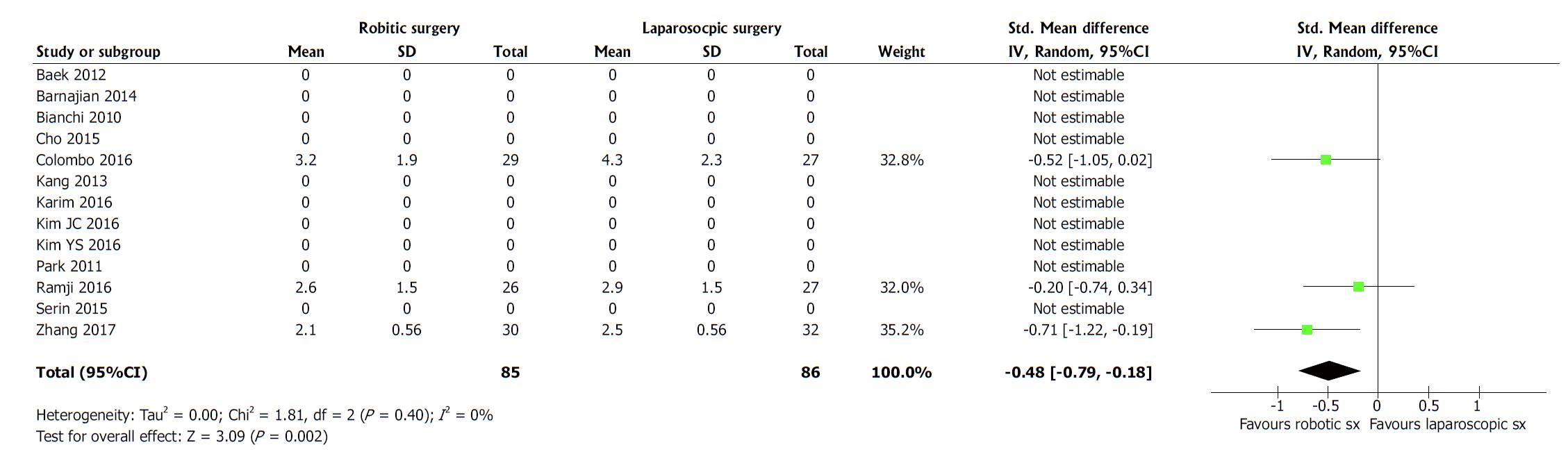
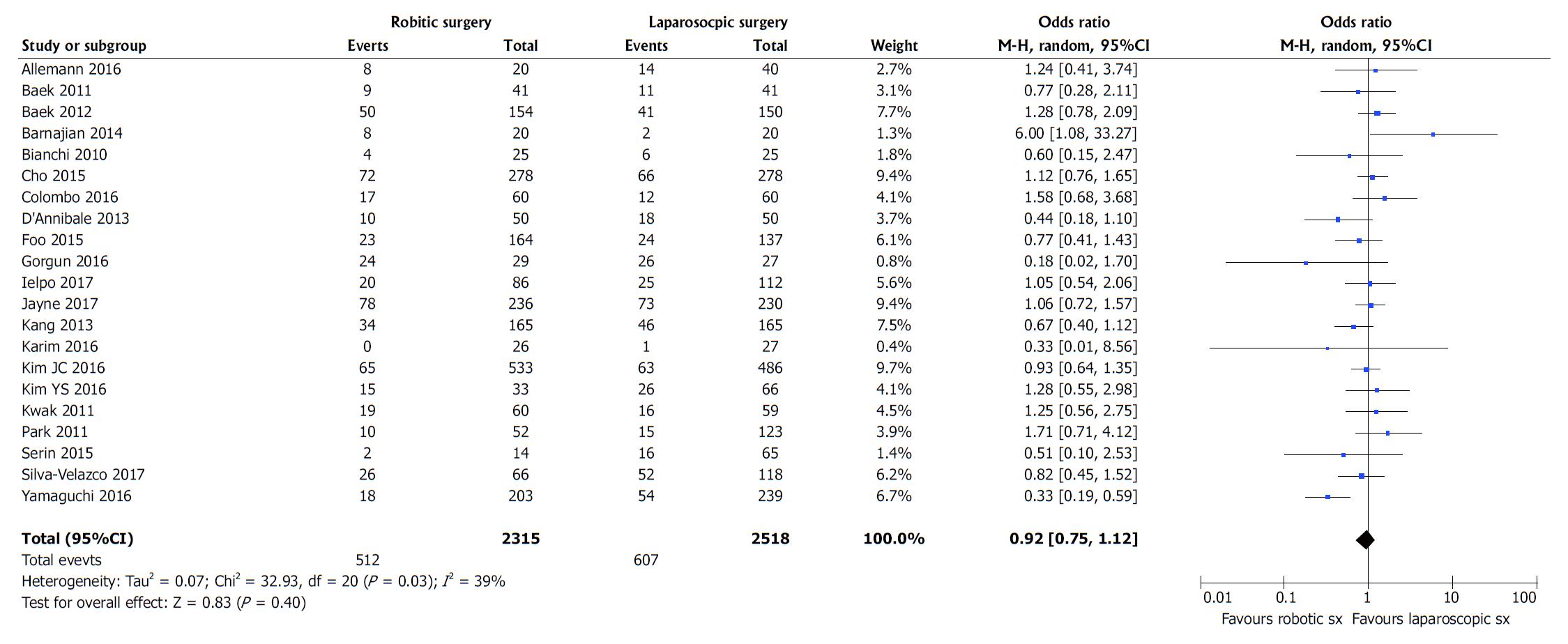
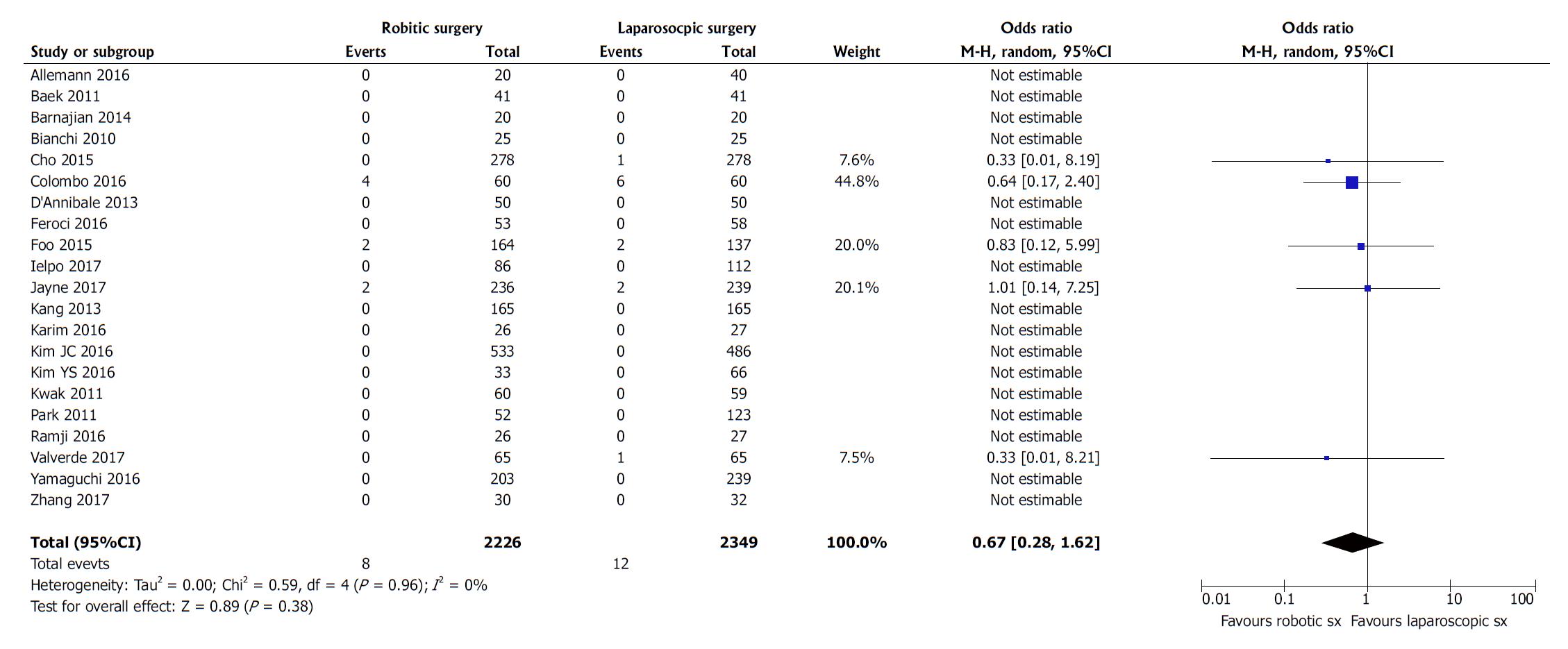
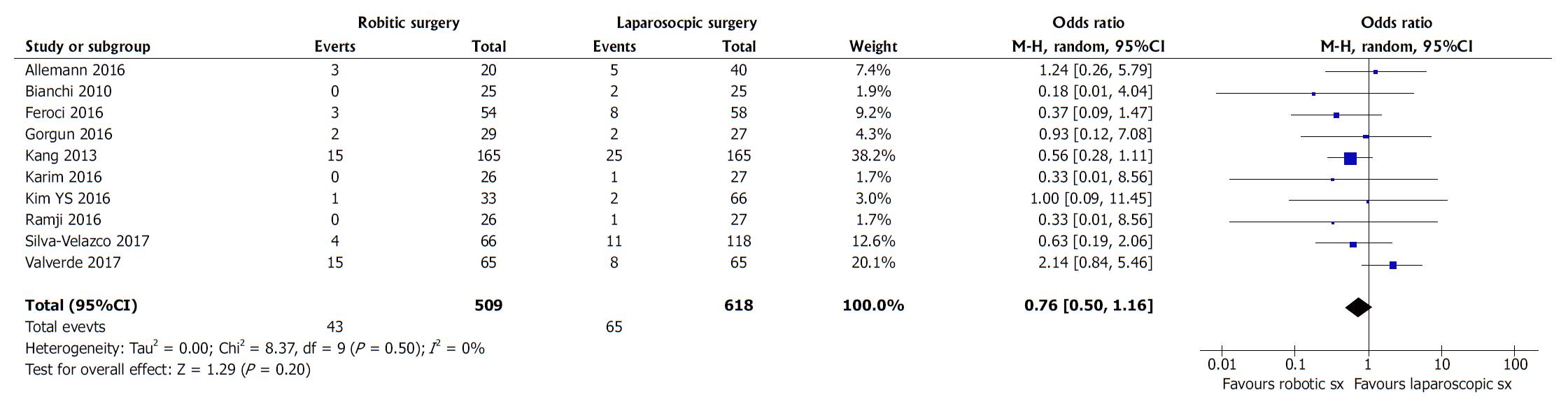
The in-hospital stay (SMD, -0.15; 95%CI: -0.27, -0.03; z = 2.46; P = 0.01; Figure 5) and time to first flatus (SMD, -0.48; 95%CI: -0.79, -0.18; z = 3.09; P = 0.002; Figure 6) in patients undergoing RTME were shorter compared to LTME group. However, the post-operative morbidity (OR, 0.92; 95%CI: 0.75, 01.12; z = 0.83; P = 0.40; Figure 7), post-operative mortality (OR, 0.67; 95%CI: 0.28, 1.62; z = 0.89; P = 0.38; Figure 8) and re-operation rate (OR, 0.76; 95%CI: 0.50, 1.16; z = 1.29; P = 0.20; Figure 9) were statistically similar in both groups.
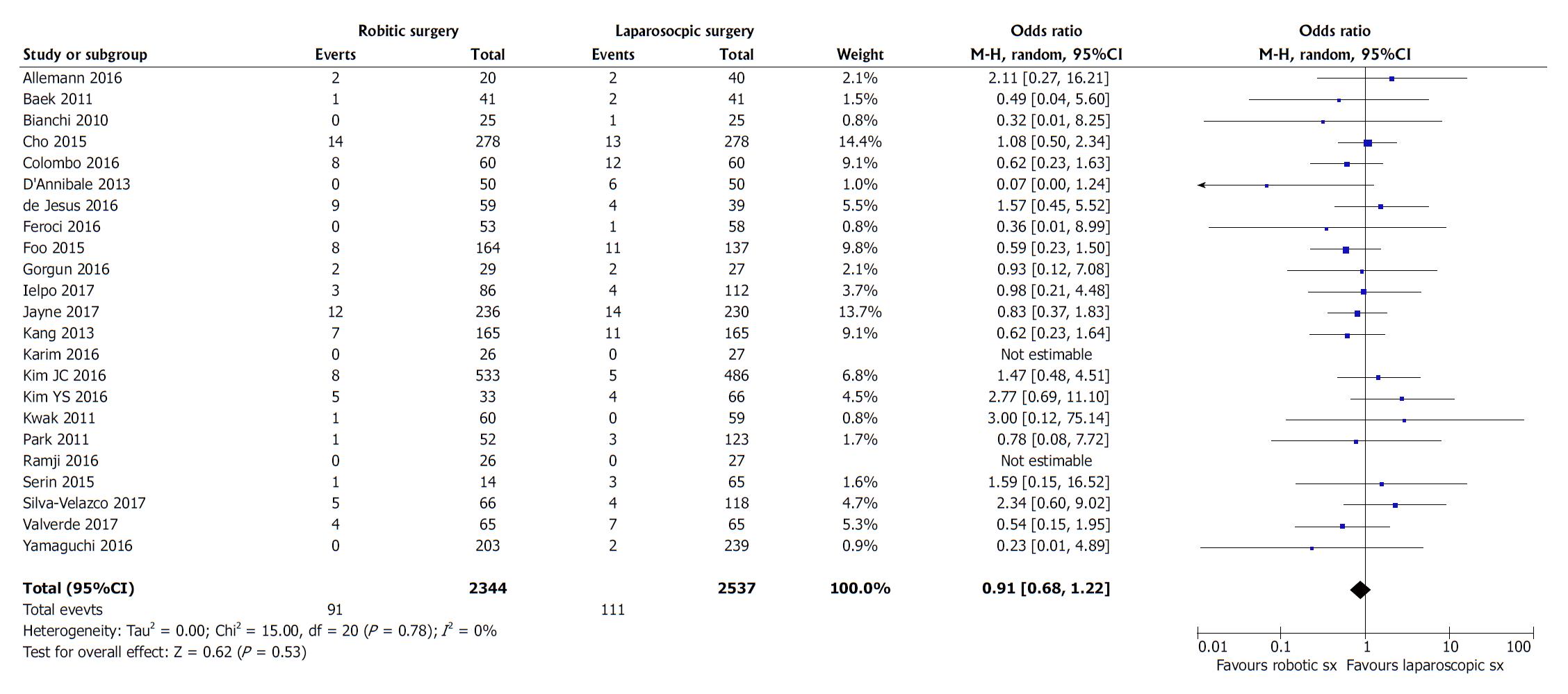
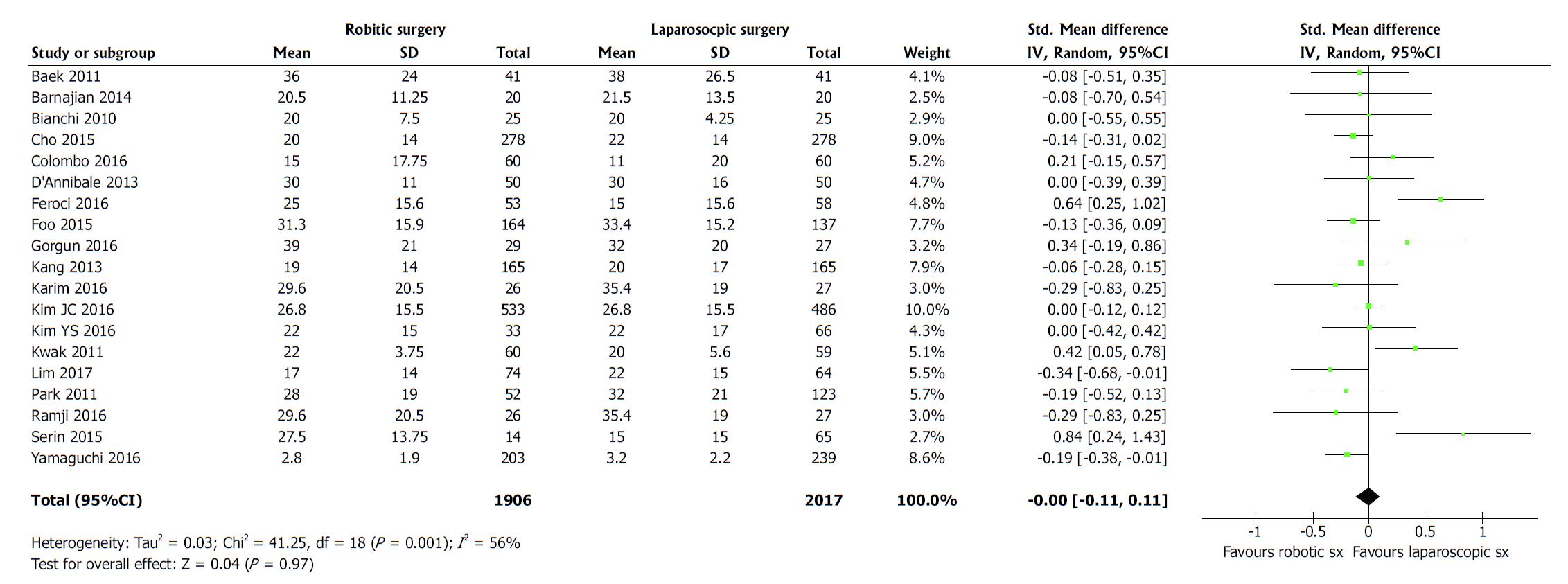
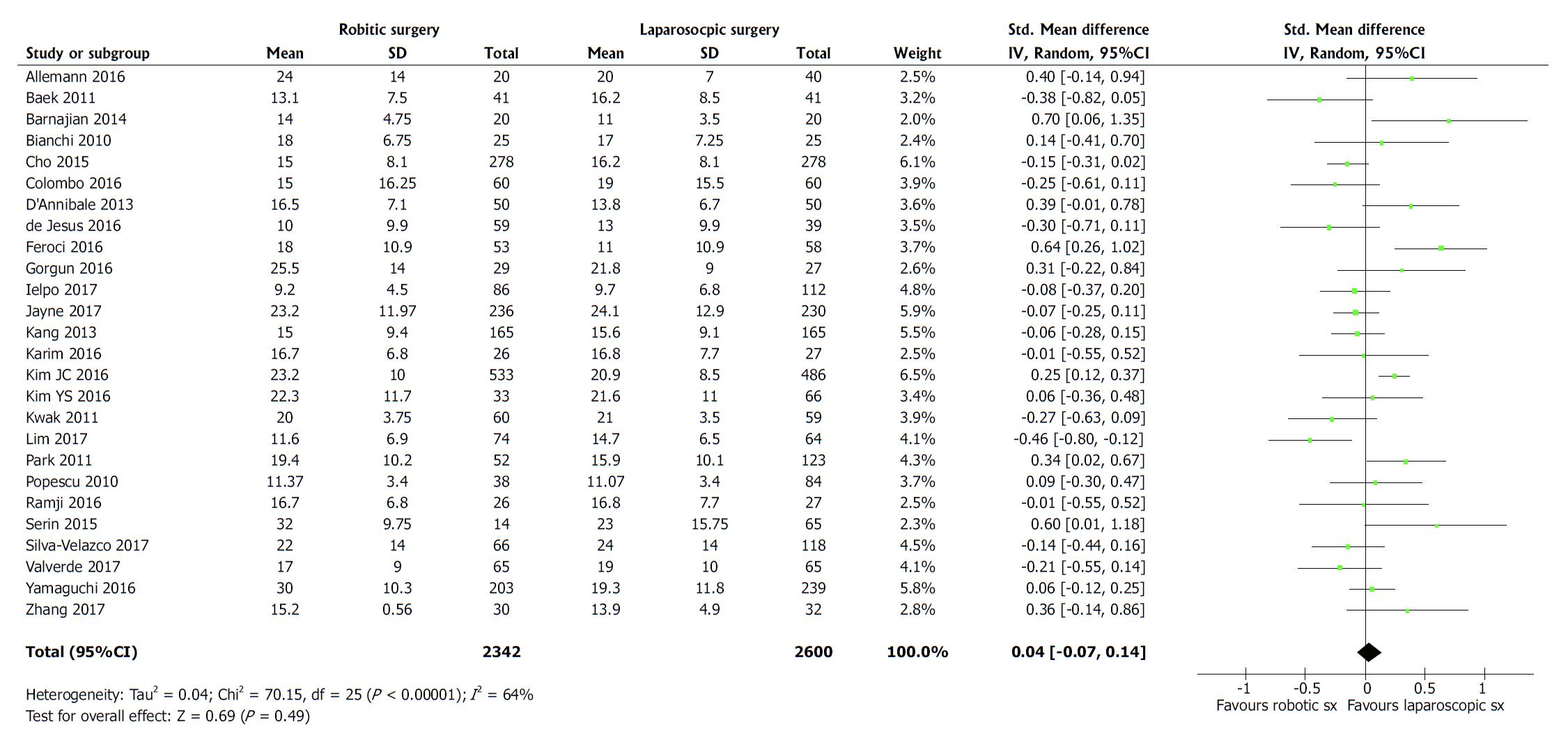
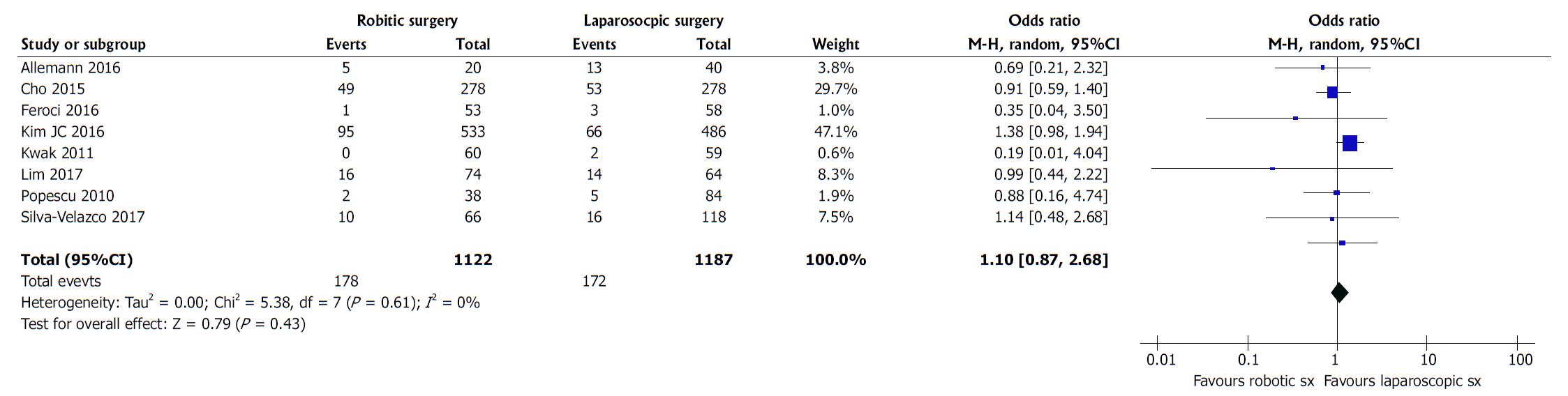
Oncological safety is one of the most important surgical outcomes for any new surgical intervention because positive circumferential resection margins are directly associated with overall survival and disease free survival in rectal cancer patients. The risk of positive circumferential resection margins (OR, 0.91; 95%CI: 0.68, 1.22; z = 0.62; P = 0.53; Figure 10), length of distal resection margins (SMD, 0.00; 95%CI: -0.11, 0.11; z = 0.04; P = 0.97; Figure 11), and lymph node yield (SMD, 0.04; 95%CI: -0.07, 0.14; z = 0.69; P = 0.49; Figure 12) were statistically similar in both groups. Therefore, the risk of local and distant recurrence (OR, 1.10; 95%CI: 0.87, 1.39; z = 0.79; P = 0.43; Figure 13) was also found to be similar in both groups.
Colorectal cancer is the third most common cancer diagnosis internationally. The highest incidence of colorectal cancer is reported the Europe, North America and Australia[1]. The highest incidence of colorectal cancer is in the anatomical area of rectum. In 2015 in the United Kingdom out of 41599 people diagnosed with colorectal cancer, 27% of these were located in the rectum. The incidence is slightly higher in men making up 32% of all colorectal cancer diagnoses compared to 23% for women[2]. With the introduction of the total meso-rectal excision (TME), developed in 1989 by Professor Heald, survival rates and the rates of local recurrence have significantly improved[3,4]. A TME is defined as an en bloc resection of the rectal tumour with endo-pelvic fascia to excise circumferential margins[5]. The decision to undertake a TME is influenced by several factors including distance of the cancer from the anal verge, degree of invasion into the pelvic walls, presence of metastases to regional lymph nodes, the patient’s co-morbidities and the ability to withstand trans-abdominal surgery[6]. LTME has risen to become the gold standard for rectal cancer suitable for surgical resection[7]. Many trials including the COLOR II trial established that it gave similar oncological outcomes compared to an open approach[8,9] and further studies showed it resulted in shorter length of stay, less pain and quicker resumption of normal diet[10,11]. The main reason behind these proven advantages of the laparoscopic TME is the reduced surgical trauma and tissue handling compared to open TME. As the use of robotics in surgery becomes more commonplace in gynaecological and urological procedures, the question arises on whether it has a place in colorectal surgery. Specifically, a TME demands precise dissection in an area that is difficult to visualise and access. These difficult aspects of a TME could be improved upon by robotics which offers a direct angle entry view, a stable retraction platform and more movement of instrument freedom[12,13]. Some studies have shown that robotic TME (RTME) results in shorter length of stay, whilst other studies have shown that there is no difference in hospital stay, oncological outcomes or rates of converting procedures to open. There is an argument that in terms of cost, the use of robotics is more expensive than laparoscopic instruments and the learning curve for surgeons is longer and requires more cases than for a LTME.
Based upon the findings of this largest ever series on the role of robotic surgery in rectal cancer resection, the RTME is certainly a feasible technique and oncologically safe surgical intervention but failed to demonstrate any superiority over LTME for many surgical outcomes. Mere advantage of robotic surgery was noted in only three post-operative outcomes, that is early passage of flatus, lower risk of conversion and shorter hospitalization. It seems like these advantages may not truly reflect into the routine use of RTME in rectal cancer surgery and therefore, the examination of current 28 studies to date did not designate a major value of RTME over LTME. Demonstration of this conclusion has already been reported in previously published meta-analyses[14-21,57].
These findings needs further evaluation on the background of recently published ROLARR[42] trial. Among operative outcomes, current study indicates similar blood loss and longer duration of operation and these both outcomes are concordant with the findings of ROLARR[42] trial. The risk of conversion to open surgery was found to be lower in RTME arm of current study. Similarly the risk of conversion was lower in RTME group (8.1%) compared to LTME group (12.2%) in the ROLARR[42] trial but statistically it failed to demonstrate any significance. The length of hospital stay was similar between both groups in the ROLARR[42] trial but current study shows significant reduction in the hospitalization time in patients undergoing RTME. Post-operative mortality, morbidity and re-operation rate were consistently similar in all included studies, current study and in the ROLARR[42] trial. The oncological outcomes such as positive circumferential resection margins, length of distal resection margins, lymph node yield and recurrence rate were also not different. The publication of the ROLARR[42] trials has answered several questions about the feasibility, safety and comparative equivalence of RTME and non-inferiority of LTME too. In addition, RTME seems to be relatively expensive[29,42,58,59] and less cost-effective procedure and therefore routine use of this approach may not be justified for TME.
Authors frankly accept the major limitations of this study and the most apparent is the combined analysis of an RCT[42] and 27 case control studies. Despite this limitation, the outcomes are almost matching with the conclusions of the only RCT[42] published on this subject. Other confounding factors which can potentially be influencing the final outcome are diverse inclusion and exclusion criteria among included studies; variable post-operative follow up duration; lack of an agreed follow up screening pathways; presence and absence of the use of neoadjuvant chemoradiotherapy in the recruited population; use of variable diagnostic pathways in included studies and variable experience of the operating surgeons especially in the RTME group. More RCTs are needed to consolidate the findings of ROLARR trial[42] and current study. Better outcomes and reduced cost may be anticipated in future trials due to the use of cost effective advanced technology and operating surgeons with extensive experience in robotic surgery. Until then the ROLARR trial and current study may provide the best possible evidence in this relatively innovative intervention for rectal cancer management.
Robotic total meso-rectal excision (TME) is used at least for a decade to treat rectal cancer and the only evidence in favour of robotic TME was based on case control studies. Recently first ever RCT evaluating feasibility of robotic TME was published as ROLARR trial. This aims of this study was to strengthen the existing evidence on this technique which is mainly based upon the meta-analysis of case control studies and compare it with the results of ROLARR trial.
Although robotic TME is being presented a way forward for rectal resection but its superiority over laparoscopic TME is not proven yet. Most of the evidence was based upon the systematic review of case-controlled studies, the publication of ROLARR trial is an attempt to answer this question. Comparison between the findings of ROLARR trial and systematic review of case-controlled trials can guide the surgeons in future about role of robotic TME.
The objective of this systematic review is to strengthen the existing evidence on the role of robotics for TME technique which is mainly based upon the meta-analysis of case control studies and compare it with the results of recently published ROLARR trial reporting robotic TME vs laparoscopic TME.
Standard medical databases were searched. RCTs and all types of comparative studies reporting the effectiveness of robotic TME vs laparoscopic TME in the management of rectal cancer were retrieved and their data was extracted. The extracted data was analyzed using the principles of meta-analysis to generate higher level of evidence. RevMan 5.3 was used for statistical analysis and GradePro was used to generate summary of evidence.
One RCT (ROLARR trial) and 27 other comparative studies reporting the non-oncological and oncological outcomes following robotic TME vs laparoscopic TME were included in this review. In the random effects model analysis using the statistical software Review Manager 5.3, the RTME was associated with longer operation time (SMD, 0.46; 95%CI: 0.25, 0.67; z = 4.33; P = 0.0001), early passage of first flatus (P = 0.002), lower risk of conversion (P = 0.00001) and shorter hospitalization (P = 0.01). The statistical equivalence was seen between robotic TME and laparoscopic TME for non-oncological variables like blood loss, morbidity, mortality and re-operation risk. The oncological variables such as recurrence (P = 0.96), number of harvested nodes (P = 0.49) and positive circumferential resection margin risk (P = 0.53) were also comparable in both groups. The length of distal resection margins was similar in both groups.
Robotic TME is feasible and oncologically safe but failed to demonstrate any superiority over laparoscopic TME for many surgical outcomes except early passage of flatus, lower risk of conversion, lower conversion to laparotomy rate and shorter hospitalization.
Robotic TME failed to demonstrate superiority over laparoscopic TME. Laparoscopic TME may continuously be used to treat rectal cancer. More RCTs are needed to consolidate the findings of ROLARR trial [42] and current study. Better outcomes and reduced cost may be anticipated in future trials due to the use of cost effective advanced technology and operating surgeons with extensive experience in robotic surgery. Until then the ROLARR trial and current study may provide the best possible evidence in this relatively innovative intervention for rectal cancer management.
Manuscript source: Invited manuscript
Specialty type: Oncology
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Freha NA, Mastoraki A S- Editor: Ji FF L- Editor: A E- Editor: Tan WW
| 1. | American Cancer Society. Key Statistics for Colorectal Cancer. Accessed on. 2018;Aug 3 Available from: https://www.cancer.org/cancer/colon-rectal-cancer/about/key-statistics.html. |
| 2. | Cancer Research UK. Cancer incidence statistics. Available from: http://www.cancerresearchuk.org/health-professional/cancer-statistics/incidence. |
| 3. | Heald RJ, Ryall RD. Recurrence and survival after total mesorectal excision for rectal cancer. Lancet. 1986;1:1479-1482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1867] [Cited by in RCA: 1914] [Article Influence: 49.1] [Reference Citation Analysis (0)] |
| 4. | Maurer CA, Renzulli P, Kull C, Käser SA, Mazzucchelli L, Ulrich A, Büchler MW. The impact of the introduction of total mesorectal excision on local recurrence rate and survival in rectal cancer: long-term results. Ann Surg Oncol. 2011;18:1899-1906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 81] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 5. | Rodríguez-Luna MR, Guarneros-Zárate JE, Tueme-Izaguirre J. Total Mesorectal Excision, an erroneous anatomical term for the gold standard in rectal cancer treatment. Int J Surg. 2015;23:97-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Monson JR, Weiser MR, Buie WD, Chang GJ, Rafferty JF, Buie WD, Rafferty J; Standards Practice Task Force of the American Society of Colon and Rectal Surgeons. Practice parameters for the management of rectal cancer (revised). Dis Colon Rectum. 2013;56:535-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 301] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 7. | Moran B, Karandikar S, Geh I. Association of Coloproctology of Great Britain & Ireland (ACPGBI): Guidelines for the Management of Cancer of the Colon, Rectum and Anus (2017) - Introduction. Colorectal Dis. 2017;19 Suppl 1:6-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MH, de Lange-de Klerk ES, Lacy AM, Bemelman WA, Andersson J, Angenete E. A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med. 2015;372:1324-1332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 864] [Cited by in RCA: 930] [Article Influence: 93.0] [Reference Citation Analysis (0)] |
| 9. | Green BL, Marshall HC, Collinson F, Quirke P, Guillou P, Jayne DG, Brown JM. Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg. 2013;100:75-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 483] [Cited by in RCA: 497] [Article Influence: 38.2] [Reference Citation Analysis (0)] |
| 10. | Kennedy RH, Francis EA, Wharton R, Blazeby JM, Quirke P, West NP, Dutton SJ. Multicenter randomized controlled trial of conventional versus laparoscopic surgery for colorectal cancer within an enhanced recovery programme: EnROL. J Clin Oncol. 2014;32:1804-1811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 158] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 11. | Chen W, Li Q, Qiu P, Jiang L, Fu Z, Fan Y, Li D, Liu P, Tang L. Comparison of perioperative outcomes between laparoscopic and open surgery for mid-low rectal cancer with total mesorectal excision following neoadjuvant chemoradiotherapy. J Cancer Res Ther. 2016;12:C199-C204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 12. | Mohd Azman ZA, Kim SH. A review on robotic surgery in rectal cancer. Transl Gastroenterol Hepatol. 2016;1:5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Weaver KL, Grimm LM Jr, Fleshman JW. Changing the Way We Manage Rectal Cancer-Standardizing TME from Open to Robotic (Including Laparoscopic). Clin Colon Rectal Surg. 2015;28:28-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Cheong C, Kim NK. Minimally Invasive Surgery for Rectal Cancer: Current Status and Future Perspectives. Indian J Surg Oncol. 2017;8:591-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Trastulli S, Cirocchi R, Listorti C, Cavaliere D, Avenia N, Gullà N, Giustozzi G, Sciannameo F, Noya G, Boselli C. Laparoscopic vs open resection for rectal cancer: a meta-analysis of randomized clinical trials. Colorectal Dis. 2012;14:e277-e296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 119] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 16. | Hu L, Yao L, Li X, Jin P, Yang K, Guo T. Effectiveness and safety of robotic-assisted versus laparoscopic hepatectomy for liver neoplasms: A meta-analysis of retrospective studies. Asian J Surg. 2017;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 17. | Li X, Wang T, Yao L, Hu L, Jin P, Guo T, Yang K. The safety and effectiveness of robot-assisted versus laparoscopic TME in patients with rectal cancer: A meta-analysis and systematic review. Medicine (Baltimore). 2017;96:e7585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 18. | Xiong B, Ma L, Huang W, Zhao Q, Cheng Y, Liu J. Robotic versus laparoscopic total mesorectal excision for rectal cancer: a meta-analysis of eight studies. J Gastrointest Surg. 2015;19:516-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 113] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 19. | Wang Y, Zhao GH, Yang H, Lin J. A Pooled Analysis of Robotic Versus Laparoscopic Surgery for Total Mesorectal Excision for Rectal Cancer. Surg Laparosc Endosc Percutan Tech. 2016;26:259-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 20. | Ortiz-Oshiro E, Sánchez-Egido I, Moreno-Sierra J, Pérez CF, Díaz JS, Fernández-Represa JÁ. Robotic assistance may reduce conversion to open in rectal carcinoma laparoscopic surgery: systematic review and meta-analysis. Int J Med Robot. 2012;8:360-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 21. | Broholm M, Pommergaard HC, Gögenür I. Possible benefits of robot-assisted rectal cancer surgery regarding urological and sexual dysfunction: a systematic review and meta-analysis. Colorectal Dis. 2015;17:375-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 82] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 22. | Higgins JPT, Green S (eds). Cochrane Handbook for Systematic Reviews of Interventions. Available from: http://www.cochrane-handbook.org. |
| 23. | Review Manager (RevMan) [Computer program]. Version 5.0. The Nordic Cochrane Centre, The Cochrane Collaboration: Copenhagen 2008; . |
| 24. | DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26739] [Cited by in RCA: 30401] [Article Influence: 779.5] [Reference Citation Analysis (0)] |
| 25. | Demets DL. Methods for combining randomized clinical trials: strengths and limitations. Stat Med. 1987;6:341-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 854] [Cited by in RCA: 798] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 26. | Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539-1558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21630] [Cited by in RCA: 25779] [Article Influence: 1120.8] [Reference Citation Analysis (0)] |
| 27. | Egger M, Smith GD, Altman DG, editors . Systematic reviews in healthcare. BMJ Publishing, London. 2006;. |
| 28. | Deeks JJ, Altman DG, Bradburn MJ. Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. Systemic reviews in health care: meta-analysis in context. 2nd edn. BMJ Publication group. Editor(s): In: Egger M, Smith GD, Altman DG, editors. London 2001; 285-312. [DOI] [Full Text] |
| 29. | Allemann P, Duvoisin C, Di Mare L, Hübner M, Demartines N, Hahnloser D. Robotic-Assisted Surgery Improves the Quality of Total Mesorectal Excision for Rectal Cancer Compared to Laparoscopy: Results of a Case-Controlled Analysis. World J Surg. 2016;40:1010-1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 30. | Baek SJ, Kim SH, Cho JS, Shin JW, Kim J. Robotic versus conventional laparoscopic surgery for rectal cancer: a cost analysis from a single institute in Korea. World J Surg. 2012;36:2722-2729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 121] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 31. | Baek JH, Pastor C, Pigazzi A. Robotic and laparoscopic total mesorectal excision for rectal cancer: a case-matched study. Surg Endosc. 2011;25:521-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 127] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 32. | Barnajian M, Pettet D 3rd, Kazi E, Foppa C, Bergamaschi R. Quality of total mesorectal excision and depth of circumferential resection margin in rectal cancer: a matched comparison of the first 20 robotic cases. Colorectal Dis. 2014;16:603-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 33. | Bianchi PP, Ceriani C, Locatelli A, Spinoglio G, Zampino MG, Sonzogni A, Crosta C, Andreoni B. Robotic versus laparoscopic total mesorectal excision for rectal cancer: a comparative analysis of oncological safety and short-term outcomes. Surg Endosc. 2010;24:2888-2894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 190] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 34. | Cho MS, Baek SJ, Hur H, Min BS, Baik SH, Lee KY, Kim NK. Short and long-term outcomes of robotic versus laparoscopic total mesorectal excision for rectal cancer: a case-matched retrospective study. Medicine (Baltimore). 2015;94:e522. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 103] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 35. | Colombo PE, Bertrand MM, Alline M, Boulay E, Mourregot A, Carrère S, Quénet F, Jarlier M, Rouanet P. Robotic Versus Laparoscopic Total Mesorectal Excision (TME) for Sphincter-Saving Surgery: Is There Any Difference in the Transanal TME Rectal Approach? : A Single-Center Series of 120 Consecutive Patients. Ann Surg Oncol. 2016;23:1594-1600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 36. | D’Annibale A, Pernazza G, Monsellato I, Pende V, Lucandri G, Mazzocchi P, Alfano G. Total mesorectal excision: a comparison of oncological and functional outcomes between robotic and laparoscopic surgery for rectal cancer. Surg Endosc. 2013;27:1887-1895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 192] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 37. | de Jesus JP, Valadão M, de Castro Araujo RO, Cesar D, Linhares E, Iglesias AC. The circumferential resection margins status: A comparison of robotic, laparoscopic and open total mesorectal excision for mid and low rectal cancer. Eur J Surg Oncol. 2016;42:808-812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 38. | Feroci F, Vannucchi A, Bianchi PP, Cantafio S, Garzi A, Formisano G, Scatizzi M. Total mesorectal excision for mid and low rectal cancer: Laparoscopic vs robotic surgery. World J Gastroenterol. 2016;22:3602-3610. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 46] [Cited by in RCA: 61] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 39. | Law WL, Foo DCC. Comparison of short-term and oncologic outcomes of robotic and laparoscopic resection for mid- and distal rectal cancer. Surg Endosc. 2017;31:2798-2807. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 64] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 40. | Gorgun E, Ozben V, Costedio M, Stocchi L, Kalady M, Remzi F. Robotic versus conventional laparoscopic rectal cancer surgery in obese patients. Colorectal Dis. 2016;18:1063-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 41. | Ielpo B, Duran H, Diaz E, Fabra I, Caruso R, Malavé L, Ferri V, Nuñez J, Ruiz-Ocaña A, Jorge E. Robotic versus laparoscopic surgery for rectal cancer: a comparative study of clinical outcomes and costs. Int J Colorectal Dis. 2017;32:1423-1429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 42. | Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J, Quirke P, West N, Rautio T, Thomassen N. Effect of Robotic-Assisted vs Conventional Laparoscopic Surgery on Risk of Conversion to Open Laparotomy Among Patients Undergoing Resection for Rectal Cancer: The ROLARR Randomized Clinical Trial. JAMA. 2017;318:1569-1580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 689] [Cited by in RCA: 919] [Article Influence: 114.9] [Reference Citation Analysis (0)] |
| 43. | Kang J, Yoon KJ, Min BS, Hur H, Baik SH, Kim NK, Lee KY. The impact of robotic surgery for mid and low rectal cancer: a case-matched analysis of a 3-arm comparison--open, laparoscopic, and robotic surgery. Ann Surg. 2013;257:95-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 164] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 44. | Ramji KM, Cleghorn MC, Josse JM, MacNeill A, O’Brien C, Urbach D, Quereshy FA. Comparison of clinical and economic outcomes between robotic, laparoscopic, and open rectal cancer surgery: early experience at a tertiary care center. Surg Endosc. 2016;30:1337-1343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 61] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 45. | Kim YS, Kim MJ, Park SC, Sohn DK, Kim DY, Chang HJ, Nam BH, Oh JH. Robotic Versus Laparoscopic Surgery for Rectal Cancer after Preoperative Chemoradiotherapy: Case-Matched Study of Short-Term Outcomes. Cancer Res Treat. 2016;48:225-231. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 46. | Kim JC, Yu CS, Lim SB, Park IJ, Kim CW, Yoon YS. Comparative analysis focusing on surgical and early oncological outcomes of open, laparoscopy-assisted, and robot-assisted approaches in rectal cancer patients. Int J Colorectal Dis. 2016;31:1179-1187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 47. | Kwak JM, Kim SH, Kim J, Son DN, Baek SJ, Cho JS. Robotic vs laparoscopic resection of rectal cancer: short-term outcomes of a case-control study. Dis Colon Rectum. 2011;54:151-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 145] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 48. | Park JS, Choi GS, Lim KH, Jang YS, Jun SH. S052: a comparison of robot-assisted, laparoscopic, and open surgery in the treatment of rectal cancer. Surg Endosc. 2011;25:240-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 147] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 49. | Popescu I, Vasilescu C, Tomulescu V, Vasile S, Sgarbura O. The minimally invasive approach, laparoscopic and robotic, in rectal resection for cancer. A single center experience. Acta Chir Iugosl. 2010;57:29-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 50. | Ramji KM, Cleghorn MC, Josse JM, MacNeill A, O'Brien C, Urbach D, Quereshy FA. Comparison of clinical and economic outcomes between robotic, laparoscopic, and open rectal cancer surgery: early experience at a tertiary care center. Surg Endosc. 2016;30:1337-1343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 61] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 51. | Serin KR, Gultekin FA, Batman B, Ay S, Kapran Y, Saglam S, Asoglu O. Robotic versus laparoscopic surgery for mid or low rectal cancer in male patients after neoadjuvant chemoradiation therapy: comparison of short-term outcomes. J Robot Surg. 2015;9:187-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 52. | Silva-Velazco J, Dietz DW, Stocchi L, Costedio M, Gorgun E, Kalady MF, Kessler H, Lavery IC, Remzi FH. Considering Value in Rectal Cancer Surgery: An Analysis of Costs and Outcomes Based on the Open, Laparoscopic, and Robotic Approach for Proctectomy. Ann Surg. 2017;265:960-968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 69] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 53. | Valverde A, Goasguen N, Oberlin O, Svrcek M, Fléjou JF, Sezeur A, Mosnier H, Houdart R, Lupinacci RM. Robotic versus laparoscopic rectal resection for sphincter-saving surgery: pathological and short-term outcomes in a single-center analysis of 130 consecutive patients. Surg Endosc. 2017;31:4085-4091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 54. | Yamaguchi T, Kinugasa Y, Shiomi A, Tomioka H, Kagawa H, Yamakawa Y. Robotic-assisted vs. conventional laparoscopic surgery for rectal cancer: short-term outcomes at a single center. Surg Today. 2016;46:957-962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 74] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 55. | Zhang H, Yuan W, Zhou Q, Gu X, Wang F. [Efficacy comparison of robotic and laparoscopic radical surgery in the treatment of middle-low rectal cancer]. Zhonghua Wei Chang Wai Ke Za Zhi. 2017;20:540-544. [PubMed] |
| 56. | Lin S, Jiang HG, Chen ZH, Zhou SY, Liu XS, Yu JR. Meta-analysis of robotic and laparoscopic surgery for treatment of rectal cancer. World J Gastroenterol. 2011;17:5214-5220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 88] [Cited by in RCA: 89] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 57. | Park S, Kim NK. The Role of Robotic Surgery for Rectal Cancer: Overcoming Technical Challenges in Laparoscopic Surgery by Advanced Techniques. J Korean Med Sci. 2015;30:837-846. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 58. | Chen ST, Wu MC, Hsu TC, Yen DW, Chang CN, Hsu WT, Wang CC, Lee M, Liu SH, Lee CC; Health Economics and Outcome Research Group, National Taiwan University Hospital. Comparison of outcome and cost among open, laparoscopic, and robotic surgical treatments for rectal cancer: A propensity score matched analysis of nationwide inpatient sample data. J Surg Oncol. 2018;117:497-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 59. | Guadagni S, Di Franco G, Gianardi D, Palmeri M, Ceccarelli C, Bianchini M, Furbetta N, Caprili G, D’Isidoro C, Moglia A. Control Comparison of the New EndoWrist and Traditional Laparoscopic Staplers for Anterior Rectal Resection with the Da Vinci Xi: A Case Study. J Laparoendosc Adv Surg Tech A. 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |