Copyright
©The Author(s) 2023.
World J Gastrointest Oncol. Jun 15, 2023; 15(6): 925-942
Published online Jun 15, 2023. doi: 10.4251/wjgo.v15.i6.925
Published online Jun 15, 2023. doi: 10.4251/wjgo.v15.i6.925
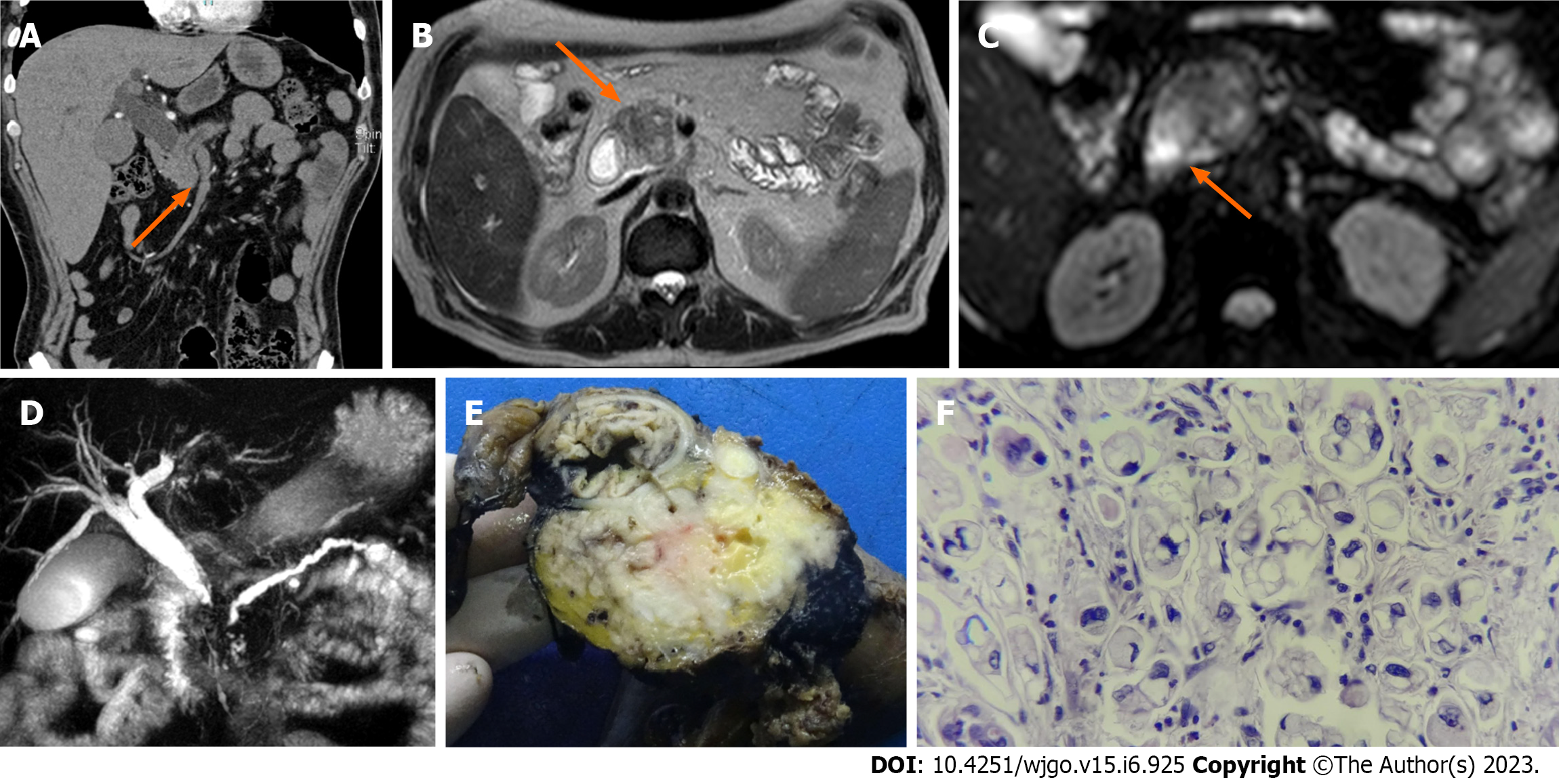
Figure 1 A 62-year-old male patient with a history of abdominal pain and jaundice.
A: Contrast-enhanced abdominal tomography shows a poorly enhanced hypocaptured lesion (orange arrow); B: Magnetic resonance imaging (MRI) in the T2 sequence shows a hypointense lesion (orange arrow); C: MRI in the diffusion sequence shows a lesion with restriction (orange arrow); D: In magnetic resonance cholangiopancreatography, the double duct sign is evident; E: Macroscopic specimen of the head of the pancreas in which there is a whitish mass; F: Slides report poorly differentiated pancreatic ductal adenocarcinoma of the pancreas with high-grade signet ring cells with perineural infiltration and invasion of the duodenum and ampulla of Vater.
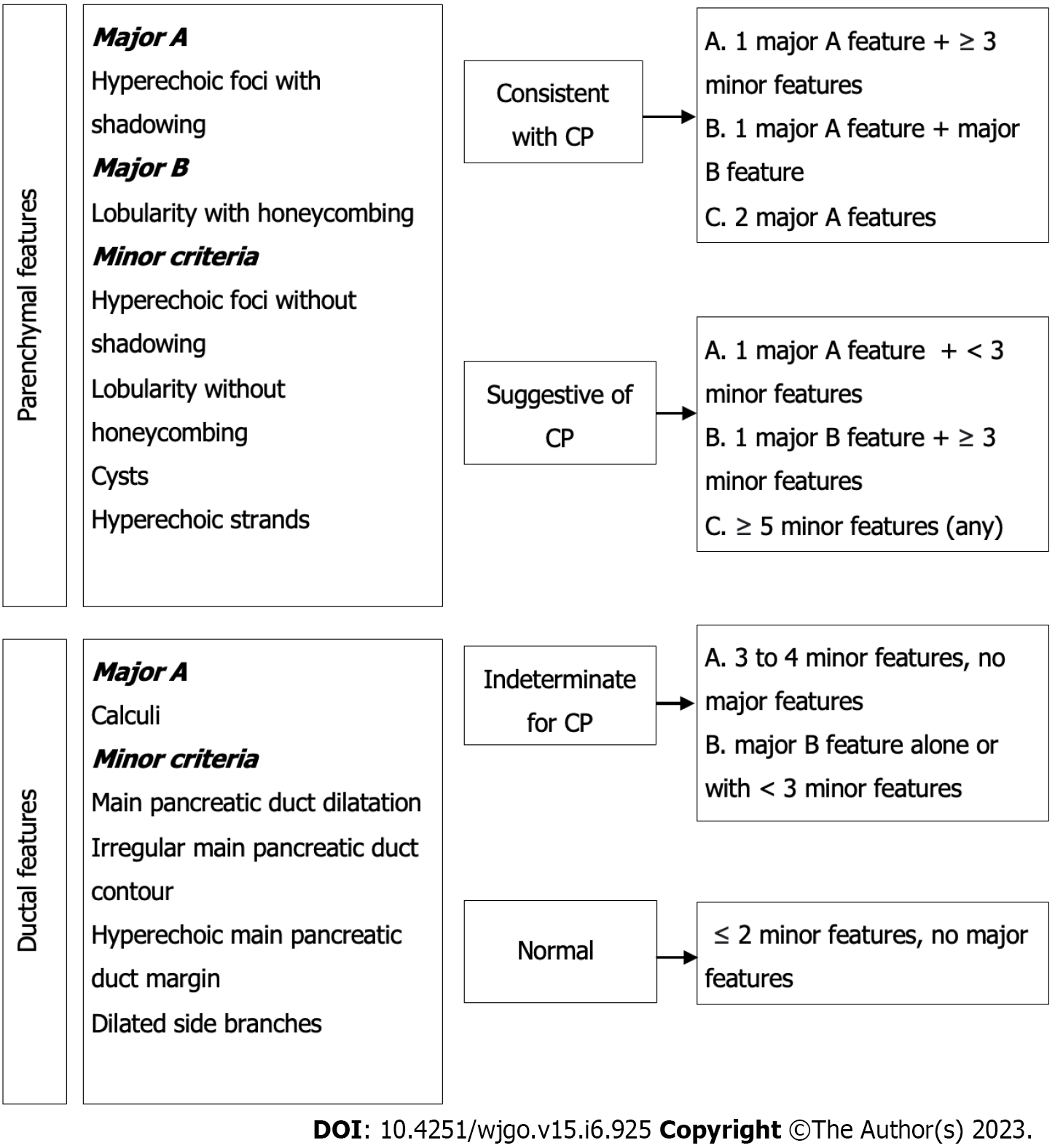
Figure 2 Rosemont classification for chronic pancreatitis.
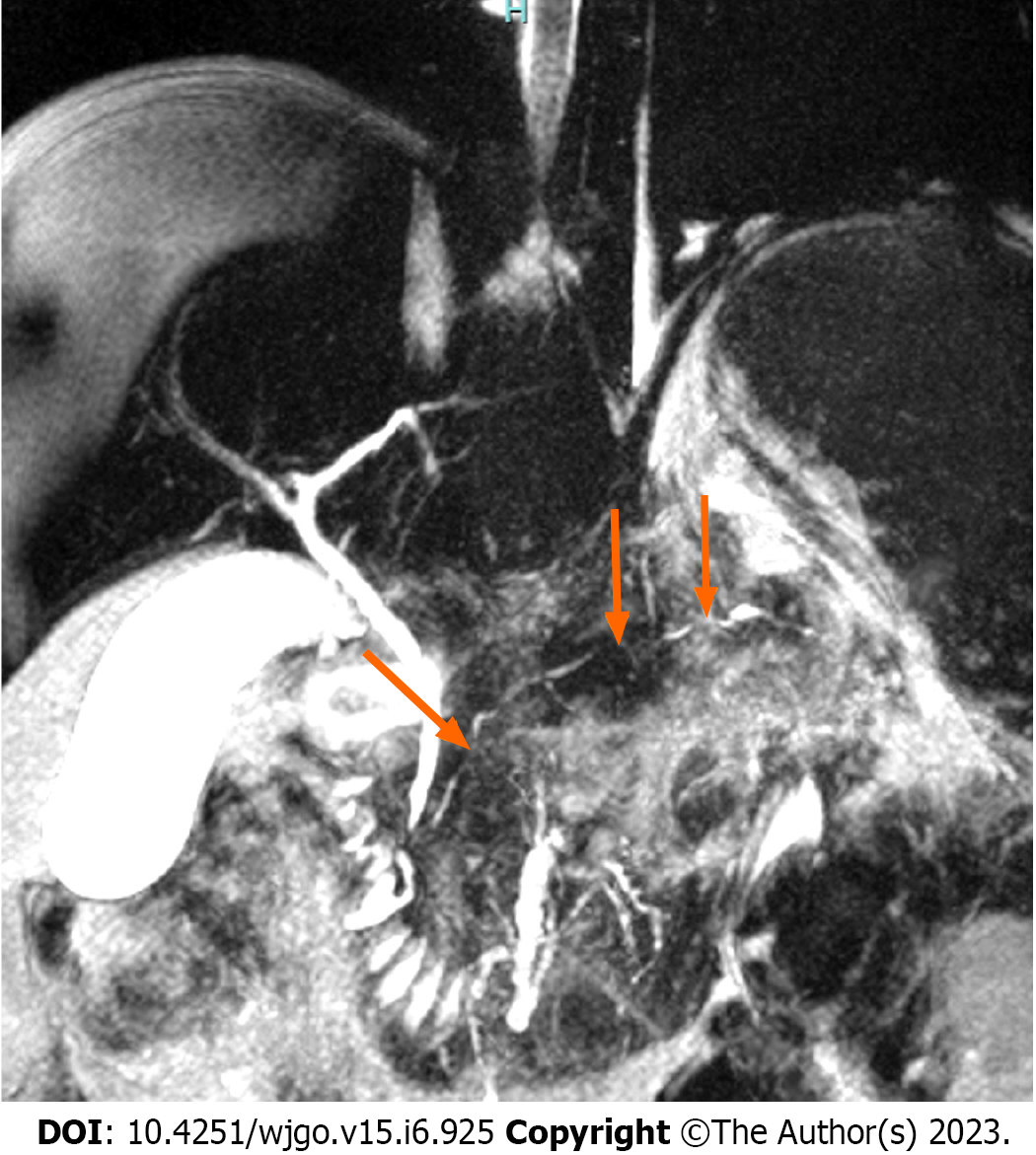
Figure 3 A 38-year-old man was diagnosed with autoimmune pancreatitis.
The magnetic resonance cholangiopancreatography shows a pancreatic duct with multiple stenoses (orange arrow) without upstream dilation.
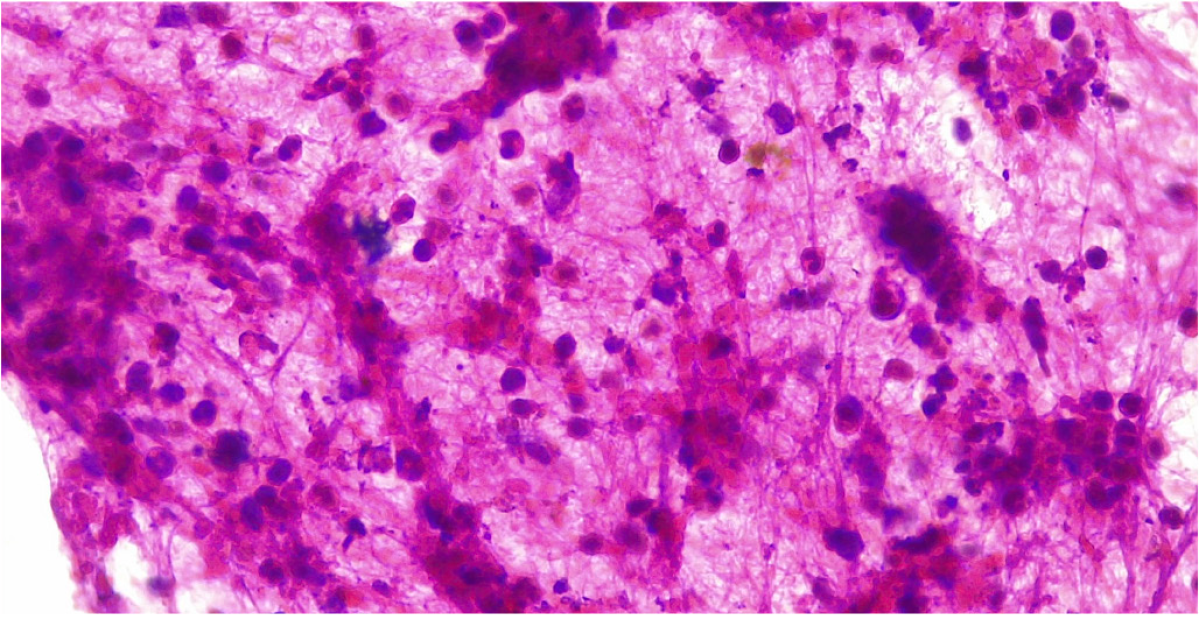
Figure 4 Endoscopic ultrasound guided fine needle biopsy of a type 2 autoimmune pancreatitis.
Specimens shows dense lymphocyte infiltrate with scattered neutrophils. Citation: Pelaez-Luna M, Soriano-Rios A, Lira-Treviño AC, Uscanga-Domínguez L. Steroid-responsive pancreatitides. World J Clin Cases 2020; 8: 3411-3430. Published by Baishideng Publishing Group Inc[60] (Supplementary material).
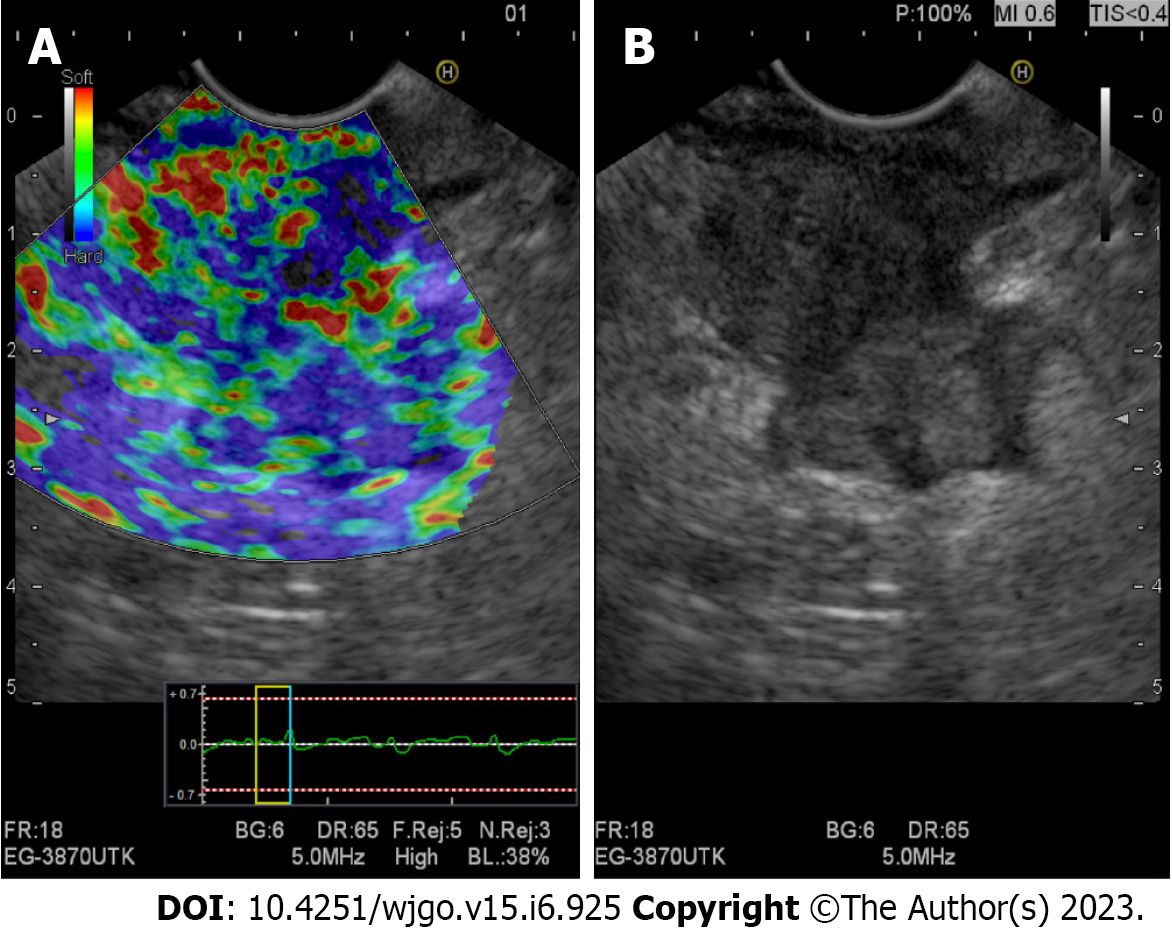
Figure 5 Evaluation of a pancreatic adenocarcinoma using qualitative endoscopic ultrasound elastography.
A: Elastography showing a heterogeneous stiff pattern (stiffer areas are shown in blue); B: Linear array endoscopic ultrasound (B-mode) imaging of the same pancreatic mass.
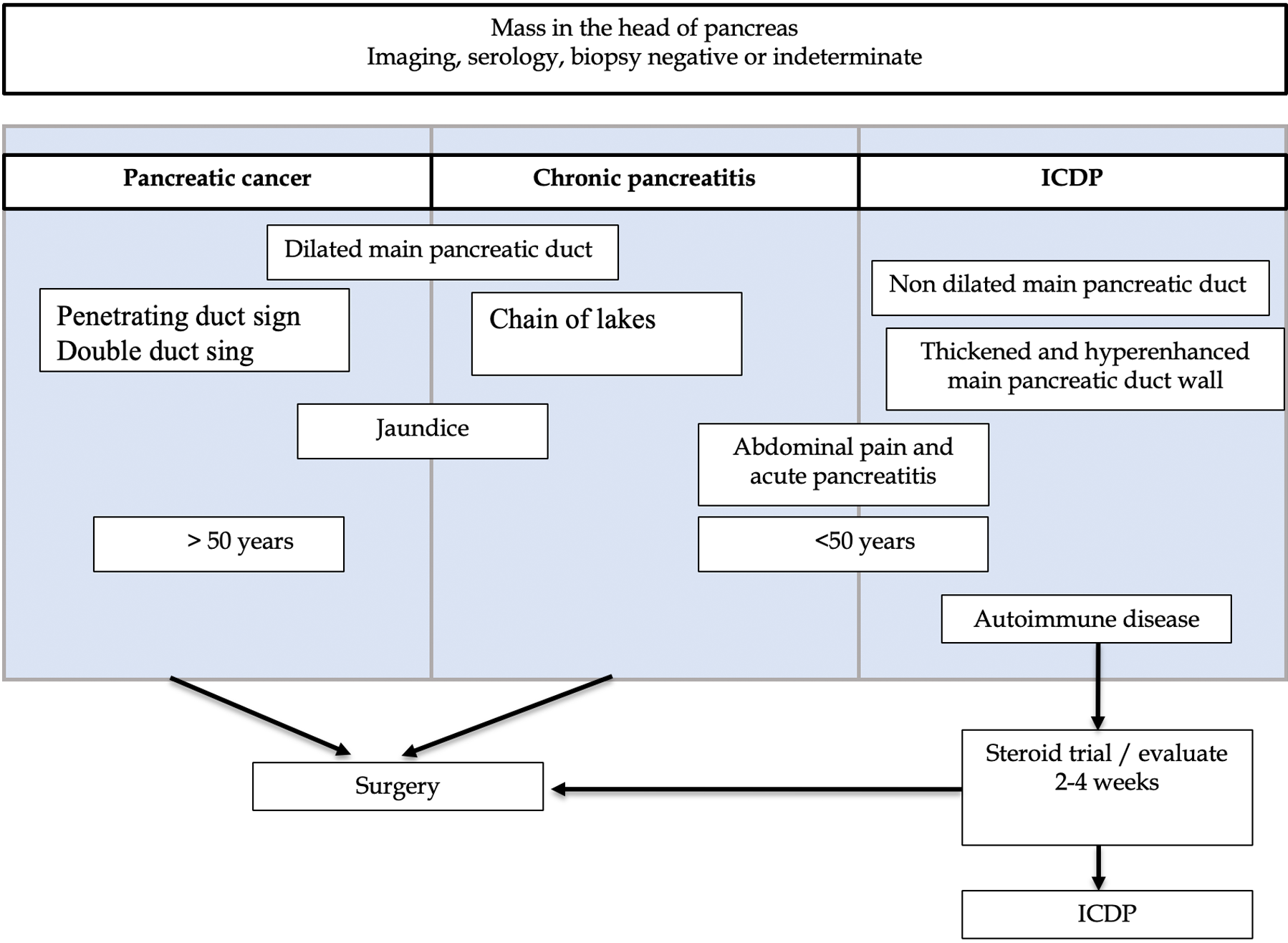
Figure 6 Differences in pancreatic masses.
IDCP: Idiopathic duct-centric pancreatitis. Citation: Peláez-Luna M, Medina-Campos C, Uscanga-Domínuez L, Hernandez-Calleros J, Chan-Nuñez C, Negrete E, Angeles A. A Nondilated Main Pancreatic Duct Predicts Type 2 Autoimmune Pancreatitis: Comparative Study of Resected Pancreatic Head Masses. Digestion 2020; 101: 137-143. Published by Karger Publishers[67] (Supplementary material).
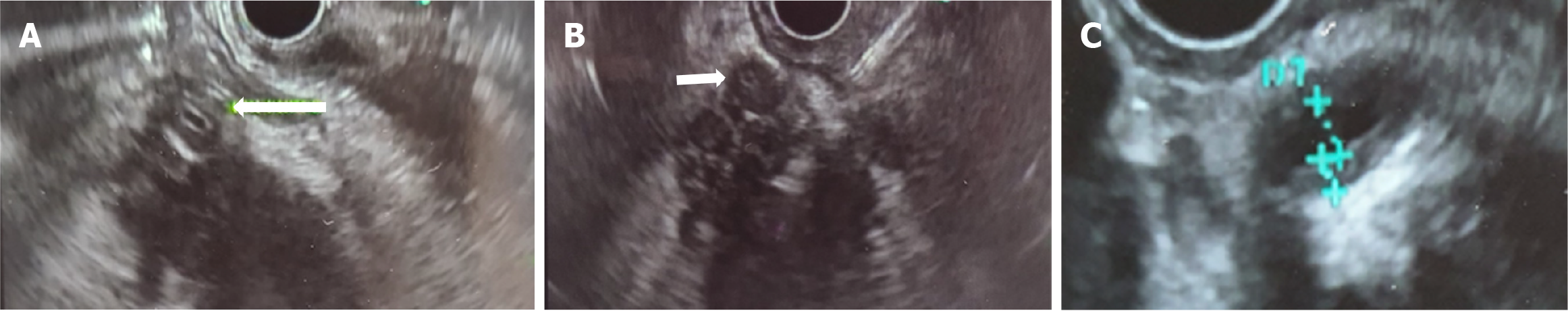
Figure 7 Ductal wall thickening (biliary/pancreatic) in 2 cases of type 2 autoimmune pancreatitis.
A: Hypoechoic mass in the head of the pancreas, arrow shows common bile duct (CBD) with hypoechoic symmetrical wall thickening in a histology confirmed type 2 autoimmune pancreatitis (AIP); B. Fine needle biopsy of a hypoechoic mass in the head of the pancreas. Arrow shows CBD with hypoechoic symmetrical wall thickening in the same case of a histology confirmed type 2 AIP; C: Homogeneous, symmetric main pancreatic duct wall thickening in other case of with histology confirmed type 2 AIP. Citation: Pelaez-Luna M, Soriano-Rios A, Lira-Treviño AC, Uscanga-Domínguez L. Steroid-responsive pancreatitides. World J Clin Cases 2020; 8: 3411-3430. Published by Baishideng Publishing Group Inc[60] (Supplementary material).
- Citation: Tornel-Avelar AI, Velarde Ruiz-Velasco JA, Pelaez-Luna M. Pancreatic cancer, autoimmune or chronic pancreatitis, beyond tissue diagnosis: Collateral imaging and clinical characteristics may differentiate them. World J Gastrointest Oncol 2023; 15(6): 925-942
- URL: https://www.wjgnet.com/1948-5204/full/v15/i6/925.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v15.i6.925