Copyright
©The Author(s) 2018.
World J Gastrointest Oncol. Nov 15, 2018; 10(11): 381-397
Published online Nov 15, 2018. doi: 10.4251/wjgo.v10.i11.381
Published online Nov 15, 2018. doi: 10.4251/wjgo.v10.i11.381
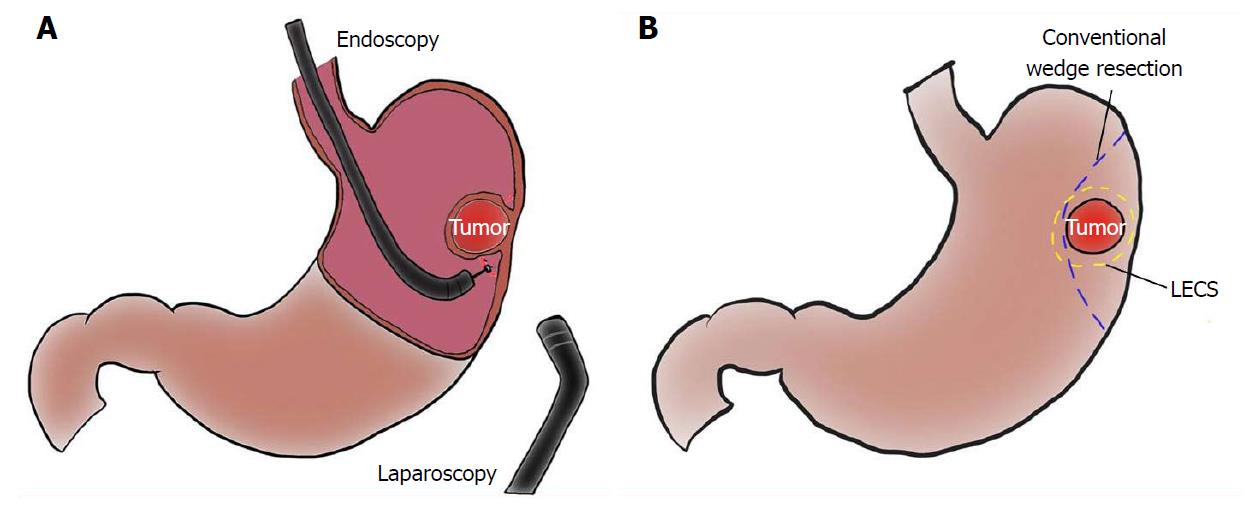
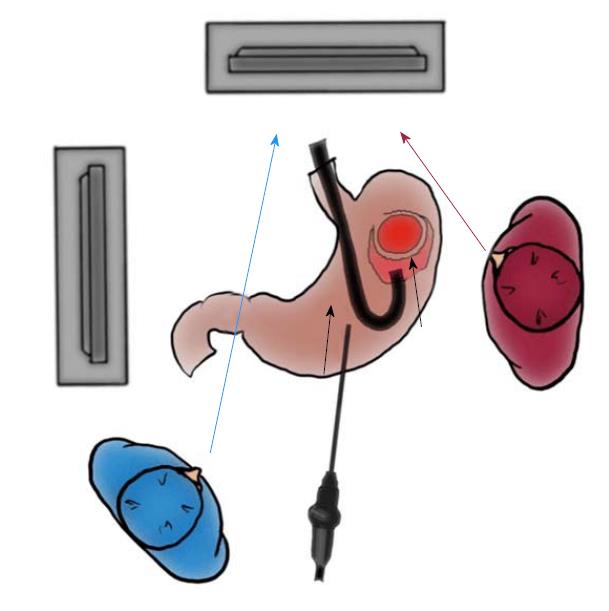
Figure 1 Schema of laparoscopic and endoscopic cooperative surgery, and comparison of resection line between laparoscopic and endoscopic cooperative surgery and conventional wedge resection.
A: Laparoscopic and endoscopic cooperative surgery (LECS) is a combined procedure involving laparoscopy and endoscopy; B: The resection line of LECS minimizes the surgical margin, securing an adequate distance from the tumor. Conventional wedge resection is too close to the tumor and involves excessive wall dissection.
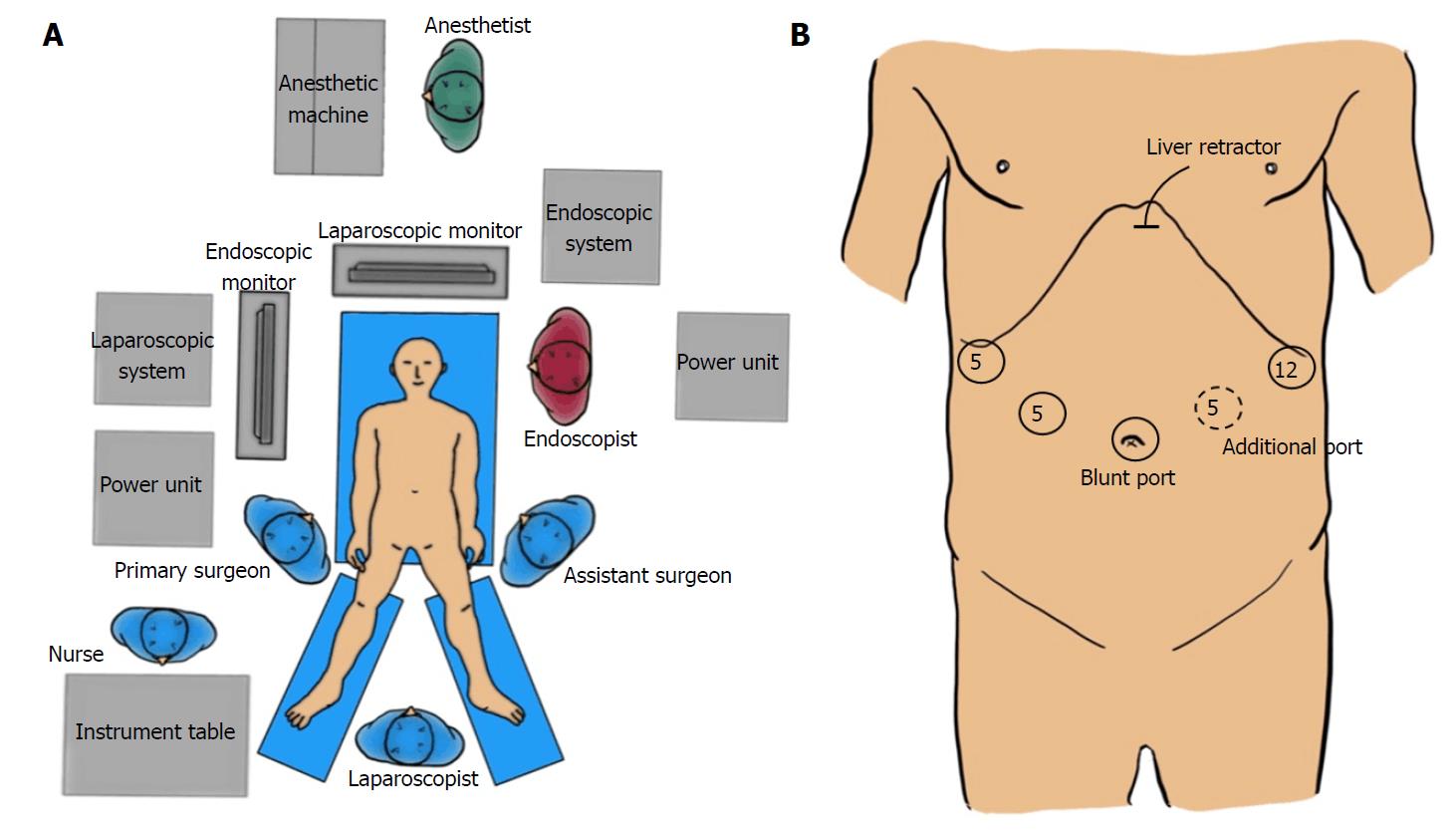
Figure 2 Set-up of staffs and devices in the operation theater and port placement.
A: Apparatus position and staff placement in the operation room; B: Port placement.
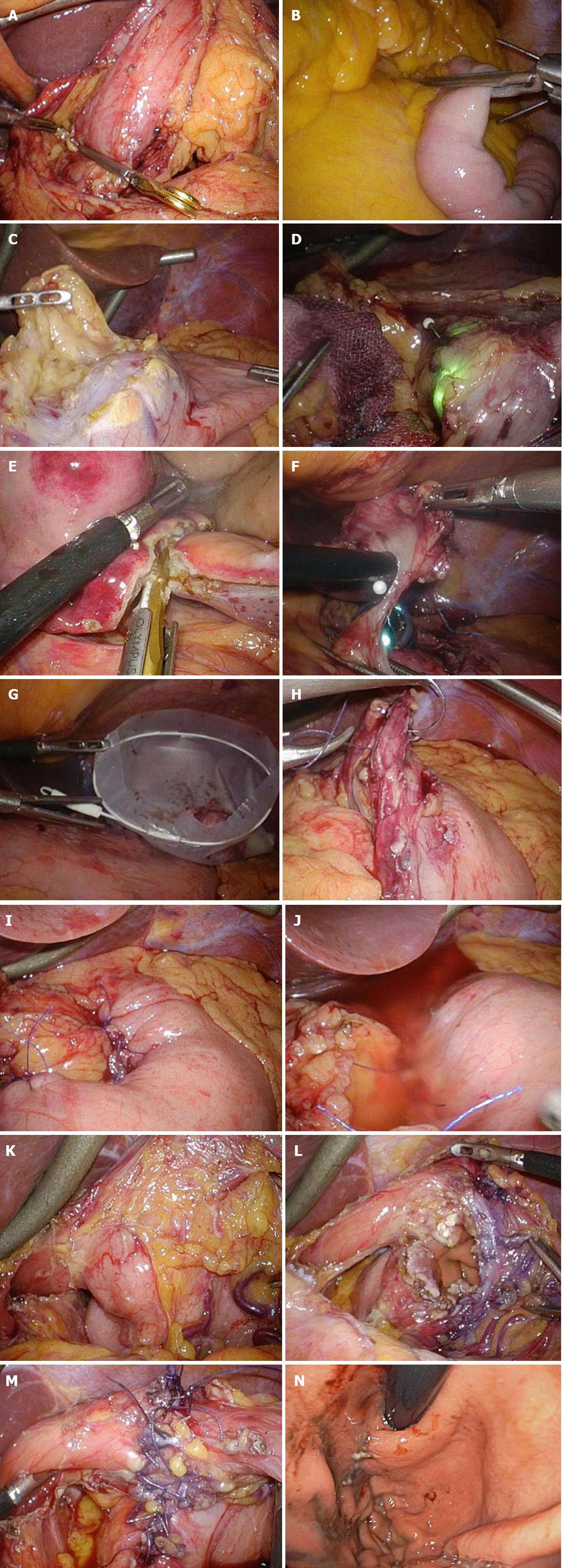
Figure 3 Intraoperative laparoscopic view of laparoscopic and endoscopic cooperative surgery.
A and B: Clamping of the (A) antrum or (B) jejunum should be performed using clamp forceps. This allows for adequate gastric expansion that provides an intraluminal working field for the endoscopic intervention; C: The surrounding fat tissue and vessels of the gastric wall are dissected, and the target wall is then mobilized to the ventral side; D: The laparoscopic surgeon should mobilize the gastric wall and prevent it from touching any surrounding organs for a safe intraluminal intervention. The pneumoperitoneal pressure and light intensity of laparoscopy are decreased to avoid disturbing the endoscopist; E: The laparoscopic surgeon can dissect the proximal gastric wall on behalf of the interventional endoscopist, if necessary; F: The surgeon and the endoscopist cooperate to complete the operation while avoiding injury to the adjacent organs; G: The resected specimen is placed in a plastic bag and removed intraluminally using endoscopy; H: The mucosal layer is closed with a running 4-0 absorbable suture thread; I: The seromuscular layer is closed with interrupted 3-0 absorbable sutures; J: A leak test is performed after suturing. K: This image depicts a case involving a tumor located in the posterior wall near the EGJ; The target gastric wall is turned as much as possible with a marginal free space established by carbon dioxide gas. The right side of the EGJ has enough working space laparoscopically; L: The defect of the gastric wall tends to become larger than many physicians expect; M: The defect in the gastric wall is closed with the laparoscopic hand-sewn technique in a layer-to-layer fashion; N: Intraluminal view after suturing. The absence of stenosis and malformation is confirmed. EGJ: Esophagogastric junction.
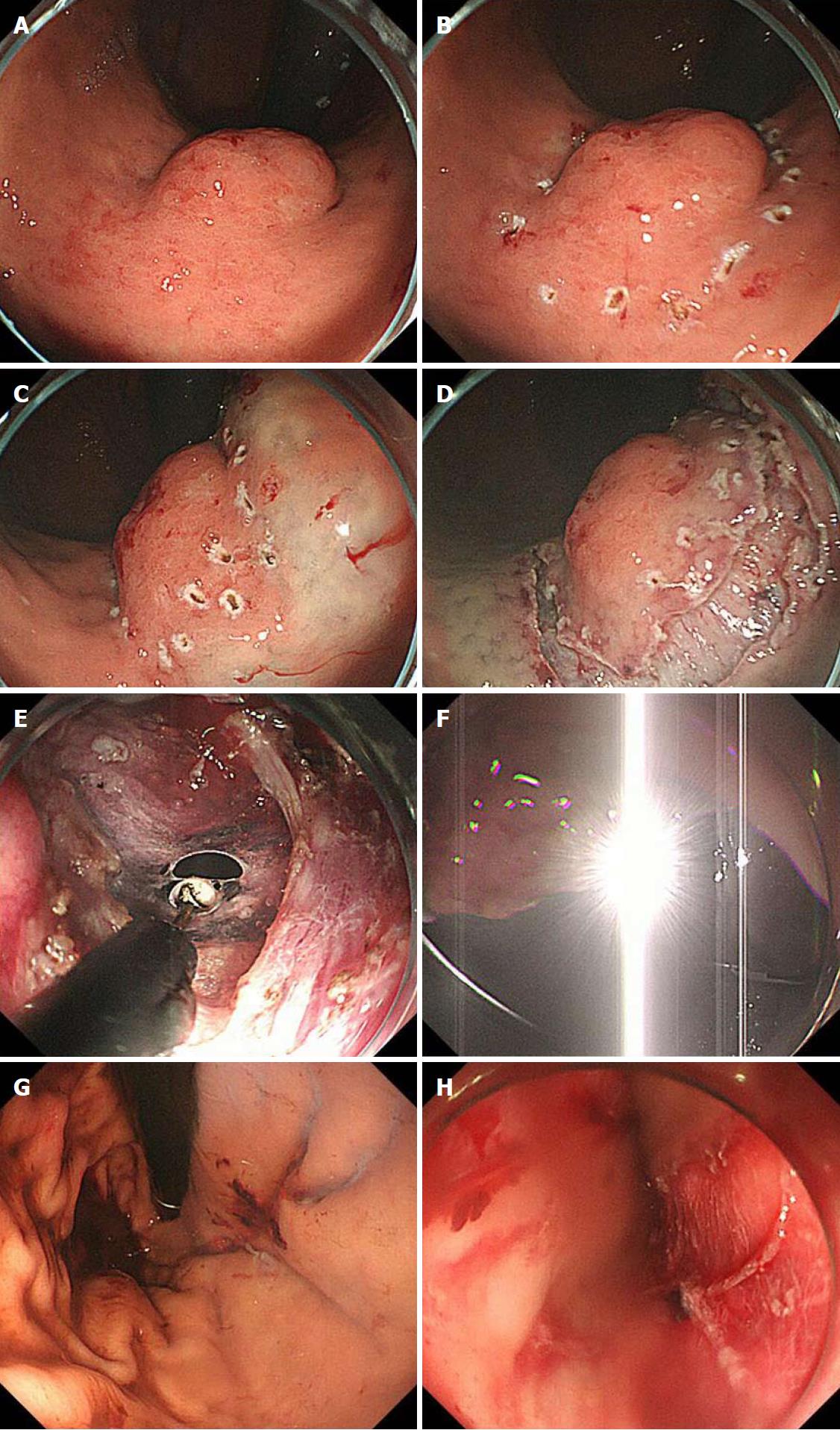
Figure 4 Intraoperative endoscopic view of laparoscopic and endoscopic cooperative surgery.
A: First, the location of the tumor is confirmed; B: The periphery of the tumor is marked using argon plasma coagulation as close as possible to the tumor edge; C: Glycerin mixed with indigo blue is injected into the submucosal layer; D: The whole circumference of the marked area is cut using an insulation-tipped diathermic knife; E: An intentional perforation is made; F: The laparoscopic light is too dazzling for the endoscopic side; G: Intraluminal view after suturing. The absence of stenosis and malformation is confirmed; H: Esophageal mucosa injury by the plastic bag during specimen removal.
Figure 5 Importance of interventional endoscopist’s line of vision while cutting the proximal side.
The interventional endoscopist may experience some difficulties while cutting the proximal side of the gastric wall because of the reversed endoscopic image. If such difficulties are encountered, the endoscopist should turn his or her eyes to the laparoscopic monitor instead of the endoscopic monitor.
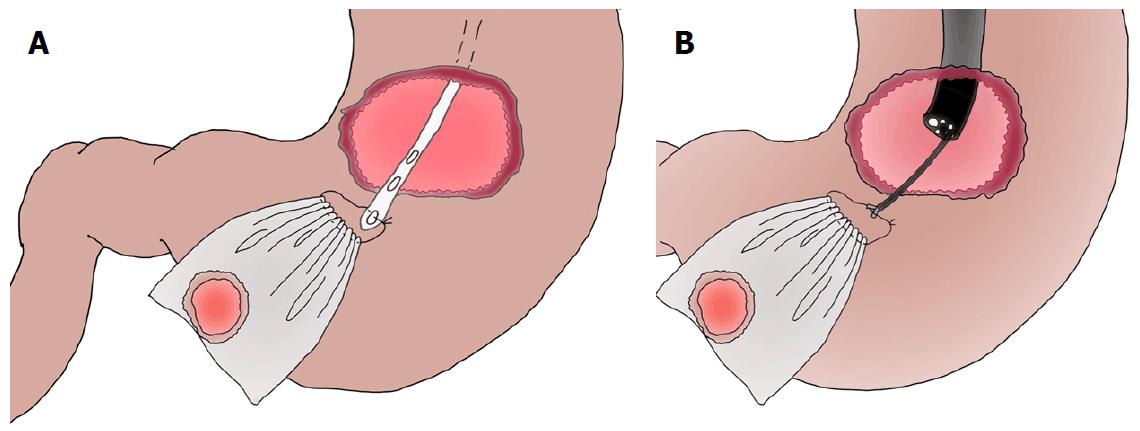
Figure 6 Options of specimen removal with plastic bag.
A: Specimen removal with a nasogastric tube; B: Specimen removal with an endoscopic forcep.
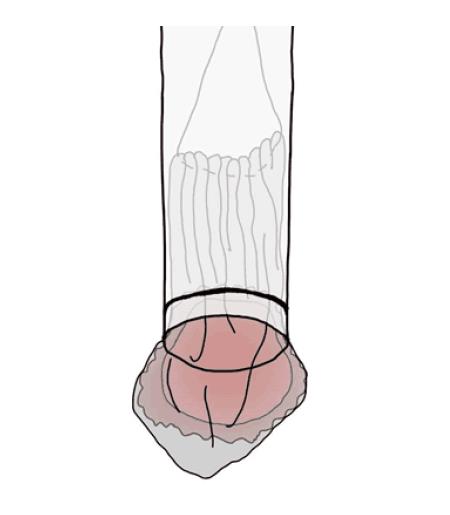
Figure 7 Effective use of an overtube when removing the specimen.
The tumor encased in the bag should be sheathed as much as possible in the overtube and removed through the mouth along with the overtube. Hence, injury to the esophageal mucosa by the plastic bag during specimen removal can be avoided.
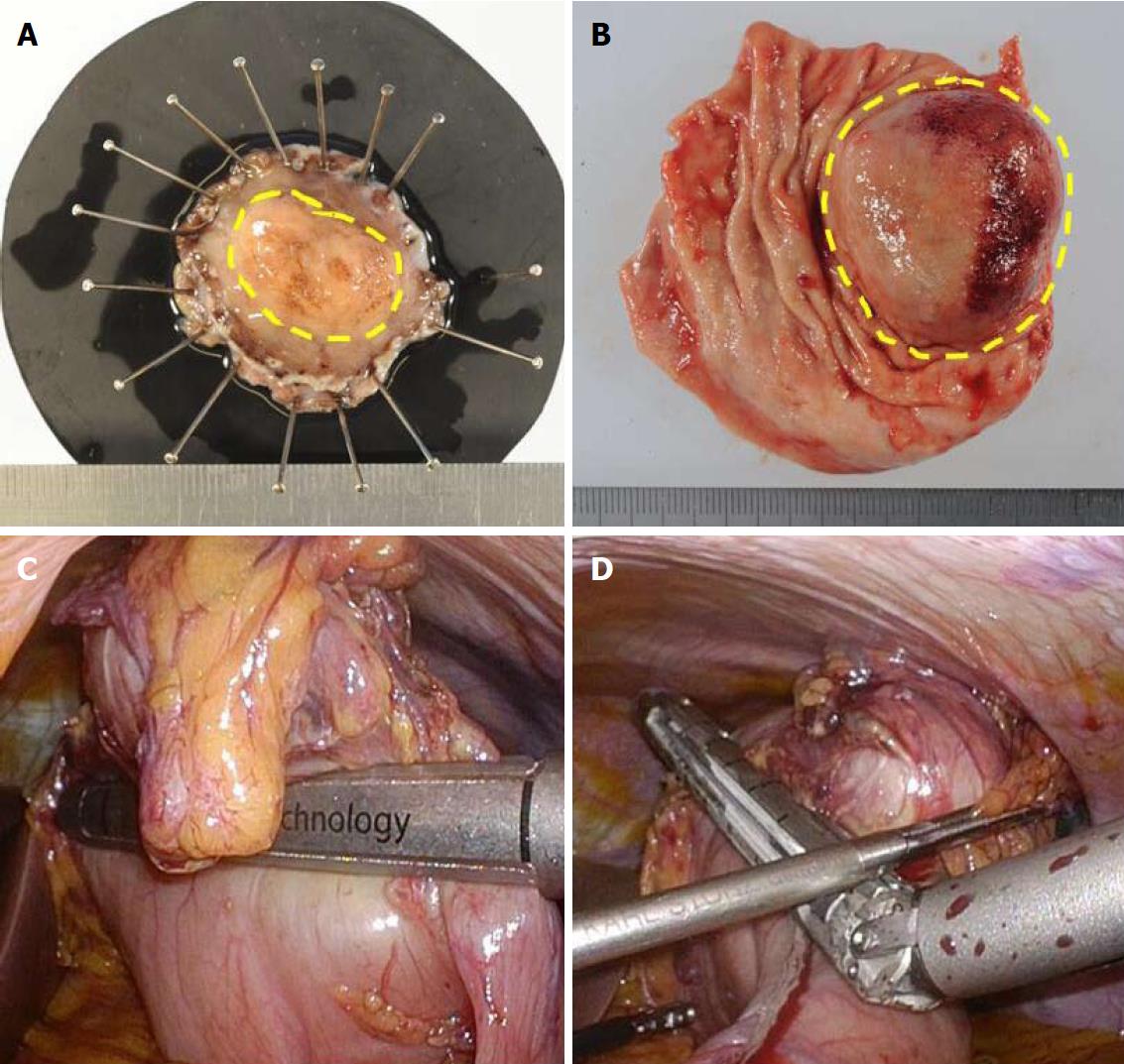
Figure 8 Comparison of surgical margins between laparoscopic and endoscopic cooperative surgery and conventional wedge resection.
A: Specimen of Laparoscopic and endoscopic cooperative surgery (LECS). The surgical margin from the tumor is kept at the proper distance; B: Specimen of conventional wedge resection. Simple wedge resection causes both excessive and inadequate resection of the gastric wall, which may lead to postoperative gastric stenosis, gastric dysfunction, and local recurrence; C and D: Intraoperative view of conventional wedge resection with a linear stapler. The resection line is as shown in Figure 1B. The specimen has a portion too close to the tumor and a portion far from the tumor.
- Citation: Aisu Y, Yasukawa D, Kimura Y, Hori T. Laparoscopic and endoscopic cooperative surgery for gastric tumors: Perspective for actual practice and oncological benefits. World J Gastrointest Oncol 2018; 10(11): 381-397
- URL: https://www.wjgnet.com/1948-5204/full/v10/i11/381.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v10.i11.381