Published online Sep 16, 2017. doi: 10.4253/wjge.v9.i9.494
Peer-review started: February 14, 2017
First decision: May 17, 2017
Revised: July 1, 2017
Accepted: July 21, 2017
Article in press: July 24, 2017
Published online: September 16, 2017
Processing time: 213 Days and 9 Hours
In the report, we describe a case of refractory benign esophageal strictures from esophageal cancer after an operation for the placement of three partially covered self-expanding metal stents (SEMSs), which were all embedded in the esophageal wall. Using the stent-in-stent technique, the three embedded SEMSs were successfully removed without significant complications. To the best of our knowledge, few cases of the successful removal of multiple embedded esophageal SEMSs have been reported in the literature. This case also highlights that the stent-in-stent technique is effective for removing multiple embedded esophageal SEMSs.
Core tip: Stent embedding is a common complication that precludes the safe removal of stents. The article reports a case of benign esophageal strictures with three stents embedded and remained in place for over a year. We successfully removed the three embedded stents by using the stent-in-stent technique. The stent-in-stent technique is effective for the removal of multiple stents that are embedded in the esophageal wall.
- Citation: Liu XQ, Zhou M, Shi WX, Qi YY, Liu H, Li B, Xu HW. Successful endoscopic removal of three embedded esophageal self-expanding metal stents. World J Gastrointest Endosc 2017; 9(9): 494-498
- URL: https://www.wjgnet.com/1948-5190/full/v9/i9/494.htm
- DOI: https://dx.doi.org/10.4253/wjge.v9.i9.494
The placement of esophageal self-expanding metal stents (SEMSs) is commonly used to treat benign and malignant esophageal disorders, such as esophageal strictures and fistulas. SEMSs should be removed in a timely manner to avoid severe long-term complications for benign esophageal diseases. However, stent embedding is a common complication that precludes the safe removal of stents. This article reports the successful removal of three embedded esophageal SEMSs from a patient with benign esophageal strictures by using the stent-in-stent technique.
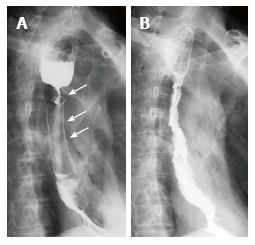
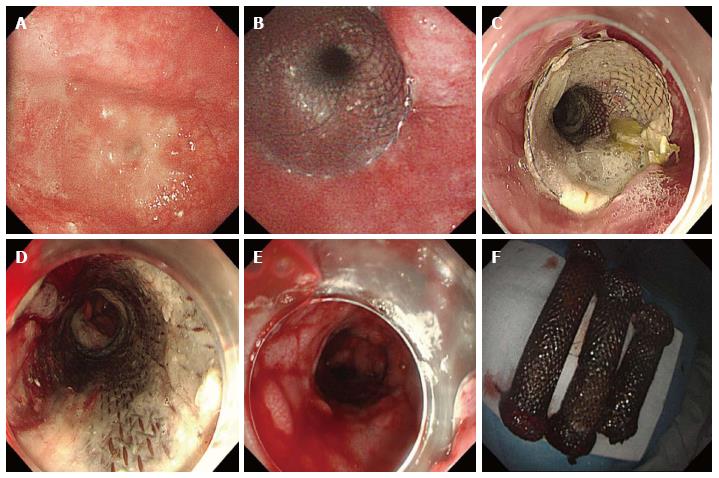
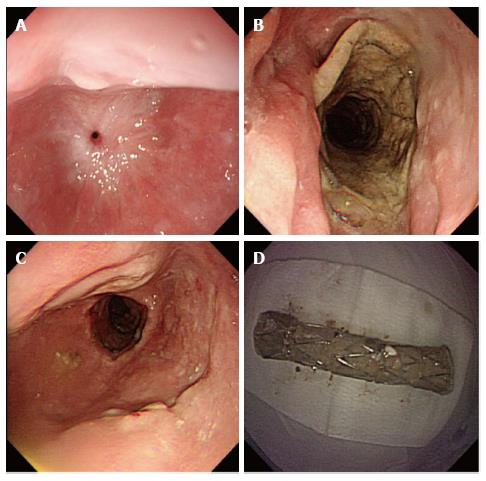
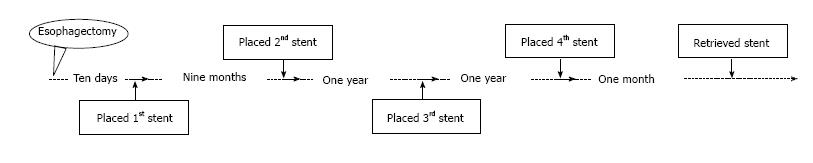
A 65-year-old male patient underwent a radical resection of distal esophageal carcinoma more than 2 years ago. The esophageal tumor located in 32 cm from the upper incisors, and there was no lymph node metastasis. Excision of inferior segmental esophagus and cardia of stomach and high intrathoracic anastomosis using gastric tube were performed in the patient. The postoperative pathological diagnosis was moderately differentiated esophageal squamous cell carcinoma. The first partially covered SEMS was placed at the local hospital for treating a gastroesophageal anastomotic fistula, which occurred ten days after the surgery. There was a benign stricture which was located the upper of stent after nine months the first stent placement. The second and third partially covered SEMSs were successively placed for the palliation of dysphagia from a benign esophageal stricture at another hospital, without the removal of the first stent. The patient was admitted to our hospital with recurrent dysphagia. A barium meal meal examination showed three visible metal stents and severe esophageal stricture (Figure 1A). Gastroscopy revealed a benign esophageal stricture located 25 cm from the upper incisors, which a conventional gastroscope (GIF-XQ260; Olympus Medical Systems, Tokyo, Japan) could not pass (Figure 2A). The proximal cup of the third stent was completely embedded in hyperplastic tissue. An ultrathin endoscope (GIF-XQ260N; Olympus Medical Systems, Tokyo, Japan) was subsequently used to scrape through the strictures and demonstrated that no embedded distal cups of stents. Removal of the embedded stents was attempted, but failed. Then, the fourth SEMS was placed inside the original stents to achieve pressure necrosis (Figure 2B and C). After the stent placement, the dysphagia was alleviated and the quality of the patient’s life was significantly improved. A month later, the fourth stent was retrieved by endoscopy. Meanwhile, we attempted but failed to remove the other three stents (Figure 2D). A week later, we attempted to retrieve the stents again and successfully removed all the initial stents without significant complications (Figure 2E). The upper gastrointestinal contrast X-ray study revealed no contrast extravasation, and the patient was allowed a semi-liquid diet (Figure 1B). The patient developed recurrent dysphagia 5 wk after stent removal, which was resolved after the temporary placement of a fully covered SEMS for 4 wk (Figure 3). No dysphagia or further complications occurred during 6-mo follow-up period.
Stent placement is widely used in the treatment of a variety of benign and malignant esophageal strictures, which can quickly and effectively dilate strictures and relieve dysphagia[1,2]. The temporary placement of an esophageal stent has become an effective treatment for refractory benign esophageal strictures owing to its longer-lasting dilatation effects, ability to maintain luminal patency and simultaneous stretching of the strictures[3-5]. However, for the management of benign esophageal strictures, the long-term placement of stents is deprecated because of the potential for adverse events, such as migration, bleeding, fistula formation, hyperplastic tissue overgrowth or ingrowth stent restenosis and damage to surrounding organs[6]. The optimal stenting duration remains unclear and should be individualized depending on the type and characteristics of the stricture. Generally, it is recommended that stents remain in place for 4-8 wk and no more than 16 wk for benign esophageal strictures to maximize the success and minimize the risk of a hyperplastic tissue reaction[1,7]. If stents need to be in place for a long time, upper endoscopy performed at 4-wk intervals is necessary to determine whether the stent has become embedded in the esophageal wall[7].
In our patient’s case, three SEMSs remained in place for over a year, and the upper ends of them were completely embedded. Thus, the removal of stents was difficult and inevitably associated with bleeding and mucosal tears[8]. However, without the removal of the stents, the stricture could not be dilated to an adequate diameter by endoscopic dilatation, which is the most common initial treatment for benign esophageal strictures. In addition, with the successive placement of the stents, the esophageal stricture moved upward, and there was no space to place a new stent. Gastrostomy and nasogastric tube placement are alternative treatment strategies, but they all have negative influences on the patient’s quality of life[9]. Percutaneous endoscopic gastrostomy is impossible for patients with intrathoracic stomach. Furthermore, these patients are often unwilling or not in a suitable enough condition to undergo a complex surgical procedure. Therefore, stent removal is imperative, whether for the prevention of long-term complications or for facilitating further treatment.
We temporarily placed a new stent within the initial stents according to the stent-in-stent technique to facilitate the mobilization and safe removal of all stents by inducing pressure ischemia of the granulation tissue. Ultimately, three embedded stents were successfully removed without serious complications (Figure 4). Previous studies have shown that the stent-in-stent technique is a safe and effective method for removing single embedded esophageal stents[10]. This is the first report showing that the stent-in-stent technique also applies to the removal of multiple stents that have become embedded in the esophageal wall.
For the management of benign esophageal strictures, the placement of stents is a minimally invasive treatment option, but it still requires serious consideration because of the potential for adverse events. Even when stent removal is very difficult for benign esophageal diseases, permanent stent placement should be avoided, and the stent-in-stent technique can be attempted.
This article reports a case of successful removal of three embedded esophageal self-expanding metal stents (SEMSs) in a patient who has benign esophageal strictures.
The patient had refractory benign esophageal stricture of esophagus cancer after operation and was placed three partially covered SEMSs.
The benign esophageal stricture differentiated with malignant stricture by pathology inspection.
The laboratory testing were tumor markers, and the results are generally negative.
Barium meal examination of the patient showed three visible metal stents and severe esophageal stricture.
The postoperative pathologic diagnosis was moderately differentiated esophageal squamous cell carcinoma.
With the assistance of the stent-in-stent technique, the three embedded SEMSs were successfully removed with no significant complications.
For the management of benign esophageal strictures, the placement of stents is a minimally invasive treatment option, but it still requires serious consideration because of the potential for adverse events. Even when stent removal is very difficult for benign esophageal diseases, permanent stent placement should be avoided, and the stent-in-stent technique can be attempted.
The authors reported a case of refractory benign esophageal strictures with three stent embedded in the esophagus and successfully treated with a sten-in-stent technique. The case is interesting and the case report is well-written with nice picture demonstration and therefore is worth to share with the readers who care or treat such patients.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Serban ED, Tseng PH S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Spaander MC, Baron TH, Siersema PD, Fuccio L, Schumacher B, Escorsell À, Garcia-Pagán JC, Dumonceau JM, Conio M, de Ceglie A, Skowronek J, Nordsmark M, Seufferlein T, Van Gossum A, Hassan C, Repici A, Bruno MJ. Esophageal stenting for benign and malignant disease: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:939-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 208] [Article Influence: 23.1] [Reference Citation Analysis (1)] |
| 2. | Mangiavillano B, Pagano N, Arena M, Miraglia S, Consolo P, Iabichino G, Virgilio C, Luigiano C. Role of stenting in gastrointestinal benign and malignant diseases. World J Gastrointest Endosc. 2015;7:460-480. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 29] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (1)] |
| 3. | Suzuki T, Siddiqui A, Taylor LJ, Cox K, Hasan RA, Laique SN, Mathew A, Wrobel P, Adler DG. Clinical Outcomes, Efficacy, and Adverse Events in Patients Undergoing Esophageal Stent Placement for Benign Indications: A Large Multicenter Study. J Clin Gastroenterol. 2016;50:373-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 4. | Eloubeidi MA, Talreja JP, Lopes TL, Al-Awabdy BS, Shami VM, Kahaleh M. Success and complications associated with placement of fully covered removable self-expandable metal stents for benign esophageal diseases (with videos). Gastrointest Endosc. 2011;73:673-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 77] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 5. | Dua KS, Vleggaar FP, Santharam R, Siersema PD. Removable self-expanding plastic esophageal stent as a continuous, non-permanent dilator in treating refractory benign esophageal strictures: a prospective two-center study. Am J Gastroenterol. 2008;103:2988-2994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 103] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 6. | Bick BL, Song LM, Buttar NS, Baron TH, Nichols FC, Maldonado F, Katzka DA, Enders FT, Topazian MD. Stent-associated esophagorespiratory fistulas: incidence and risk factors. Gastrointest Endosc. 2013;77:181-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 7. | Siersema PD. Stenting for benign esophageal strictures. Endoscopy. 2009;41:363-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 51] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 8. | Wadhwa RP, Kozarek RA, France RE, Brandabur JJ, Gluck M, Low DE, Traverso LW, Moonka R. Use of self-expandable metallic stents in benign GI diseases. Gastrointest Endosc. 2003;58:207-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 106] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 9. | Repici A, Small AJ, Mendelson A, Jovani M, Correale L, Hassan C, Ridola L, Anderloni A, Ferrara EC, Kochman ML. Natural history and management of refractory benign esophageal strictures. Gastrointest Endosc. 2016;84:222-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 10. | DaVee T, Irani S, Leggett CL, Berzosa Corella M, Grooteman KV, Wong Kee Song LM, Wallace MB, Kozarek RA, Baron TH. Stent-in-stent technique for removal of embedded partially covered self-expanding metal stents. Surg Endosc. 2016;30:2332-2341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |