Published online Feb 16, 2017. doi: 10.4253/wjge.v9.i2.77
Peer-review started: July 18, 2016
First decision: September 7, 2016
Revised: September 23, 2016
Accepted: November 1, 2016
Article in press: November 2, 2016
Published online: February 16, 2017
Processing time: 216 Days and 5.6 Hours
To examine the result of the use of 0.025-inch guidewire (GW) VisiGlide2TM as the first choice in the endoscopic retrograde cholangiopancreatography (ERCP)-related procedures without selecting the patient in a multicenter prospective study.
ERCP using 0.025-inch GW VisiGlide2TM as the first choice was conducted in patients who have needed ERCP, and its accomplishment rate of procedure, procedural time, incidence of accidental symptoms were compared with those of ERCP using 0.025-inch GW VisiGlideTM.
The accomplishment rate of procedure was 97.5% (197/202), and procedural time was 23.930 ± 16.207 min. The accomplishment rate of procedure using 0.025-inch GW VisiGlideTM was 92.3% (183/195), and procedural time was 31.285 ± 19.122 min, thus the accomplishment rate of procedure was significantly improved and procedural time was significantly shortened (P < 0.05). Accidental symptoms by ERCP-related procedures were observed in 3.0% (6/202), and all were conservatively alleviated.
When 0.025-inch GW VisiGlide2TM was used for ERCP-related procedure as the first choice, it showed high accomplishment rate of procedure and low incidence of accidental symptoms, suggesting it can be used as the universal GW. Clinical Trial Registry (UMIN0000016042).
Core tip: When 0.025-inch guidewire (GW) VisiGlide2TM was used for endoscopic retrograde cholangiopancreatography-related procedure as the first choice, it showed high accomplishment rate of procedure and low incidence of accidental symptoms, suggesting it can be used as the universal GW.
- Citation: Sakai Y, Tsuyuguchi T, Hirata N, Nakaji S, Shimura K, Nishikawa T, Fujimoto T, Hamano T, Nishino T, Yokosuka O. Clinical utility of 0.025-inch guidewire VisiGlide2TM in the endoscopic retrograde cholangiopancreatography-related procedures. World J Gastrointest Endosc 2017; 9(2): 77-84
- URL: https://www.wjgnet.com/1948-5190/full/v9/i2/77.htm
- DOI: https://dx.doi.org/10.4253/wjge.v9.i2.77
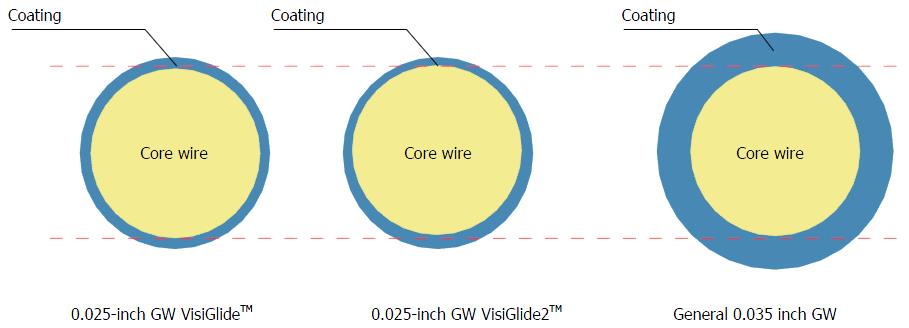
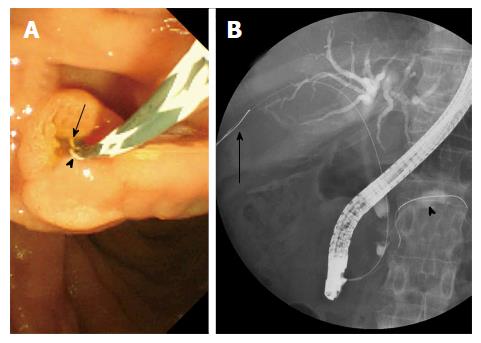
Endoscopic retrograde cholangiopancreatography (ERCP)-related procedures have played a very important role for diagnosis/treatment of biliary and pancreatic disease. In ERCP-related procedures, it is needless to say that the guidewire (GW) is essential in performing the procedure safely, and elevating the accomplishment rate of the procedure. There are the GWs of various diameters, but the GW which has been used as the first choice was of 0.035 inches considering the stability of procedure[1-12]. The 0.025-inch GW is thin and excellent in breaking through the stenosis and selecting the branch but problematic in visibility and rigidity, which has not been used as the first choice[1-12]. It has been used in the case in which it was impossible to break through the stenosis even by using 0.035-inch GW, and in particular, peroral cholangioscopy (POCS) and placement of metallic stent (MS) have generally been conducted with 0.035-inch GW because of the problem of rigidity[8-12]. Previously, after 0.025-inch GW was used for breaking through the stenosis, GW was switched to 0.035 inch GW to stabilize the procedure, and the procedure was re-started. However, together with advancement of the endoscope, GW was improved, and it has become possible to use VisiGlideTM with excellent visibility and sufficient rigidity in spite of the external diameter of 0.025-inch in the clinical setting. As a result, we have treated a number of patients in whom ERCP-related procedure can be accomplished using only this GW. However, there remained still problems that GW must be changed due to seeking failure in some patients, and GW perforation comparatively frequently occurs[13]. After that, it has become possible to use VisiGlide2TM remodeled from VisiGlideTM in the clinical setting (Figure 1)[14]. VisiGlide2TM has excellent endoscopic visibility (Figure 2), and also has improved fluoroscopic visibility of GW using 2 radiopaque chips similarly to VisiGlideTM (Figure 3). Although it has thinness of 0.025-inch (0.63 mm), its special processing method ensures rigidity equivalent to that of 0.035 inch (0.89 mm) (Figure 4). It is the GW that was devised to reduce GW perforation, the accidental symptom observed in use of VisiGlideTM, by making the tip flexible. The torque device for 0.025-inch GW VisiGlideTM was compliant to 0.035 inch previously, whereas that for 0.025-inch GW VisiGlide2TM has become compliant to 0.025-inch, thus torque transmissibility was improved.
We decided to examine the accomplishment rate of procedures and the incidence of accidental symptoms in the use of 0.025-inch GW VisiGlide2TM as the first-choice universal GW in the ERCP-related procedures.
All the patients with biliary and pancreatic diseases, who were decided to undergo ERCP in 5 institutions participating in this clinical study in a month of December 2014, were included. A 0.025-inch GW (VisiGlide2: Olympus Corp. Japan straight type or angle type) was used. For cannulation, catheters PR-104Q, PR110Q-1, PR-233Q and Clever-Cut3V (Olympus Corp. Japan) were used. The endoscopes used were JF200, JF240, JF260V, and TJF260V (Olympus Corp. Japan). Prospective data collected in multicenter study were compared with those obtained from multicenter prospective study of 0.025-inch GW VisiGlideTM which we have already reported[13]. Patients treated using VisiGlide2TMare shown. There were 202 patients including 122 males and 80 females, and the age was 72.9 (36 to 98) years old on average. The ERCP was conducted aiming at bile duct in 190 patients and pancreatic duct in 12 patients. There were 80 patients undergoing ERCP for the first time and 122 patients on whom papillary treatment has already been implemented. The case in which 0.025-inch guidewire VisiGlide2TM was used as a versatile GW and the scheduled procedure could be accomplished only with VisiGlide2TM at the ERCP was considered as the success of procedure, and the success rate and the incidence of accidental symptom were examined. Patients with difficulty in selective biliary cannulation were defined as patients who are considered by an investigator to be difficult cases for biliary cannulation after over 10 min performing papilla cannulation through the frontal view. If such patients were observed, the following procedures were used to achieve biliary cannulation at the investigator’s discretion: Needle knife precut papillotomy starting at orifice, transpancreatic precut papillotomy and pancreatic duct guidewire indwelling method. For patients with moderate or severe cholangitis, urgent ERCP was performed according to the Tokyo Guideline[15]. Iatrogenic morbidity was assessed according to the criteria of Cotton et al[16]. The observation period was 30 d after the procedure and any coincidental events noted during the period were considered as early coincidental events. All the treatment procedures were performed after obtaining the informed consent in writing from the patients. Assessment of this GW was performed based on approval of ethical committee of each institution, and registered at UMIN Clinical Trial Registry (UMIN0000016042-VIP2 study).
Person χ2 test with Yates correction and Fisher’s exact test, when appropriate, were used for statistical analysis of categorical variables. Data were Statistical analyses were performed with SPSS software version 18 (SPSS, Chicago, IL). A P value less than 0.05 was regarded as indicating a statistically significant.
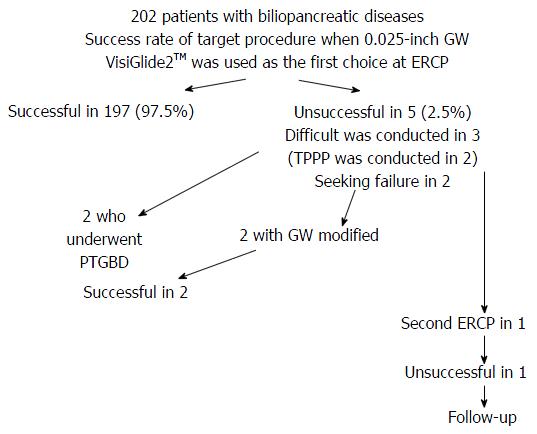
Comparisons of patient background and disease background are shown (Table 1). There was no significant difference between VisiGlide2TM and VisiGlideTM in the patient background. The accomplishment rate of procedure only with VisiGlide2TM was 97.5% (197/202). The procedural time was 23.930 ± 16.207 (4-65) min. Use of VisiGlide2TM enabled significantly to elevate accomplishment rate of procedure and shorten procedural time compared with VisiGlideTM (P < 0.05) (Table 2). Of patients who failed accomplishment of the procedure, GW was changed in 2 patients. Of 2 patients, the procedure was successful in 1 patient using RadifocusTM (RF-GS25263 TERUMO Japan), and the procedure was also successful in 1 patient using NaviproTM (Boston Scientific Corp. Natick, MA). Three patients had difficulty in selective bile duct insertion and 2 were acute cholecystitis patients to whom percutaneous transhepatic gallbladder drainage was inserted. One patient was clinically suspicious spontaneous passage of bile duct stone, and underwent unsuccessfully second ERCP, and followed-up. The final success rate of ERCP was 98.5% (199/202) (Figure 5). Among the patients succeeded in insertion into the bile duct and not undergoing papillary treatment, 74 patients underwent papillary treatment. The papillary treatment was successful in all the 74 patients conducted, the success rate of 100% (74/74) (Table 3). After papillary treatment, we underwent the procedure of purpose. The success rate was 99.4% (331/333) (Table 4). Accidental symptoms were observed at 3.0% (6/202). Bleeding, pancreatitis and perforation were observed at 1.0% (2/202), 1.5% (3/202) and 0.5% (1/202), respectively. Although there was no significant difference in accidental symptoms between VisiGlide2TM and VisiGlideTM, GW perforation, which was observed in 2.1% (4/194) when VisiGlideTM was used, was not found when VisiGlide2TM was used (Table 5). All the accidental symptoms were mild and conservatively alleviated.
| VisiGlide2TM | VisiGlideTM | P value | ||
| Sex | 122 males | 113 males | NS | |
| 80 females | 81 females | |||
| Age | 72.871 ± 11.403 (36-98) | 70.834 ± 11.824 (38-95) | NS | |
| Disease | Bile duct stone | 113 | 103 | NS |
| Cholangiocarcinoma | 31 | 26 | NS | |
| Chronic pancreatitis | 14 | 18 | NS | |
| Pancreatic cancer | 18 | 16 | NS | |
| Gallbladder cancer | 3 | 6 | NS | |
| Hepatolithiasis | 1 | 5 | NS | |
| Metastatic biliary obstruction | 5 | 5 | NS | |
| IPMN | 3 | 4 | NS | |
| Benign biliary stenosis | 4 | 3 | NS | |
| Acute cholecystitis | 5 | 3 | NS | |
| PSC | 2 | 2 | NS | |
| Postoperative bile leakage | 1 | 1 | NS | |
| Pancreaticobiliary maljunction | 1 | 1 | NS | |
| Duodenal papillary cancer | 1 | 1 | NS | |
| Target region | Bile duct | 190 | 180 | NS |
| Pancreatic duct | 12 | 14 | NS | |
| Stenosed lesion | Present | 90 | 77 | NS |
| Absent | 112 | 117 | NS | |
| Procedure | Scheduled ERCP | 157 | 155 | NS |
| Emergency | 45 | 39 | NS | |
| Purpose | Diagnosis | 10 | 14 | NS |
| Diagnosis + treatment | 15 | 9 | NS | |
| Treatment | 177 | 171 | NS | |
| Papillary treatment | None | 80 | 81 | NS |
| Post EST | 110 | 101 | NS | |
| Post EPST | 12 | 12 | NS |
| VisiGlide2TM | VisiGlideTM | P value | |
| Success rate | 97.5 (197/202)% | 92.3 (180/195)% | 0.034 |
| Procedural time (min) | 23.930 ± 16.207 (4-65) | 31.285 ± 19.122 (4-117) | 0.0001 |
| VisiGlide2TM | VisiGlideTM | ||||
| Papillary treatment | n | Success rate of procedure | n | Success rate of procedure | P-value |
| EST | 67 | 100 (67/67)% | 67 | 100 (67/67)% | NS |
| EST + EPLBD | 3 | 100 (3/3)% | 5 | 100 (5/5)% | NS |
| EPST | 3 | 100 (3/3)% | 3 | 100 (3/3)% | NS |
| EPBD | 1 | 100 (1/1)% | 4 | 100 (4/4)% | NS |
| Total | 74 | 100 (74/74)% | 79 | 100 (79/79)% | NS |
| VisiGlide2TM | VisiGlideTM | ||||
| Procedure conducted | n | Success rate of procedure | n | Success rate of procedure | P value |
| ENBD | 60 | 98.3 (59/60)% | 51 | 100 (51/51)% | NS |
| ENPD | 5 | 100 (5/5)% | 3 | 100 (3/3)% | NS |
| ENGBD | 5 | 80.0 (4/5)% | 1 | 100 (1/1)% | NS |
| EGBS | 2 | 100 (2/2)% | 1 | 0 (0/1)% | NS |
| EBS | 95 | 100 (95/95)% | 78 | 100 (78/78)% | NS |
| EPS | 30 | 100 (30/30)% | 22 | 100 (22/22)% | NS |
| EML | 2 | 100 (2/2)% | 2 | 100 (2/2)% | NS |
| Placement of MS | 12 | 100 (12/12)% | 8 | 100 (8/8)% | NS |
| Lithotomy | 88 | 100 (88/88)% | 69 | 100 (69/69)% | NS |
| Bile duct biopsy | 8 | 100 (8/8)% | 9 | 100 (9/9)% | NS |
| Pancreatic duct biopsy | 0 | - | 1 | 100 (1/1)% | NS |
| Peroral cholangioscopy | 2 | 100 (2/2)% | 1 | 100 (1/1)% | NS |
| IDUS | 10 | 100 (10/10)% | 6 | 100 (6/6)% | NS |
| Bile duct brushing cytology | 12 | 100 (12/12)% | 9 | 100 (9/9)% | NS |
| Pancreatic duct brushing cytology | 2 | 100 (2/2)% | 2 | 100 (2/2)% | NS |
| Total 333 99.4 (331/333) | Total 263 99.6 (262/263)% | NS | |||
| Guidewire type straight angle | 127 | 34 | NS | ||
| 75 | 0 | NS | |||
| VisiGlide2TM | VisiGlideTM | P value | |
| n = 202 | n = 194 | ||
| Bleeding | 2 | 4 | NS |
| Pancreatitis | 3 | 1 | NS |
| Perforation | 1 | 0 | NS |
| Guidewire perforation | 0 | 4 | NS |
| Total (%) | 6 (3.0%) | 9 (4.6%) | NS |
GW is essential in conducting ERCP-related procedures to ensure the stable procedure. The functions required for the roles are visibility, insertion performance, rigidity and torqueability. Various types of GWs are available; there are a variety of differences including difference in thickness, hardness, or tip shape[17,18]. As for actual use of GW, at first the procedure was performed with 0.035-inch GW, and for patients whose stenosis cannot be broken through with 0.035-inch GW or patients with difficulty in selecting the branch, GW was switched to accomplish the procedure. The ideal GW is the universal GW which can accomplish the procedure by itself. Therefore, we evaluated 0.025-inch GW VisiGlideTM (Olympus Corp. Japan) which has visibility and rigidity not inferior to those of 0.035 inch GW, retaining superiority of the conventional 0.025-inch GW in terms of stenosis breakthrough property and branch selectivity as the universal GW[13]. The success rate of procedure was very high. VisiGlideTM has a merit of thinness as 0.025-inches as well as good rigidity and visibility because of technical progress, which could be used for implementation of POCS which was difficult in the past and placement of MS with no problem. In addition to our reports, there appeared several reports using 0.025-inch GW VisiGlideTM for ordinary ERCP[19,20], which suggests that it may be one of choices as the first choice in using GW for ERCP. However, GW perforation was comparatively frequently observed, which is the problem to be improved hereafter[13]. Although it is reported that a few GW perforations are serious accidental symptoms which need operation[21], there is a report on portobiliary fistula from GW perforation, thus there is a possibility of progressing to a serious accidental symptom, and sufficient attention is required[20]. The core of 0.025-inch GW VisiGlide2TM is the same as that of 0.025-inch GW VisiGlideTM, however, the tip of GW is improved to be flexible, which can reduce the risk of GW perforation, retaining rigidity of GW. Previously the torque device for 0.025-inch GW VisiGlideTM was compliant to 0.035 inch, however, it was improved so that torqueability is elevated, and the torque device for 0.025-inch GW VisiGlide2TM has become compliant to 0.025-inch. The advantage to use 0.025-inch GW as the first choice lies in that the free space within the forceps port is increased when compared with 0.035 inch GW, which provides higher degree of freedom at the time of operation and, in addition, enables the use of various devices, and may elevate accomplishment rate of procedure or shorten the procedural time. Recently a cannulation method to use multiple GWs at the time of performing cannulation as the double GW technique is reported[2,3]. In such a case, use of 0.025-inch GW may improve operationality when compared with insertion of multiple 0.035 inch GWs. Although it is needless to say that GW to fix papillary edge must have rigidity to some degree, the thinner the diameter of GW is, the greater the freedom of the procedure becomes, thus accomplishment rate of cannulation may be elevated. In such a sense, if it has rigidity to some degree, there is sufficient significance in using 0.025-inch GW as the first choice.
This review compared 0.025-inch GW VisiGlideTM and 0.025-inch GW VisiGlide2TM. First of all, as for the procedure, the torque device for VisiGlide2TM has become compliant to 0.025-inch GW, thus torqueability was elevated, which led to elevation of seeking ability and enabled to accomplish the procedure using only one piece of GW, and furthermore, accomplishment rate of procedure was improved and procedural time was shortened.
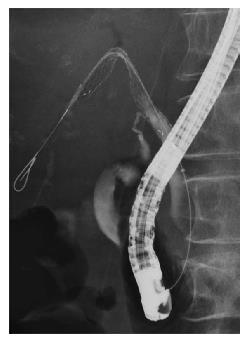
As mentioned above, MS placement was not so frequently performed using 0.025-inch GW because it does not have sufficient rigidity. However, emergence of 0.025-inch GW VisiGlideTM changed the situation drastically. Currently, 0.025-inch GW sufficiently enables placement of MS, though it depends on type of GW. 0.025-inch GW VisiGlide2TM used in this study, has no adverse consequence regarding placement of MS. Since patients who need placement of MS often have severe stenoses, it is advantageous to use 0.025-inch GW in terms of stenosis breakthrough. In addition, since 0.025-inch GW VisiGlide2TM has a sufficient rigidity, it is possible to place MS without changing GW after breaking through the stenosis. Previously, in placement of MS, if it is impossible to break through the stenosis using 0.035 inch GW, it was switched to 0.025-inch GW to continue the procedure, and when stenosis breakthrough succeeded, GW was switched again to 0.035 inch GW to perform MS placement. The procedure is very complicated. In placement of MS, use of 0.025-inch GW VisiGlide2TM may be more useful than use of 0.035 inch GW as the first choice similarly to 0.025-inch GW VisiGlideTM in terms of shortening of procedural time, and reduction in total cost of treatment. In the partial stent in stent with a MS, the procedure used in unresectable malignant hilar biliary obstruction, particularly, examination by accumulation of cases is required, but it is possibly useful. First of all, the tip of this GW has an excellent visibility under fluoroscopic control (Figure 3). Therefore, it has an advantage that the position of GW can be identified easily even if GW is placed within the contrasted intrahepatic bile duct. In conducting this procedure, usually, the procedure has been accomplished by using landmark GW, leading GW or seeking GW differently[9,10]. In this procedure, when GW is firstly placed, the GW of thin diameter is advantageous in the aspect of breaking through the stenosis. Multiple GWs are placed after breaking through the stenosis. It is considered that a thin GW with good visibility is ideal as a landmark GW. Because the rigidity is adequate, this GW is considered useful as a leading GW because there is no problem in induction of delivery of MS. In placing the next stent after placement of a stent, moreover, the thinner GW is of course more advantageous as a seeking GW in passing through the void of mesh. As described before, the GW has the rigidity possible to place MS as it is after passing through the void of mesh, and this GW is considered an ideal GW in conducting the partial stent in stent. If this GW is used, it will be able to accomplish the procedure without requiring preparation of the GWs of various characteristics. Recently there is a placement method termed side by side as MS placement for unresectable malignant hilar biliary occlusion[22]. This is the procedure to place MS by placing multiple GWs over hilar bile duct stenosis. In this case, visibility of GW placed in the intrahepatic bile duct is excellent, and in terms of breaking through the stenosis, GW of thin diameter is advantageous, thus this may be an ideal GW even in this procedure. The procedure which we must review in the future is the special procedure such as gallbladder drainage. This is the procedure to be performed for pathological evaluation in patients with suspected gallbladder cancer or in acute cholecystitis patients with hemorrhagic tendency for whom percutaneous approach is difficult[23,24]. Therefore, differently from ordinary drainage to the bile duct, chance of implementation is extremely few. According to the report so far, since the cystic duct is spirally-curved, in searching the cystic duct, GW with comparatively soft tip and high seeking ability such as RadifocusTM was comparatively frequently used[23,24]. This GW has a comparatively soft tip like RadifocusTM, and has a high rigidity as a whole. Therefore, in attempting an approach to the cystic duct, flexibility or thinness of the tip of this GW and rigidity of GW itself may make it work for the procedure in patients in whom stones are incarcerated within the cystic duct. This review showed that although sample size is small, accomplishment rate of procedure to approach the cystic duct was as high as 86% (6/7). It may be necessary to review again with a large sample size in the future. Incidence of accidental symptoms was 3.0% (6/202). As for accidental symptoms, there was no significant difference when compared with the results in use of 0.025-inch GW VisiGlideTM. Comparison with results using conventional GW showed that results of incidence of accidental symptoms were not so inferior. Although there was no significant difference, GW perforation was not observed in 0.025-inch GW VisiGlide2TM. 0.025-inch GW VisiGlide2TM has high rigidity, however, its tip is flexible, which may have reduced potentiality for occurrence of GW perforation. 0.025-inch GW VisiGlide2TM has an advantage enabling the treatment comparatively safely because its tip is flexible, so breaking through of the stenosis is often conducted in the situation forming a loop (Figure 5). As mentioned above, elevation of accomplishment rate of procedure or shortening of procedural time may be caused by discontinuation of the procedure due to GW perforation or no transferring to other procedure. This study suggested that use of 0.025-inch GW VisiGlide2TM did not develop GW perforation, and showed a low incidence of accidental symptoms as a whole, thus it may be used as a universal GW. If 0.025-inch GW can be used as a universal GW, it is expected that ERCP related treatment instruments such as the delivery sheath of MS with a thinner diameter will be developed in the future. It suggests a possibility to be more advantageous for stenosis breakthrough or others.
In conclusion, when 0.025-inch GW VisiGlide2TM was used for ERCP-related procedure as the first choice, it showed high accomplishment rate of procedure and low incidence of accidental symptoms, suggesting it can be used as the universal GW.
In endoscopic retrograde cholangiopancreatography (ERCP)-related procedures, it is needless to say that the guidewire (GW) is essential in performing the procedure safely, and elevating the accomplishment rate of the procedure. The authors decided to examine the accomplishment rate of procedures and the incidence of accidental symptoms in the use of 0.025-inch GW VisiGlide2TM as the first-choice universal GW in the ERCP-related procedures without selecting patients in a multicenter prospective study.
All the patients with biliary and pancreatic diseases, who were decided to undergo ERCP in 5 institutions participating in this clinical study in a month of December 2014, were included. A 0.025-inch GW (VisiGlide2: Olympus Corp. Japan straight type or angle type) was used. Prospective data collected in multicenter study were compared with those obtained from multicenter prospective study of 0.025-inch GW VisiGlideTM.
The accomplishment rate of procedure only with VisiGlide2TM was 97.5% (197/202). The procedural time was 23.930 ± 16.207 (4 to 65) min. Use of VisiGlide2TM enabled significantly to elevate accomplishment rate of procedure and shorten procedural time compared with VisiGlideTM (P < 0.05). There was no significant difference in accidental symptoms between VisiGlide2TM and VisiGlideTM.
All the patients with biliary and pancreatic diseases, who were decided to undergo ERCP.
0.025-inch GW VisiGlide2TM showed a high accomplishment rate of procedure and low incidence of accidental symptoms when used in ERCP-related procedures as the first choice.
This is a unique multicenter prospective study with a significant number of patients investigating an important topic, 0.025-inch guidewire VisiGlide2TM used for ERCP-related procedures as the first choice. The study results showed high accomplishment rate of procedure and low incidence of accidental symptoms. The results have a clinical impact on selecting the ideal guidewire that can accomplish the procedure by itself. This is a well-written article; the manuscript is concise, clear, comprehensive and convincing.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Boninsegna E, Malak M, Minami A, Tekin A S- Editor: Qi Y L- Editor: A E- Editor: Li D
| 1. | Nambu T, Ukita T, Shigoka H, Omuta S, Maetani I. Wire-guided selective cannulation of the bile duct with a sphincterotome: a prospective randomized comparative study with the standard method. Scand J Gastroenterol. 2011;46:109-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 2. | Herreros de Tejada A, Calleja JL, Díaz G, Pertejo V, Espinel J, Cacho G, Jiménez J, Millán I, García F, Abreu L. Double-guidewire technique for difficult bile duct cannulation: a multicenter randomized, controlled trial. Gastrointest Endosc. 2009;70:700-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 99] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 3. | Angsuwatcharakon P, Rerknimitr R, Ridtitid W, Ponauthai Y, Kullavanijaya P. Success rate and cannulation time between precut sphincterotomy and double-guidewire technique in truly difficult biliary cannulation. J Gastroenterol Hepatol. 2012;27:356-361. [PubMed] [DOI] [Full Text] |
| 4. | Youn YH, Lim HC, Jahng JH, Jang SI, You JH, Park JS, Lee SJ, Lee DK. The increase in balloon size to over 15 mm does not affect the development of pancreatitis after endoscopic papillary large balloon dilatation for bile duct stone removal. Dig Dis Sci. 2011;56:1572-1577. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Osanai M, Maguchi H, Takahashi K, Katanuma A, Yane K, Kaneko M, Hashigo S, Katoh S, Harada R, Katoh R. Safety and long-term outcomes of endoscopic papillary balloon dilation in children with bile duct stones. Gastrointest Endosc. 2011;73:619-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Jeong S, Ki SH, Lee DH, Lee JI, Lee JW, Kwon KS, Kim HG, Shin YW, Kim YS. Endoscopic large-balloon sphincteroplasty without preceding sphincterotomy for the removal of large bile duct stones: a preliminary study. Gastrointest Endosc. 2009;70:915-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 78] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 7. | Ichiya T, Maguchi H, Takahashi K, Katanuma A, Osanai M, Kin T. Endoscopic management of laparoscopic cholecystectomy-associated bile duct injuries. J Hepatobiliary Pancreat Sci. 2011;18:81-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Kitajima Y, Ohara H, Nakazawa T, Ando T, Hayashi K, Takada H, Tanaka H, Ogawa K, Sano H, Togawa S. Usefulness of transpapillary bile duct brushing cytology and forceps biopsy for improved diagnosis in patients with biliary strictures. J Gastroenterol Hepatol. 2007;22:1615-1620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Kawamoto H, Tsutsumi K, Fujii M, Harada R, Kato H, Hirao K, Kurihara N, Nakanishi T, Mizuno O, Ishida E. Endoscopic 3-branched partial stent-in-stent deployment of metallic stents in high-grade malignant hilar biliary stricture (with videos). Gastrointest Endosc. 2007;66:1030-1037. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Kawamoto H, Tsutsumi K, Harada R, Fujii M, Kato H, Hirao K, Kurihara N, Nakanishi T, Mizuno O, Ishida E. Endoscopic deployment of multiple JOSTENT SelfX is effective and safe in treatment of malignant hilar biliary strictures. Clin Gastroenterol Hepatol. 2008;6:401-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Naitoh I, Ohara H, Nakazawa T, Ando T, Hayashi K, Okumura F, Okayama Y, Sano H, Kitajima Y, Hirai M. Unilateral versus bilateral endoscopic metal stenting for malignant hilar biliary obstruction. J Gastroenterol Hepatol. 2009;24:552-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 155] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 12. | Kawakami H, Kuwatani M, Etoh K, Haba S, Yamato H, Shinada K, Nakanishi Y, Tanaka E, Hirano S, Kondo S. Endoscopic retrograde cholangiography versus peroral cholangioscopy to evaluate intraepithelial tumor spread in biliary cancer. Endoscopy. 2009;41:959-964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 76] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | Sakai Y, Tsuyuguchi T, Shimura K, Fujimoto T, Yoshida Y, Nishino T, Sakamoto D, Nakamura M, Nishino T, Sugiyama H. Can 0.025-inch guidewire VisiGlideTM become a standard in the ERCP-related procedures? -VIP study. Br J Med Med Res. 2014;4:2418-2430. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | OLYMPUS VisiGlide2. Case Report ERCP technical report (in Japanese). 2014, F0329J0-04. |
| 15. | Miura F, Takada T, Kawarada Y, Nimura Y, Wada K, Hirota M, Nagino M, Tsuyuguchi T, Mayumi T, Yoshida M. Flowcharts for the diagnosis and treatment of acute cholangitis and cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007;14:27-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [PubMed] |
| 17. | Sofuni A, Itoi T, Itokawa F, Tsuchiya T, Kurihara T, Ishii K, Tsuji S, Ikeuchi N, Tanaka R, Umeda J. Health insurance reward un Japan and devices in endoscopic procedures of pancreatobiliary disease (in Japanese). Tan to Sui. 2012;889-900. |
| 18. | Ayala JC, Labbe R, Moran M, Vera E. The loop tip wire guide: A new device to facilitate better access through the papilla. Gastrointest Endosc. 2007;65:AB236. [DOI] [Full Text] |
| 19. | Fujita N, Noda Y, Kobayashi G, Kimura K, Yago A. ERCP for intradiverticular papilla: two-devices-in-one-channel method. Endoscopic Retrograde Cholangiopancreatography. Gastrointest Endosc. 1998;48:517-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 63] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Itoi T, Itokawa F, Tsuchiya T, Kawai T, Moriyasu F. EUS-guided pancreatic pseudocyst drainage: simultaneous placement of stents and nasocystic catheter using double-guidewire technique. Dig Endosc. 2009;21 Suppl 1:S53-S56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Adler DG, Verma D, Hilden K, Chadha R, Thomas K. Dye-free wire-guided cannulation of the biliary tree during ERCP is associated with high success and low complication rates: outcomes in a single operator experience of 822 cases. J Clin Gastroenterol. 2010;44:e57-e62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 22. | Kawakami H, Kuwatani M, Kudo T, Ehira N, Yamato H, Asaka M. Portobiliary fistula: unusual complication of wire-guided cannulation during endoscopic retrograde cholangiopancreatography. Endoscopy. 2011;43 Suppl 2 UCTN:E98-E99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Itoi T, Sofuni A, Itokawa F, Kurihara T, Tsuchiya T, Moriyasu F, Yamagishi T, Serizawa H. Preoperative diagnosis and management of thick-walled gallbladder based on bile cytology obtained by endoscopic transpapillary gallbladder drainage tube. Gastrointest Endosc. 2006;64:512-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 24. | Itoi T, Kawakami H, Katanuma A, Irisawa A, Sofuni A, Itokawa F, Tsuchiya T, Tanaka R, Umeda J, Ryozawa S. Endoscopic nasogallbladder tube or stent placement in acute cholecystitis: a preliminary prospective randomized trial in Japan (with videos). Gastrointest Endosc. 2015;81:111-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 64] [Article Influence: 6.4] [Reference Citation Analysis (0)] |