Published online Jan 25, 2016. doi: 10.4253/wjge.v8.i2.86
Peer-review started: April 24, 2015
First decision: July 22, 2015
Revised: October 19, 2015
Accepted: November 24, 2015
Article in press: November 25, 2015
Published online: January 25, 2016
Processing time: 271 Days and 6.8 Hours
Peroral endoscopic myotomy (POEM) is an innovative, minimally invasive, endoscopic treatment for esophageal achalasia and other esophageal motility disorders, emerged from the natural orifice transluminal endoscopic surgery procedures, and since the first human case performed by Inoue in 2008, showed exciting results in international level, with more than 4000 cases globally up to now. POEM showed superior characteristics than the standard 100-year-old surgical or laparoscopic Heller myotomy (LHM), not only for all types of esophageal achalasia [classical (I), vigorous (II), spastic (III), Chicago Classification], but also for advanced sigmoid type achalasia (S1 and S2), failed LHM, or other esophageal motility disorders (diffuse esophageal spasm, nutcracker esophagus or Jackhammer esophagus). POEM starts with a mucosal incision, followed by submucosal tunnel creation crossing the esophagogastric junction (EGJ) and myotomy. Finally the mucosal entry is closed with endoscopic clip placement. POEM permitted relatively free choice of myotomy length and localization. Although it is technically demanding procedure, POEM can be performed safely and achieves very good control of dysphagia and chest pain. Gastroesophageal reflux is the most common troublesome side effect, and is well controllable with proton pump inhibitors. Furthermore, POEM opened the era of submucosal tunnel endoscopy, with many other applications. Based on the same principles with POEM, in combination with new technological developments, such as endoscopic suturing, peroral endoscopic tumor resection (POET), is safely and effectively applied for challenging submucosal esophageal, EGJ and gastric cardia tumors (submucosal tumors), emerged from muscularis propria. POET showed up to know promising results, however, it is restricted to specialized centers. The present article reviews the recent data of POEM and POET and discussed controversial issues that need further study and future perspectives.
Core tip: Submucosal tunnel endoscopy: Peroral endoscopic myotomy (POEM) and peroral endoscopic tumor resection (POET), constitutes a novel terrain for miniinvasive endoscopic treatment of diseases, where the surgical alternatives are totally incomparable, particularly in elderly. POEM showed exciting results in international level in treating all types of achalasia [classical (I), vigorous (II), spastic (III)], including advanced sigmoid type, failed surgical or laparoscopic Heller myotomy cases, and other esophageal motility disorders (diffuse esophageal spasm, nutcracker and jackhammer esophagus). POET was spawned from the success of POEM, and slowly expanded worldwide to treat muscularis based esophageal, esophagogastric junction and cardia submucosal tumors. Submucosal tunnel endoscopy further inspired other applications and opened promising future perspectives.
- Citation: Eleftheriadis N, Inoue H, Ikeda H, Onimaru M, Maselli R, Santi G. Submucosal tunnel endoscopy: Peroral endoscopic myotomy and peroral endoscopic tumor resection. World J Gastrointest Endosc 2016; 8(2): 86-103
- URL: https://www.wjgnet.com/1948-5190/full/v8/i2/86.htm
- DOI: https://dx.doi.org/10.4253/wjge.v8.i2.86
Peroral endoscopic myotomy (POEM)[1] is a novel, incisionless, minimal invasive endoscopic surgical procedure, which has been derived from the era of natural orifice transluminal endoscopic surgery (NOTES)[2], intended for long-term recovery from symptoms of esophageal achalasia.
POEM has successfully spread internationally, with more than fifty centers to have performed POEM worldwide[3], following the excellent initial results from pioneering centers[1,4] and definitely open the era of submucosal tunnel endoscopy in clinical practice. POEM has been extended to treat not only all types of esophageal achalasia [classical (I), vigorous (II) or spastic (III), Chicago classification[5]], but other spastic esophageal motility disorders as well[6-9].
There were modest variations among centers in technique and periprocedural management, which are currently under investigation, but all centers uniformly reported excellent efficacy and safety outcomes[3]. POEM has been also extended to include failure of previous therapies, such as botulin toxin injection (BTI) or pneumatic balloon dilatation (PBD)[10] or failed surgical or laparoscopic Heller myotomy (LHM)[11,12], advanced sigmoid-type achalasia[13-15], and also after failure of previous POEM[13]. Up to know more than 4000 POEM cases have been successfully performed worldwide, and currently there is an explosion of publications regarding POEM[3].
As an extension of the POEM technique and submucosal tunnel endoscopy, peroral endoscopic submucosal tumor resection (POET) is also introduced, and is currently increases in experience, however restricted to specialized centers[16,17].
Successful POET of esophageal and gastric SMTs is possible, due to direct access through the submucosal tunneling far from the mucosal entry, followed by successful mucosal closure even for inadvertent mucosal tunnel perforations with many techniques, such as standard clips, combined clip-endoloop technique[18], the over-the-scope clips (OTSC)[19], and finally the most recent technological progress of the endoscopic suturing device (OverStitch™; Apollo Endosurgery Austin, Texas)[20].
POET is far less invasive than the surgical alternatives, which are either gastrotomy or gastrectomy and esophagectomy for gastric and esophageal SMTs respectively, while POET can be also applied in case of contraindications or serious comorbidities[16]. However, further international experience with longer follow-up is necessary and awaited. Finally, POEM also opened other applications as well, such as endoscopic gastric pyloromyotomy for refractory gastroparesis[21].
The concept of endoscopic myotomy for treatment of achalasia, was first reported in case series in 1980[22], but it was only in 2008 when Inoue et al[1] performed the first successful clinical case of endoscopic myotomy in humans with achalasia, based on experimental data by Pasricha et al[23], Sumiyama et al[24] and Perretta et al[25]. Inoue et al[1] coined the term POEM and subsequently extended its use to treat not only achalasia, but other spastic esophageal motility disorders as well[26].
Currently, all types of symptomatic esophageal achalasia [classical (I), vigorous (II) or spastic (III), Chicago classification[5]] diagnosed by high quality (preferably high resolution) esophageal manometry[5] can be treated by POEM[27], including failure of previous therapies, such as BTI or PBD[10] or failed surgical or LHM[11,12], advanced sigmoid-type achalasia[13-15] and also after failure of previous POEM[3,13] (Table 1). POEM has been also reported in post-gastric bypass patients with achalasia[28].
| Indications |
| Absolute indications |
| Primary idiopathic achalasia of all types [classical (I), vigorous (II), spastic (III)] (Chicago |
| Classification) |
| Relative indications |
| Other hypertensive motor disorders (diffuse esophageal spasm, nutcracker or jackhammer esophagus). HRTM necessary |
| Failed surgical myotomy (POEM at the opposite site manly posterior POEM) |
| Failed pneumatic balloon dilatation |
| Failed previous POEM. Redo POEM at the opposite site mainly posterior POEM necessary |
| Advanced sigmoid type achalasia with mega esophagus (bilateral POEM may be necessary) |
| Children with achalasia (relative indication in experienced hands and specialized centers only) |
| Elderly with achalasia and comorbidities and non-surgical candidates (relative indication in experienced hands and specialized centers only) |
| Contraindications |
| Absolute contraindications |
| Severe cardiopulmonary disease or other serious disease |
| Pseudoachalasia |
| Failure in creating the submucosal tunnel because of severe fibrosis and adhesion |
| Relative contraindications |
| Severe esophagitis and/or very large ulcer in the lower esophagus |
| Recent endoscopic treatment such as EMR, ESD |
According to international IPOEMS database 43% of subjects had prior intervention such as PBD, BTI or LHM[3]. Previous therapies make POEM technically more challenging due to the presence of inflammatory fibrosis, adhesions and scars[12].
Maselli et al[29] also reported the first successful clinical case of POEM in a 3-year-old child with achalasia and Down syndrome, while lately other groups also reported POEM in children and adolescents[30,31], making age, no limitation for POEM. Currently, the pioneer centers[1,11] have no exceptions when considering the application of the POEM.
Moreover, Inoue first extended the indications of POEM to other spastic esophageal motility disorders, such as diffuse esophageal spasm, nutcracker, and jackhammer esophagus[7,8,32]. According to international survey (IPOEMS), 28% of the reported POEMs performed for other esophageal motility disorders, than achalasia[3]. In these disorders POEM permitted the longer myotomy required, which cannot be achieved via the laparoscopic approach[6-8,32].
POEM contraindications, according to the consensus, include severe pulmonary disease, esophageal irradiation, esophageal malignancy, bleeding disorder, including coagulopathy and recent esophageal surgery or endoscopic intervention, including endoscopic mucosal resection and endoscopic submucosal dissection (ESD)[3].
POEM starts with a mucosal incision, followed by submucosal tunnel creation crossing the EGJ and myotomy inside the tunnel and away from the mucosal entry. Finally the mucosal entry is closed with endoscopic clips. The equipment required for POEM are the same used for ESD, while carbon dioxide insufflation is obligatory through the entire procedure.
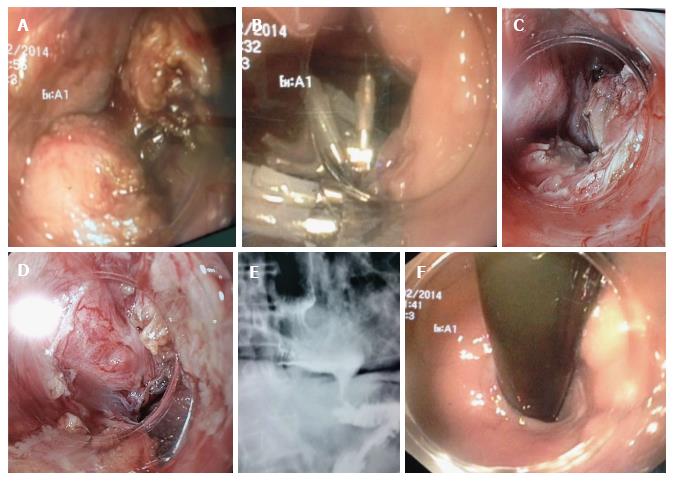
It is recommended to use spray catheter for reinjection or the injection needle to remain inside the plastic sheath, to prevent damage to the muscular layer or to mucosal flap. The width of the tunnel should be about one-third of the circumference of the esophagus. A challenge with POEM concerns the identification of the EGJ while in the tunnel, which is discussed below. At the completion of myotomy smooth passage of the endoscope through the EGJ provides confirmation of complete myotomy. Figure 1 demonstrates the critical steps of POEM.
One day postoperatively, gastroscopy and esophagogram should be routinely performed to confirm mucosal integrity and exclude complications. Adequate esophageal empty controls the efficacy of myotomy and enables oral intake. In uncomplicated cases, patients begin by drinking liquid on day 1, a soft diet on postoperative day 2, and a normal diet on postoperative day 3, while an intravenous infusion of antibiotics should be delivered for one to three days after POEM, followed by an additional four days of oral antibiotics.
The debatable issues of POEM that need further clarification are presented in detail below (Table 2).
| TT-knife vs ERBE knife vs other knives |
| Posterior vs anterior myotomy vs bilateral myotomy |
| Selective circular vs full thickness myotomy |
| EndoFLIP technique vs classical tricks to evaluate adequacy of myotomy |
| Mucosal closure clips vs OverStitch |
| POEM vs LHM or surgical myotomy |
| GERD after POEM (treatment necessary, e.g., antireflux procedure, PPIs?) |
| Training system for POEM |
| How the risk of mishaps related to POEM can be diminished? |
Currently, an important issue for discussion regarding POEM is: Which knife should be used? Inoue et al[1] introduced the triangular TT-knife, that has the advantage of permitting selective dissection of the circular muscle layer, which is the responsible muscle for achalasia, while the thin outer longitudinal muscle may remain as intact as possible, as another safety margin from mediastinum and as a guide to keep a correct dissection plane.
The flat triangular base of the TT-knife is safely touched to the longitudinal layer permitting catching and selective dissection of circular muscle bundles, while lowering the risk of damage to surrounding structures, particularly for inexperienced operator (Figure 1E).
Other knives have been also successfully used for POEM, with the Water-jet (WJ) and ERBE knives the most competitive to TT-knife[33]. They have the advantage of flushing during POEM, which, according to single center, comparative studies, resulted in shorter procedure time, mostly due to less replacement of accessories and permitted full-thickness myotomy[33,34]. The authors comparing WJ to TT-knife also reported larger injection volume and fewer bleeding episodes with WJ, which attributed to easier reinjection[33,34]. However, reinjection is important only during submucosal tunnel creation and not during myotomy, which is the most important and durative part of POEM.
Lastly, a simple and efficient modified POEM technique using TT-knife and a new method of injecting dyed saline through an integrated water jet channel, to avoid exchanging the knife for a spray catheter, which is time consuming, has been described[35].
As POEM is an innovative technique, operating time is not anymore a taboo, while the significant time variation between different groups and within the same group related to obvious inhomogeneity of achalasia patients and irrespective of the knife used, made comparative studies difficult.
In contrary, while TT-knife permits also full-thickness myotomy, selective circular myotomy is more difficult using WJ or ERBE knife, because of the round tip of the knife that does not permit easy catching of individual muscle fibers. These knives are found more appropriate to perform intentional full-thickness myotomy, although not necessary, for treating achalasia.
To our knowledge there is no sufficient international independent data, comparing different knives and up to know no knife has been proved to be more efficacious, although the largest international experience is with the less expensive TT-knife in terms of safety and efficacy.
High frequency electrosurgical energy generator (V/O 300D ERBE; Tubingen, Germany) that enables a spray-coagulation mode with noncontact tissue dissection was the standard preference of Inoue et al[1] for both submucosal tunneling and myotomy during POEM. The spray-coagulation mode makes the submucosal dissection during tunnel creation much easier, faster, and with less bleeding. Settings can be individually adjusted during the operation.
However, other coagulation modes (i.e., forced coagulation) are also acceptable during submucosal dissection and myotomy, with comparable quality to spray coagulation, in terms of safety and efficacy during POEM with excellent results.
After frequent serious complications with room air, the POEM groups have been converted to exclusively carbon dioxide insufflation during POEM[1]. Currently, CO2 gas insufflation through the endoscope, during POEM, in concordance to laparoscopic techniques, is mandatory not only to reduce mediastinal emphysema, but also to reduce the risk of air embolization.
Intratracheal intubation with positive pressure ventilation should be maintained at higher pressures than those generated by endoscopic CO2 insufflation, to reduce the risk of mediastinal emphysema during submucosal endoscopy[26,27]. Mild subcutaneous emphysema, mediastinal emphysema or pneumoperitoneum after POEM, however, should not be considered as complications but as part of this procedure in concordance to pneumomediastinum or pneumoperitoneum after laparoscopic surgery.
One of the major concerns during POEM was how deeply the muscle layer should be divided. In surgical myotomy, full-thickness myotomy is performed, as the surgeon cut from outside first the external longitudinal muscle layer to approach the inner circular muscle layer.
In initial series of POEM performed by Inoue et al[1] and subsequently by other groups[36-39], muscle cutting was intended to dissect only the circular muscle bundles, which is the responsible muscle for achalasia, while the thin longitudinal muscle layer was left intact as a safety margin between submucosal space and mediastinum.
Full-thickness myotomy is not necessary for treating esophageal achalasia and other esophageal motility disorders, and selective circular myotomy can solve the problem, according to excellent results from more than 3000 selective circular POEM cases. So intentional full-thickness myotomy is not recommended to treat achalasia and other esophageal motility disorders.
However, complete true selective circular myotomy is not possible as longitudinal muscle bundles are naturally thin enough to be widely stretched and split each other during POEM, only by mild compression of the endoscope tip, creating partially full-thickness gaps, without clinical relevance or consequences[26].
With the increasing experience in POEM and the development of sophisticated endoscopic techniques for closing mucosal gaps, some specialized centers performed intentionally full-thickness myotomy, even for achalasia, although not necessary[40,41]. However, no significant difference to selective circular myotomy was found in all parameters studied (symptom relief, procedure related parameters, manometry) except of reduced procedure time in the group of full-thickness myotomy.
In terms of safety however, nobody knows the real risks of potential complications in inexperienced hands and the consequences of the severe capnomediastinum and capnoperitoneum, following full-thickness myotomy than selective circular myotomy. Moreover, the gastroenterologist who performs POEM is not familiar to mediastinal anatomy and may have higher risk of complications, such as making accidental injuries to structures beyond the esophageal wall.
However, full-thickness myotomy opened new perspectives in the era of NOTES for further investigation, as structures beyond the esophageal wall, such as mediastinum and retroperitoneum are directly endoscopically accessible and also structures, such as the angle of His and vagus nerve[42] may be recognized during POEM. Potential future endoscopic procedures could be endoscopic retroperitoneoscopy or mediastinoscopy in a similar fashion to laparoscopy and thoracoscopy. However, these areas need further investigation.
Myotomy length in POEM is also another controversial issue for discussion. POEM permitted control of myotomy length to be as long as we wish, and achievement of longer myotomy than any surgical myotomy[8,26]. In initial POEM cases, a relatively short myotomy was performed, however long enough to achieve complete release of high LES pressure and resolve achalasia symptoms. Based on clinical results, the recommended myotomy length during POEM should to be a minimum of 7 cm, with 2 cm gastric extension.
With the introduction of high resolution topographic manometry (HRTM)[43] and Chicago classification[5], achalasia is accurately classified in three major groups, which permitted better pre-POEM evaluation of these patients.
Based on these manometric studies, patients with type II (vigorous, panesophageal pressurization) and III (spastic) achalasia, with chest pain because of spasm and/or another high-pressure zone, or other mixed esophageal motility disorders, such as diffuse esophageal spasm, nutcracker and jackhammer esophagus[7-9], longer myotomy of more than 7 cm is necessary for appropriate symptom resolution.
Khashab et al[9] recently reported the international multicenter experience from 73 patients with spastic esophageal disorders with mean myotomy length 16 cm and maximum up to 25 cm. However, myotomy length should be individualized, based on HRTM results before POEM.
According to the consensus from IPOEMS and other studies, POEM has significant efficacy in nutcracker esophagus, hypertensive LES, diffuse esophageal spasm and type III (spastic) achalasia, because in those disorders often a longer myotomy is required than cannot be achieved via the laparoscopic approach[3,6,7].
Another fundamental issue in POEM is the extension of myotomy beyond the EGJ about 2-3 cm at the gastric side. So identification of the EGJ in the submucosal space during POEM has significant importance. As clear markers for identifying the EGJ, should be checked: (1) the insertion depth of the endoscope from the incisors; (2) a marked increase of resistance when the endoscope approaches the EGJ, followed by a prompt easing when the endoscope enters the gastric submucosal area; (3) the working space in the submucosal tunnel becomes gradually narrower when the endoscope approaches closely to the LES; (4) endoscopic visual identification of palisade vessels in the submucosal layer (Figure 1C); (5) a change of vasculature in the submucosal layer in the esophageal submucosal space few vessels are observed, while gastric submucosal vasculature suddenly becomes rich looking like a spider web and finally; and (6) the ectopic innermost longitudinal muscle bundles in front of the circular muscle layer at the level of the EGJ, finding in more than 30% of cases[44].
Tattooing at the gastric cardia using indocyanine green (ICG) before POEM is reported to be one trick for identifying EGJ during POEM by recognition of the green dye at the EGJ within the submucosal tunnel[32]. However, tattooing may be impractical, time consuming, and confusing particularly in sigmoid type achalasia with dilated and helicoid esophagus. However, this issue may need further study.
Ensuring that the submucosal tunnel stays in line with the esophagus is another issue with significant importance, especially in esophageal motility disorders with tight contractions during POEM and sigmoid and dilated esophagus. There is little data regarding orientation during submucosal tunneling, and although this issue is very important it is not included in up-to-date protocols.
According to Inoue et al[26], when the cap-fitted endoscope introduced into the submucosal space and then pushed, tends to advance only in line with the esophagus and its round tip tends to move to the center of the elliptical cross-section of the submucosal tunnel.
However, this is not always the case, especially during anterior myotomy to the lesser gastric curvature, because there are no objective markers to sustain correct direction and inexperienced endoscopists may easily loose the orientation, when they are inside the submucosal space (tornado tunnel).
Orientation within submucosal space may be easier during posterior myotomy to the greater gastric curvature because the existence of more objective guiding anatomic markers, such as the ankle of His, and the compression from the spinal cord[13]. However this issue needs further confirmation in comparative studies.
Another question regarding POEM, is on which side myotomy should be done? In initial POEM cases, Inoue et al[1] performed anterior myotomy, to avoid damage to the angle of His and sling muscle bundles that are located at opposite direction at the greater gastric curvature, which might be a natural barrier to postoperative reflux of gastric contents. Since then anterior myotomy has been established and accepted by most endoscopists worldwide[36-39]. In fact, the International Peroral myotomy survey (IPOEMS), showed that 14 of 16 centers preferred the anterior approach[3].
Alternatively, posterior myotomy at 5 o’clock position, leading to the greater gastric curvature, is a promising safe modification of the POEM technique, with high rates of technical and clinical success, according to few centers[13,45]. Posterior myotomy has the theoretical advantage of easy access to EGJ and better orientation within the submucosal tunnel, because of spinal cord and the ankle of His[13].
Moreover, anterior myotomy is precluded by previous procedures such as failed surgical Heller myotomy or by other anatomic considerations that obscure the normal dissection planes[12,13]. Also, in patients with advanced sigmoid type achalasia with megaesophagus, the identification of the EGJ may be difficult during anterior myotomy, resulted in an incomplete gastric myotomy and poor symptom relief[13].
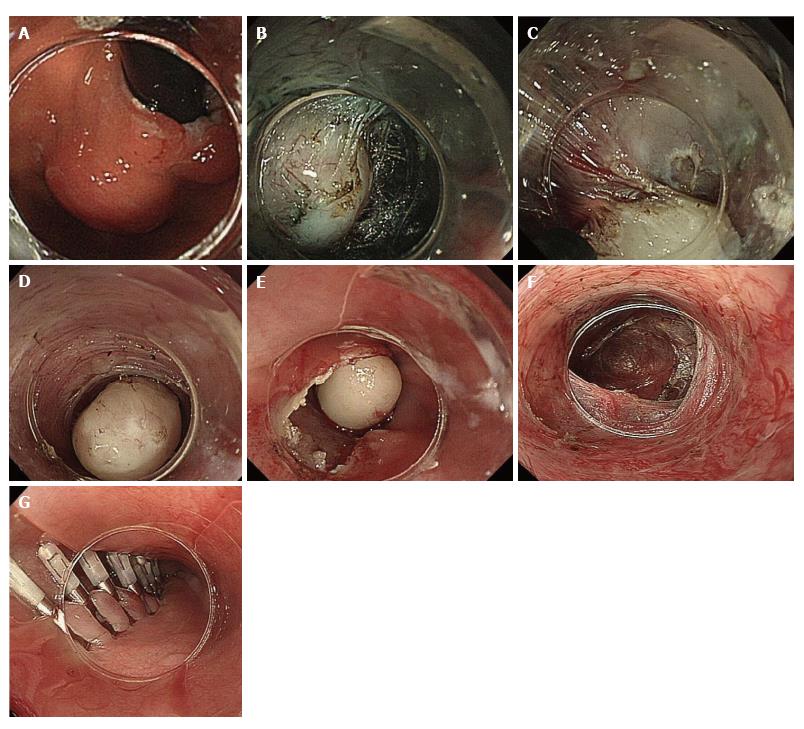
Posterior myotomy may be especially useful in cases of redoPOEM[32], POEM post-Heller myotomy[11,12] or when the EGJ is difficult to recognize because of supervening anatomic constraints or in sigmoid type achalasia with megaesophagus (Figure 2)[15]. However, no comparative studies have been yet published. A multicenter prospective single blind randomized clinical trial is currently underway, to investigate the optimal technique to myotomy (anterior vs posterior approach) for POEM.
Maintaining the integrity of the mucosal flap and the reliable closure of the mucosal entry during POEM is paramount in preventing leakage of esophageal contents into the mediastinum. Most centers employ clips for closure of the mucosal entry of the tunnel[1,36-39]. When a completion of the closure with standard clips is unsuccessful, the combined clip-endoloop technique has been successfully applied, comparable to endoscopic full-thickness resection in other areas of the GI tract[18].
Alternatively, in failed cases, successful mucosal closure has been reported with the OTSC in two POEM cases[19], and fibrin sealant[46], however these techniques are more expensive.
There are also few groups who have also successfully used an endoscopic suture device (OverStitch™ Endoscopic Suturing System; Apollo Endosurgery Austin, Texas) for closure of inadvertent mucosal tunnel perforations, particularly for mucosal flap injuries at the EGJ[20]. These groups[11,20] are also more comfortable with full-thickness myotomy, because they have the possibility to close any perforation either by clipping or by suturing. They reported on 25 mucosal closures without statistically significant differences in closure time, complications or mean costs[34], however these results are debatable. Moreover, there are no comparative studies between different methods of mucosal closure, also regarding the cost-effectiveness.
During POEM the endoscopist is able to immediately assess the adequacy and completeness of myotomy by passing the endoscope through EGJ at the end of the procedure[26]. The rationale of POEM is to extend myotomy 2-3 cm to the gastric side in order to cut all responsible for achalasia, circular muscle fibers at the EGJ. However, endoscopic measurements of adequate myotomy are subjective and empirical, often imprecise and may be affected by many biases.
Some POEM groups assess the EGJ distensibility quantitatively, immediately at the end of the procedure, with the EndoFLIP (Endoluminal Functional Lumen Imaging Probe) system, trying to objectively confirm the adequacy of myotomy, however without clear results and no real benefit[47,48]. The EndoFLIP (Crospon Ltd., Galway, Ireland) system, uses impedance planimetry for real-time measurements of the EGJ diameter, through a specific balloon-tipped catheter[48].
The rationale of the EndoFLIP use during POEM is that the possibility to measure the diameter of the EGJ before and after POEM may reveal cases of incomplete myotomy, before the closure of mucosal entry as it was the case in one patient reported by Familiari et al[48]. The endoscope was inserted again in the submucosal tunnel and additional muscular bundles were cut at the EGJ.
According to these studies, EndoFLIP was found to be potentially useful during LHM, but no real benefit was proved in POEM cases[48,49]. Obviously, the effects of myotomy on the diameter of EGJ are often unpredictable and not really controllable with POEM. Some authors studied the EndoFlip technique, concluded that EndoFLIP during POEM may be impractical and the real role, if any, should be evaluated in further multicenter studies[48]. To our opinion EndoFLIP may be confusing, time consuming, troublesome, especially in advanced, sigmoid type achalasia and costly.
Sigmoid type achalasia subdivided into S1 and S2 subtypes based on radiological signs on computed tomography. In S1 achalasia, the esophageal lumen is tortuous, but the direction is still downward. S2 type is an extremely advanced sigmoid form, where the esophageal lumen is tortuous and turns upwards[1].
Sigmoid type 2, (S2) was initially considered as an exclusion criterion for POEM. In this very advanced form of achalasia, the maximal tortuosity of the esophageal lumen does not allow smooth food passage, which occurs by gravity when the patient is upright. It was hypothesized that simple myotomy could not relieve symptoms and straightening of the curved esophagus was recommended in addition to laparoscopic myotomy[1].
However, based on the excellent initial results, Inoue et al[1] first proceeded to successful POEM in 9 patients with sigmoid-type achalasia, and reported them in his initial publication[1]. Since then other groups also reported successful POEM in advanced sigmoid achalasia[14,15,50].
Currently sigmoid type of achalasia is not yet considered as a contraindication for POEM, although it may produce even more technical difficulties, especially in remaining perpendicular to circular layer during myotomy. Moreover, in advanced sigmoid type (S2) achalasia, which is usually presented in advanced age, with multiple co-morbidities, and contraindications for major surgery such as esophagectomy, and with a history of potential multiple previous therapies, such as PBD or even surgery, POEM may be the only available therapy. In these advanced sigmoid type (S2) achalasia, with potential extremely thick circular muscle layer, posterior or bilateral POEM[15] (Figure 2), may be the more appropriate approach, however without definite literature data. Further international experience in this specific subgroup is necessary and is awaited.
Although surgical or LHM resulted in good-excellent long-term results in 90% of achalasia patients, failures do occur[51]. According to Gockel et al[51] the most common causes of surgical myotomy failures are persistent achalasia or early recurrence due to inadequate or incomplete myotomy; early scarring or fibrosis; early fusion or healed myotomy; while other causes are tight fundoplication; peptic stricture due to gastroesophageal reflux (GERD); late recurrence due to progression to advanced sigmoid megaesophagus; diffuse esophageal spasm; progression to esophageal cancer; and others.
Treatment of failed surgical myotomy is a challenging, difficult urgent problem, with controversial data[51]. Redo Heller myotomy has lower efficacy and more postoperative complications, because it is more technically demanding due to the presence of adhesions, fibrosis, and scars from previous surgery according to Wang and Li[52].
Onimaru et al[12] and Zhou et al[11] reported successful rescue POEM on 10 and 12 achalasia patients respectively, with persistent or recurrent symptoms after previous surgical myotomy, with excellent (> 90%) short-term results and without complications.
Both LES resting pressure and symptom score were improved in short-term. The authors have not encountered any difficulties in extending the adequate POEM myotomy down to the stomach because of the presence of fundoplication.
In the rescue POEM, myotomy was performed at the axis opposite to the previous myotomy (mainly posterior axis), to avoid facing scars and submucosal fibrosis from previous surgery. In cases which the axis of previous surgical myotomy could not be clearly identified, myotomy was made at the standard 2 o’clock axis at the proximal esophagus and then rotated to a different axis at the area of the EGJ[12]. Rescue POEM, however, is highly demanding procedure compared to standard POEM and may be better performed by experts.
As the positive international experience with POEM increases, with explosion of international centers performing POEM, there is a criticism in the literature regarding the superiority of POEM to alternative standard 100-year-old surgical or LHM[53]. One of the major arguments for surgical myotomy is that “the approach is outside the mucosa”[54]. However intact mucosa is not any more a “taboo” in the modern era of NOTES as mucosal gap can be safely and effectively closed after the procedure, according to excellent results from more than 4000 POEM cases worldwide, up-to date[1,3,4,36-39]. Moreover, with surgery anatomical structures around EGJ are permanently cut and mobilized, and LHM should always be accompanied with partial fundoplication due to risk of severe GERD. Advantages and disadvantages of POEM vs LHM are presented in Table 3.
| POEM | LHM | |
| Advantages of POEM | ||
| Myotomy length | Longer myotomy up to 25 cm | Short myotomy maximum 6 cm |
| Minimally invasive method | Invasive (major surgery) | |
| Hospitalization | Less hospitalization (1-5 d) | Longer hospitalization > 5 d |
| Myotomy depth | Selective circular myotomy possible | Only full-thickness myotomy |
| Other esophageal motility disorders | Effective for esophageal spasm, nut cracker and jackhammer esophagus | Combined laparoscopic and thoracoscopic approach is necessary to obtain equivalent myotomy |
| Sigmoid achalasia | Effective in all types of achalasia even in end-stage, sigmoid type (S2) achalasia with megaesophagus | Major surgery such as esophagectomy may be necessary |
| Elderly patients | Effective in elderly with comorbidities and contraindications | Contra indication for surgery |
| In failed surgical | POEM after failed surgical myotomy is effective | Redo-surgery often with high rates of failure and complications |
| Cost | Lower hospitalization and lower cost | Higher cost in combination to surgical procedure |
| GERD | Less common and lower severity. No antireflux procedure (fundoplication) necessary at the moment. Further study necessary | Fundoplication necessary and routinely performed Complications from fundoplication |
| Does not preclude surgery | POEM more difficult after LHM | |
| Bilateral POEM possible | ||
| Disadvantages of POEM | ||
| POEM | Surgery | |
| Follow-up | Short follow-up (novel technique) | Longer follow-up |
| POEM restricted to specialized centers | Common surgical or laparoscopic procedure overall available | |
| Training | Difficult (no so many centers) | Overall available |
Furthermore, POEM permitted endoscopists to approach and cut the responsible muscle of achalasia (the circular muscle layer at the EGJ), through the submucosal space with the most delicate mode, leaving the surrounding structures intact[1].
Few non-randomized studies[53,55-57] exist comparing POEM to LHM, with conflicting results[55]. A recent meta-analysis of comparative studies between LHM and POEM showed equivalent short-term outcomes and similar results for adverse events, perforation rate, operative time and a non-significant trend toward a reduced length of hospital stay in the POEM group[54,58].
Further, randomized comparative studies of LHM and POEM are required. However, conducting studies comparing a novel endoscopic procedure mainly performed by gastroenterologists to a standard LHM performed exclusively by surgeons, in a population of achalasia with large inhomogeneity regarding type, stage and severity are extremely difficult.
All studies comparing POEM to LHM have not focused to specific subgroups of achalasia patients, i.e., end-stage achalasia, with sigmoid type and megaesophagus with contraindications for major surgery. In these particular cases, as well as in other mixed esophageal motility disorders, POEM is the potential only acceptable treatment, according to up-to date positive experience[11,13,15,26]. The exciting results from POEM make objective, comparative studies to LHM difficult, with many ethical issues also emerged.
Failure of POEM to control achalasia symptoms, does not exclude future surgery (LHM), because POEM does not involve adjacent tissues surrounding the lower esophagus[13].
The most common causes of POEM failures are persistent achalasia or early recurrence due to inadequate or incomplete myotomy; end-stage, sigmoid type (S2) achalasia with megaesophagus, where one side (mainly anterior) myotomy is not sufficient and overlooked mixed esophageal motility disorders that need longer myotomy[13]. In these failed POEM cases, redo-POEM at the opposite (posterior) direction is recommended and it has been successfully reported[13]. Longer follow-up, with greater number of patients and further studies focusing on failed POEM are necessary.
Acute or late POEM related complications varied greatly among different reports[59] (Table 4). According to recent pooled analyses, minor complications include: Gas-related complications, such as capno/pneumoperitoneum (30%), subcutaneous emphysema (32%), and capno/pneumomediastinum (10%-22%)[39,58-60]. Major operative adverse events include tunnel mucosal perforation resulted to mediastinal or peritoneal leak, acute peritonitis, pleural effusion, GI fistula (0.3%), postoperative bleeding (1.1%) and a single death (1/4000 POEM cases, 0.025% mortality)[58].
| Common complications |
| Gas-related complications (minor) |
| Subcutaneous emphysema (31.6%) |
| Capno/pneumomediastinum (10%-22%) |
| Capno/pneumothorax (11%) |
| Capno/pneumoperitoneum (30.6%)[58] |
| Mucosal injury-perforation (mediastinal or peritoneal leak) (0.3%) (major) |
| Mediastinitis (insufficient data) |
| Peritonitis (insufficient data) |
| Retroperitoneal abscess (2 proved cases reported) |
| Pleural effusion (insufficient data) |
| Pneumonitis (insufficient data) |
| GI fistula (insufficient data) |
| Fever (temperature > 38 °C) |
| Severe postoperative pain |
| Rare complications |
| Delay postoperative bleeding (1.1%) |
| Hematoma within the tunnel |
| Submucosal infection |
| Mortality (0.025%) (Single death/4000 POEM cases) |
Major bleeding in the tunnel is unusual but may require reentry for hemostasis, longer hospitalization time or even blood transfusion[29,46,61]. Post-POEM reflux esophagitis reported in 19% of patients, although there is controversy in the literature regarding incidence and severity of post-POEM GERD[58].
Minor pneumomediastinum, or mild subcutaneous emphysema, just after POEM, could be as high as 100%, with incidence between 10%-22%[39,59,60], however, without clinical significance or requirement of special treatment, and should not be considered as a complication. This phenomenon should be considered similar to the pneumomediastinum seen post thoracoscopic surgery or post-ESD[26,60,62].
However, gas-related complications may cause discomfort, which is usually relieved through conservative treatment, while in more severe cases vast gas accumulation may occur in the chest, abdominal cavity, mediastinum or under the skin, while acute respiratory and circulatory failure may occur. In such setting emergency invasive interventions of deflation via subcutaneous puncture and if necessary closed thoracic drainage should be taken for symptom relief[26,41,45].
Severe pneumothorax (up to 2.5%[45]) need chest tube placement, reported in the very early series of POEM[4], when air was insufflated instead of carbon dioxide gas, while thereafter no such severe complication is reported, at least from pioneering centers[6,11,15].
Furthermore, despite the theoretical dangerous “downside”, according to centers with large number of POEM cases, although long myotomy have been performed up to 25 cm[8], no clinically severe mediastinitis has been reported at the moment[4,11,26].
Selective circular myotomy is preferred by most researchers trying to preserve longitudinal muscular layer in order to reduce the chance of gas entry into the thoracic and abdominal cavity. Full-thickness myotomy, however did not increase the occurrence of gas-related complications, although further studies are necessary[41].
Sigmoid-type esophagus was found to be independent risk factor for the occurrence of gas related complications, due to esophageal twisting, which might form a state of high pressure within the tunnel, so as to cause such complication as subcutaneous emphysema, pneumothorax and pneumoperitoneum[59].
Mucosal tear during POEM, particularly at the high-pressure zone of the EGJ or cardia, which are considered as true perforations, have been also reported (0.3%), particularly in early POEM series[4,12,26,32,58]. These complications were usually treated conservatively with observation, prolonged fasting and longer intravenous antibiotic therapy. In two cases with sub diaphragmatic abscess, external drainage was necessary, with optional outcome thereafter.
The mucosal defects have been adequately closed by multiple clips[12,26,32], fibrin sealant[46], or by the clip-endoloop technique[18] and lately by endoscopic suture device (OverStitch™ Endoscopic Suturing System; Apollo Endosurgery Austin, Texas)[20]. Temporary dysphagia is also reported in one patient after multiple clipping at the EGJ[26].
According to International POEM group, only a single, unpublished[58], POEM related death is currently reported and outside from the large POEM volume Asian centers, that reported no deaths[32,50]. So, POEM related mortality at the moment, is estimated to be 0.025% (one out of 4000 POEM cases globally). However, POEM related mortality should be compared to mortality of the surgical alternatives, which are the surgical, or LHM. According to recent (2015) study on national outcomes, the mortality rate of LHM was (4/1237) 0.3%[63] (almost 10-times more than POEM), with 2.4% major complications, 3.1% readmissions and 2.3% reoperation[63].
Moreover, the existing international experience from great number of patients, showed that POEM is a totally safe procedure, applied safely and effectively to all age spectrum from children to octogenarians, and also to patients with severe co-morbidities and contraindications for surgery[1,36-39,45,59,64,65]. However, future prospective, randomized, comparative, multicenter studies, on POEM related complications, also focusing on 30-d mortality rate after POEM (procedure and not procedure related), are necessary and awaited.
LHM is routinely accompanied by antireflux procedure, to prevent postoperative GERD, because the natural antireflux mechanisms are impaired, while in POEM no antireflux procedure is recommended, since the hiatal attachments are left untouched and the flap-valve mechanism intact[1].
Theoretically to minimize the risk of post-POEM reflux, anterior myotomy has been recommended, to avoid damage to the angle of His, and the oblique muscle layer of the EGJ, which are natural barriers to postoperative gastric reflux, located posterior laterally[1]. Sigmoid-type esophagus was found to be independent risk factor for the occurrence of GERD after POEM[59].
There are controversial results regarding post-POEM GERD, with incidence varied between 5%-46% in published series[3,4,12,32,36-39,45,53,61,64,66] (Table 5). Inoue et al[1] and other initial multicenter studies[1,36-39,45,59], reported no symptomatic or mild endoscopic (LA grade A) post-POEM GERD, and concluded that GERD is minor or no problem after POEM. In contrary, according to a recent European multicenter study, GERD was the most common adverse event after POEM, with esophagitis diagnosed in 42% of patients, though usually mild[60].
| Ref. | Patients (n) | Mean age (yr) | Eckardt score (pre/post) | LES pressure (pre/post) (mmHg) | Follow-up (mo) | Efficacy | Objective GERD evidence n (%) |
| Onimaru et al[12], Yokohama, Japan | 300 | 45 (3-87) | 6.13/1.33 | 27.3/13.4 | 12 | 98% | 10% |
| Zhou et al[4], Fudan, China | 42 | 44 (10-70) | 2.5 (1-6) | 100% | |||
| Minami et al[32], Nagasaki, Japan | 28 | 52 (19-84) | 6.7/0.7 | 71.2/21 | 16 | 100% | Esophagitis 39.3% |
| Swanström et al[65], Portland, Oregon | 18 | 59 (22-88) | 6/0 | 45/16.8 | 6 | 94% | Esophagitis grade 1 |
| 28% | |||||||
| +pH study | |||||||
| 46% | |||||||
| Costamagna et al[39], Rome, Italy | 11 | 41 (23-68) | 7.1/1.1 | 45.1/16.9 | 3 | 100% | |
| Chiu et al[64], Hong Kong, China | 16 | 47 (22-87) | 5.5/0 | 43.6/29.8 | 3 | 100% | +pH study 3/15 (20%) |
| Hungness et al[53], Chicago, Illinois | 18 | 38 (22-69) | 7/1 | 19/9 | 63 | 89% | Esophagitis LA 33.3% |
| A 13.3% | |||||||
| B 13.3% | |||||||
| C 6.7% | |||||||
| Von Renteln et al[60], European, CT | 70 | 45 | 6.9/1 | 27.6/8.9 | 12 | 82% | Esophagitis 42% |
| LA class | |||||||
| A 29.2% | |||||||
| B 12.3% | |||||||
| Stavropoulos et al[85], Mineola, New York | 100 | 52 | 7.8/0.2 | 44.2/17.6 | 13.3 | 96% | 17/53 (32%) |
| (17-93) | |||||||
| Verlaan et al[37], Amsterdam, The Netherlands | 10 | 43 | 8/1 | 20.5/6.8 | 3 | 100% | 60% |
| LA class | |||||||
| A 30% | |||||||
| B 30% |
There is controversy between studies and within the same study regarding the definition of post-POEM GERD. GERD can be defined on base of symptoms, 24-h pH monitoring and endoscopy data. Familiari et al[48] reported incidence of GERD of 57% based on pH monitoring, 33% based on endoscopic findings and 14% based on symptoms. This discrepancy is found to all studies, however, they all agree that GERD after POEM is not severe and can be successfully treated with proton-pump inhibitors.
In the largest POEM series with longer follow-up, the risk of GERD after POEM varies between 10%-30%, with average 10%, with excellent control under proton pump inhibitors (PPIs)[32]. Although this issue needs further long-term studies, at the present no antireflux procedure is recommended during POEM.
The overall results of POEM worldwide, showed excellent symptom improvement (using Eckardt score pre- and post-POEM) between 82%-100%, (mean 90%)[1,3,4,36-39]. Efficacy of POEM was also studied using manometry and timed barium esophagogram, showing significant improvement in LES pressure and esophageal emptying in 66% and 80% post-POEM, respectively[12,26,37,38,53,58] (Table 5). However, more data on long-term efficacy of POEM is needed, and awaited.
As POEM constitutes a new endoscopic, pure NOTES procedure, which opens the era of submucosal endoscopy, emerged important ethical and training issues. Although theoretically POEM may have dangerous “downside” this has not been yet proved according to successful international experience from more than 4000 POEM cases globally. However, in order to diminish the risk of mishaps an appropriate training program for acquiring adequacy for performing safe and effective POEM is urgently needed.
A simple, cheap and reproducible, non-survival porcine animal model has been established for training in POEM, without the need for concern about complications[67-69]. Pig is the most appropriate animal model for training in POEM, due to its similarities to the human anatomy, while the porcine esophagus has the advantage of easy mobilization due to absence of tight junctions to surrounding organs.
However, there are significant differences between the porcine and human esophagus, particularly in patients with achalasia. Human submucosa is more hard than porcine’s and esophageal circular muscle layer in achalasia is thicker, with multiple high-pressure contractions, while in cadaveric pig model the muscle is thin and without any contraction. Thus, mucosotomy and submucosal tunneling dissection are difficult in porcine due to tissue pliability and poor tissue distention[68].
The low incidence of achalasia (0.3%-1% per 100000 population)[70], in combination with the risk of serious complications, related to the technically demanding POEM procedure, has made training difficult[68,71]. Neither gastroenterologists nor surgeons are absolutely familiar with submucosal endoscopy. While endoscopists are familiar with endoluminal procedures and more experienced in handling endoscope within the natural lumen, surgeons, are familiar with laparoscopic/thoracospocic procedures and can more easily recognize the structures beyond the mucosa[68,71].
POEM however is a procedure that requires both capabilities. Good endoscope manipulation, recognition of luminal structures and surgical knowledge of extraluminal structures especially vessels, nerves and mediastinal anatomy. Moreover, delicate skills are also needed[68,71]. With the worldwide expansion of centers starting performing POEM training program, in POEM procedure is more urgent. Until recently, there are no standard training guidelines for training. The pioneers in POEM proposed a two stage training system for POEM.
First is preclinical training, during which the experienced trainee -which is familiar with handling GI endoscope, has perfect knowledge of esophageal and EGJ anatomy, knowledge of the pathophysiology of achalasia and knowledge of the POEM procedure, including set up of device and patient care during perioperative period- has to follow observation of POEM performed by specialists, and then practice in the animal or cadaveric model, about 46 (range 12-154) hours, according to recent international consensus[26,27,67-69,71]. Some other centers proposed use of clinical proctor system with 2 median number of proctored cases[71].
Second step is the clinical training, with POEM in humans with achalasia, performed under careful guidance and observation by specialists, and finally, performance of POEM in humans, with 20 POEM procedures needed to cover the learning curve[67,68,71]. However, there is still controversy in the literature regarding POEM operator background and training program focusing on “learning curve”, while objective, neutral studies in this issues are difficult[72-74].
The exciting results of POEM[1,3,11,36-39] for esophageal achalasia, has further inspired other endoscopic miniinvasive treatments, such as POET[16,17] for en bloc resection of SMTs using the submucosal tunnel technique, particularly for esophageal, EGJ and gastric cardia tumors originating from the muscularis propria.
Endoscopic resection of SMTs originating from the mucularis mucosa (such as leiomyomas) and possibly the submucosa, has been also reported, with a variety of other techniques[75], from simple snaring to endoscopic submucosal dissection (ESD), because the muscle layer can be preserved[76,77]. Tumors however, originating from the muscularis propria have to be resected by thoracoscopy or laparoscopy[78].
Endoscopic snare full-thickness resection with adequate closure of the perforation with OTSC[19], or clips and an endoloop[18] or endoscopic suturing[20] has been successfully reported for small gastric SMTs (diameter < 2-3 cm)[79]. ESD has been also reported for the removal of EGJ SMTs, with satisfactory results[80]. Endoscopic partial resection using the unroofing technique has been also safely and effectively applied for definite pathological diagnosis of small SMTs[81].
The EGJ, however, is a difficult location for endoscopic resection because it is adjacent to the diaphragm, complicating the endoscopic resection with movement from breathing as well as esophageal peristalsis, in combination with narrow lumen or sharp angle, while SMTs of the EGJ are often irregular, lobulated and may grow annylarly, with potential increased risks of perforation and mediastinal infection, especially for SMTs originating from the muscularis propria. Conventional endoscopic muscularis excavation causes large mucosal defects which are difficult to close and often result in strictures[17].
Submucosal tunnel endoscopy, permitting approach to SMTs through a submucosal tunnel, tumor dissection within the tunnel, “en bloc” removal through a mucosal opening far from the tumor, and finally mucosal closure by clips. Submucosal tunnel endoscopy, permitted a controlled, standardized assess to previously taboo spaces, such as the muscle layer, mediastinum and peritoneum, which has been popularized with POEM[1,3,11,36-39].
Xu et al[17] and Inoue et al[16], based upon the POEM concept for treatment of achalasia, further described the technical principles for POET and performed the first successful POET clinical cases for esophageal, EGJ and gastric cardia SMTs originating from the muscularis propria. Since then POET has been used by other centers[16,17,82,83] as well. However, further international experience is necessary and awaited before the popularization of POET.
The absolute and relative indications and contraindications of POET are described in Table 6. POET for esophageal, EGJ or gastric cardia SMTs, is far less invasive than, the technically demanding and invasive, surgical alternatives, which are either partial proximal gastrectomy for EGJ SMTs and esophagectomy for esophageal SMTs, while for lesions in the middle or distal stomach can be resected easily via laparoscopic approach[16,27] (Table 7). Moreover, surgical resection of cardia SMTs, have high risk of esophageal stricture development.
| Absolute indications |
| Suspected or confirmed GIST of the esophagus and gastric cardia larger than 2-3 cm and lower than 5 cm, and tumor growth on follow-up |
| Suspected or confirmed leiomyoma of the esophagus and gastric cardia larger than > 2-3 cm and < 5 cm |
| Esophageal or gastric cardia SMTs in elderly with comorbidities and non-surgical candidates completed the above criteria (only in experienced hands and specialized centers) |
| POET does not exclude surgery. Complete histological diagnosis possible with POET |
| Relative indications |
| Esophageal and gastric SMT more than 5 cm (full-thickness resection using submucosal tunnel technique possible) (in experienced hands and specialized centers only and within studies) |
| Contraindication |
| Suspected or proved malignancy of SMTs |
| Advantages of POET | ||
| POET | Surgical myotomy | |
| Minimally invasive method | Invasive (major surgery) | |
| Hospitalization | Less hospitalization (1-5 d) | Longer hospitalization > 5 d |
| Specimen for complete histology possible | ||
| Does not preclude surgery | ||
| Elderly patients | Effective in elderly with comorbidities and contraindications (only specialized centers) | Contra indication for surgery |
| Cost | Lower hospitalization and lower cost | Higher cost in combination to surgical procedure |
| Disadvantages of POET | ||
| POET | Surgery | |
| Follow-up | Short follow-up (novel technique) | Longer follow-up |
| POEM | POET restricted to specialized centers | Common surgical or laparoscopic procedure overall available |
| Training | Difficult (only few centers worldwide) | Overall available |
| Outcome | Complete curable resection may be not possible in malignant GIST cases | Complete resection possible |
Based on the experience from specialized centers[16,27,80,82], absolute indication for POET includes suspected or confirmed gastrointestinal stromal tumor (GIST) and leiomyoma of the esophagus, gastric cardia and EGJ larger than 2-3 cm, if they are causing symptoms, increasing in size on follow-up or have high risk features on biopsy, endoscopic ultrasound (EUS) or computed tomography[16,27]. SMTs lower than 2 cm are low risk lesions and life-long surveillance by endoscopy/EUS is indicated. Some authors stated that in these small size (< 2 cm) SMTs, POET may offer definitive histologic diagnosis by achieving en bloc resection and may eliminate the need for life-long surveillance[40], however the current surveillance practice has not yet changed. Contraindication for POET is suspected or confirmed malignancy. In suspected malignant cases, EUS puncture is indicated for tissue diagnosis and if malignant, the patients were primarily referred for surgical resection.
POET is also advantageous because it could be also applied in case of contraindications for the above-mentioned major operations, particularly in patients with serious comorbidities[16]. Although, initial experience of POET in a small series of patients and from specialized centers, was exciting in terms of safety and efficacy, further international experience with greater number of patients and longer follow-up is necessary and awaited.
The general set up of POET is the same as during POEM procedure[1], including longitudinal mucosal incision, entrance to the submucosal space, creation of the submucosal tunnel, and approaching the SMTs. Only the final step is different and individualized based on the specifics of each case (Figure 3).
In POET the initial 2-cm longitudinal mucosal incision, is made at approximately 5 cm orally to the proximal margin of the SMT. The submucosal tunnel is created in the same way as Inoue et al[1] first described for POEM. The submucosal tunnel advanced towards the SMT and then extended beyond the tumor to prepare enough space to finally resect the tumor under direct vision.
In the final stage of POET the SMT is enucleated using combination of electrocautery knives [TT-knife and insulated tip (IT) knife] after dissection of muscle fibers connected to the SMT. The IT-knife is useful to dissect from the distal to proximal direction, and to mobilize the SMT. Then, extraction of the mobilized SMT is followed by suctioning the tumor into the cap device and removes it through the mucosal entry. Finally, the mucosal entry was closed tightly in similar manner as in POEM[1], mainly with endoscopic clips. Endoscopic suturing is alternatively used in difficult cases, by other groups[40].
The follow-up includes gastroscopy the following day to evaluate the mucosal integrity and contrast media swallow to check for leakage, and if normal started clear liquid diet and gradually regular diet the next days. Annual endoscopic follow-up was then recommended.
Inoue et al[16] described successful complete POET in seven patients, four cardia and three esophageal SMTs, without complications. Histologically, one GIST, five leiomyomas and one aberrant pancreas were found. Only in the rare case of aberrant pancreas, additional mucosal resection was required, while in the other six tumors, resection margins were clear. No short-term complications reported[16].
POET also showed excellent results in long-term, according to a recent report from a pioneering center with large number of patients (290 patients with 4 years follow-up), showing no residual tumor, local tumor recurrence or distant metastasis[82]. According to literature available to us, no POET-related deaths were currently reported.
However, taking into account that POET is a relatively new technique with potential dangerous “downside”, future international, prospective, multicenter studies, focusing also on complications (procedure and not procedure related), are necessary and awaited. At the moment POET is restricted only to pioneering centers and within protocols. On the other hand, POET should be also considered as endoscopic surgical procedure and should be compared to surgical equivalents, which are for esophageal and EGJ lesions the esophagectomy and esophagogastrectomy, respectively.
Submucosal tunnel endoscopy opened other possibilities as well, such as exploration of peritoneal and thoracic cavities through transgastric peritoneoscopy[84] (Table 8). Lastly, another application of submucosal tunnel endoscopy, is the peroral pyloromyotomy as a potential treatment of gastroparesis using endoscopic submucosal tunneling similar to the concept of POEM[21].
| Endoscopic vagotomy? |
| Endoscopic thoracoscopy? |
| Endoscopic retroperitoneoscopy? |
| Endoscopic peritoneoscopy? |
| Endoscopic sympathectomy |
Submucosal tunnel endoscopy, including POEM and POET, constitutes a novel terrain for minimal invasive endoscopic treatment of various diseases, such as achalasia and other esophageal motility disorders and esophageal, EGJ and gastric cardia SMTs, which showed exciting results in international level, and superior characteristics than the standard 100-year-old surgical alternatives.
Technological advancements in the era of NOTES, such as endoscopic suturing techniques, permitted endoscopists to become more aggressive, with submucosal tunnel endoscopy including endoscopic full-thickness resections, to be performed safely and successfully. Submucosal tunnel endoscopy opened many possibilities for miniinvasive endoscopic treatment in diseases where the surgical equivalents in terms of aggressiveness are totally incomparable, particularly in elderly patients with co-morbidities.
POEM has been globally popularized, with excellent results even from small centers, while it has been extended further to become the treatment of choice not only for all types of achalasia [classical (I), vigorous (II), spastic (III)], including advanced sigmoid (S1 and S2) type, but also for failed surgical or LHM cases, and other esophageal motility disorders (diffuse esophageal spasm, nutcracker and jackhammer esophagus).
POET was spawned from the success of POEM, and slowly expanded worldwide to safely and successfully treat muscularis propria based SMTs in challenging locations in esophagus, EGJ and gastric cardia, with minimally invasive endoscopic procedure.
However, larger number of patients and long-term outcome of POEM and more experience of POET is necessary and is awaited. POEM and POET inspire many other NOTES interventions utilizing the submucosal tunnel approach.
P- Reviewer: Buanes TA, Kopacova M, Negreanu L S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1168] [Cited by in RCA: 1234] [Article Influence: 82.3] [Reference Citation Analysis (1)] |
| 2. | Kalloo AN, Singh VK, Jagannath SB, Niiyama H, Hill SL, Vaughn CA, Magee CA, Kantsevoy SV. Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc. 2004;60:114-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1037] [Cited by in RCA: 903] [Article Influence: 43.0] [Reference Citation Analysis (0)] |
| 3. | Stavropoulos SN, Modayil RJ, Friedel D, Savides T. The International Per Oral Endoscopic Myotomy Survey (IPOEMS): a snapshot of the global POEM experience. Surg Endosc. 2013;27:3322-3338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 203] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 4. | Zhou PH, Cai MY, Yao LQ, Zhong YS, Ren Z, Xu MD, Chen WF, Qin XY. [Peroral endoscopic myotomy for esophageal achalasia: report of 42 cases]. Zhonghua Weichang Waike Zazhi. 2011;14:705-708. [PubMed] |
| 5. | Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology. 2008;135:1526-1533. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 661] [Cited by in RCA: 553] [Article Influence: 32.5] [Reference Citation Analysis (0)] |
| 6. | Kandulski A, Fuchs KH, Malfertheiner P. Jackhammer esophagus: high-resolution manometry and therapeutic approach using peroral endoscopic myotomy (POEM). Dis Esophagus. 2014;Jan 27; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 7. | Minami H, Isomoto H, Yamaguchi N, Ohnita K, Takeshima F, Inoue H, Nakao K. Peroral endoscopic myotomy (POEM) for diffuse esophageal spasm. Endoscopy. 2014;46 Suppl 1 UCTN:E79-E81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 8. | Shiwaku H, Inoue H, Beppu R, Nakashima R, Minami H, Shiroshita T, Yamauchi Y, Hoshino S, Yamashita Y. Successful treatment of diffuse esophageal spasm by peroral endoscopic myotomy. Gastrointest Endosc. 2013;77:149-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 85] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 9. | Khashab MA, Messallam AA, Onimaru M, Teitelbaum EN, Ujiki MB, Gitelis ME, Modayil RJ, Hungness ES, Stavropoulos SN, El Zein MH. International multicenter experience with peroral endoscopic myotomy for the treatment of spastic esophageal disorders refractory to medical therapy (with video). Gastrointest Endosc. 2015;81:1170-1177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 138] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 10. | Sharata A, Kurian AA, Dunst CM, Bhayani NH, Reavis KM, Swanström LL. Peroral endoscopic myotomy (POEM) is safe and effective in the setting of prior endoscopic intervention. J Gastrointest Surg. 2013;17:1188-1192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 102] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 11. | Zhou PH, Li QL, Yao LQ, Xu MD, Chen WF, Cai MY, Hu JW, Li L, Zhang YQ, Zhong YS. Peroral endoscopic remyotomy for failed Heller myotomy: a prospective single-center study. Endoscopy. 2013;45:161-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 137] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 12. | Onimaru M, Inoue H, Ikeda H, Yoshida A, Santi EG, Sato H, Ito H, Maselli R, Kudo SE. Peroral endoscopic myotomy is a viable option for failed surgical esophagocardiomyotomy instead of redo surgical Heller myotomy: a single center prospective study. J Am Coll Surg. 2013;217:598-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 124] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 13. | Onimaru M, Inoue H, Ikeda H, Sato C, Sato H, Phalanusitthepha C, Santi EG, Grimes KL, Ito H, Kudo SE. Greater curvature myotomy is a safe and effective modified technique in per-oral endoscopic myotomy (with videos). Gastrointest Endosc. 2015;81:1370-1377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Hu JW, Li QL, Zhou PH, Yao LQ, Xu MD, Zhang YQ, Zhong YS, Chen WF, Ma LL, Qin WZ. Peroral endoscopic myotomy for advanced achalasia with sigmoid-shaped esophagus: long-term outcomes from a prospective, single-center study. Surg Endosc. 2015;29:2841-2850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 15. | Eleftheriadis N, Protopapas A, Katsogridakis J, Hatzitolios AI. Successful peroral endoscopic myotomy for radical treatment of sigmoid-type esophageal achalasia by Greek gastroenterologists. Ann Gastroenterol. 2014;27:430-431. [PubMed] |
| 16. | Inoue H, Ikeda H, Hosoya T, Onimaru M, Yoshida A, Eleftheriadis N, Maselli R, Kudo S. Submucosal endoscopic tumor resection for subepithelial tumors in the esophagus and cardia. Endoscopy. 2012;44:225-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 209] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 17. | Xu MD, Cai MY, Zhou PH, Qin XY, Zhong YS, Chen WF, Hu JW, Zhang YQ, Ma LL, Qin WZ. Submucosal tunneling endoscopic resection: a new technique for treating upper GI submucosal tumors originating from the muscularis propria layer (with videos). Gastrointest Endosc. 2012;75:195-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 236] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 18. | Ye LP, Yu Z, Mao XL, Zhu LH, Zhou XB. Endoscopic full-thickness resection with defect closure using clips and an endoloop for gastric subepithelial tumors arising from the muscularis propria. Surg Endosc. 2014;28:1978-1983. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 71] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 19. | Saxena P, Chavez YH, Kord Valeshabad A, Kalloo AN, Khashab MA. An alternative method for mucosal flap closure during peroral endoscopic myotomy using an over-the-scope clipping device. Endoscopy. 2013;45:579-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 20. | Modayil R, Friedel D, Stavropoulos SN. Endoscopic suture repair of a large mucosal perforation during peroral endoscopic myotomy for treatment of achalasia. Gastrointest Endosc. 2014;80:1169-1170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Khashab MA, Stein E, Clarke JO, Saxena P, Kumbhari V, Chander Roland B, Kalloo AN, Stavropoulos S, Pasricha P, Inoue H. Gastric peroral endoscopic myotomy for refractory gastroparesis: first human endoscopic pyloromyotomy (with video). Gastrointest Endosc. 2013;78:764-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 209] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 22. | Ortega JA, Madureri V, Perez L. Endoscopic myotomy in the treatment of achalasia. Gastrointest Endosc. 1980;26:8-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 101] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 23. | Pasricha PJ, Hawari R, Ahmed I, Chen J, Cotton PB, Hawes RH, Kalloo AN, Kantsevoy SV, Gostout CJ. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy. 2007;39:761-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 360] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 24. | Sumiyama K, Gostout CJ, Rajan E, Bakken TA, Knipschield MA, Marler RJ. Submucosal endoscopy with mucosal flap safety valve. Gastrointest Endosc. 2007;65:688-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 172] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 25. | Perretta S, Dallemagne B, Donatelli G, Diemunsch P, Marescaux J. Transoral endoscopic esophageal myotomy based on esophageal function testing in a survival porcine model. Gastrointest Endosc. 2011;73:111-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 26. | Inoue H, Tianle KM, Ikeda H, Hosoya T, Onimaru M, Yoshida A, Minami H, Kudo SE. Peroral endoscopic myotomy for esophageal achalasia: technique, indication, and outcomes. Thorac Surg Clin. 2011;21:519-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 130] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 27. | Inoue H, Santi EG, Onimaru M, Kudo SE. Submucosal endoscopy: from ESD to POEM and beyond. Gastrointest Endosc Clin N Am. 2014;24:257-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 28. | Yang D, Draganov PV. Peroral endoscopic myotomy (POEM) for achalasia after Roux-en-Y gastric bypass. Endoscopy. 2014;46 Suppl 1 UCTN:E11-E12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 29. | Maselli R, Inoue H, Misawa M, Ikeda H, Hosoya T, Onimaru M, Yoshida A, Eleftheriadis N, Suzuki K, Kudo S. Peroral endoscopic myotomy (POEM) in a 3-year-old girl with severe growth retardation, achalasia, and Down syndrome. Endoscopy. 2012;44 Suppl 2 UCTN:E285-E287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 30. | Familiari P, Marchese M, Gigante G, Boskoski I, Tringali A, Perri V, Costamagna G. Peroral endoscopic myotomy for the treatment of achalasia in children. J Pediatr Gastroenterol Nutr. 2013;57:794-797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 31. | Chen WF, Li QL, Zhou PH, Yao LQ, Xu MD, Zhang YQ, Zhong YS, Ma LL, Qin WZ, Hu JW. Long-term outcomes of peroral endoscopic myotomy for achalasia in pediatric patients: a prospective, single-center study. Gastrointest Endosc. 2015;81:91-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 77] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 32. | Minami H, Inoue H, Haji A, Isomoto H, Urabe S, Hashiguchi K, Matsushima K, Akazawa Y, Yamaguchi N, Ohnita K. Per-oral endoscopic myotomy: emerging indications and evolving techniques. Dig Endosc. 2015;27:175-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 33. | Cai MY, Zhou PH, Yao LQ, Xu MD, Zhong YS, Li QL, Chen WF, Hu JW, Cui Z, Zhu BQ. Peroral endoscopic myotomy for idiopathic achalasia: randomized comparison of water-jet assisted versus conventional dissection technique. Surg Endosc. 2014;28:1158-1165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 60] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 34. | Friedel D, Modayil R, Iqbal S, Grendell JH, Stavropoulos SN. Per-oral endoscopic myotomy for achalasia: An American perspective. World J Gastrointest Endosc. 2013;5:420-427. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 35] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 35. | Khashab MA, Messallam AA, Saxena P, Kumbhari V, Ricourt E, Aguila G, Roland BC, Stein E, Nandwani M, Inoue H. Jet injection of dyed saline facilitates efficient peroral endoscopic myotomy. Endoscopy. 2014;46:298-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 36. | von Renteln D, Inoue H, Minami H, Werner YB, Pace A, Kersten JF, Much CC, Schachschal G, Mann O, Keller J. Peroral endoscopic myotomy for the treatment of achalasia: a prospective single center study. Am J Gastroenterol. 2012;107:411-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 273] [Cited by in RCA: 251] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 37. | Verlaan T, Rohof WO, Bredenoord AJ, Eberl S, Rösch T, Fockens P. Effect of peroral endoscopic myotomy on esophagogastric junction physiology in patients with achalasia. Gastrointest Endosc. 2013;78:39-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 83] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 38. | Swanstrom LL, Kurian A, Dunst CM, Sharata A, Bhayani N, Rieder E. Long-term outcomes of an endoscopic myotomy for achalasia: the POEM procedure. Ann Surg. 2012;256:659-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 214] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 39. | Costamagna G, Marchese M, Familiari P, Tringali A, Inoue H, Perri V. Peroral endoscopic myotomy (POEM) for oesophageal achalasia: preliminary results in humans. Dig Liver Dis. 2012;44:827-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 122] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 40. | Friedel D, Modayil R, Stavropoulos SN. Per-oral endoscopic myotomy: major advance in achalasia treatment and in endoscopic surgery. World J Gastroenterol. 2014;20:17746-17755. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (1)] |
| 41. | Li QL, Chen WF, Zhou PH, Yao LQ, Xu MD, Hu JW, Cai MY, Zhang YQ, Qin WZ, Ren Z. Peroral endoscopic myotomy for the treatment of achalasia: a clinical comparative study of endoscopic full-thickness and circular muscle myotomy. J Am Coll Surg. 2013;217:442-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 126] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 42. | Phalanusitthepha C, Inoue H, Ikeda H, Sato H, Sato C, Hokierti C. Peroral endoscopic myotomy for esophageal achalasia. Ann Transl Med. 2014;2:31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 43. | Pandolfino JE, Roman S. High-resolution manometry: an atlas of esophageal motility disorders and findings of GERD using esophageal pressure topography. Thorac Surg Clin. 2011;21:465-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 44. | Eleftheriadis N, Inoue H, Ikeda H, Onimaru M, Yoshida A, Maselli R, Santi G, Kudo SE. In vivo observation of aberrant innermost longitudinal muscle bundles in front of the circular muscle layer at the level of the esophagogastric junction during peroral endoscopic myotomy. Gastrointest Endosc. 2013;78:676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 45. | Ren Z, Zhong Y, Zhou P, Xu M, Cai M, Li L, Shi Q, Yao L. Perioperative management and treatment for complications during and after peroral endoscopic myotomy (POEM) for esophageal achalasia (EA) (data from 119 cases). Surg Endosc. 2012;26:3267-3272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 165] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 46. | Li H, Linghu E, Wang X. Fibrin sealant for closure of mucosal penetration at the cardia during peroral endoscopic myotomy (POEM). Endoscopy. 2012;44 Suppl 2 UCTN:E215-E216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 47. | Rieder E, Swanström LL, Perretta S, Lenglinger J, Riegler M, Dunst CM. Intraoperative assessment of esophagogastric junction distensibility during per oral endoscopic myotomy (POEM) for esophageal motility disorders. Surg Endosc. 2013;27:400-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 79] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 48. | Familiari P, Gigante G, Marchese M, Boskoski I, Bove V, Tringali A, Perri V, Onder G, Costamagna G. EndoFLIP system for the intraoperative evaluation of peroral endoscopic myotomy. United European Gastroenterol J. 2014;2:77-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 61] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 49. | Teitelbaum EN, Soper NJ, Pandolfino JE, Kahrilas PJ, Hirano I, Boris L, Nicodème F, Lin Z, Hungness ES. Esophagogastric junction distensibility measurements during Heller myotomy and POEM for achalasia predict postoperative symptomatic outcomes. Surg Endosc. 2015;29:522-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 127] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 50. | Li QL, Zhou PH. Perspective on peroral endoscopic myotomy for achalasia: Zhongshan experience. Gut Liver. 2015;9:152-158. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 51. | Gockel I, Timm S, Sgourakis GG, Musholt TJ, Rink AD, Lang H. Achalasia--if surgical treatment fails: analysis of remedial surgery. J Gastrointest Surg. 2010;14 Suppl 1:S46-S57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 52. | Wang L, Li YM. Recurrent achalasia treated with Heller myotomy: a review of the literature. World J Gastroenterol. 2008;14:7122-7126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 38] [Cited by in RCA: 40] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 53. | Hungness ES, Teitelbaum EN, Santos BF, Arafat FO, Pandolfino JE, Kahrilas PJ, Soper NJ. Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy. J Gastrointest Surg. 2013;17:228-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 192] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 54. | Wei M, Yang T, Yang X, Wang Z, Zhou Z. Peroral esophageal myotomy versus laparoscopic Heller’s myotomy for achalasia: a meta-analysis. J Laparoendosc Adv Surg Tech A. 2015;25:123-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 55. | Ujiki MB, Yetasook AK, Zapf M, Linn JG, Carbray JM, Denham W. Peroral endoscopic myotomy: A short-term comparison with the standard laparoscopic approach. Surgery. 2013;154:893-897; discussion 897-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 125] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 56. | Teitelbaum EN, Rajeswaran S, Zhang R, Sieberg RT, Miller FH, Soper NJ, Hungness ES. Peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy produce a similar short-term anatomic and functional effect. Surgery. 2013;154:885-891; discussion 891-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 62] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 57. | Kumagai K, Tsai JA, Thorell A, Lundell L, Håkanson B. Per-oral endoscopic myotomy for achalasia. Are results comparable to laparoscopic Heller myotomy? Scand J Gastroenterol. 2015;50:505-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 58. | Patel K, Abbassi-Ghadi N, Markar S, Kumar S, Jethwa P, Zaninotto G. Peroral endoscopic myotomy for the treatment of esophageal achalasia: systematic review and pooled analysis. Dis Esophagus. 2015;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 91] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 59. | Wang X, Tan Y, Zhang J, Liu D. Risk factors for gas-related complications of peroral endoscopic myotomy in achalasia. Neth J Med. 2015;73:76-81. [PubMed] |
| 60. | Von Renteln D, Fuchs KH, Fockens P, Bauerfeind P, Vassiliou MC, Werner YB, Fried G, Breithaupt W, Heinrich H, Bredenoord AJ. Peroral endoscopic myotomy for the treatment of achalasia: an international prospective multicenter study. Gastroenterology. 2013;145:309-11.e1-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 265] [Cited by in RCA: 249] [Article Influence: 20.8] [Reference Citation Analysis (1)] |
| 61. | Minami H, Isomoto H, Yamaguchi N, Matsushima K, Akazawa Y, Ohnita K, Takeshima F, Inoue H, Nakao K. Peroral endoscopic myotomy for esophageal achalasia: clinical impact of 28 cases. Dig Endosc. 2014;26:43-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 80] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 62. | Tamiya Y, Nakahara K, Kominato K, Serikawa O, Watanabe Y, Tateishi H, Takedatsu H, Toyonaga A, Sata M. Pneumomediastinum is a frequent but minor complication during esophageal endoscopic submucosal dissection. Endoscopy. 2010;42:8-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 63. | Ross SW, Oommen B, Wormer BA, Walters AL, Matthews BD, Heniford BT, Augenstein VA. National outcomes of laparoscopic Heller myotomy: operative complications and risk factors for adverse events. Surg Endosc. 2015;29:3097-3105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 64. | Chiu PW, Wu JC, Teoh AY, Chan Y, Wong SK, Liu SY, Yung MY, Lam CC, Sung JJ, Chan FK. Peroral endoscopic myotomy for treatment of achalasia: from bench to bedside (with video). Gastrointest Endosc. 2013;77:29-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 88] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 65. | Swanström LL, Rieder E, Dunst CM. A stepwise approach and early clinical experience in peroral endoscopic myotomy for the treatment of achalasia and esophageal motility disorders. J Am Coll Surg. 2011;213:751-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 111] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 66. | Inoue H, Ikeda H, Hosoya T, Yoshida A, Onimaru M, Minami H, Kudo SE. [Per-oral endoscopic myotomy (POEM) for esophageal achalasia]. Nihon Shokakibyo Gakkai Zasshi. 2012;109:728-731. [PubMed] |
| 67. | Ren Y, Tang X, Zhi F, Liu S, Wu J, Peng Y, Jiang B, Gong W. A stepwise approach for peroral endoscopic myotomy for treating achalasia: from animal models to patients. Scand J Gastroenterol. 2015;50:952-958. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 68. | Eleftheriadis N, Inoue H, Ikeda H, Onimaru M, Yoshida A, Hosoya T, Maselli R, Kudo SE. Training in peroral endoscopic myotomy (POEM) for esophageal achalasia. Ther Clin Risk Manag. 2012;8:329-342. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 79] [Cited by in RCA: 81] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 69. | Perretta S, Dallemagne B, Marescaux J. STEPS to POEM: introduction of a new technique at the IRCAD. Surg Innov. 2012;19:216-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 70. | Mikaeli J, Islami F, Malekzadeh R. Achalasia: a review of Western and Iranian experiences. World J Gastroenterol. 2009;15:5000-5009. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 71. | Stavropoulos SN, Desilets DJ, Fuchs KH, Gostout CJ, Haber G, Inoue H, Kochman ML, Modayil R, Savides T, Scott DJ. Per-oral endoscopic myotomy white paper summary. Gastrointest Endosc. 2014;80:1-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 121] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 72. | Teitelbaum EN, Soper NJ, Arafat FO, Santos BF, Kahrilas PJ, Pandolfino JE, Hungness ES. Analysis of a learning curve and predictors of intraoperative difficulty for peroral esophageal myotomy (POEM). J Gastrointest Surg. 2014;18:92-98; discussion 98-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 88] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 73. | Kumta NA, Mehta S, Kedia P, Weaver K, Sharaiha RZ, Fukami N, Minami H, Casas F, Gaidhane M, Lambroza A. Peroral endoscopic myotomy: establishing a new program. Clin Endosc. 2014;47:389-397. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 74. | Kurian AA, Dunst CM, Sharata A, Bhayani NH, Reavis KM, Swanström LL. Peroral endoscopic esophageal myotomy: defining the learning curve. Gastrointest Endosc. 2013;77:719-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 147] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 75. | Schmidt A, Bauder M, Riecken B, Caca K. Endoscopic resection of subepithelial tumors. World J Gastrointest Endosc. 2014;6:592-599. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 76. | Schlag C, Wilhelm D, von Delius S, Feussner H, Meining A. EndoResect study: endoscopic full-thickness resection of gastric subepithelial tumors. Endoscopy. 2013;45:4-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 77. | Wang L, Fan CQ, Ren W, Zhang X, Li YH, Zhao XY. Endoscopic dissection of large endogenous myogenic tumors in the esophagus and stomach is safe and feasible: a report of 42 cases. Scand J Gastroenterol. 2011;46:627-633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 78. | Kent M, d’Amato T, Nordman C, Schuchert M, Landreneau R, Alvelo-Rivera M, Luketich J. Minimally invasive resection of benign esophageal tumors. J Thorac Cardiovasc Surg. 2007;134:176-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 84] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 79. | Kim GH. Endoscopic resection of subepithelial tumors. Clin Endosc. 2012;45:240-244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 80. | Li QL, Yao LQ, Zhou PH, Xu MD, Chen SY, Zhong YS, Zhang YQ, Chen WF, Ma LL, Qin WZ. Submucosal tumors of the esophagogastric junction originating from the muscularis propria layer: a large study of endoscopic submucosal dissection (with video). Gastrointest Endosc. 2012;75:1153-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 94] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 81. | Lee CK, Chung IK, Lee SH, Lee SH, Lee TH, Park SH, Kim HS, Kim SJ, Cho HD. Endoscopic partial resection with the unroofing technique for reliable tissue diagnosis of upper GI subepithelial tumors originating from the muscularis propria on EUS (with video). Gastrointest Endosc. 2010;71:188-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 71] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 82. | Wang XY, Xu MD, Yao LQ, Zhou PH, Pleskow D, Li QL, Zhang YQ, Chen WF, Zhong YS. Submucosal tunneling endoscopic resection for submucosal tumors of the esophagogastric junction originating from the muscularis propria layer: a feasibility study (with videos). Surg Endosc. 2014;28:1971-1977. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 83. | Ye LP, Zhang Y, Mao XL, Zhu LH, Zhou X, Chen JY. Submucosal tunneling endoscopic resection for small upper gastrointestinal subepithelial tumors originating from the muscularis propria layer. Surg Endosc. 2014;28:524-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 110] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 84. | Lee SH, Kim SJ, Lee TH, Chung IK, Park SH, Kim EO, Lee HJ, Cho HD. Human applications of submucosal endoscopy under conscious sedation for pure natural orifice transluminal endoscopic surgery. Surg Endosc. 2013;27:3016-3020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 85. | Stavropoulos SN, Harris MD, Hida S, Brathwaite C, Demetriou C, Grendell J. Endoscopic submucosal myotomy for the treatment of achalasia (with video). Gastrointest Endosc. 2010;72:1309-1311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |