Published online Sep 16, 2013. doi: 10.4253/wjge.v5.i9.461
Revised: July 22, 2013
Accepted: August 12, 2013
Published online: September 16, 2013
Processing time: 128 Days and 17.2 Hours
Pseudocysts of the pancreas are not rare, but spontaneous perforation and/or fistulization occurs in fewer than 3% of these pseudocysts. Perforation into the free peritoneal cavity, stomach, duodenum, colon, portal vein, pleural cavity and through the abdominal wall has been reported. Spontaneous rupture of the pancreatic pseudocyst into the surrounding hollow viscera is rare and, may be associated with life-threatening bleeding. Such cases require emergency surgical intervention. Uncomplicated rupture of pseudocyst is an even rarer occurrence. We present a case of spontaneous resolution of a pancreatic pseudocyst with gastric connection without bleeding. A 67-year-old women with a large pancreatic pseudocyst resulting from a complication of chronic pancreatitis was referred to our institution. During hospital stay, there was sudden decrease in the size of epigastric lump. Repeat computed tomography (CT) revealed that the size of the pseudocyst had decreased significantly; however, gas was observed in stomach and pseudocyst along with rent between lesser curvature of stomach and pseudocyst suggestive of spontaneous cystogastric fistula.The fistula tract occluded spontaneously and the patient recovered without any complication or need for surgical treatment. After 5 wk, follow up CT revealed complete resolution of pseudocyst. Esophagogastroduodenoscopy revealed that the orifice was completely occluded with ulcer at the site of previous fistulous opening.
Core tip: Spontaneous rupture of the pancreatic pseudocyst into the surrounding hollow viscera is rare and, may be associated with life-threatening bleeding. Such cases require emergency surgical intervention. Uncomplicated rupture of pseudocyst is an even rarer occurrence. We present a case of spontaneous resolution of a pancreatic pseudocyst with gastric connection without bleeding. Only few cases had been reported in literature till date. We managed the case conservatively without surgical intervention.
- Citation: Somani PO, Jain SS, Shah DK, Khot AA, Rathi PM. Uncomplicated spontaneous rupture of pancreatic pseudocyst into stomach: A case report. World J Gastrointest Endosc 2013; 5(9): 461-464
- URL: https://www.wjgnet.com/1948-5190/full/v5/i9/461.htm
- DOI: https://dx.doi.org/10.4253/wjge.v5.i9.461
Pseudocysts of the pancreas are not rare, but spontaneous perforation and/or fistulization occurs in fewer than 3% of these pseudocysts[1]. Spontaneous rupture of the pancreatic pseudocysts is known to occur into the stomach, duodenum, biliary tract, renal collecting system, colon and bronchial tree[2]. However, most of these spontaneous ruptures are associated with bleeding complications needing emergency surgical intervention[3]. Spontaneous rupture of the pancreatic pseudocyst into the surrounding hollow viscera is rare and, whenever it occurs, is associated with life-threatening bleeding. Uncomplicated rupture of pseudocyst is an even rarer occurrence[4]. We present a case of spontaneous resolution of a pancreatic pseudocyst with gastric connection.
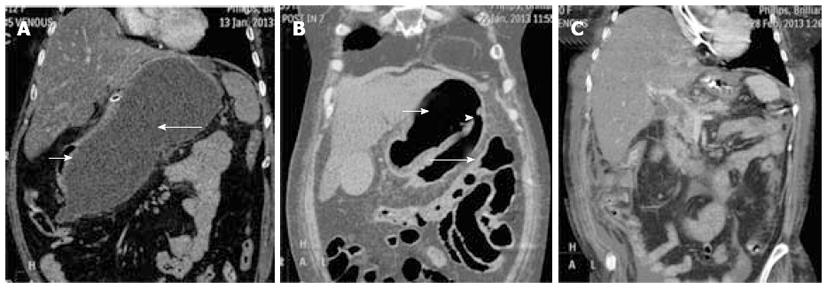
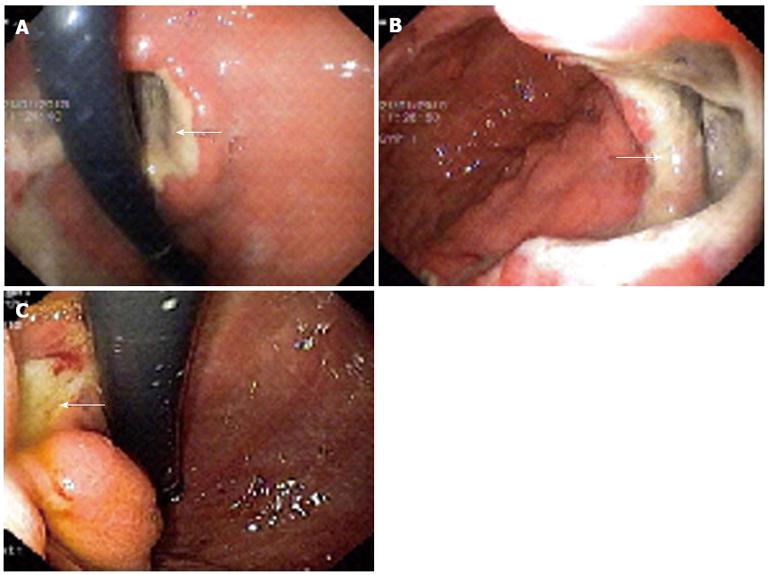
A 67-year-old female was admitted to hospital with one month history of abdominal pain and recurrent vomiting. She had history of recurrent episodes of similar abdominal pain in past. She also noticed fullness in upper abdomen. On admission, vitals were stable. On examination there was cystic lump in epigastrium around 8 cm × 6 cm with mild tenderness. Rest of the Physical examination was unremarkable. Haemoglobin was 12.7 g/dL (normal range, 12-16 g/dL), serum amylase level was 180 U/L (normal range, 28-160 U/L); lipase, 94 U/L (normal range, 0-60 U/L) and other laboratory parameters were within normal limits. On admission, computed tomography (CT) of abdomen (Figure 1A) revealed a pseudocyst measuring 20 cm × 12 cm arising from body and tail compressing the stomach along with atrophic pancreas suggestive of chronic pancreatitis. Patient was managed conservatively. After ten days we noticed sudden decrease in the size of epigastric lump. Repeat CT revealed that the size of the pseudocyst had decreased significantly; however, gas was observed in stomach and pseudocyst along with rent between lesser curvature of stomach and pseudocyst suggestive of spontaneous cystogastric fistula (Figure 1B). Esophagogastroduodenoscopy (EGD) showed a 2.5-cm orifice of the fistula along the lesser curvature of stomach (Figure 2A and B). Patient was hemodynamically stable and without any complications, so was managed conservatively. After 5 wk, follow up CT revealed complete resolution of pseudocyst (Figure 1C). EGD revealed that the orifice was completely occluded with ulcer at the site of previous fistulous opening (Figure 2C).
Pseudocysts occur in about 25% of patients with chronic pancreatitis and are most common in alcoholic chronic pancreatitis. The natural history of pseudocysts in chronic pancreatitis is not fully defined. Overall, complications of pseudocysts occur in 20% to 40% of cases. Complications include compression of large peripancreatic vessels, stomach or duodenum; infection; hemorrhage; and development of a fistula. Treatment is not necessary in all patients. Patients who have mature pseudocysts smaller than 6 cm, minimal or no symptoms, no complications, and are reliable may be managed conservatively. Even larger pseudocysts that remain asymptomatic can be managed expectantly. Very large pseudocysts, an enlarging pseudocyst and symptomatic or complicated pseudocysts require therapy. Therapy for pseudocysts can be surgical, percutaneous or endoscopic. Surgical therapy has been used most extensively and usually involves cyst decompression into a loop of small bowel or stomach, often coupled with a pancreatic ductal drainage procedure. Surgical therapy has a long-term success rate of 90% and an operative mortality of less than 3%[5].
There are many mechanisms that lead to resolution of a pseudocyst. At times, it regresses after the inflammatory reaction resolves or it can resolve spontaneously with natural drainage to the duodenum through the pancreatic duct. When erosion of a pseudocyst occurs near the gastrointestinal tract and a fistula is formed, the fistula can lead to resolution of the pseudocyst. In some cases, the pseudocyst can resolve as it leaks or ruptures into the abdominal cavity[6]. It is expected that temporary or permanent resolution of the pseudocyst will occur with drainage through a fistula between the pseudocyst and the gastrointestinal tract[7]. As high-density protein from the pseudocyst moves to the gastrointestinal tract through a fistula, patients manifest sudden clinical improvement with resolution of the pseudocyst after temporary symptoms of diarrhoea, vomiting abscess and blood or hematochezia. When the pseudocyst resolves as a result of fistula formation, the patient does not require surgery. When a patient develops hematochezia, this may imply that the fistula exists near the large intestine, whereas hematemesis may imply that it exists near the stomach or duodenal wall. The locations in the gastrointestinal tract most vulnerable to fistula formation, in patients with pancreatitis, are the transverse colon and splenic flexure, followed by the duodenum; however, the small intestine, stomach and esophagus are uncommon locations[8].
The rupture of pancreatic pseudocysts into surrounding viscera is a well-known phenomenon. Usually, spontaneous drainage and amelioration of symptoms result when the pseudocyst ruptures into the hollow gastrointestinal tract. Three pathogenetic mechanisms of bleeding and rupture of pancreatic pseudocysts have been suggested. First, uncontrolled severe inflammation and activated lytic enzymes, such as elastase and trypsin, might cause progressive digestion of the elastic component of the vessel wall, with consequent erosion and disruption. Second, pseudocysts might produce erosion of vessels as a consequence of persistent compression, ischemia and the elastolytic action of enzymatic contact. Third, the inflammatory process and the pseudocyst might cause compression or thrombosis in the portal or splenic vein, leading to localized portal hypertension[3].
The patient presented here had epigastric mass on admission and was found to have pseudocyst on CT abdomen. After ten days patient had sudden decrease in the size of epigastric lump for which she underwent CT abdomen which showed gas in stomach and pseudocyst along with rent between lesser curvature of stomach and pseudocyst suggestive of spontaneous cystogastric fistula. Patient was hemodynamically stable and without any complications like gastrointestinal bleeding or anemia. After 5 wk repeat CT abdomen showed resolution of pseudocyst and fistula.
Unlike the formation of a fistula between the large intestine and the pseudocyst, a fistula between the stomach and the pseudocyst does not require urgent surgery, unless it is accompanied by abscess formation or bleeding[8].
Severe acute pancreatitis (SAP) is known to be complicated by fistulization into the neighboring organs. Pancreatocolonic fistulas are the most common, whereas pancreatogastric fistulas are the rarest. In a study from the Mayo Clinic, fistulization was reported in 25 (41%) of the 61 patients operated for SAP. Fourteen of them had cutaneous fistulas, whereas 19 had gastrointestinal (GI) tract fistulas (8 colonic, 5 duodenal, 4 enteric and 2 gastric). A majority of these fistulas are reported after necrosectomy, and rarely is the diagnosis made preoperatively[9].
Rupture of a bleeding pseudocyst into the stomach is rare[3]. Uncomplicated rupture of pseudocyst is an even rarer occurrence[4]. There are only few case reports in literature of uncomplicated spontaneous rupture of pseudocyst into stomach[4,6,8,10].
In conclusion, we have presented a case of patient with a pseudocyst, resulting from a complication of chronic pancreatitis, which resolved spontaneously through the formation of a fistula between the pseudocyst and the stomach. The fistula occluded spontaneously and the patient recovered without complication or need for surgical treatment.
P- Reviewers Amornyotin S, Rabago L S- Editor Zhai HH L- Editor A E- Editor Wu HL
| 1. | Lillemoe KD, Yeo CJ. Management of complications of pancreatitis. Curr Probl Surg. 1998;35:1-98. [PubMed] |
| 2. | Tanaka A, Takeda R, Utsunomiya H, Kataoka M, Mukaihara S, Hayakawa K. Severe complications of mediastinal pancreatic pseudocyst: report of esophagobronchial fistula and hemothorax. J Hepatobiliary Pancreat Surg. 2000;7:86-91. [PubMed] |
| 3. | Urakami A, Tsunoda T, Kubozoe T, Takeo T, Yamashita K, Imai H. Rupture of a bleeding pancreatic pseudocyst into the stomach. J Hepatobiliary Pancreat Surg. 2002;9:383-385. [PubMed] |
| 4. | Mir MF, Shaheen F, Gojwari TA, Singh M, Nazir P, Ahmad S. Uncomplicated spontaneous rupture of the pancreatic pseudocyst into the gut--CT documentation: a series of two cases. Saudi J Gastroenterol. 2009;15:135-136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Feldman M, Friedman LS, Brandt LJ. Sleisenger and Fordtran’s gastrointestinal and liver disease: pathophysiology, diagnosis, management. 9th ed. Philadelphia: Saunders 2010; 1010. |
| 6. | Ali J, Greenberg H. Spontaneous gastric decompression of pancreatic pseudocyst. Can J Surg. 1992;35:104-106. [PubMed] |
| 7. | Clements JL, Bradley EL, Eaton SB. Spontaneous internal drainage of pancreatic pseudocysts. AJR Am J Roentgenol. 1976;126:985-991. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 20] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Yeom HJ, Yi SY. Spontaneous resolution of pancreatic gastric fistula. Dig Dis Sci. 2007;52:561-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Tsiotos GG, Smith CD, Sarr MG. Incidence and management of pancreatic and enteric fistulas after surgical management of severe necrotizing pancreatitis. Arch Surg. 1995;130:48-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 86] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 10. | Brand A, Lankisch PG. Symptomless spontaneous rupture of a pancreatic pseudocyst into the stomach. Rofo. 1989;151:618-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |