Published online May 16, 2013. doi: 10.4253/wjge.v5.i5.240
Revised: July 2, 2012
Accepted: March 15, 2013
Published online: May 16, 2013
AIM: To assess the risk of colonic polyps, adenomas and advanced neoplastic lesions (ANL) in patients with sporadic gastric polyps, especially those with fundic gland polyps (FGP).
METHODS: Clinical records of patients who had performed an upper and a lower digestive endoscopy between September 2007 and August 2008 were retrospectively analyzed. A case-control study was carried out, calling patients with gastric polyps as “cases” and patients without gastric polyps as “controls”. The risk of colonic polyps, adenomas and ANL (villous component ≥ 25%, size ≥ 10 mm, or high grade dysplasia) was assessed [odds ratio (OR) and its corresponding 95%CI].
RESULTS: Two hundred and forty seven patients were analyzed: 78 with gastric polyps (cases) and 169 without gastric polyps (controls). Among the cases, the majority of gastric polyps were FGP (80%, CI: 69-88) and hyperplastic (20%, CI: 12-31); 25% had colonic polyps (25% hyperplastic and 68% adenomas, from which 45% were ANL). Among the controls, 20% had colonic polyps (31% hyperplastic and 63% adenomas, from which 41% were ANL). The patients with sporadic FGP had an OR of 1.56 (CI: 0.80-3.04) for colonic polyps, an OR of 1.78 (CI: 0.82-3.84) for colonic adenomas, and an OR of 0.80 (CI: 0.21-2.98) for ANL. Similar results were found in patients with gastric polyps in general.
CONCLUSION: The results of this study did not show more risk of colorectal adenomas or ANL neither in patients with sporadic gastric polyps nor in those with FGP.
Core tip: The risk of colonic adenomas in patients who have sporadic gastric polyps, especially those of fundic gland polyps (FGP), is still to be definitely determined. The purpose of our study was to assess the risk of colonic polyps, adenomas and advanced neoplastic lesions in patients who have sporadic gastric polyps, especially of FGP, due to the fact that these are the most common gastric polyps in our population.
- Citation: Cimmino DG, Mella JM, Luna P, González R, Pereyra L, Fischer C, Mohaidle A, Vizcaino B, Medrano MA, Hadad A, Pedreira S, Boerr L. Risk of colorectal polyps in patients with sporadic gastric polyps: A case-control study. World J Gastrointest Endosc 2013; 5(5): 240-245
- URL: https://www.wjgnet.com/1948-5190/full/v5/i5/240.htm
- DOI: https://dx.doi.org/10.4253/wjge.v5.i5.240
The occurrence of gastric and duodenal polyps is higher in several colonic polyposis syndromes[1,2]. However, the risk of colonic polyps and adenomas in patients who have sporadic gastric polyps, especially the fundic gland polyps (FGP), remains controversial.
Several authors have studied the relationship between the presence of different types of gastric polyps and the risk of colonic polyps and adenomas[3]. Yang et al[4] reported that the patients who have gastric adenomas could be more prone to present colorectal adenomas, and suggested that in the case of gastric adenomas the patient should be prescribed a screening colonoscopy.
However, the risk of colonic adenomas in patients who have sporadic gastric polyps, especially those of FGP, is still to be definitely determined.
It has been reported that patients suffering from familial adenomatous polyposis (FAP) show an increased incidence of gastric fundic gland polyps; there are series[5] showing that up to 88% of these patients have FGP. The presence of this type of gastric polyps is supposed to be a marker of colonic neoplasia among the general population. In a retrospective study, Teichmann et al[6] showed that patients who had gastric fundic gland polyps were more prone to suffer from colorectal neoplasias. Nevertheless, Dickey et al[7] could not confirm Teichmann’s findings in a prospective study.
The purpose of our study was to assess the risk of colonic polyps, adenomas and advanced neoplastic lesions (ANL) in patients who have sporadic gastric polyps, especially of FGP, due to the fact that these are the most common gastric polyps in our population.
A case-control study was carried out. Patients with gastric polyps were regarded as “cases” and those without them as “controls”. The clinical records of patients who had undergone an upper and a lower digestive endoscopy between September 2007 and August 2008 were retrospectively analysed. Those patients with previous digestive endoscopies, an inadequate colonic cleansing, an incomplete colonoscopy, gastric or colonic surgeries, and intestinal inflammatory disease were excluded.
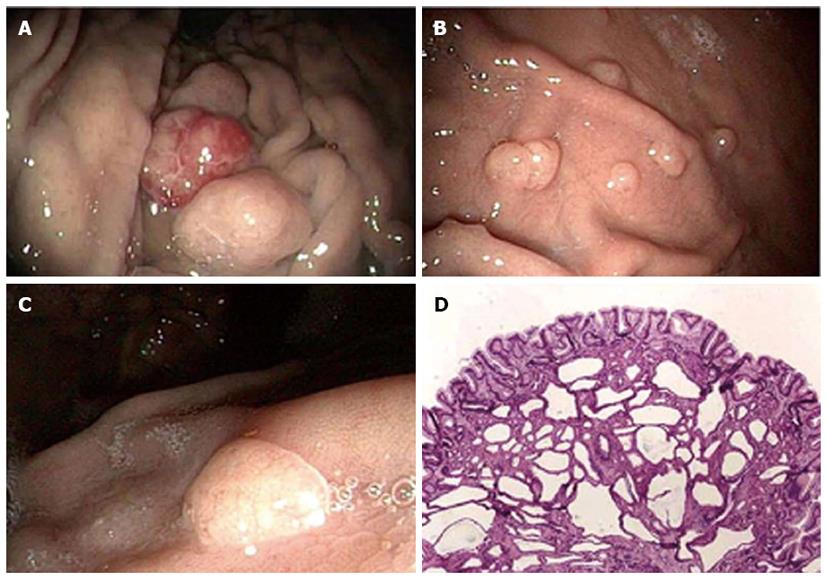
Those patients with gastric polyps were identified by an electronic search in the Endoscopy database. The final diagnosis of the different types of gastric polyps was histopathologically assessed. The presence of fundic gland polyps was suspected by the finding of sessile polyps at the body or fundus of the stomach, with their typical appearance (Figure 1). The diagnosis was confirmed by the histological analysis of polyps resections (polypectomies with forceps or snares). The fundic gland polyps diagnosis was based on the finding of enlarged glands in a cystic shape, covered with fundic epithelium (parietal cells and chief cells) mixed with normal glands, generally without inflammation or evidence of dysplasia. Besides, the grade of inflammation of the gastric mucosa was mostly determined by antral and gastric body biopsies. Gastritis were arbitrary classified in two types. Firstly, “active or severe gastritis” were analysed together and they were diagnosed when the gastric mucosa showed acute inflammatory infiltrate. Secondly, “mild or inactive gastritis” were also analysed together and they were diagnosed by the presence of minor inflammatory lymphoplasmacytic infiltrates. Normal gastric biopsies (which is unusual in our medical field) were also analysed together with those that showed “mild-minor or inactive” inflammation. Infection with Helicobacter pylori (H. pylori) was histopathologically determined due to the presence of curved bacilli typical of H. pylori by using Giemsa’s stain. The diagnosis of the different types of colonic polyps was histopathologically determined.
The risk of colonic polyps, adenomas and ANL (defined as villous component ≥ 25%, size ≥ 10 mm or high grade dysplasia) was assessed in patients with gastric polyps in general, and in particular, in those with FGP.
For constant variables, the media with its corresponding SD was calculated. The nominal variables were expressed in percentages with their corresponding 95%CI. The risk of colonic polyps, adenomas and ANL was calculated, measured in odds ratio (OR) with its corresponding 95%CI, using the Fischer’s test. Results were considered significant when the OR’s with their CI did not include the 1. In order to assess the influence on the main outcomes of the variables that were significantly different between the cases and controls (Table 1), a binary logistic regression model was carried out by introducing these variables, in order to prove if these variables were independent predictor of the outcomes. The relationship between the presence of FGP and the H. pylori infection was also analysed. The SPSS 17.1 software for Windows was used.
| Characteristics of patients | With gastric polyps (n = 78) | Without gastric polyps (n = 169) | P value |
| Age years old (average ± SD) | 62 ± 11 | 61 ± 14 | 0.51 |
| Sex (%women, CI) | 71% (59-81) | 61% (53-68) | 0.11 |
| Gastric polyps (%patients, CI) | |||
| Fundic gland polyps | 80% (69-88) | Did not have gastric polyps | |
| Hyperplastic | 20% (12-31) | ||
| Indications of the UGIEs (%patients, CI) | |||
| Epigastralgia | 38% (29-50) | 46% (39-54) | 0.14 |
| Gastroesophageal reflux | 22% (13-32) | 9% (5-15) | < 0.01 |
| Anemia | 10% (4-19) | 8% (4-13) | 0.32 |
| Abdominal pain | 8% (3-16) | 10% (6-16) | 0.31 |
| Digestive bleeding | 4% (1-10) | 6 % (3-11) | 0.30 |
| Screening | 6 % (2-14) | 9% (5-14) | 0.35 |
| Other | 12% (4-19) | 12% (4-13) | 0.32 |
| Gastric mucosa histology (%patients, CI) | |||
| Minor gastritis | 76% (65-85) | 68% (60-76) | 0.15 |
| Severe gastritis | 24% (15-35) | 32% (24-39) | 0.15 |
| Helicobacter pylori infection (%positives, CI) | 20% (11-31) | 29% (22-38) | 0.07 |
| Indications of the colonoscopies (%patients, CI) | |||
| Screening | 37% (26-49) | 43% (35-50) | 0.25 |
| Abdominal pain | 17% (9-27) | 23% (17-30) | 0.16 |
| Constipation | 18% (10-28) | 7% (3-11) | < 0.01 |
| Anemia | 13% (6-22) | 9% (5-14) | 0.23 |
| Digestive bleeding | 4% (1-11) | 7% (3-12) | 0.24 |
| Other | 11% (5-21) | 11% (6-15) | 0.12 |
| Colonic polyps (%patients, CI) | 25% (16-37) | 20% (14-26) | 0.17 |
| Type of colonic polyps (%colonic polyps, CI) | |||
| Hyperplastic | 25% (7-52) | 31% (16-49) | 0.95 |
| Adenomas | 68% (41-89) | 63% (45-78) | 0.63 |
| ANL | 45% (16-76) of the adenomas | 41% (21-63) of the adenomas | 0.82 |
We analyzed 247 patients (Table 1). Seventy-eight had gastric polyps, from which 62 were of FGP. Table 1 shows the characteristics of patients with and the without gastric polyps.
Among the cases the media age was 62 ± 11 years old, and 71% (CI: 59%-81%) of the patients were women. Most of gastric polyps were FGP (80%, CI: 69%-88%) and hyperplastic (20%, CI: 12%-31%); no gastric adenomas were found. Seventy six percent (76%, CI: 65%-85%) of the patients had inactive or minor gastritis in the gastric mucosa biopsies, and 24% (CI: 15%-35%) had active or severe gastritis. H. pylori infection detected by gastric biopsies was found in 20% (CI: 11%-31%) of patients. The most common indications for the upper gastrointestinal endoscopies (UGIEs) were: epigastralgia (38%) and typical gastroesophageal reflux disease (GERD) symptoms (22%). Twenty five percent (25%, CI: 16%-37%) of the cases had colonic polyps from which 25% were hyperplastic and 68% were adenomas (45% of the adenomas were ANL). The most common indications for colonoscopies were: colorectal cancer screening (37%) and constipation (18%).
Among the controls, the media age was 61 ± 14 years old, and 61% (CI: 53%-68%) of the patients were women. Sixty eight percent (68%, CI: 60%-76%) of the controls had inactive or minor gastritis in the gastric biopsies and 32% (CI: 24%-39%) had active or severe gastritis. The gastric biopsies showed that 29% (CI: 22%-38%) of the patients had H.pylori infection. The most common indications for the UGIEs were: epigastralgia (46%) and typical GERD symptoms (9%). Twenty percent (20%, CI: 14%-26%) of patients had colonic polyps, from which 31% were hyperplastic and 63% were adenomas (41% of these adenomas were ANL). The most common indications for the colonoscopies were: colorectal cancer screening (43%) and abdominal pain (23%).
Within the patients who had colonic polyps, none of them had colonic polyposis at the moment of the colonic examination. The average number of colonic polyps in each patient who had colonic polyps was 1.46 ± 1 polyp, and the range was from 1 to 6 polyps (in only one patient we found 6 polyps in the colon, from which 3 were hyperplastic and 3 adenomas).
The prevalence of gastric infection due to H. pylori was lower among the patients who had gastric polyps in comparison with the ones without them (29% vs 20%, P = 0.07). This difference was significantly bigger when the group of patients with and without FGP were analyzed (31% vs 14%, P = 0.01); the relative chances of having the H. pylori infection were 63% less (OR: 0.37, CI: 0.16-0.86) in the patients who had FGP.
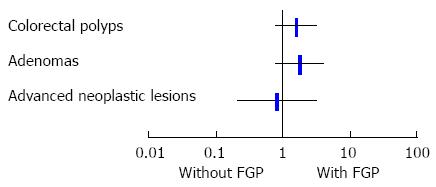
Table 2 shows the main outcomes. Patients with gastric polyps had an OR of 1.41 (CI: 0.75-2.68) for having colonic polyps, an OR of 1.63 (CI: 0.77-3.42) for having adenomas, and an OR of 1.67 (CI: 0.56-5.01) for ANL. Patients with FGP (Figure 2) had an OR of 1.56 (CI: 0.80-3.04) for having colonic polyps, an OR of 1.78 (CI: 0.82-3.84) for having colonic adenomas, and an OR of 0.80 (CI: 0.21-2.98) for ANL. When using a binary logistic regression model for detecting influences on the risk of colonic polyps, adenomas and ANL between cases and controls (Table 3), we observed that the indications of the endoscopies (especially typical GERD symptoms and constipation) and the H. pylori infection were not determinants of our main outcomes.
| Colonic polyps | Colonic adenomas | ANL | |
| (OR, 95%CI) | (OR, 95%CI) | (OR, 95%CI) | |
| Presence of gastric polyps | 1.41 | 1.63 | 1.67 |
| (0.75-2.68) | (0.77-3.42) | (0.56-5.01) | |
| Presence of gastric fundic gland polyps | 1.56 | 1.78 | 0.8 |
| (0.80-3.04) | (0.82-3.84) | (0.21-2.98) |
| P value | |||
| Colonic polyps | Colonic adenomas | ANL | |
| Female sex | 0.488 | 0.121 | 0.369 |
| GERD | 0.457 | 0.969 | 0.525 |
| Constipation | 0.083 | 0.865 | 0.613 |
| Helicobacter pylori infection | 0.557 | 0.292 | 0.772 |
The aim of this study was to establish the risk of colonic polyps and adenomas in patients with gastric polyps, especially those of FGP. We did not find any relationship between the presence of FGP and colorectal polyps (OR: 1.56, CI: 0.80-3.04). In addition, we could not prove that the presence of this kind of gastric polyps predisposed patients to ANL (which might be considered as a surrogate outcome of colorectal cancer; OR: 0.80, CI: 0.21-2.98). It is very important to point out that in our study there were no patients with colonic polyposis syndromes, and therefore, among the patients who had gastric polyps, their origin could be labelled as “sporadic”. Our results are important because they are different from other author’s.
In 2002, in a prospective study, Jung et al[8] concluded that patients who had FGP (Elster’s cysts) could have a higher incidence of colorectal tumours and should undergo a diagnostic colonoscopy. These authors found a highly remarkable preponderance of colon adenocarcinoma (12.5%) among the 65 patients analysed who had FGP. In our study none of the 62 patients who had FGP presented colorectal cancer.
In 2005, Declich et al[9] suggested that patients who had sporadic FGP should undergo a colonoscopy since they could be more prone to have colonic adenomas. However, in their study, such conclusion is not clearly justified or stated.
In 2008, in a retrospective study, Teichmann et al[6] showed that patients who had gastric fundic gland polyps were more prone to suffer from colorectal neoplasias (15.5% in patients with FGP vs 9.2% in controls, P < 0.05), although they could not prove a higher occurrence of colonic polyps. In their study, the FGPs were diagnosed in patients undergoing endoscopies because of gastrointestinal bleeding, which in term could have originated a selection bias. According to this, the positive relationship between gastric fundic gland polyps and colorectal cancer could be influenced by bias in the process of selection of the patients included in the study. In our study, the gastrointestinal bleeding accounted for less than 10% of the endoscopy indications. We also carried out a logistic regression to determine the influence of the endoscopy indications on the main outcomes.
In 2009, Genta et al[10] published the biggest cohort, so far, of patients who had FGP. They assessed the risk of presenting colorectal neoplasias in patients with FGP. The authors analysed 6081 patients who had FGP and showed that the risk of presenting colorectal adenomas was higher among the women who had FGP (OR: 1.43, 95%CI: 1.26-1.63) and would not be increased among the men. They also showed that patients without FGP could be 29 times more prone to be infected with the H. pylori bacteria as compared to the patients who had FGP (OR: 29, 95%CI: 20-41). In our study, gastric infection with the bacteria H. pylori was almost 3 times more frequent in patients without FGP than in patients with them (OR: 2.65, CI: 1.15-6.27). The presence of FGP was related to a relative reduction of 63% in the risk of H. pylori infection. We couldn´t infer that female sex could be a conclusive element in the presence of colonic lesions in patients with FGP as we found that sex had not influence in our main outcomes (Table 3).
Advantages: (1) strict exclusion criteria based on the factors which could increase the power of the bias and modify the analysed groups; (2) thorough description of the characteristics of the patients analysed in both groups; (3) none of the patients included was given a colonic polyposis diagnosis; and (4) correct statistical analysis. Limits: it is a retrospective study.
In the daily practice it is very common to attend patients with “sporadic” FGP which are nowadays the most usual type of gastric polyps in our medical field. The results of this study did not show an increase in the risk of colorectal adenomas or ANL neither in patients with sporadic polyps of FGP, nor in patients with gastric polyps in general. It is very important to point out that we didn´t find gastric adenomas in the patients included, because it is well known that the presence of gastric adenomas have already been shown to be a risk for colorectal adenomas[4]. In our population, the prevalence of gastric adenomas is extremely low. It might be because Argentina has a population with low basal risk for gastric cancer, and also because of the low prevalence of H. pylori infection (close to 15%-30%) in our patients.”
These results are important because they mark a distinguishing difference between patients with “sporadic” gastric fundic gland polyps and patients who present colonic polyposis hereditary syndromes and who have gastric fundic gland polyps.
In accordance with the findings of other authors, the patients with FGP would be more prone to have “normal” stomachs (“normal, mild or minor” gastritis) and would have less chances of having the H. pylori infection. Unfortunately, as our study was retrospective, we could not analyze any connection between proton pump inhibitors (PPI) intake and the presence of FGP, because we could not get secure data about how many patients were on long PPI treatment at the moment of their endoscopies.
Nowadays, it is common to find incidental gastric polyps in upper gastrointestinal endoscopies. It is well known that the incidence of gastric and duodenal polyps is higher in several colonic polyposis syndromes. However, the risk of finding colonic polyps and adenomas in patients with sporadic gastric polyps, especially the fundic gland polyps (FGP), is not well established. The aim of this study was to assess the risk of presenting colonic polyps, adenomas and advanced neoplastic lesions (ANL) in patients with sporadic gastric polyps, especially those with sporadic FGP.
These results are important because they are different from other author’s. The authors did not find any relationship between the presence of FGP and colorectal polyps [odds ratio (OR) 1.56, CI: 0.80-3.04]. In addition, the authors could not prove that the presence of this kind of gastric polyps predisposed patients to ANL (which might be considered as a surrogate outcome of colorectal cancer; OR: 0.80, CI: 0.21-2.98). It is very important to point out that in this study there were no patients with colonic polyposis syndromes, and therefore, among the patients who had gastric polyps, their origin could be labelled as “sporadic”.
In the daily practice it is very common to attend patients with “sporadic” FGP which are nowadays the most usual type of gastric polyps in this medical field. The results of this study suggest that patients with FGP gastric polyps do not have an increase in the risk of colorectal adenomas or ANL.
The study by Dr. Cimmino et al is interesting and important from clinical point of view. During advanced upper gastrointestinal (GI) endoscopy and colonoscopy person see more and more polyps either in the upper GI tract or in the large bowel. The authors analyzed 78 gastric polyp cases and 169 controls without gastric polyps. Colonoscopy was performed in all cases and the authors studied whether the presence of gastric polyps increases the risk of colorectal polyps. They detected that neither sporadic gastric polyps nor FGP are risks for colorectal adenomas and polyps.
P- Reviewers Rácz I, Campo SMA S- Editor Song XX L- Editor A E- Editor Zhang DN
| 1. | Gu GL, Wang SL, Wei XM, Bai L. Diagnosis and treatment of Gardner syndrome with gastric polyposis: a case report and review of the literature. World J Gastroenterol. 2008;14:2121-2123. |
| 2. | Attard TM, Cuffari C, Tajouri T, Stoner JA, Eisenberg MT, Yardley JH, Abraham SC, Perry D, Vanderhoof J, Lynch H. Multicenter experience with upper gastrointestinal polyps in pediatric patients with familial adenomatous polyposis. Am J Gastroenterol. 2004;99:681-686. |
| 3. | Cappell MS, Fiest TC. A multicenter, multiyear, case-controlled study of the risk of colonic polyps in patients with gastric polyps. Are gastric adenomas a new indication for surveillance colonoscopy? J Clin Gastroenterol. 1995;21:198-202. |
| 4. | Yang MH, Son HJ, Lee JH, Kim MH, Kim JY, Kim YH, Chang DK, Rhee PL, Kim JJ, Rhee JC. Do we need colonoscopy in patients with gastric adenomas? The risk of colorectal adenoma in patients with gastric adenomas. Gastrointest Endosc. 2010;71:774-781. |
| 5. | Bianchi LK, Burke CA, Bennett AE, Lopez R, Hasson H, Church JM. Fundic gland polyp dysplasia is common in familial adenomatous polyposis. Clin Gastroenterol Hepatol. 2008;6:180-185. |
| 6. | Teichmann J, Weickert U, Riemann JF. Gastric fundic gland polyps and colonic polyps - is there a link, really? Eur J Med Res. 2008;13:192-195. |
| 7. | Dickey W, Kenny BD, McConnell JB. Prevalence of fundic gland polyps in a western European population. J Clin Gastroenterol. 1996;23:73-75. |
| 8. | Jung A, Vieth M, Maier O, Stolte M. Fundic gland polyps (Elster’s cysts) of the gastric mucosa. A marker for colorectal epithelial neoplasia? Pathol Res Pract. 2002;198:731-734. |
| 9. | Declich P, Tavani E, Ferrara A, Caruso S, Bellone S. Sporadic fundic gland polyps: clinico-pathologic features and associated diseases. Pol J Pathol. 2005;56:131-137. |
| 10. | Genta RM, Schuler CM, Robiou CI, Lash RH. No association between gastric fundic gland polyps and gastrointestinal neoplasia in a study of over 100,000 patients. Clin Gastroenterol Hepatol. 2009;7:849-854. |