Published online Mar 16, 2013. doi: 10.4253/wjge.v5.i3.138
Revised: November 8, 2012
Accepted: January 5, 2013
Published online: March 16, 2013
Processing time: 183 Days and 23.7 Hours
Gastric antral vascular ectasia (GAVE) has been recognized as one of the important causes of occult and obscure gastrointestinal bleeding. The diagnosis is typically made based on the characteristic endoscopic features, including longitudinal row of flat, reddish stripes radiating from the pylorus into the antrum that resemble the stripes on a watermelon. These appearances, however, can easily be misinterpreted as moderate to severe gastritis. Although it is believed that capsule endoscopy (CE) is not helpful for the study of the stomach with its large lumen, GAVE can be more likely to be detected at CE rather than conventional endoscopy. CE can be regarded as “physiologic” endoscopy, without the need for gastric inflation and subsequent compression of the vasculature. The blood flow of the ecstatic vessels may be diminished in an inflated stomach. Therefore, GAVE may be prominent in CE. We herein describe a case of active bleeding from GAVE detected by CE and would like to emphasize a possibility that CE can improve diagnostic yields for GAVE.
- Citation: Ohira T, Hokama A, Kinjo N, Nakamoto M, Kobashigawa C, Kise Y, Yamashiro S, Kinjo F, Kuniyoshi Y, Fujita J. Detection of active bleeding from gastric antral vascular ectasia by capsule endoscopy. World J Gastrointest Endosc 2013; 5(3): 138-140
- URL: https://www.wjgnet.com/1948-5190/full/v5/i3/138.htm
- DOI: https://dx.doi.org/10.4253/wjge.v5.i3.138
Although gastric antral vascular ectasia (GAVE) has been recognized as the uncommon cause of chronic anemia, its active bleeding has been documented very rarely. We present a case of active bleeding from GAVE detected by capsule endoscopy (CE).
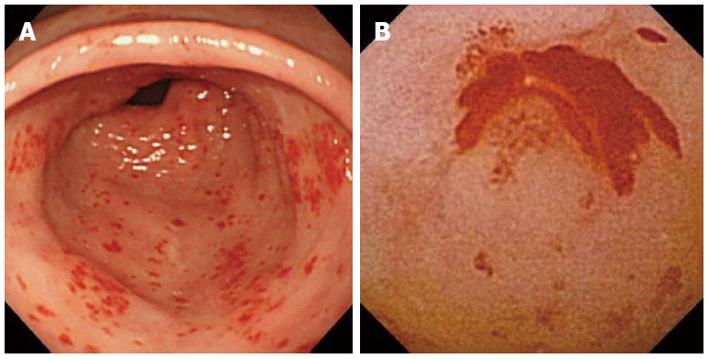
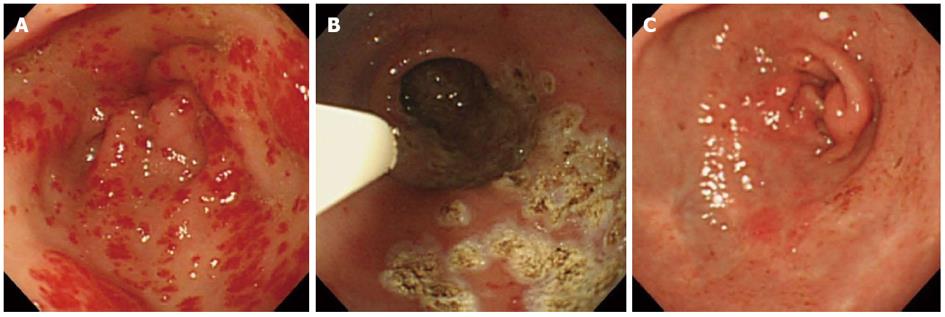
A 77-year-old woman who had had mitral valve replacement with warfarin presented with dyspnea. Heart failure due to anemia was diagnosed. Fecal occult blood test was positive and repeated blood transfusion was required. The diagnosis of superficial gastritis was made by first endoscopy and was not regarded as the bleeding source (Figure 1A). Colonoscopy was negative. CE was performed for the examination of the small intestine, which disclosed active bleeding from GAVE (Figure 1B). Repeated endoscopy showed the classical “watermelon stomach” appearance of GAVE (Figure 2A). GAVE was then treated with repeated endoscopic argon plasma coagulation (APC), abolishing blood transfusion (Figure 2B). Follow-up endoscopy disclosed the improvement of GAVE with scar formation (Figure 2C).
GAVE has been described in association with various diseases, including liver cirrhosis and chronic renal failure[1]. It is one of the important causes of occult and obscure gastrointestinal bleeding[2]. The diagnosis is typically made based on the characteristic endoscopic appearance. The endoscopic features include longitudinal row of flat, reddish stripes radiating from the pylorus into the antrum that resemble the stripes on a watermelon or a diffuse pattern of small, punctuate spots primarily in the antrum. These appearances, however, can easily be misinterpreted as moderate to severe gastritis[3], as in this case. Recent studies indicated that GAVE can be more likely to be detected at CE rather than conventional endoscopy[4-7]. CE can be regarded as “physiologic” endoscopy, without the need for gastric inflation and subsequent compression of the vasculature[5]. The blood flow of the ecstatic vessels may be diminished in an inflated stomach[6]. Therefore, GAVE may be prominent in CE. Our case illustrates a possibility that CE can improve diagnostic yields for GAVE. Appropriate diagnosis and treatments including APC are critical for the favorable outcome.
P- Reviewers Sumiyama K, Su MY S- Editor Gou SX L- Editor A E- Editor Zhang DN
| 1. | Gostout CJ, Viggiano TR, Ahlquist DA, Wang KK, Larson MV, Balm R. The clinical and endoscopic spectrum of the watermelon stomach. J Clin Gastroenterol. 1992;15:256-263. [PubMed] |
| 2. | Bresci G. Occult and obscure gastrointestinal bleeding: Causes and diagnostic approach in 2009. World J Gastrointest Endosc. 2009;1:3-6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Yamada M, Nishimura D, Hoshino H, Katada N, Sano H, Kato K. Gastric antral vascular ectasia successfully treated by endoscopic electrocoagulation. J Gastroenterol. 1998;33:546-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Raju GS, Morris K, Boening S, Carpenter D, Gomez G. Capillary refilling sign demonstrated by capsule endoscopy. Gastrointest Endosc. 2003;58:936-937. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Kitiyakara T, Selby W. Non-small-bowel lesions detected by capsule endoscopy in patients with obscure GI bleeding. Gastrointest Endosc. 2005;62:234-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 42] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 6. | Sidhu R, Sanders DS, McAlindon ME. Does capsule endoscopy recognise gastric antral vascular ectasia more frequently than conventional endoscopy? J Gastrointestin Liver Dis. 2006;15:375-377. [PubMed] |
| 7. | Rimbaş M, Haidar A, Voiosu MR. Computed virtual chromoendoscopy - enhanced videocapsule endoscopy is of potential benefit in gastric antral vascular ectasia syndrome refractory to endoscopic treatment. J Gastrointestin Liver Dis. 2011;20:307-310. [PubMed] |