Published online Feb 16, 2010. doi: 10.4253/wjge.v2.i2.54
Revised: September 12, 2009
Accepted: September 19, 2009
Published online: February 16, 2010
Upper gastrointestinal hemorrhage (UGIH) is an urgent disease that is often encountered in daily medical practice. Endoscopic hemostasis is currently indispensable for the treatment of UGIH. Initially, when UGIH is suspected, a cause of UGIH is presumed from the medical interview and physical findings. After ample primary treatment, urgent endoscopy is performed. Many methods of endoscopic hemostasis are in wide use, including hemoclip, injection and thermo-coagulation methods. Although UGIH develops from a wide variety of diseases, such as esophageal varices and gastric and duodenal ulcer, hemostasis is almost always possible. Identification of the causative diseases, primary treatment and characteristic features of endoscopic hemostasis are needed to allow appropriate treatment.
- Citation: Anjiki H, Kamisawa T, Sanaka M, Ishii T, Kuyama Y. Endoscopic hemostasis techniques for upper gastrointestinal hemorrhage: A review. World J Gastrointest Endosc 2010; 2(2): 54-60
- URL: https://www.wjgnet.com/1948-5190/full/v2/i2/54.htm
- DOI: https://dx.doi.org/10.4253/wjge.v2.i2.54
Upper gastrointestinal hemorrhage (UGIH) is an urgent disease often encountered in daily medical practice. Massive hemorrhage influences the circulatory dynamic state, causes various problems with internal organs, and can of course prove fatal. Quickly grasping patient status, starting primary treatment, and stopping bleeding is thus important. Endoscopic hemostasis is widely known to be useful in treating UGIH[1-5]. However, difficult cases in endoscopic hemostasis still exist, and emergency operation or angiographic embolization is required on occasion[6-9]. To achieve quick hemostasis in UGIH, mastering the methods and limitations of endoscopic hemostasis is imperative. Here we review clinical methods of endoscopic hemostasis for UGIH, based on our experience.
Patients with UGIH present with various symptoms, such as hematemesis, melena and progressive anemia. Sources of bleeding other than the digestive tract must first be excluded, including hemoptysis, epistaxis, and discrimination of lower digestive hemorrhage[10]. Table 1 shows causative diseases for UGIH. Peptic ulcer is the most common causative disease[1,6,11,12]. When UGIH is suspected, causes of UGIH may be presumed from the medical interview and physical findings. The strategy for hemostasis of UGIH with primary treatment is then considered.
| Esophagus | Esophageal varices |
| Esophagitis | |
| Mallory-weiss syndrome | |
| Esophageal cancer | |
| Others (aortointestinal fistula, foreign body, etc.) | |
| Stomach | Ulcer (peptic ulcer, NSAID-associated ulcer, dieulafoy’s lesion, etc.) |
| AGML | |
| Gastric varices | |
| Gastric cancer | |
| Other tumor (GIST, malignant lymphoma, etc.) | |
| Vascular ectasia, GAVE, PHG | |
| Hyperplastic polyp | |
| Others (foreign body, etc.) | |
| Duodenum | Ulcer (peptic ulcer, NSAID-associated ulcer, dieulafoy’s lesion, etc.) |
| Duodenitis | |
| Duodenal varices | |
| Diverticulum | |
| Tumor (cancer, malignant lymphoma, GIST, etc.) | |
| Invasion of malignant tumor (pancreas, bile duct, etc.) | |
| Others (hemobilia, aortointestinal fistula, etc.) |
A firm grasp of the systemic status is important. Signs of shock, pallor, prostration, perspiration, pulselessness and pulmonary insufficiency suggest massive digestive hemorrhage. Above all, stabilization of the circulatory dynamic state by intravenous injection of extracellular fluid is crucial[10]. In addition, an inhibitor of gastric acid-secretion should be given as quickly as practically possible, as gastric acid inhibits blood coagulation[13]. If massive hemorrhage is suspected from gastroesophageal varices in patients with liver disease, vasoactive drugs (such as terlipressin, somatostatin and octreotide) should be started for initial management before therapeutic endoscopy[14,15]. Temporary balloon tamponade, such as Sengstaken-Blakemore tubes, must be used with care to prevent further complications[16,17]. If coagulopathy is present, transfusion is necessary. When the circulatory dynamic state is stable and UGIH has been judged as a cause of shock, urgent endoscopy is performed.
The methods of endoscopic hemostasis are shown in Table 2. Hemostasis can be performed using independent or combined methods. The hemoclip grips the exposed blood vessel directly and stops bleeding. Destruction of organization is minimal, and hemostatic ability is high[18]. However, this method requires technical skill to maintain a front view of the exposed blood vessel. When difficulty is encountered, a transparent cap can prove useful[19].
| Mechanical method | Hemoclip |
| Balloon tamponade | |
| Ligation (EVL, detachable snare) | |
| Injection method | Ethanol |
| Epinephrine | |
| Monoethanolamine oleate | |
| Polidocanol | |
| N-butyl-2-cyanoacrylate | |
| Thermo-coagulation | APC |
| Heater prove | |
| Hemostatic forceps | |
| Microwaves | |
| Laser (Nd-YAG, diode, etc.) | |
| Hemostyptic sprays | Thrombin |
| Sodium alginate | |
| Fibrin glue |
Injection methods are effective over a wider range than the hemoclip method, and can be used even if a front view of the bleeding point cannot be maintained. A combination of injection method and other methods is even more effective[20]. However, careful attention is required, due to the risk of delayed perforation.
Thermo-coagulation methods are also effective if a front view of the bleeding point cannot be maintained. These techniques are useful in many cases[21,22], but again carry the possibility of delayed perforation.
As the last method, hemostyptic sprays are used as supplementary treatments[20]. Various methods of hemostasis are selected by adjusting to the individual’s condition.
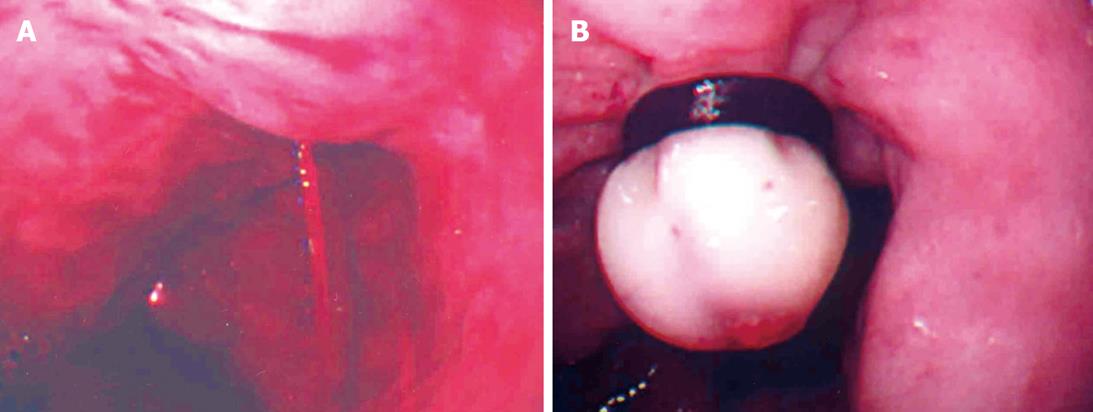
Esophageal varices are frequent in patients with liver cirrhosis. If bleeding from the esophageal varices continues, endoscopic balloon tamponade can be effective for stopping bleeding. Next, endoscopic variceal ligation (EVL) is generally used at the bleeding point (Figure 1A and B). After temporary hemostasis, aiming toward permanent hemostasis is desirable.
In the EVL method, application of the bands is started at the gastroesophageal junction and progresses cephalad in a helical fashion. EVL sessions are repeated at approximately 2-wk intervals until varices are obliterated, usually requiring 2 to 4 ligation sessions. EVL is a safer method than endoscopic injection sclerotherapy (EIS)[23]. When technical factors, such as ulcer scars, do not allow ligation band placement, EIS is selected.
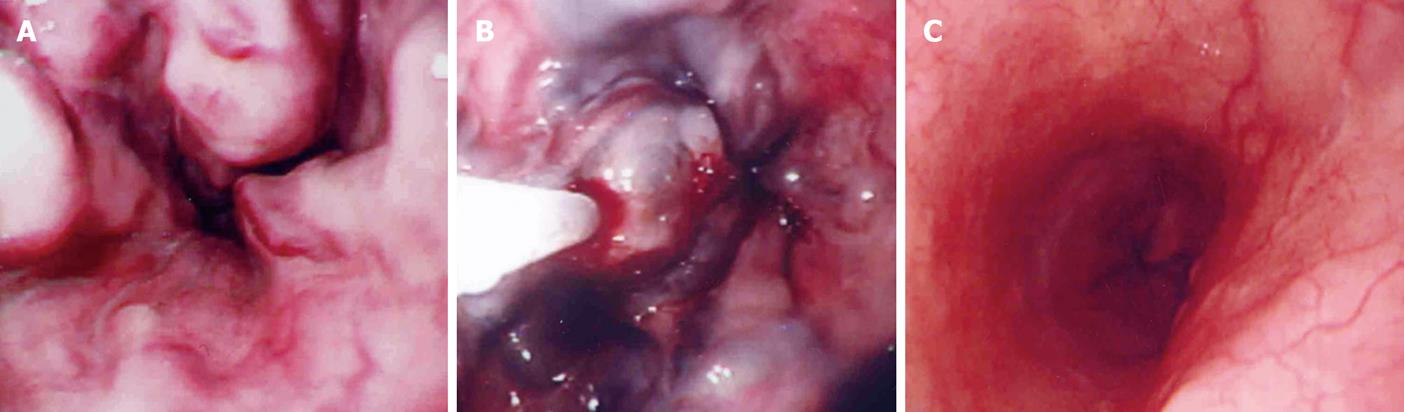
In EIS, to prevent variceal recurrence, complete obliteration of feeder vessels should be verified under fluoroscopy (Figure 2A-C)[24]. Also, combined EVL and EIS treatment is reportedly superior to a single method[25,26].
Recently, bacterial infections and/or endotoxaemia have been associated with failure to control variceal bleeding, earlier variceal rebleeding, abnormalities in coagulation, vasodilatation of the systemic vasculature, and worsening liver function[27]. Prophylactic antibiotics are recommended for patients with bleeding varices[28].
There are no clear hemostasis options as salvage for failure of endoscopic therapy. A transjugular intrahepatic portosystemic shunt (TIPS) procedure is effective to prevent variceal rebleeding, but it may cause complications such as portosystemic encephalopathy[29,30]. Despite being an invasive procedure, a portocaval shunt operation is one of the effective choices in patients with Child’s A or B. Patients with Child’s B or C cirrhosis should be evaluated for transplantation[23,31].
Gastric varices cause massive hemorrhage and can be fatal. Identifying the tributaries of the gastric varices is most important, and contrast-enhanced CT is useful for appraisal. Depending on their location and relation to esophageal varices, gastric varices can be classified as gastrooesophageal varices (GOV) and isolated gastric varices (IGV). Each of these can be further subdivided as follows: GOV1 (extension of oesophageal varices along lesser curve) and GOV2 (extension of oesophageal varices towards fundus); and IGV1 (varices in the fundus) and IGV2 (isolated varices anywhere in the stomach)[32]. If traffic with esophageal varices is seen, EIS from the esophageal varices is effective. In cases of IGV1, endoscopic injection of N-butyl-2-cyanoacrylate[33,34] and combined EVL methods[35] are reportedly safe and effective. If a gastro-renal shunt exists, balloon-occluded retrograde obliteration (B-RTO) under angiography is possible[36,37].
When endoscopic therapy fails, TIPS and surgical operation are mentioned as salvage in the same way as esophageal varices. Splenectomy is quite effective in treating gastric varices due to segmental portal hypertension. For gastric varices bleeding due to generalized portal hypertension, a shunt operation is often effective[23,38].
Gastric and duodenal ulcers include various ulcers such as peptic ulcer, ulcers associated with use of non-steroidal anti-inflammatory drugs (NSAIDs) and Dieulafoy’s lesion. All of these ulcers can cause UGIH, which then needs treatment.
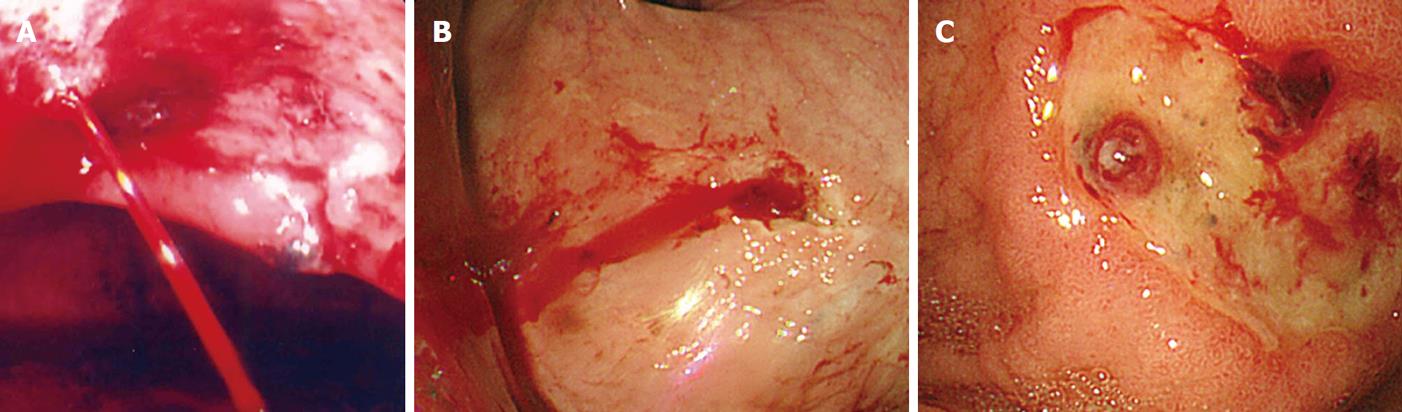
Previous studies have clarified adaptations of hemostasis for hemorrhagic ulcer. Table 3 shows the modified Forrest classification for hemorrhagic gastric ulcer[1,39] Adaptation is decided according to the state of the exposed blood vessel at the base of the ulcer[40-42]. Specifically, spurting bleeding (Figure 3A), oozing bleeding (Figure 3B) and non-bleeding visible vessels (Figure 3C) need to be treated. Clot clinging to the ulcer base should be carefully removed by washing, suction and forceps until the ulcer base is visible. Ulcers can be treated with independent or combined methods. As each method offers certain characteristic features, discussing the advantages and disadvantages of these methods is difficult[43,44]. In previous reports, a combination of injection methods with other methods has appeared superior to injection methods alone[44-49]. Dieulafoy’s lesion can be treated with these endoscopic hemostasis methods[50,51]. Acute gastric mucosal lesions apply to gastric ulcers.
| Active bleeding | Type Ia: spurting bleeding |
| Type Ib: oozing bleeding | |
| Recent bleeding | Type IIa: non-bleeding visible vessel |
| Type IIb: adherent blood clot | |
| Type IIc: black base | |
| No bleeding | Type III: no stigma |
After temporary hemostasis, systemic second-look endoscopy with retreatment the next day significantly reduces the risk of recurrent bleeding[52]. Administration of a proton pump inhibitor (PPI) after hemostasis is also important[53] and Helicobacter pylori should be eradicated in peptic ulcers showing positive results for this bacteria[54].
Endoscopic hemostasis for severe upper gastrointestinal bleeding due to tumor, such as cancer, gastrointestinal stromal tumor, and malignant lymphoma, is effective as temporary hemostasis[55]. Argon plasma coagulation is useful, in particular, for different cases of identification of the vessel responsible for the bleeding[56,57]. However, permanent hemostasis is difficult in many cases due to diffuse bleeding. Early consultation with a surgeon is warranted in cases where hemostasis is difficult to achieve.
Mallory-Weiss syndrome heals spontaneously in many cases, but endoscopic therapy is occasionally necessary to stop bleeding. Various methods have been reported, such as Hemoclip placement, epinephrine injection and band ligation[58,59].
The few cases of reflux esophagitis requiring endoscopic hemostasis are treated with a PPI, and most cases heal with conservative therapy. However, when an anticoagulant drug is being administered or bleeding tendencies exist, chronic bleeding can continue. These cases must be treated by addressing the bleeding tendency[60].
UGIH is sometimes induced by vascular ectasia, such as gastric antral vascular ectasia, diffuse antral vascular ectasia or portal hypertensive gastropathy. In many cases, the cause of vascular ectasia is unclear. Chronic bleeding from vascular ectasia is typically noticed by progressive anemia. Argon plasma coagulation[61,62] and endoscopic band ligation[63] are useful for hemostasis.
Hyperplastic polyps of the stomach are usually asymptomatic, but can cause UGIH leading to anemia. The majority of such lesions are benign, but when a polyp exceeds 2 cm in maximum diameter, the frequency of focal cancer increases. Pathological diagnosis of large polyps is thus desirable[64].
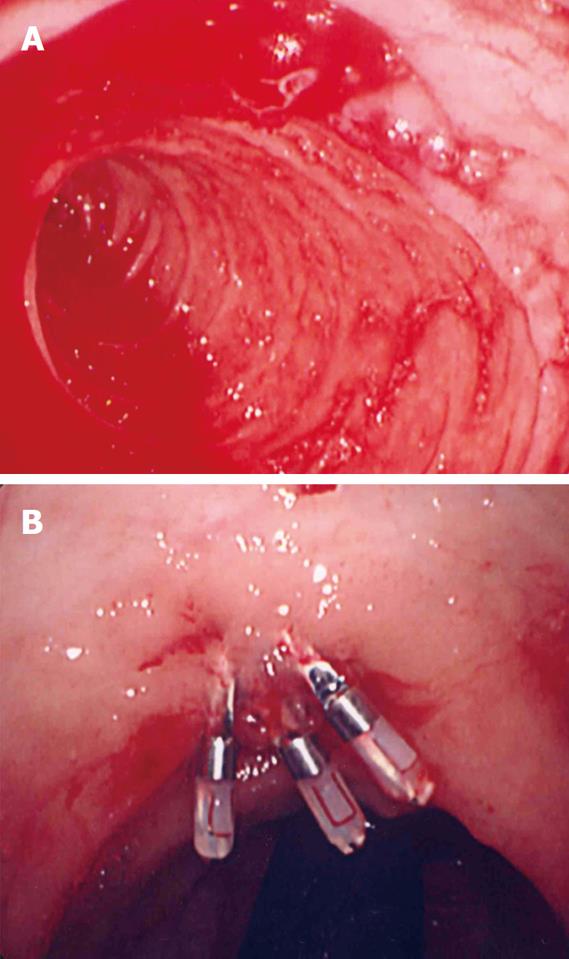
Duodenal diverticulum is a rare cause of UGIH, and endoscopy is reportedly useful for diagnosis and treatment of this condition[65]. Patients receive various endoscopic therapies, such as thermo-coagulation, injection, and hemoclip. The point of the hemoclip method is to grasp a vessel, diverticulum and other tissue (Figure 4A and B).
We have provided an outline of endoscopic hemostasis for UGIH. For the digestive endoscopist, endoscopic hemostasis is a field that cannot be avoided. Being prepared to take proper measures is important. As the causes of UGIH differ in various patients, knowledge of UGIH including causes and preferred treatments requires constant attention.
Peer reviewers: Akira Hokama, MD, PhD, First Department of Internal Medicine, University of the Ryukyus, 207 Uehara, Nishihara, Okinawa 903-0215, Japan; Sherman M Chamberlain, Associate Professor of Medicine, Section of Gastroenterology, BBR-2538, Medical College of Georgia, Augusta, GA 30912, United States
| 1. | Kohler B, Riemann JF. Upper GI-bleeding--value and consequences of emergency endoscopy and endoscopic treatment. Hepatogastroenterology. 1991;38:198-200. |
| 2. | Sacks HS, Chalmers TC, Blum AL, Berrier J, Pagano D. Endoscopic hemostasis. An effective therapy for bleeding peptic ulcers. JAMA. 1990;264:494-499. |
| 3. | Jensen DM, Kovacs TO, Jutabha R, Machicado GA, Gralnek IM, Savides TJ, Smith J, Jensen ME, Alofaituli G, Gornbein J. Randomized trial of medical or endoscopic therapy to prevent recurrent ulcer hemorrhage in patients with adherent clots. Gastroenterology. 2002;123:407-413. |
| 4. | Sung JJ, Chan FK, Lau JY, Yung MY, Leung WK, Wu JC, Ng EK, Chung SC. The effect of endoscopic therapy in patients receiving omeprazole for bleeding ulcers with nonbleeding visible vessels or adherent clots: a randomized comparison. Ann Intern Med. 2003;139:237-243. |
| 5. | Kahi CJ, Jensen DM, Sung JJ, Bleau BL, Jung HK, Eckert G, Imperiale TF. Endoscopic therapy versus medical therapy for bleeding peptic ulcer with adherent clot: a meta-analysis. Gastroenterology. 2005;129:855-862. |
| 6. | Starlinger M, Becker HD. Upper gastrointestinal bleeding--indications and results in surgery. Hepatogastroenterology. 1991;38:216-219. |
| 7. | Rockall TA. Management and outcome of patients undergoing surgery after acute upper gastrointestinal haemorrhage. Steering Group for the National Audit of Acute Upper Gastrointestinal Haemorrhage. J R Soc Med. 1998;91:518-523. |
| 8. | Keller FS, Routh WD. Angiographic diagnosis and management. Hepatogastroenterology. 1991;38:207-215. |
| 9. | Loffroy R, Guiu B, Cercueil JP, Lepage C, Latournerie M, Hillon P, Rat P, Ricolfi F, Krausé D. Refractory bleeding from gastroduodenal ulcers: arterial embolization in high-operative-risk patients. J Clin Gastroenterol. 2008;42:361-367. |
| 10. | Cappell MS, Friedel D. Initial management of acute upper gastrointestinal bleeding: from initial evaluation up to gastrointestinal endoscopy. Med Clin North Am. 2008;92:491-509, xi. |
| 11. | Henrion J, Schapira M, Ghilain JM, Maisin JM, De Maeght S, Deltenre P, Moulart M, Delaunoit T. Upper gastrointestinal bleeding: What has changed during the last 20 years? Gastroenterol Clin Biol. 2008;Epub ahead of print. |
| 12. | van Leerdam ME. Epidemiology of acute upper gastrointestinal bleeding. Best Pract Res Clin Gastroenterol. 2008;22:209-224. |
| 13. | Lau JY, Leung WK, Wu JC, Chan FK, Wong VW, Chiu PW, Lee VW, Lee KK, Cheung FK, Siu P. Omeprazole before endoscopy in patients with gastrointestinal bleeding. N Engl J Med. 2007;356:1631-1640. |
| 14. | Dell'Era A, de Franchis R, Iannuzzi F. Acute variceal bleeding: pharmacological treatment and primary/secondary prophylaxis. Best Pract Res Clin Gastroenterol. 2008;22:279-294. |
| 15. | Villanueva C, Balanzó J. Variceal bleeding : pharmacological treatment and prophylactic strategies. Drugs. 2008;68:2303-2324. |
| 16. | Cook D, Laine L. Indications, technique, and complications of balloon tamponade for variceal gastrointestinal bleeding. J Intensive Care Med. 1992;7:212-218. |
| 17. | Chong CF. Esophageal rupture due to Sengstaken-Blakemore tube misplacement. World J Gastroenterol. 2005;11:6563-6565. |
| 18. | Lai YC, Yang SS, Wu CH, Chen TK. Endoscopic hemoclip treatment for bleeding peptic ulcer. World J Gastroenterol. 2000;6:53-56. |
| 19. | Kim JI, Kim SS, Park S, Han J, Kim JK, Han SW, Choi KY, Chung IS, Chung KW, Sun HS. Endoscopic hemoclipping using a transparent cap in technically difficult cases. Endoscopy. 2003;35:659-662. |
| 20. | Park WG, Yeh RW, Triadafilopoulos G. Injection therapies for nonvariceal bleeding disorders of the GI tract. Gastrointest Endosc. 2007;66:343-354. |
| 21. | Chung SC, Lau JY, Rutgeerts P, Fennerty MB. Thermal coagulation for nonvariceal bleeding. Endoscopy. 2002;34:89-92. |
| 22. | Kanai M, Hamada A, Endo Y, Takeda Y, Yamakawa M, Nishikawa H, Torii A. Efficacy of argon plasma coagulation in nonvariceal upper gastrointestinal bleeding. Endoscopy. 2004;36:1085-1088. |
| 23. | Sass DA, Chopra KB. Portal hypertension and variceal hemorrhage. Med Clin North Am. 2009;93:837-853, vii-viii. |
| 24. | Naritaka Y, Shimakawa T, Isohata N, Asaka S, Konno S, Murayama M, Yoshimatsu K, Shiozawa S, Katsube T, Ogawa K. Long-term results of endoscopic injection sclerotherapy in 602 patients with esophageal varices. Hepatogastroenterology. 2008;55:2096-2102. |
| 25. | Bhargava DK, Pokharna R. Endoscopic variceal ligation versus endoscopic variceal ligation and endoscopic sclerotherapy: a prospective randomized study. Am J Gastroenterol. 1997;92:950-953. |
| 26. | Yoshida H, Mamada Y, Taniai N, Tajiri T. New methods for the management of esophageal varices. World J Gastroenterol. 2007;13:1641-1645. |
| 27. | Thalheimer U, Triantos CK, Samonakis DN, Patch D, Burroughs AK. Infection, coagulation, and variceal bleeding in cirrhosis. Gut. 2005;54:556-563. |
| 28. | Rerknimitr R, Chanyaswad J, Kongkam P, Kullavanijaya P. Risk of bacteremia in bleeding and nonbleeding gastric varices after endoscopic injection of cyanoacrylate. Endoscopy. 2008;40:644-649. |
| 29. | Colombato L. The role of transjugular intrahepatic portosystemic shunt (TIPS) in the management of portal hypertension. J Clin Gastroenterol. 2007;41 Suppl 3:S344-S351. |
| 30. | Zheng M, Chen Y, Bai J, Zeng Q, You J, Jin R, Zhou X, Shen H, Zheng Y, Du Z. Transjugular intrahepatic portosystemic shunt versus endoscopic therapy in the secondary prophylaxis of variceal rebleeding in cirrhotic patients: meta-analysis update. J Clin Gastroenterol. 2008;42:507-516. |
| 31. | Orloff MJ, Isenberg JI, Wheeler HO, Haynes KS, Jinich-Brook H, Rapier R, Vaida F, Hye RJ. Randomized trial of emergency endoscopic sclerotherapy versus emergency portacaval shunt for acutely bleeding esophageal varices in cirrhosis. J Am Coll Surg. 2009;209:25-40. |
| 32. | Sarin SK, Lahoti D. Management of gastric varices. Baillieres Clin Gastroenterol. 1992;6:527-548. |
| 33. | Seewald S, Ang TL, Imazu H, Naga M, Omar S, Groth S, Seitz U, Zhong Y, Thonke F, Soehendra N. A standardized injection technique and regimen ensures success and safety of N-butyl-2-cyanoacrylate injection for the treatment of gastric fundal varices (with videos). Gastrointest Endosc. 2008;68:447-454. |
| 34. | Belletrutti PJ, Romagnuolo J, Hilsden RJ, Chen F, Kaplan B, Love J, Beck PL. Endoscopic management of gastric varices: efficacy and outcomes of gluing with N-butyl-2-cyanoacrylate in a North American patient population. Can J Gastroenterol. 2008;22:931-936. |
| 35. | Sugimoto N, Watanabe K, Watanabe K, Ogata S, Shimoda R, Sakata H, Eguchi Y, Mizuta T, Tsunada S, Iwakiri R. Endoscopic hemostasis for bleeding gastric varices treated by combination of variceal ligation and sclerotherapy with N-butyl-2-cyanoacrylate. J Gastroenterol. 2007;42:528-532. |
| 36. | Ninoi T, Nishida N, Kaminou T, Sakai Y, Kitayama T, Hamuro M, Yamada R, Nakamura K, Arakawa T, Inoue Y. Balloon-occluded retrograde transvenous obliteration of gastric varices with gastrorenal shunt: long-term follow-up in 78 patients. AJR Am J Roentgenol. 2005;184:1340-1346. |
| 37. | Hiraga N, Aikata H, Takaki S, Kodama H, Shirakawa H, Imamura M, Kawakami Y, Takahashi S, Toyota N, Ito K. The long-term outcome of patients with bleeding gastric varices after balloon-occluded retrograde transvenous obliteration. J Gastroenterol. 2007;42:663-672. |
| 38. | Lee JH, Han HS, Kim HA, Koo MY. Long-term results of fundectomy and periesophagogastric devascularization in patients with gastric fundal variceal bleeding. World J Surg. 2009;33:2144-2149. |
| 39. | Heldwein W, Schreiner J, Pedrazzoli J, Lehnert P. Is the Forrest classification a useful tool for planning endoscopic therapy of bleeding peptic ulcers? Endoscopy. 1989;21:258-262. |
| 40. | Bleau BL, Gostout CJ, Sherman KE, Shaw MJ, Harford WV, Keate RF, Bracy WP, Fleischer DE. Recurrent bleeding from peptic ulcer associated with adherent clot: a randomized study comparing endoscopic treatment with medical therapy. Gastrointest Endosc. 2002;56:1-6. |
| 41. | Jensen DM, Kovacs TO, Jutabha R, Machicado GA, Gralnek IM, Savides TJ, Smith J, Jensen ME, Alofaituli G, Gornbein J. Randomized trial of medical or endoscopic therapy to prevent recurrent ulcer hemorrhage in patients with adherent clots. Gastroenterology. 2002;123:407-413. |
| 42. | Sung JJ, Chan FK, Lau JY, Yung MY, Leung WK, Wu JC, Ng EK, Chung SC. The effect of endoscopic therapy in patients receiving omeprazole for bleeding ulcers with nonbleeding visible vessels or adherent clots: a randomized comparison. Ann Intern Med. 2003;139:237-243. |
| 43. | Bianco MA, Rotondano G, Marmo R, Piscopo R, Orsini L, Cipolletta L. Combined epinephrine and bipolar probe coagulation vs. bipolar probe coagulation alone for bleeding peptic ulcer: a randomized, controlled trial. Gastrointest Endosc. 2004;60:910-915. |
| 44. | Yuan Y, Wang C, Hunt RH. Endoscopic clipping for acute nonvariceal upper-GI bleeding: a meta-analysis and critical appraisal of randomized controlled trials. Gastrointest Endosc. 2008;68:339-351. |
| 45. | Park CH, Joo YE, Kim HS, Choi SK, Rew JS, Kim SJ. A prospective, randomized trial comparing mechanical methods of hemostasis plus epinephrine injection to epinephrine injection alone for bleeding peptic ulcer. Gastrointest Endosc. 2004;60:173-179. |
| 46. | Calvet X, Vergara M, Brullet E, Gisbert JP, Campo R. Addition of a second endoscopic treatment following epinephrine injection improves outcome in high-risk bleeding ulcers. Gastroenterology. 2004;126:441-450. |
| 47. | Sung JJ, Tsoi KK, Lai LH, Wu JC, Lau JY. Endoscopic clipping versus injection and thermo-coagulation in the treatment of non-variceal upper gastrointestinal bleeding: a meta-analysis. Gut. 2007;56:1364-1373. |
| 48. | Marmo R, Rotondano G, Piscopo R, Bianco MA, D’Angella R, Cipolletta L. Dual therapy versus monotherapy in the endoscopic treatment of high-risk bleeding ulcers: a meta-analysis of controlled trials. Am J Gastroenterol. 2007;102:279-289; quiz 469. |
| 49. | Laine L, McQuaid KR. Endoscopic therapy for bleeding ulcers: an evidence-based approach based on meta-analyses of randomized controlled trials. Clin Gastroenterol Hepatol. 2009;7:33-47; quiz 1-2. |
| 50. | Yamaguchi Y, Yamato T, Katsumi N, Imao Y, Aoki K, Morita Y, Miura M, Morozumi K, Ishida H, Takahashi S. Short-term and long-term benefits of endoscopic hemoclip application for Dieulafoy’s lesion in the upper GI tract. Gastrointest Endosc. 2003;57:653-656. |
| 51. | Iacopini F, Petruzziello L, Marchese M, Larghi A, Spada C, Familiari P, Tringali A, Riccioni ME, Gabbrielli A, Costamagna G. Hemostasis of Dieulafoy’s lesions by argon plasma coagulation (with video). Gastrointest Endosc. 2007;66:20-26. |
| 52. | Marmo R, Rotondano G, Bianco MA, Piscopo R, Prisco A, Cipolletta L. Outcome of endoscopic treatment for peptic ulcer bleeding: Is a second look necessary? A meta-analysis. Gastrointest Endosc. 2003;57:62-67. |
| 53. | Massó González EL, García Rodríguez LA. Proton pump inhibitors reduce the long-term risk of recurrent upper gastrointestinal bleeding: an observational study. Aliment Pharmacol Ther. 2008;28:629-637. |
| 54. | Ford AC, Delaney BC, Forman D, Moayyedi P. Eradication therapy in Helicobacter pylori positive peptic ulcer disease: systematic review and economic analysis. Am J Gastroenterol. 2004;99:1833-1855. |
| 55. | Savides TJ, Jensen DM, Cohen J, Randall GM, Kovacs TO, Pelayo E, Cheng S, Jensen ME, Hsieh HY. Severe upper gastrointestinal tumor bleeding: endoscopic findings, treatment, and outcome. Endoscopy. 1996;28:244-248. |
| 56. | Johanns W, Luis W, Janssen J, Kahl S, Greiner L. Argon plasma coagulation (APC) in gastroenterology: experimental and clinical experiences. Eur J Gastroenterol Hepatol. 1997;9:581-587. |
| 57. | Kawamura H, Inamori M, Akiyama T, Akimoto K, Fujita K, Takahashi H, Yoneda M, Abe Y, Kubota K, Ueno N. Argon plasma coagulation for a bleeding gastrointestinal stromal tumor. Digestion. 2007;75:164. |
| 58. | Huang SP, Wang HP, Lee YC, Lin CC, Yang CS, Wu MS, Lin JT. Endoscopic hemoclip placement and epinephrine injection for Mallory-Weiss syndrome with active bleeding. Gastrointest Endosc. 2002;55:842-846. |
| 59. | Cho YS, Chae HS, Kim HK, Kim JS, Kim BW, Kim SS, Han SW, Choi KY. Endoscopic band ligation and endoscopic hemoclip placement for patients with Mallory-Weiss syndrome and active bleeding. World J Gastroenterol. 2008;14:2080-2084. |
| 60. | Costa ND, Cadiot G, Merle C, Jolly D, Bouche O, Thiéfin G, Zeitoun P. Bleeding reflux esophagitis: a prospective 1-year study in a university hospital. Am J Gastroenterol. 2001;96:47-51. |
| 61. | Kwan V, Bourke MJ, Williams SJ, Gillespie PE, Murray MA, Kaffes AJ, Henriquez MS, Chan RO. Argon plasma coagulation in the management of symptomatic gastrointestinal vascular lesions: experience in 100 consecutive patients with long-term follow-up. Am J Gastroenterol. 2006;101:58-63. |
| 62. | Herrera S, Bordas JM, Llach J, Ginès A, Pellisé M, Fernández-Esparrach G, Mondelo F, Mata A, Cárdenas A, Castells A. The beneficial effects of argon plasma coagulation in the management of different types of gastric vascular ectasia lesions in patients admitted for GI hemorrhage. Gastrointest Endosc. 2008;68:440-446. |
| 63. | Wells CD, Harrison ME, Gurudu SR, Crowell MD, Byrne TJ, Depetris G, Sharma VK. Treatment of gastric antral vascular ectasia (watermelon stomach) with endoscopic band ligation. Gastrointest Endosc. 2008;68:231-236. |
| 64. | Jain R, Chetty R. Gastric hyperplastic polyps: a review. Dig Dis Sci. 2009;54:1839-1846. |
| 65. | Chen YY, Yen HH, Soon MS. Impact of endoscopy in the management of duodenal diverticular bleeding: experience of a single medical center and a review of recent literature. Gastrointest Endosc. 2007;66:831-835. |