Published online Aug 16, 2024. doi: 10.4253/wjge.v16.i8.483
Revised: June 26, 2024
Accepted: July 3, 2024
Published online: August 16, 2024
Processing time: 72 Days and 14.2 Hours
Multisystem inflammatory syndrome in adults (MIS-A) is a rare but severe di
We present a 58-year-old Chinese man diagnosed with MIS-A. His chief comp
Gastrointestinal involvement in MIS-A is not uncommon. Intestinal involvement predominates, and esophageal involvement is rarely reported. Esophageal ulcer with bleeding could also be a manifestation of MIS-A.
Core Tip: Multisystem inflammatory syndrome in adults (MIS-A) is a rare but severe disease occurring several weeks after severe acute respiratory syndrome coronavirus 2 infection. We present a 58-year-old Chinese man diagnosed with MIS-A who had multiple organ damage. The patient had melena and gastroscopy indicated esophageal ulcer and severe esophagitis. His condition improved after prednisone and other supportive treatment. Clinicians should take MIS-A into consideration when they face unexplained inflammation and multiorgan damage. Gastrointestinal involvement in MIS-A is not unco
- Citation: Yang N, Liu Z, Jin T, Xin HW, Gu L, Zheng Y, Zhou HX, Li N, Liu XJ. Esophageal ulcer and multisystem inflammatory syndrome after COVID-19: A case report. World J Gastrointest Endosc 2024; 16(8): 483-488
- URL: https://www.wjgnet.com/1948-5190/full/v16/i8/483.htm
- DOI: https://dx.doi.org/10.4253/wjge.v16.i8.483
Multisystem inflammatory syndrome (MIS) is a rare but severe disease related to COVID-19. It develops in adults and children with inflammation of different organs including the gastrointestinal tract, heart, kidneys, skin and hematopoietic system. When this phenomenon occurs in people aged > 21 years, it is called MIS in adults (MIS-A)[1]. Here, we report a case of MIS-A in a 58-year-old man after the 2022 severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) omicron variant in Beijing, China.
A 58-year-old male patient was admitted to hospital in January 2023, with a chief complaint of fever for 1 day, acco
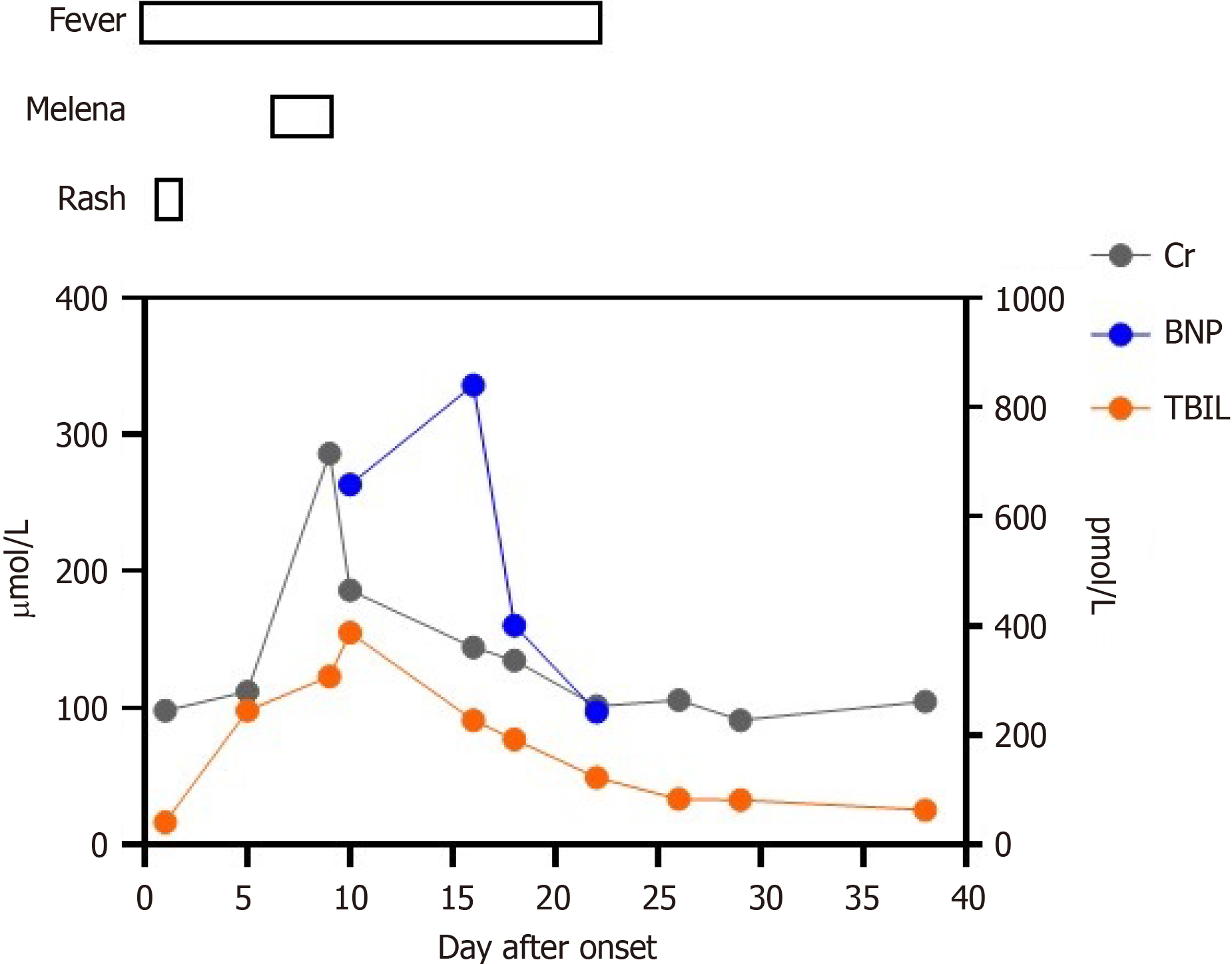
The patient's highest body temperature was 39.6℃. He was first treated with empirical antibiotics of biapenem and supportive treatment. On day 6, melena suddenly occurred and his hemoglobin dropped to 64 g/L. Gastroscopy in
He was diagnosed with SARS-CoV-2 infection by antigen test 5 weeks before, with symptoms of mild upper respiratory tract infection. The antigen test was negative 4 weeks before onset of fever.
The patient had no specific personal history. His uncle was diagnosed with rhabdomyolysis and the cause was unknown.
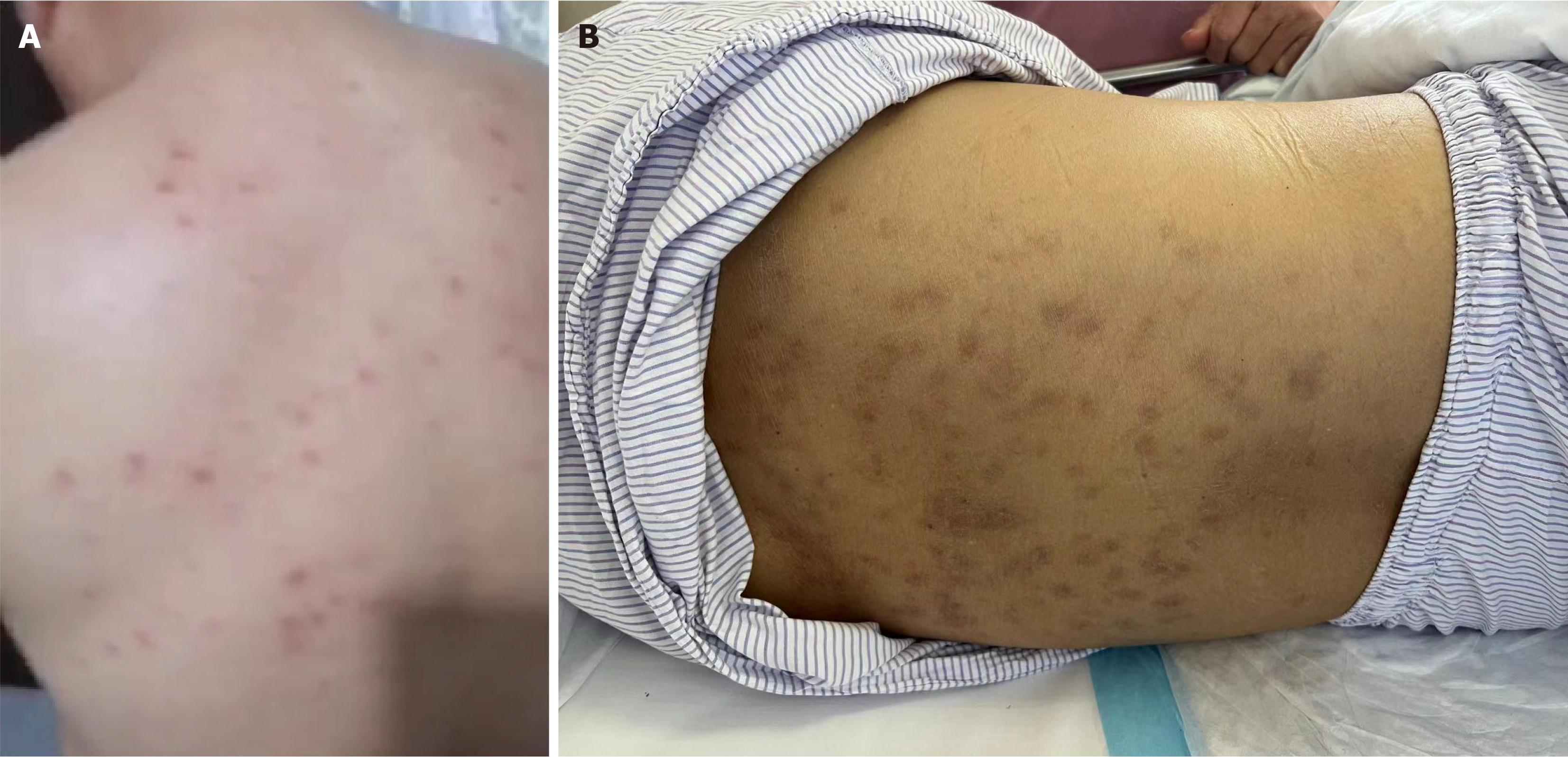
On the first day of hospitalization, the patient had rashes on his back (Figure 3A). He had no palpable lymph node enlargement. Then his skin and sclera were gradually stained yellow. On day 12 of complained symptoms, the rash remained and turned darker (Figure 3B).
The polymerase chain reaction test for SARS-CoV-2 was negative. Immunoglobulin G antibody for SARS-CoV-2 was positive. His laboratory indexes showed abnormal liver function, hypoproteinemia, coagulation disorder, and acute renal insufficiency. On day 16, brain natriuretic peptide increased significantly. Repeated blood culture and sputum culture did not show growth of bacteria or fungi. Epstein–Barr virus DNA in the blood was positive, with low viral load. Blood analysis did not show atypic lymphocytes or elevated lymphocyte count. His autoantibody test and bone marrow examination were normal. No hemophagocytes were seen in the bone marrow.
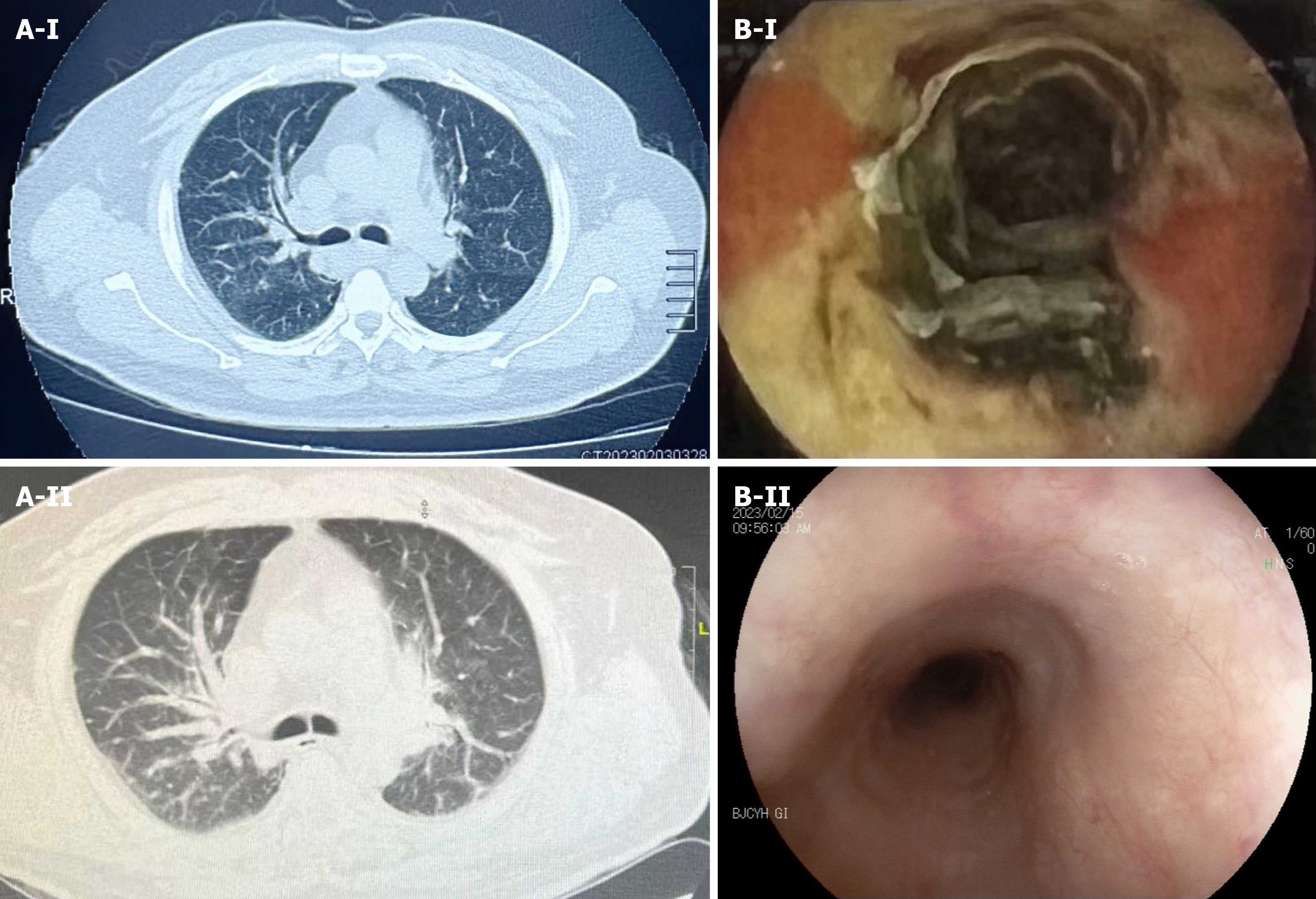
Chest computed tomography (CT) revealed lung inflammation without typical features of viral pneumonia (Figure 1A). His abdominal imaging was normal without hepatosplenomegaly. CT on day 12 revealed pneumonedema (Figure 1A). Echocardiography showed reduced left ventricular systolic and diastolic function, as well as mild pericardial effusion. Venous thrombosis was found in the left lower extremity by ultrasound examination.
MIS-A.
The patient was administered oral glucocorticoid 40 mg/d (approximately 0.5 mg/kg/d).
Ferrit and interleukin-6 were lower than before. A second gastroscopy on day 19 showed that the esophageal ulcer was completely healed (Figure 1B). The patient was discharged on day 32.
It was found that the rate of MIS-A was 9.9% and MIS-A-related mortality was 35.3%[2]. MIS usually occurred about 4 weeks after COVID-19 infection. In a recent systematic review[3], the organ systems most affected by MIS-A were hematological (92%), cardiovascular (87%), gastrointestinal (83%) and respiratory (74%). Our patient had multiple organ damage, including gastrointestinal tract, liver, heart and kidneys, at approximately 5 weeks after SARS-CoV-2 infection onset. Compared with patients with multisystem inflammatory syndrome in children (MIS-C), patients with MIS-A were more likely to have cardiac dysfunction and thrombosis[3,4]. MIS-C patients were more likely to present with dermatological and mucocutaneous manifestations[5].
In another systematic review, 73.4% of MIS-A patients had gastrointestinal symptoms[6]. Two cases of MIS-C undergoing endoscopy have been reported[7,8]. One had severe active gastroduodenitis and patchy colitis, and the other had complicated terminal ileitis, requiring ileocecal resection. Nonaka and colleagues[9] reported a 68-year-old male MIS-A patient whose intestine had extensive erosions from the duodenum to the ileum. The patient underwent arterial embolization and then small intestine resection because of hemorrhage. They also reported a 63-year-old man diagnosed with MIS-A with extensive erosion of the intestinal tract. A German medical team[10] reported a 27-year-old man dia
SARS-CoV-2 is implicated in the mechanism of MIS. The angiotensin-converting enzyme 2 receptor, which is used by SARS-CoV-2 to gain cell entry, is abundant in most organs[11]. The cytokine storm is also a potential driver of symptoms. Multiple cytokines including interleukin (IL)-1β, IL-6, IL-8, IL-10, IL-17, and interferon-γ are elevated in MIS-C patients[12]. MIS is also associated with thrombotic microangiopathy, which is characterized by microangiopathic hemolytic anemia and thrombocytopenia[13]. Future studies should elucidate the multi-factorial pathogenesis of MIS-A in order to identify the markers for treatment and prevention.
Gastrointestinal involvement in MIS-A is not uncommon. Intestinal involvement predominates, and esophageal involvement is rarely reported. We report a case of MIS-A with fever, rash and multiple organ dysfunction accompanied by esophageal ulcer. After glucocorticoid therapy, fever and multiple organ dysfunction were relieved, and the eso
| 1. | Das B, Joshi D, Vineeth VK, Naveen AS, Gopalakrishnan R, Ramasubramanian V, Yamuna Devi VR, Nambi PS. Post-COVID multisystem inflammatory syndrome in adults: a study from a tertiary care hospital in south India. Indian J Med Res. 2022;156:669-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Serin I, Sari ND, Gunaltili M, Karakilic A, Gulesir B, Kal Kolik B, Cevik G, Sungurlu H, Keskin M, Baltik M, Cakmak O, Cinli TA. Enigma of COVID-19: is "multisystem inflammatory syndrome in adults" (MIS-A) predictable? BMC Infect Dis. 2022;22:300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Patel P, DeCuir J, Abrams J, Campbell AP, Godfred-Cato S, Belay ED. Clinical Characteristics of Multisystem Inflammatory Syndrome in Adults: A Systematic Review. JAMA Netw Open. 2021;4:e2126456. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 125] [Cited by in RCA: 139] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 4. | Su Y, Xing H, Shen W, Li M, Xu Y, Li Y. Fatal multisystem inflammatory syndrome in a 78-year-old adult after severe COVID-19 pneumonia during 2022 Omicron variant epidemic in Shanghai, China. J Infect Public Health. 2023;16:418-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 5. | Chow EJ. The Multisystem Inflammatory Syndrome in Adults With SARS-CoV-2 Infection-Another Piece of an Expanding Puzzle. JAMA Netw Open. 2021;4:e2110344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 6. | Kunal S, Ish P, Sakthivel P, Malhotra N, Gupta K. The emerging threat of multisystem inflammatory syndrome in adults (MIS-A) in COVID-19: A systematic review. Heart Lung. 2022;54:7-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 37] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 7. | Sweeny KF, Zhang YJ, Crume B, Martz CA, Blessing MM, Kahn SA. Inflammatory Bowel Disease Presenting With Concurrent COVID-19 Multisystem Inflammatory Syndrome. Pediatrics. 2021;147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | Tong CW, Jiwane A. A complicated case of terminal ileitis post-COVID-19 infection requiring bowel resection. J Surg Case Rep. 2022;2022:rjac457. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 9. | Nonaka T, Bunya N, Nakayama R, Hagiwara S, Uemura S, Harada K, Narimatsu E. Two cases of multisystem inflammatory syndrome in adults after improvement in severe acute respiratory distress syndrome due to coronavirus disease 2019. Acute Med Surg. 2022;9:e737. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 10. | Rieper K, Sturm A. [First Cases of Multisystem Inflammatory Syndrome following SARS-CoV-2 infection in Adults in Germany]. Dtsch Med Wochenschr. 2021;146:598-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Maltezou HC, Pavli A, Tsakris A. Post-COVID Syndrome: An Insight on Its Pathogenesis. Vaccines (Basel). 2021;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 110] [Cited by in RCA: 109] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 12. | Carter MJ, Fish M, Jennings A, Doores KJ, Wellman P, Seow J, Acors S, Graham C, Timms E, Kenny J, Neil S, Malim MH, Tibby SM, Shankar-Hari M. Peripheral immunophenotypes in children with multisystem inflammatory syndrome associated with SARS-CoV-2 infection. Nat Med. 2020;26:1701-1707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 308] [Article Influence: 61.6] [Reference Citation Analysis (0)] |
| 13. | Campbell CM, Kahwash R. Will Complement Inhibition Be the New Target in Treating COVID-19-Related Systemic Thrombosis? Circulation. 2020;141:1739-1741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 205] [Article Influence: 41.0] [Reference Citation Analysis (0)] |