Published online Mar 16, 2023. doi: 10.4253/wjge.v15.i3.191
Peer-review started: December 22, 2022
First decision: January 3, 2023
Revised: January 9, 2023
Accepted: February 8, 2023
Article in press: February 8, 2023
Published online: March 16, 2023
Processing time: 83 Days and 14 Hours
Ectopic pancreatic tissue is a congenital anomaly where a part of pancreatic tissue is located outside of the pancreas and lacks vascular or anatomical commu
We present a case of an 81-year-old patient presenting with anemia, with right colonic neoplasia and carbohydrate antigen 19-9 above the normal values. She underwent laparoscopic right hemicolectomy. The final histology was consistent with a primitive adenocarcinoma with ductal morphology and solid-predominant growth pattern. Benign ectopic pancreatic tissue was absent in the surgical specimen.
The case describes a very rare complete degeneration of a colonic ectopic pan
Core Tip: Ectopic pancreatic tissue is a congenital anomaly. Currently, only two anecdotal cases of malignant transformation of colonic ectopic pancreatic tissue have been described. We present a case of an 81-year-old patient with a primitive adenocarcinoma of the right colon, with ductal morphology and solid-predominant growth pattern. Carbohydrate antigen 19-9 value was above the normal values, and both pancreas and biliary tree were healthy. Benign ectopic pancreatic tissue was missing in the surgical specimen. This observation is suggestive of a complete degeneration of a rare colonic ectopic pancreatic tissue or, even more interesting, the first description of a primitive ductal adenocarcinoma of the colon.
- Citation: Conti CB, Mulinacci G, Tamini N, Jaconi M, Zucchini N. Colonic ductal adenocarcinoma case report: New entity or rare ectopic degeneration? World J Gastrointest Endosc 2023; 15(3): 191-194
- URL: https://www.wjgnet.com/1948-5190/full/v15/i3/191.htm
- DOI: https://dx.doi.org/10.4253/wjge.v15.i3.191
Ectopic pancreatic tissue is a congenital anomaly where a part of pancreatic tissue is located outside of the pancreas and lacks vascular or anatomical communication with it while showing the same histological features: Pancreatic acinar formation, duct development and islets of Langerhans. Ectopic pancreatic tissue is found in 0.2% of laparotomies and 0.5%-14.0% of autopsies. The most common locations are the stomach (25%-40%), duodenum (9%-36%) and proximal jejunum (0.5%-35.0%). The ileum, including ectopic pancreas within Meckel diverticulum, accounts for 2.8% to 7.5% of cases, being the fourth most common site. The colon, appendix, mesentery, esophagus, liver, gallbladder, bile duct, spleen, umbilical cord, retroperitoneal cavity, lung and mediastinum are extremely rare sites[1]. Usually ectopic pancreas is an asymptomatic condition. However, the complications described in the literature are pancreatitis, bleeding, intussusception and malignant degeneration[2,3].
According to the Guillou description, carcinoma arising from ectopic pancreatic tissue is surely diagnosed when tumor cells are found within or close to the ectopic pancreas. A transitional area between pancreatic structures and carcinoma is clearly detected and the benign ectopic pancreatic tissue shows acini and ductal structures[4].
Currently, the literature reports only two anecdotal cases of malignant transformation of colonic ectopic pancreatic tissue: One occurred in the splenic flexure and one in the sigmoid colon[5].
A 81-year-old woman underwent colonoscopy for severe anemia (hemoglobin 6 g/dL) in the absence of overt gastrointestinal bleeding.
She had ongoing anticoagulant therapy due to atrial fibrillation. The liver enzyme test, cholestasis test and two previous abdominal sonography exams were normal. However, of note, blood tests showed carbohydrate antigen 19-9 (CA 19-9) value repeatedly above normal values (2 × upper limit of normal) since 2016.
The medical history of the patient reported a loss of 4 kg in the previous 6 mo, and an invasive lobular carcinoma of the breast occurred 10 years prior to admission.
Family history was unremarkable. The patient did not smoke and did not drink alcohol. She was normal weight before the weight loss occurred due to the neoplasia.
The patient’s vital signs were normal. She was pale due to the anemia and reported fatigue. No abnormal findings were present at the physical examination, apart from the atrial fibrillation.
Liver enzyme and cholestasis tests were normal.
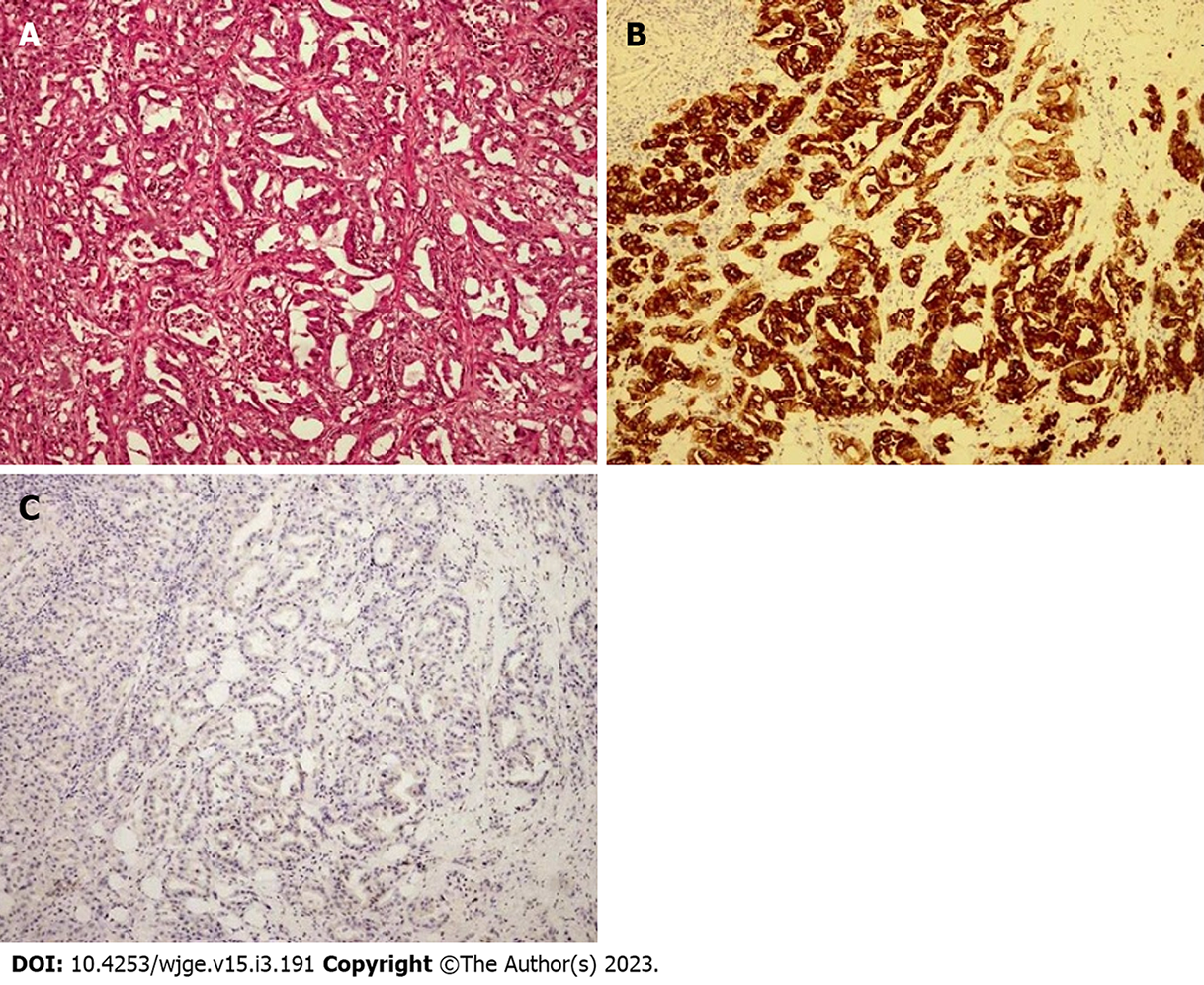
Two previous abdominal sonography exams were normal. Computed tomography scan, performed after the diagnosis of the colonic neoplasia showed local peritoneal infiltration and local lymphadenopathies, in the absence of distant organ metastasis. Colonoscopy revealed a large lesion of 40 mm in size extending from the ileocecal valve fold to the ascending colon. The superficial pattern, the spontaneous bleeding and the ulcerated surface suggested the diagnosis of primitive colonic neoplasia. Biopsies were taken. The terminal ileum results were normal. Surprisingly, the histological diagnosis was consistent with a primitive ductal adenocarcinoma of the colon (Figure 1A). A total body computed tomography scan showed local peritoneal infiltration and local lymphadenopathies, in the absence of distant organ metastasis. Notably, both the pancreas and biliary tree did not report abnormalities. CEA was normal, whereas CA 19-9 value was 3 × upper limit of normal. Cholestasis and liver enzyme tests were again normal.
The final histology of the surgical specimen confirmed the diagnosis of adenocarcinoma with ductal morphology and solid-predominant growth pattern.
After a multidisciplinary discussion, the patient underwent surgical treatment, with laparoscopic right hemicolectomy and ileocolic anastomosis. The final histology of the surgical specimen confirmed the diagnosis of adenocarcinoma with ductal morphology and solid-predominant growth pattern. The immunohistochemistry documented the diffuse positive staining for cytokeratin 7 and the absence of CDX2 immunoreactivity (Figure 1B and C). CK20, GATA3, PAX8, and ER were also negative. The final lymph node involvement occurred in three pericolic lymph nodes out of thirteen.
The outcome was very good, with no complications. The follow-up imaging performed six months after surgery was negative. The patient was very satisfied with the outcome and the curative surgery.
We described a rare case of primitive ductal adenocarcinoma of the right colon. The neoplasia was located in the right colon and included part of the ileocecal valve. Thus, it was mandatory to rule out an ileal origin[1]. The ileum was both macroscopically and microscopically intact. Interestingly, the pathologist did not recognize a benign ectopic pancreatic tissue in the surgical specimen. This observation suggests the complete degeneration of a rare colonic ectopic pancreas or, even more interesting, the first description of a primitive ductal adenocarcinoma of the colon.
In our opinion, it is useful to consider the existence of this entity, although very rare, in the diagnostic workup of patients with clinical suspicion of organic disease and elevated CA 19-9 value.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bal’afif F, Indonesia; Samizadeh B, Iran S-Editor: Chen YL L-Editor: Filipodia P-Editor: Chen YL
| 1. | Cazacu IM, Luzuriaga Chavez AA, Nogueras Gonzalez GM, Saftoiu A, Bhutani MS. Malignant Transformation of Ectopic Pancreas. Dig Dis Sci. 2019;64:655-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 2. | Rezvani M, Menias C, Sandrasegaran K, Olpin JD, Elsayes KM, Shaaban AM. Heterotopic Pancreas: Histopathologic Features, Imaging Findings, and Complications. Radiographics. 2017;37:484-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 109] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 3. | Xiang S, Zhang F, Xu G. Ectopic pancreas in the ileum: An unusual condition and our experience. Medicine (Baltimore). 2019;98:e17691. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Guillou L, Nordback P, Gerber C, Schneider RP. Ductal adenocarcinoma arising in a heterotopic pancreas situated in a hiatal hernia. Arch Pathol Lab Med. 1994;118:568-571. [PubMed] |
| 5. | Gallo G, Mangogna A, Manco G, Caramaschi S, Salviato T. Pancreatic ductal adenocarcinoma in colonic wall: metastatic disease or cancerized pancreatic ectopic tissue? Surg Case Rep. 2020;6:80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |