Published online Oct 16, 2022. doi: 10.4253/wjge.v14.i10.642
Peer-review started: June 3, 2022
First decision: June 27, 2022
Revised: July 29, 2022
Accepted: September 13, 2022
Article in press: September 13, 2022
Published online: October 16, 2022
Processing time: 130 Days and 13.4 Hours
Gastrointestinal (GI) polyposis is a rare condition in GI diseases. To date about 500 cases of Cronkhite-Canada syndrome (CCS) have been reported worldwide.
We report a 60-year-old female patient who presented with dyspepsia, abdominal pain, and weight loss of 1-year duration. Her physical examination showed al
The patient was diagnosed as having CCS.
Core Tip: Cronkhite-Canada syndrome (CCS) is a rare acquired polyposis with unknown aetiology. To date about 500 cases have been reported worldwide. We herein report an Egyptian patient with CCS. Most of CCS cases were reported from Japan, and to our knowledge, our case is the first case reported from Egypt and North Africa. Cases presenting with gastrointestinal (GI) polyposis and marked thickened gastric mucosa and folds represent challenging cases and diagnostic dilemmas. The diagnosis was based on history, physical examination, endoscopic findings, and histology. CCS is typically characterized by GI symptoms, such as diarrhea and skin changes (e.g., alopecia, pigmentation, and nail dystrophy), while endoscopic features include diffuse polyps throughout the entire GIT, except for the esophagus. Pathological types of polyps in CCS mainly include inflammatory, hyperplastic, hamartomatous, and/or adenomatous polyps. CCS can be complicated by many diseases and has a malignant tendency with a high mortality rate. Till now, there has been no uniform standard treatment for CCS.
- Citation: Alzamzamy AE, Aboubakr A, Okasha HH, Abdellatef A, Elkholy S, Wahba M, Alboraie M, Elsayed H, Othman MO. Cronkhite-Canada syndrome: First case report from Egypt and North Africa. World J Gastrointest Endosc 2022; 14(10): 642-647
- URL: https://www.wjgnet.com/1948-5190/full/v14/i10/642.htm
- DOI: https://dx.doi.org/10.4253/wjge.v14.i10.642
Cronkhite-Canada syndrome (CCS) is one of the rarest nonhereditary diseases[1], and its exact aetiology is still unknown[2], with around 500 cases having been described in the literature[3]. Most of CCS cases were reported from Japan, and to our knowledge, our case is the first case reported from Egypt and North Africa.
Patient with CCS usually presents with gastrointestinal (GI) symptoms such as abdominal pain, weight loss, and diarrhea, or with other symptoms such as onychodystrophy, alopecia, hyperpigmentation of the skin, and rarely vitiligo[4]. GI polyposis is the main endoscopic feature in CCS, which is commonly non-neoplastic and rather inflammatory, hyperplastic, hamartomatous, and/or ad
A 60-year-old female patient presented with dyspepsia, abdominal pain, and weight loss of 1-year duration.
The patient denied other GI or anaemic symptoms. She was a non-smoker and did not drink alcohol.
The patient’s past medical history was free apart from prolonged proton-pump inhibitor (PPI) intake.
There was no family history of gastrointestinal polyposis or colorectal malignancy.
The physical examination was unremarkable apart from alopecia (Figure 1A) and onychodystrophy (Figure 1B).
The patient’s laboratory profile was within normal limits including a full complete blood picture (CBC), chemistry, serum albumin, serum calcium, urine analysis, antinuclear antibody (ANA), and IgG-4.
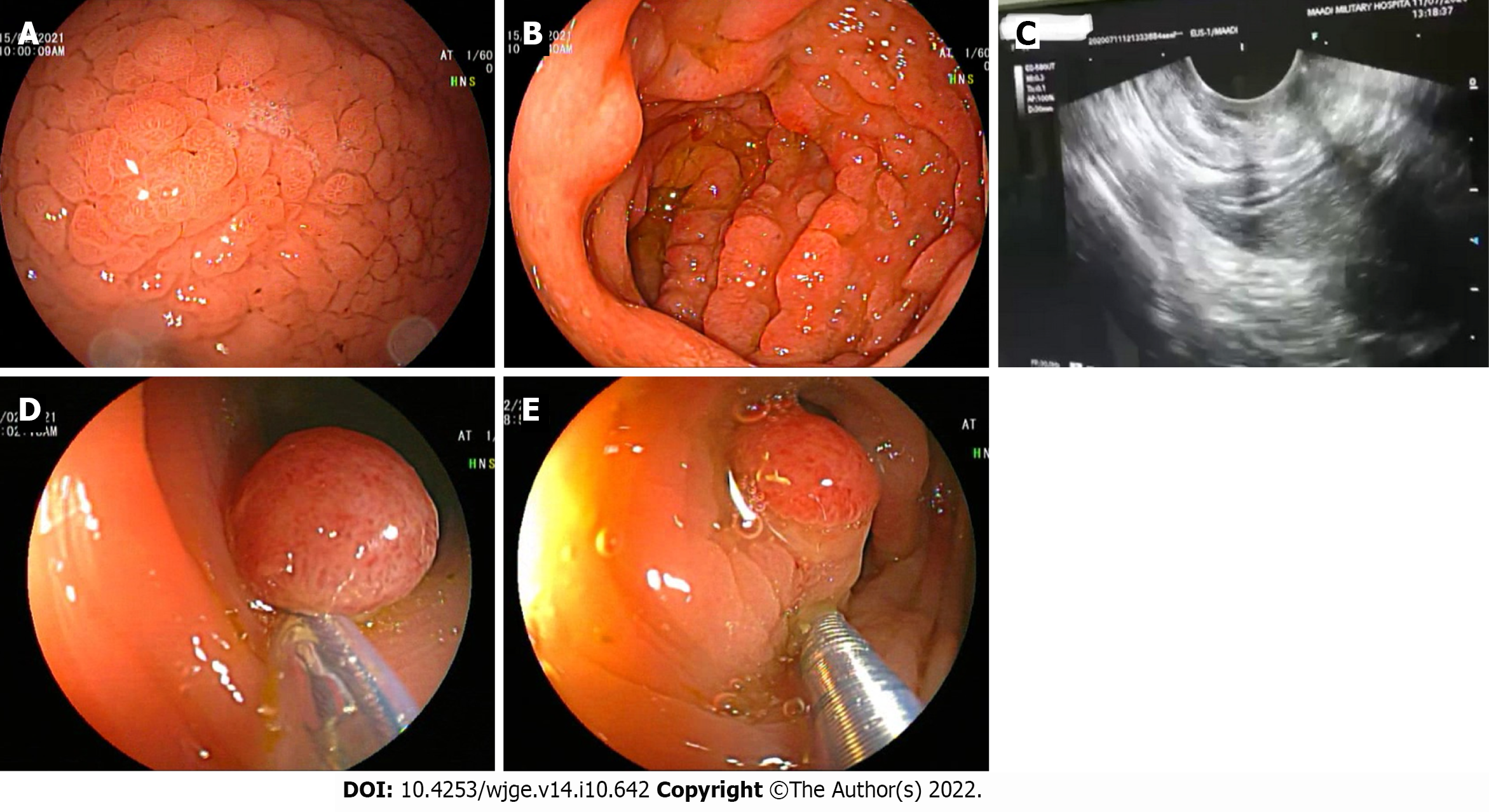
Oesophago-gastro-duodenoscopy (OGD) revealed diffuse markedly thickened gastric mucosa involving the whole stomach (fundus, body, and antrum), with thickened and tortuous gastric rugae, and nu
Endoscopic ultrasound was done later and showed a significantly hypertrophic mucosa and mus
Colonoscopy showed multiple variable-sized, sessile, and pedunculated polyps (~15), scattered at different parts of the colon. Snaring of the large polyps was done after submucosal injection (Figure 2D and E), and histopathological examination showed typical features of benign juvenile-like and hamartomatous polyps without dysplastic changes, while pathology of other polyps revealed tubular adenomatous polyps with low-grade dysplasia.
Both push enteroscopy and terminal ileoscopy showed no polyposis with a normal mucosa in the 3rd and 4th portions of the duodenum, the proximal jejunum, and the terminal ileum.
Computerized tomography (CT) scan of the abdomen & pelvis with oral and intravenous (IV) contrast revealed mild circumferential mural thickening of the gastric wall.
The patient was diagnosed as having CCS.
The patient started a sequential therapy for H. pylori infection with complete eradication, followed by a proton pump inhibitor (40 mg once daily), prednisolone (30 mg/d), and mesalazine (500 mg QID) for 6 mo.
In our case, the following differential diagnoses were raised and discussed with our gastroenterologists: CCS, MD, other polyposis syndromes (such as familiar adenomatous polyposis, Gardner syndrome, juvenile polyposis, Peutz-Jeghers syndrome, and Turcot syndrome), lymphoma, amyloidosis, duodenal gastric heterotopia, and gastric malignancies.
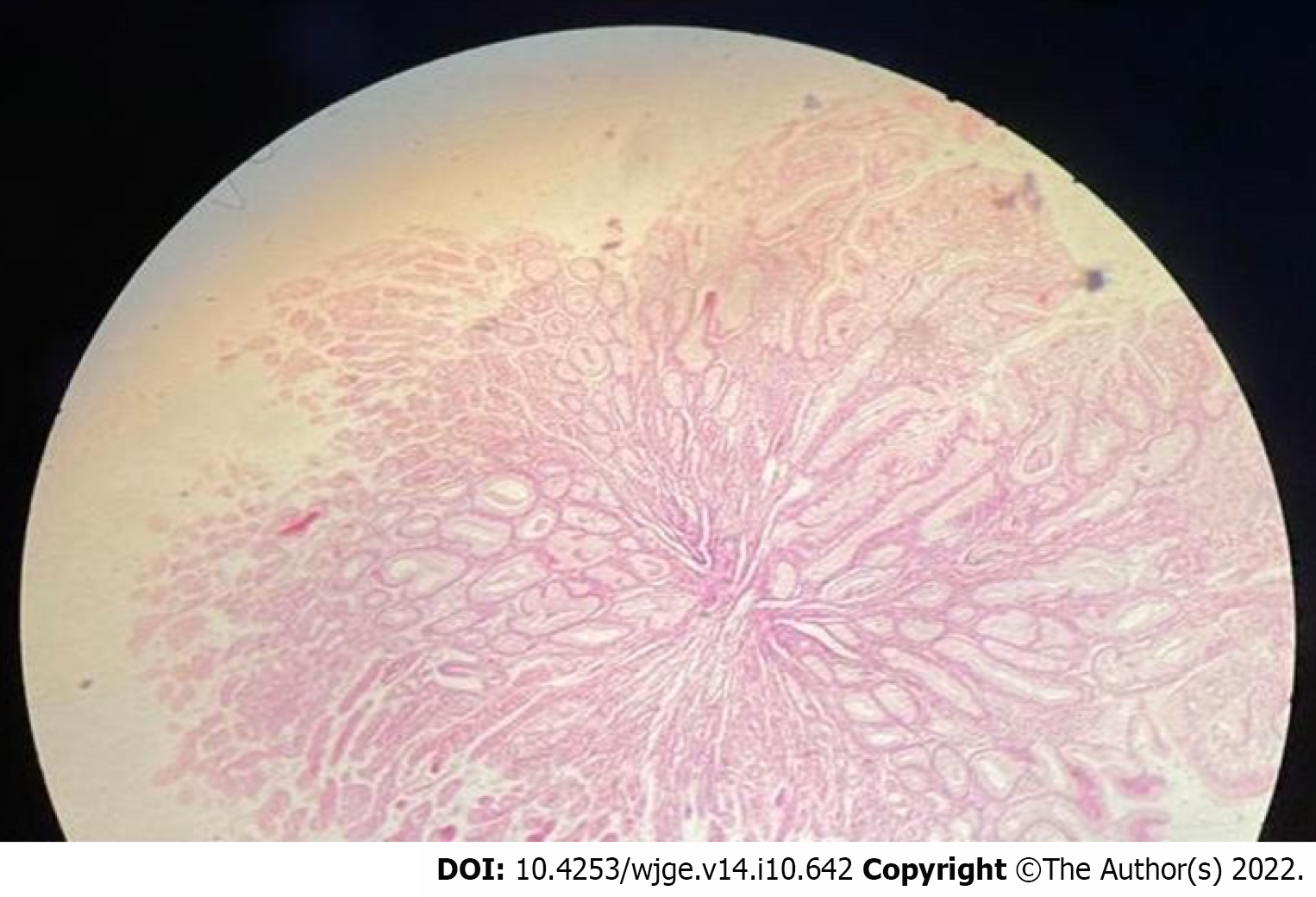
The final diagnosis was based on the medical history, physical examination, endoscopic findings, and the histopathological examination. The presence of anomalies of ectodermal tissues (such as alopecia and nail dystrophy), gastrointestinal polyposis (hamartomatous and adenomatous polyps), markedly thickened gastric mucosa and folds, abdominal pain, weight loss, and marked foveolar gland hyperplasia; all was in favour of the CCS. On the other hand, there was no protein-losing enteropathy, diarrhea, hypoalbuminaemia, or skin pigmentation.
Lymphoma was excluded due to sparing of the muscularis propria. Furthermore, markedly thickened gastric mucosa and folds and the histopathological examination which revealed marked foveolar gland hyperplasia were consistent with MD. In addition, abdominal pain and weight loss are common presentation of MD, but the presence of colonic polyps, and antral and duodenal infiltration, and the absence of hypoproteinaemia decreased the possibility for MD.
The patient started a sequential therapy for H. pylori infection with complete eradication, followed by a proton pump inhibitor (40 mg once daily), prednisolone (30 mg/d), and mesalazine (500 mg QID) for 6 mo.
Common complications of CCS include anemia, intussusception, rectal prolapse, and GI bleeding, as well as other less common ones such as recurrent severe acute pancreatitis, myelodysplastic syndrome, cecal intussusception, portal thrombosis, membranous glomerulonephritis, and osteoporotic fractures that may result from malabsorption of calcium or prolonged glucocorticoid therapy or both. The most serious complication is malignancy; however, the incidence of CCS-related cancer is estimated to be 5%-25%, especially gastric and colon cancer[6].
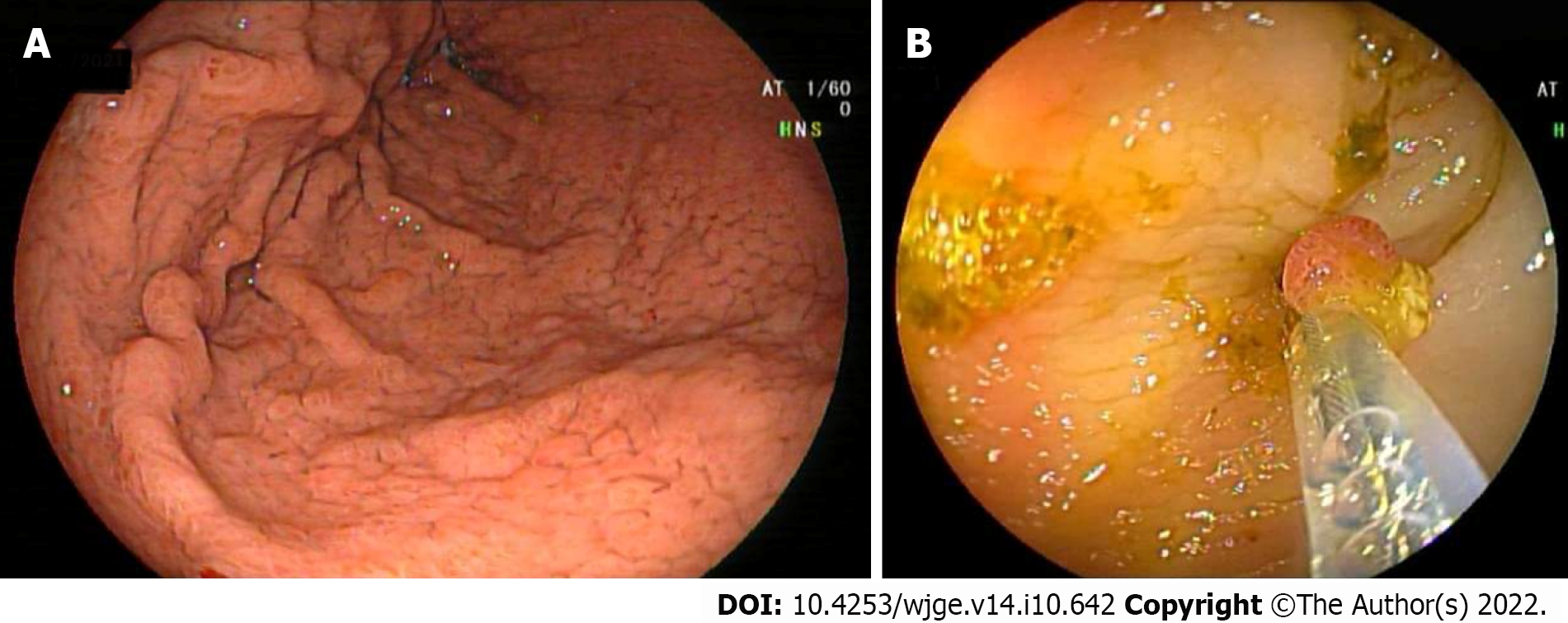
The follow-up endoscopies (OGD and colonoscopy) after 6 and 12 mo of treatment showed significant remission with a reduced number of gastric and colonic polyps and regression of hypertrophic gastric folds (Figure 4). Consequently, the patient's clinical condition was markedly improved, and the prednisolone dose was reduced gradually to 7.5 mg/d, but the mesalazine dose remained the same.
There is a tendency of malignant transformation or coexistence of gastrointestinal malignancies in patients with CCS. Therefore, endoscopic documentation of regression in CCS is important despite the lower incidence of CCS-related cancer in remission patients. Therefore, the comprehensive endoscopic annual surveillance either via chromoendoscopy or directed biopsy from irregular polyps, to exclude pre-cancer lesions before development of invasive carcinoma is mandatory; however, there are still no recommended guidelines to be followed[7].
Nutritional support, electrolytes, and mineral and vitamin supplementation remain the cornerstone in treatment of CCS beside antibiotics and corticosteroids; however, the definitive treatment is still unknown[4,7].
Till now, there is still much that needs to know about this syndrome. In this context, the most important issue is to maintain treatment monitoring and provide appropriate measure to prevent relapse[8].
CCS is a form of uncommon, acquired polyposis with obscure aetiology. To date around 500 cases have been reported all over the world. Most of CCS cases were reported from Japan, and to our knowledge, our case is the first case reported from Egypt and North Africa. CCS is generally characterized by GI symptoms, such as diarrhea and skin changes (e.g., alopecia, skin pigmentation, and onychodystrophy), while GI polyposis is the main endoscopic feature in CCS, which is commonly non-neoplastic and mainly include inflammatory, hyperplastic, hamartomatous, and/or adenomatous polyps. CCS has a malignant potential, and some cases may develop gastric and colorectal malignancies during the disease course. Till now, there is no uniform standard treatment for CCS.
We would like to acknowledge our hospitals and their workers, nurses, and staff members for all the support and help in this study and throughout our careers.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American Society for Gastrointestinal Endoscopy.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Egypt
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Li J, China; Murata K, Japan S-Editor: Chen YL L-Editor: Wang TQ P-Editor: Chen YL
| 1. | Yuan W, Tian L, Ai FY, Liu SJ, Shen SR, Wang XY, Liu F. Cronkhite-Canada syndrome: A case report. Oncol Lett. 2018;15:8447-8453. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Schulte S, Kütting F, Mertens J, Kaufmann T, Drebber U, Nierhoff D, Töx U, Steffen HM. Case report of patient with a Cronkhite-Canada syndrome: sustained remission after treatment with corticosteroids and mesalazine. BMC Gastroenterol. 2019;19:36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Wu ZY, Sang LX, Chang B. Cronkhite-Canada syndrome: from clinical features to treatment. Gastroenterol Rep (Oxf). 2020;8:333-342. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 4. | Kopáčová M, Urban O, Cyrany J, Laco J, Bureš J, Rejchrt S, Bártová J, Tachecí I. Cronkhite-Canada syndrome: review of the literature. Gastroenterol Res Pract. 2013;2013:856873. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Asokkumar R, Mesenas S, Soetikno R. Endoscopic features of Cronkhite-Canada syndrome. Endoscopy. 2021;53:E411-E412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Haghighi S, Noorali S, Mohammad Alizadeh AH. Cronkhite-Canada Syndrome Associated with Metastatic Colon Cancer. Case Rep Gastroenterol. 2018;12:109-115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Liu Y, Zhang L, Yang Y, Peng T. Cronkhite-Canada syndrome: report of a rare case and review of the literature. J Int Med Res. 2020;48:300060520922427. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Dharmik P, Mani TM. A case with rare manifestation of Cronkhite-Canada Syndrome with remission after treatment and literature review. Glob J Medical Clin Case Rep. 2018;5:025-029. [DOI] [Full Text] |