Published online Sep 16, 2021. doi: 10.4253/wjge.v13.i9.407
Peer-review started: April 19, 2021
First decision: June 13, 2021
Revised: June 23, 2021
Accepted: August 12, 2021
Article in press: August 12, 2021
Published online: September 16, 2021
Processing time: 143 Days and 22.3 Hours
Ulcerative colitis (UC) is characterised by mucosal inflammation from the rectum to its proximal area in a symmetric and continuous fashion. However, although uncommon, we encounter cases of UC with rectal sparing in the initial stage.
To evaluate the clinical characteristics and clinical course for rectal sparing UC compared with typical UC.
We looked at records from 2004 to 2015, and selected patients who were newly diagnosed with UC, and who could be followed up for at least 5 years in our hospital. We then retrospectively analysed the medical records and endoscopic findings of those patients. To compare the clinical course and prognosis, we matched each patient with rectal sparing UC 1:3 with controls by age, sex, and disease extent.
Of 619 UC patients, 24 (3.9%) showed rectal sparing at diagnosis. During the follow-up period (median 8 years), in two (8.3%) of the 24 patients, rectal sparing remained through follow-up inspections; but for the other 22 (91.7%) patients, obvious rectal inflammation was found at follow-up endoscopy. Of the 24 patients, 8 (33.3%) were initially misdiagnosed with infectious colitis. No diagnosis was changed to Crohn’s disease. The uses of corticosteroid or biologic agents, hospitalisation rate, and colectomy rates were not different between the rectal sparing UC group and typical UC group.
Some patients with UC can reveal atypical patterns of disease distribution, such as rectal sparing in its initial stage; but despite this, the clinical course and prognosis may not differ from those of typical UC patients.
Core Tip: Ulcerative colitis (UC) is characterised by mucosal inflammation from the rectum to its proximal area in a symmetric and continuous fashion. However, the atypical distribution of UC, such as skip inflammation or rectal sparing can be encountered at initial stage, making diagnosis difficult in usual practice although it is uncommon. As a matter of fact, some studies concerning pediatric UC patients were reported, but its clinical significance and incidence is not known well in adult UC patients. Our study is the only study that evaluated the clinical characteristics and prognosis of adult rectal sparing-typed UC compared with typical UC.
- Citation: Choi YS, Kim JK, Kim WJ. Clinical characteristics and prognosis of patients with ulcerative colitis that shows rectal sparing at initial diagnosis. World J Gastrointest Endosc 2021; 13(9): 407-415
- URL: https://www.wjgnet.com/1948-5190/full/v13/i9/407.htm
- DOI: https://dx.doi.org/10.4253/wjge.v13.i9.407
Ulcerative colitis (UC) is an idiopathic inflammatory bowel disease that is characterised by mucosal inflammation in a continuous and symmetrical fashion from rectum to colon. Recently, however, together with the easy availability and technical advance of colonoscopy, some reports have demonstrated atypical disease distribution of UC, such as skipped lesion, rectal sparing, and upper gastrointestinal tract involvement of ulcerative colitis[1-6]. Moreover, early and increasing diagnosis of UC may also raise the possibility of this diagnostic perplexity, and make it more difficult to differentiate UC from other colitis that can show similar endoscopic findings, such as infectious colitis (i.e., bacterial, amoebic, tuberculous, etc.), ischemic colitis, radiation-induced colitis, drug-induced colitis, eosinophilic colitis, lymphoma, and solitary rectal ulcer syndrome[7].
Atypical distribution of UC, such as rectal sparing, can be encountered in patients with UC during treatment, when the mucosal healing of ulcerative proctitis is achieved by topical treatment with mesalamine or corticorsteroids[8]. This condition can also be found more frequently in paediatric UC patients[9-11]. Nevertheless, although uncommon, it can be noted even in adult patients, even at the initial UC diagnosis. In fact, challenging cases of UC with rectal sparing can be encountered at initial diagnosis, which may lead to misdiagnosis.
The clinical characteristics and significance of rectal sparing UC are not known well. Some previous reports have suggested that rectal sparing UC was associated with primary sclerosing cholangitis[12,13]. However, the clinical study concerning its clinical courses and prognosis is still insufficient, although some Japanese studies reported that rectal sparing type UC was related to poor prognosis[14,15]. The aim of the present study was to evaluate the clinical characteristics and clinical course for rectal sparing UC, compared to typical UC.
We looked at the records of 905 patients [median age: 39 years; range: (16-81) years] who were newly diagnosed with UC at Daehang Hospital, Seoul, Korea, from January 2004 to December 2015; all UC patients were initially diagnosed and regularly followed for at least 5 years in our clinic.
We then retrospectively investigated a number of baseline patient demographics, which included sex and age, time of diagnosis, symptom duration, perinuclear antineutrophil cytoplasmic antibody status, white cell count, erythrocyte sedimentation rate, C-reactive protein levels, initial disease extent, endoscopic findings (new development of rectal inflammation on follow-up endoscopy as well as initial findings), clinical courses including hospitalisation or colectomy, and medication history.
To compare the clinical course and prognosis, we matched each patient with rectal sparing UC (n = 24) 1:3 with controls who had typical continuous and symmetric pattern of UC without rectal sparing (n = 72) to reduce bias; we matched the controls with the cases by age, gender, and disease extent. Primary study outcomes were the cumulative use of corticosteroid. Secondary outcomes were the use of biologic agents (including infliximab, adalimumab, golimumab, vedolizumab, or tofacitinib), hospitalisation of patients, and colectomy in patients with UC with and without rectal sparing at diagnosis. We collected and retrospectively analysed all data through December 31, 2015, or until loss to follow-up. The UC patients who were not on follow-up for less than 5 years were excluded from the analysis. The study was approved by the ethics committee of Daehang Hospital.
UC was definitively diagnosed in those who met the following criteria: (1) Typical history of diarrhea, blood and pus in the stool, or both, for longer than four weeks; (2) Typical sigmoidoscopic or colonoscopic picture with loss of vascularity, friability, granularity, and/or ulcerations of the colorectal mucosa in a continuous and circumferential pattern in the rectum; and (3) Characteristic histopathologic signs of inflammation on biopsy, such as chronic inflammation or distortion of crypt architecture, inflammation of crypts, crypt abscesses, increased chronic inflammatory cells in the lamina propria, erosions, and/or ulcers[16]. Proctitis was categorised when disease extent was limited to the rectum (E1), left-sided colitis when disease extent was limited to the proportion of the colon distal to the splenic flexure (E2), and extensive disease when the disease extended proximal to the splenic flexure, including pancolitis (E3)[17,18]. In the case of UC with rectal sparing, left-sided colitis (E2) and pancolitis (E3) were defined as the same without rectal involvement. We defined rectal sparing as no evidence of mucosal inflammation of the rectal mucosa by colonoscopy, such as normal transparent mucosa with visible capillary vasculature. Endoscopic findings were reviewed by two experienced endoscopists in random order (Kim JK and Choi YS).
We used the χ2 test to compare the categorical variables, and the independent t test to compare the continuous variables. We calculated the cumulative rates of corticosteroids use using the Kaplan-Meier method, and we used the log-rank test to compare the categorical variables. We considered P < 0.05 to be statistically significant, and conducted all calculations using SPSS version 15.0 statistical software package (SPSS Inc., Chicago, IL, United States).
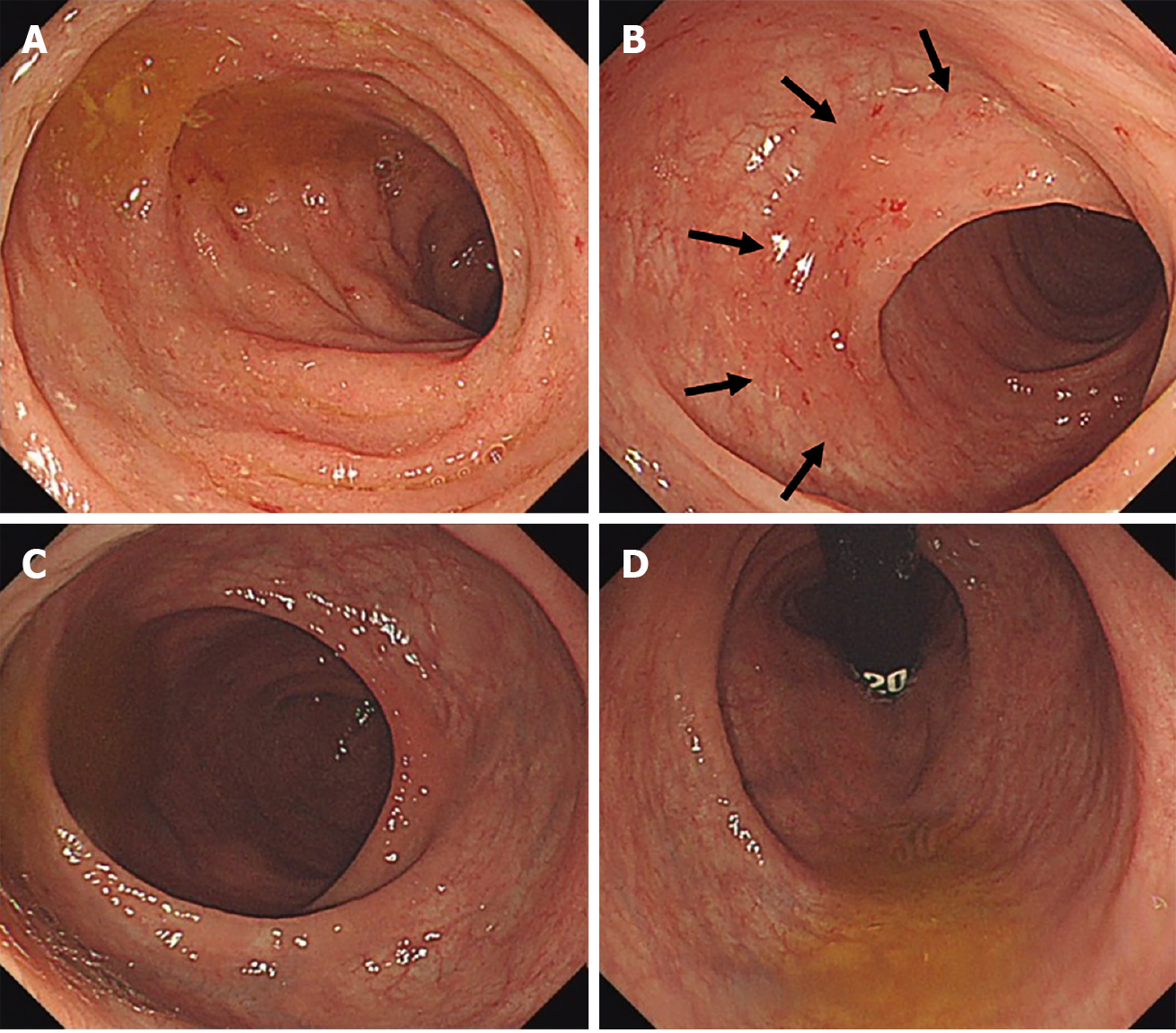
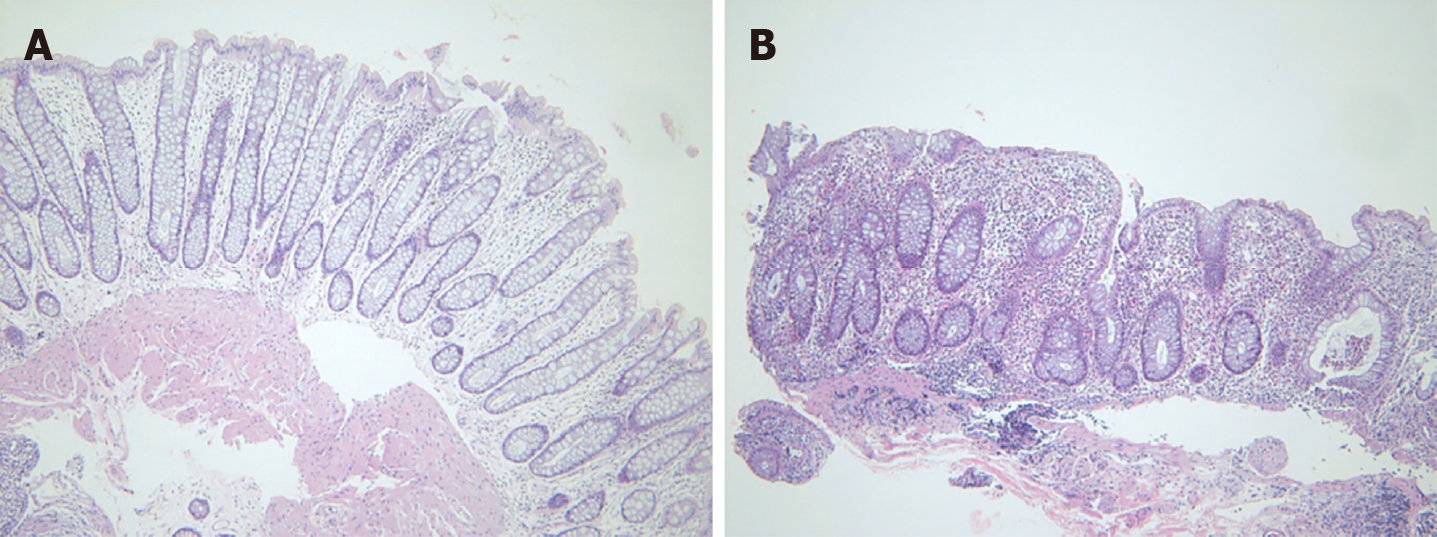
Of 619 UC patients, 24 (3.9%) showed rectal sparing by colonoscopy at initial diagnosis (Figures 1 and 2). Of the 24 patients, 16 (66.7%) had a disease extent beyond splenic flexure (E3), while 8 (33.3%) of the 24 patients were limited before splenic flexure (E2) with rectal sparing. During the follow-up period [median 9 years, range (5-15) years], in two (8.3%) of the 24 patients, rectal sparing remained through follow-up inspections; but for the other 22 (91.7%) patients, obvious rectal inflammation was found at follow-up endoscopy. Of the 24 patients, 8 (33.3%) were initially misdiagnosed with infectious colitis, and empirical antibiotics were administered. No diagnosis was changed from ulcerative colitis to Crohn’s disease (Table 1).
| Rectal spring UC at diagnosis (n = 24) | |
| Age (yr) | 35.8 ± 11.0 |
| Sex (male:female) | 19:5 |
| Disease distribution | |
| Extensive colitis (E3) with rectal sparing | 16 (66.7%) |
| Left-sided colon (E2) with rectal sparing | 8 (33.3%) |
| Initial Diagnosis | |
| IBD-U | 8 (33.3%) |
| Infectious colitis | 7 (29.2%) |
| UC | 7 (29.2%) |
| Nonspecific | 2 (8.3%) |
| Symptom duration | 2 mo (2 wk to 60 mo) |
| Laboratory findings | |
| WBC (count/mm3) | 6475.9 ± 2273.4 |
| ESR (mm/h) | 17.4 ± 13.9 |
| CRP (mg/dL) | 0.4 ± 0.7 |
| p-ANCA positive | 4 (16.7%) |
| Follow-up endoscopy (follow-up period median 9 yr, 5-15 yr) | |
| Persistence of rectal sparing | 2 (8.3%) |
| Appearance of proctitis | 22 (91.7%) |
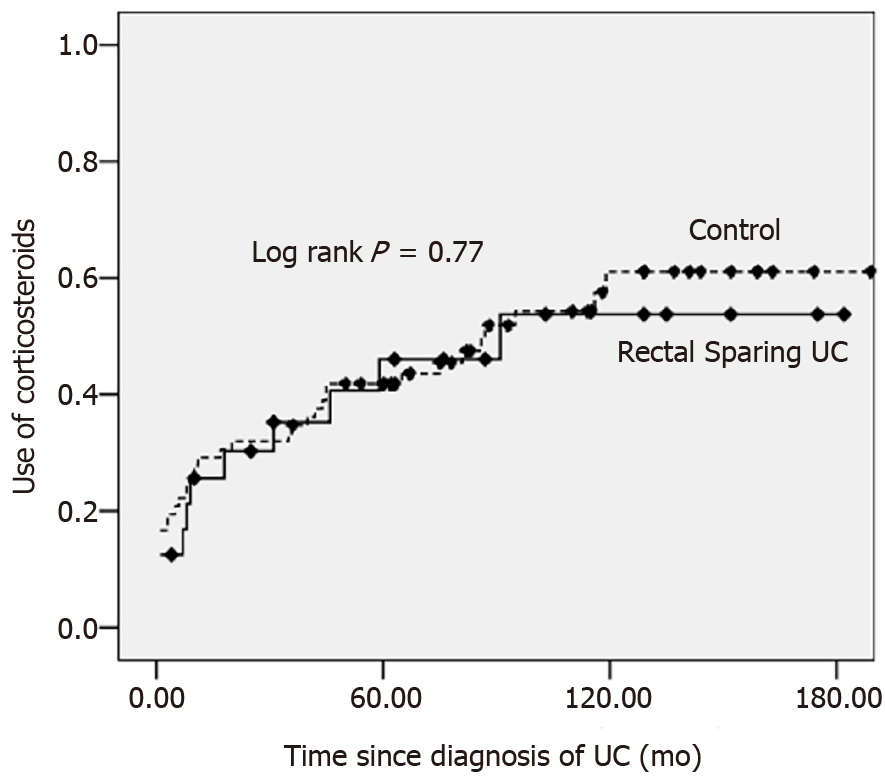
During the follow-up period [median: 115 mo; range: (60-194) mo], in the UC with rectal sparing group, 11 of 24 patients (45.8%) were treated with systemic corticosteroid therapy; in the control group, 38 of 72 patients (52.8%) were treated with systemic corticosteroid. The median time to use corticosteroids were 91 mo in rectal sparing group and 87 mo in control group, respectively. The cumulative rates of ever use of corticosteroid in rectal sparing group and in the control were 35.3%, 46.0% and 53.8% vs 34.7%, 41.8% and 61.1% at 3, 5 and 10 years, respectively (log rank: P = 0.77) (Figure 3).
In the UC with rectal sparing group, 4 patients (16.7%) were treated with biologic agents; in the control group, 10 patients (13.9%) with biologic agent, which did not significantly differ (Table 2). In the UC with rectal sparing group, 4 patients (16.7%) received hospital treatment, and 2 patients (8.3%) underwent total colectomy at maximal follow-up; in the control group, 16 patients (22.2%) were hospitalised, and 2 patients were colectomised, which also did not significantly differ (Table 3).
| No. | Age at diagnosis | Sex | Initial endoscopic finding | No. of systemic steroid use | Indication for biologics | History of biologics | Colectomy |
| 1 | 21 | F | RS | 4 | Steroid dependent | infliximab | - |
| 2 | 30 | F | RS | 2 | Steroid refractory | Infliximab (failed) | + |
| 3 | 31 | F | RS | 9 | Steroid dependent | golimumab | - |
| 4 | 35 | M | RS | 2 | Steroid refractory | Infliximab (failed) | + |
| 5 | 15 | F | RI | 3 | Steroid refractory | golimumab | |
| 6 | 22 | F | RI | 1 | Steroid refractory | Infliximab (failed) | + |
| 7 | 20 | F | RI | 7 | Steroid dependent | golimumab topacitinib | - |
| 8 | 33 | M | RI | 4 | Steroid refractory | infliximab | - |
| 9 | 34 | M | RI | 2 | Steroid refractory | Infliximab (failed) | + |
| 10 | 35 | M | RI | 4 | Steroid refractory | golimumab | - |
| 11 | 39 | M | RI | 3 | Steroid refractory | golimumab | - |
| 12 | 41 | F | RI | 4 | Steroid dependent | golimumab | - |
| 13 | 44 | M | RI | 5 | Steroid refractory | golimumab | - |
| 14 | 48 | M | RI | 2 | Steroid refractory | golimumab | - |
| Rectal sparing UC (n = 24) | Control (n = 72) | P value | |||
| Age | 35.8 ± 11.0 | 36.6 ± 10.6 | Matched | ||
| Sex (male:female) | 19:5 | 57:15 | Matched | ||
| Disease extent (E2/E3) | 8/16 | 24/48 | Matched | ||
| Follow-up period (mo) | 103.4 ± 41.3 | 109.4 ± 41.6 | 0.5 | ||
| Clinical outcomes | |||||
| Use of systemic corticosteroid | 0.77 | ||||
| 3-yr cumulative rate | 35.3% | 34.7% | |||
| 5-yr cumulative rate | 46.0% | 41.8% | |||
| 10-yr cumulative rate | 53.8% | 61.1% | |||
| Use of biologics | 4 (16.7%) | 10 (13.9%) | 0.74 | ||
| Hospitalization | 4 (16.7%) | 16 (22.2%) | 0.77 | ||
| Colectomy | 2 (8.3%) | 2 (2.8%) | 0.26 | ||
Although “rectal involvement” and “continuous and symmetric fashion” are known well as typical colonoscopic findings of ulcerative colitis, rectal sparing or non-continuous distribution of mucosal inflammation can be found by colonoscopy in usual practice. For example, it is common in patients with UC who receive local therapy, such as suppository, enema, or foam type of mesalamine, or corticosteroid enema. However, unfortunately, if it is at the moment of initial diagnosis, it is a challenge to an endoscopist, although clinical or pathologic correlation is necessary for the definitive diagnosis of UC. In any event, is it possible to encounter rectal sparing in a newly diagnosed UC patient? If so, how often? Is the prognosis of this case different from a typical one?
To the best of our knowledge, our study is the only study that evaluated the clinical prognosis of adult UC patients who showed rectal sparing at the stage of initial diagnosis. In fact, the studies analysing the incidence of rectal sparing UC are very rare, because initial endoscopic data can be modified by prior treatment in tertiary or referred hospital, and differential diagnostic methods from infectious colitis, such as culture, serologic test, or PCR, have limitations in primary practice. In one Korean data, eight (3.3%) of the 240 patients had rectal sparing at initial colonoscopy[3]. They suggested that the atypically-distributed UC, including rectal sparing UC, seemed to be uncorrelated with poor prognosis, in terms of rates of remission, relapse, disease extension, colectomy, and mortality. However, the prognosis of rectal sparing UC is still debatable, because in the previous study, the number of patients with rectal sparing was too small (n = 8), and follow-up data was insufficient, because of relatively short follow-up period [median 69 mo, range (2 to 238) mo].
In contrast to prior clinical studies suggesting the unfavourable prognosis of UC with rectal sparing, our result concluded that clinical course and prognosis were not different from those of typical UC patients. Oshitani et al[14] suggest that rectal sparing may be associated with intractability or a tendency to relapse; but that data included the patients with relapsing type of UC, which means that study demon
In contrast to adult UC, paediatric UC patients seem to have different clinical patterns. Rajwal et al[19] reported that rectal sparing was more frequent, and found in 23% of children with newly diagnosed and untreated UC; and that the presence of rectal sparing may be related to less responsiveness to conventional medical treatment. Glickman et al[11] reported that the endoscopic rectal sparing was found in 9% (6 of 73) and pathologic rectal sparing in 30% (absolute 3% vs relative 27%) of paediatric patients with newly diagnosed UC. Interestingly, according to their result, in the adult control group (n = 38), no patient showed endoscopic rectal sparing, but one patient revealed pathologic relative rectal sparing.
Already in the 1980s, one report demonstrated 12 cases of rectal sparing UC, in which double-contrast barium enema showed an apparently normal rectum but an abnormal colon; but in all cases, the author reported that rectal biopsy showed changes compatible with ulcerative colitis[20]. Although the study subjects were different from ours, because those cases included the patients after and during medical treatment, their study suggested that rectal sparing of UC had been challenging diagnostically. As early detection of ulcerative colitis is possible thanks to the easy availability of colonoscopy and advanced imaging techniques, we can hypothesise that atypical pattern of colonoscopic findings in a patient with ulcerative colitis can be observed more frequently. In fact, in our data, most of the UC patients with rectal sparing showed rectal lesion during the follow-up examination, which means that the atypical distribution of mucosal inflammation may be found temporarily at an early stage. In one of our cases (Figure 2), a biopsy obtained at rectal sparing area demonstrated normal pathologic finding, although it is not certain whether normal-looking mucosa by colonoscopy is really pathologically intact, because pathologic evaluation at skipped lesion was not performed in all cases.
We should think outside the box, and reconsider the stereotype of ulcerative colitis, such as rectal involvement with continuity, and symmetricity in colonoscopy. In the present study, a third of patients were initially diagnosed with infectious colitis, because the results of stool and pathologic examination were nonspecific, and so proper management was delayed. However, there was no case of diagnostic change to Crohn’s disease in our data. In two of 24 cases, rectal sparing has persisted for more than 10 years; one 30-year-old male has mucosal inflammation on cecum and ascending colon, while a 46-year-old female showed mucosal inflammation on ascending, transverse, and descending colon in a homogenous, symmetric, and continuous fashion. In cases like this, definitive diagnosis of ulcerative colitis is still not easy. Both are being kept stable on mesalamine therapy during the follow-up period.
There are some limitations to this study. First, the definition of rectal sparing was ambiguous. For example, in this study, it is based only on endoscopical findings, and additional pathologic correlation was insufficient. However, at initial diagnosis, biopsies tend to be obtained only at grossly inflamed mucosa, because the extent of UC is generally classified according to endoscopic features, rather than histologic features. To define the rectal sparing more with more confidence, prospective designed study is needed. Second, the number of patients with rectal sparing UC was relatively small, so survival analysis in comparison with the control group was impossible. Long-term survival analysis is required to draw a more reliable conclusion. To minimise this limitation inevitably caused by retrospective analysis, we included the patients who could be followed up for more than five years [medium follow-up period was 115 mo; range (60 to 194) mo], and matched each UC patient with rectal sparing with controls.
In conclusion, adult patients with UC can reveal atypical patterns of disease distribution, such as rectal sparing; and the incidence at initial diagnosis was rare, but existed in 3.9%. The clinical course and prognosis that we can assume through the need for advanced treatment, hospitalisation, and colectomy did not differ from that of typical UC patients. We trust that this information can be useful in making an accurate diagnosis, and understanding the various disease phenotypes of UC.
In practice, atypical pattern of ulcerative colitis (UC) such as rectal sparing UC is a challenge to endoscopist in timely diagnosis of UC, therefore we retrospectively reviewed the data of our clinic to study the clinical feature of these atypical pattern of UC, and their prognosis as well.
As early diagnosis and progression of diagnostic tools such as endoscopic, imaging techniques become possible, the detection of atypical pattern of inflammatory bowel disease seems to be possible. If we clarify the clinical characteristics, it will be helpful to understand the pathophysiology of inflammatory bowel disease.
The main object of this study is to predict the clinical course of these atypical pattern of UC. There are very rare report concerning this subject. A few reports demonstrated the poorer prognosis, but our experiences were out of accord.
As atypical pattern of UC is very rare and difficult to define in the early stage of UC, prospectively-designed study seems to be impossible, therefore, we (three different inflammatory bowel disease experts) inevitably analyzed the chart, pathologic report and mainly endoscopic images, and reached agreement.
Some reports suggested that the atypical pattern of UC may have a poor clinical outcome such as higher rate of colectomy, but we demonstrated the different results because the patient selection was not similar to the previous studies. Advanced treatment, hopitalization and colectomy rates did not different between rectal sparing UC and typical UC patients.
According to a few previous reports, the prognosis of UC showing atypical pattern is debatable. Our data propose that various form of UC phenotype can be possible and their prognosis seems to be similar to the typical one. Further study is needed to predict the prognosis of UC.
In the future, further prospective studies to clarify the pathophysicology as well as prognosis of other various atypical patterns of UC is warranted.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zhang H S-Editor: Yan JP L-Editor: A P-Editor: Guo X
| 1. | Mutinga ML, Odze RD, Wang HH, Hornick JL, Farraye FA. The clinical significance of right-sided colonic inflammation in patients with left-sided chronic ulcerative colitis. Inflamm Bowel Dis. 2004;10:215-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 42] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Choi YS, Kim WJ, Kim JK, Kim DS, Lee DH. Efficacy of topical 5-aminosalicylate monotherapy in patients with ulcerative proctitis with skip inflammation. J Gastroenterol Hepatol. 2018;33:1200-1206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Park SH, Yang SK, Park SK, Kim JW, Yang DH, Jung KW, Kim KJ, Ye BD, Byeon JS, Myung SJ, Kim JH. Atypical distribution of inflammation in newly diagnosed ulcerative colitis is not rare. Can J Gastroenterol Hepatol. 2014;28:125-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Choi YS, Kim JK, Kim WJ, Kim MJ. Remission of diffuse ulcerative duodenitis in a patient with ulcerative colitis after infliximab therapy: a case study and review of the literature. Intest Res. 2019;17:273-277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Joo M, Odze RD. Rectal sparing and skip lesions in ulcerative colitis: a comparative study of endoscopic and histologic findings in patients who underwent proctocolectomy. Am J Surg Pathol. 2010;34:689-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (1)] |
| 6. | Terashima S, Hoshino Y, Kanzaki N, Kogure M, Gotoh M. Ulcerative duodenitis accompanying ulcerative colitis. J Clin Gastroenterol. 2001;32:172-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 39] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Lee HS, Choe J, Lee HJ, Hwang SW, Park SH, Yang DH, Kim KJ, Ye BD, Byeon JS, Myung SJ, Yoon YS, Yu CS, Kim JH, Yang SK. Change in the diagnosis of inflammatory bowel disease: a hospital-based cohort study from Korea. Intest Res. 2016;14:258-263. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Bernstein CN, Shanahan F, Anton PA, Weinstein WM. Patchiness of mucosal inflammation in treated ulcerative colitis: a prospective study. Gastrointest Endosc. 1995;42:232-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 120] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | Washington K, Greenson JK, Montgomery E, Shyr Y, Crissinger KD, Polk DB, Barnard J, Lauwers GY. Histopathology of ulcerative colitis in initial rectal biopsy in children. Am J Surg Pathol. 2002;26:1441-1449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 82] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 10. | Watson AJ, Johnston AT, Barker PM, Youngson GG, Bisset WM, Mahomed AA. The presentation and management of juvenile-onset chronic inflammatory bowel disease in Northeastern Scotland. J Pediatr Surg. 2002;37:83-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Glickman JN, Bousvaros A, Farraye FA, Zholudev A, Friedman S, Wang HH, Leichtner AM, Odze RD. Pediatric patients with untreated ulcerative colitis may present initially with unusual morphologic findings. Am J Surg Pathol. 2004;28:190-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 91] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 12. | Loftus EV Jr, Harewood GC, Loftus CG, Tremaine WJ, Harmsen WS, Zinsmeister AR, Jewell DA, Sandborn WJ. PSC-IBD: a unique form of inflammatory bowel disease associated with primary sclerosing cholangitis. Gut. 2005;54:91-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 515] [Cited by in RCA: 518] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 13. | Sinakos E, Samuel S, Enders F, Loftus EV Jr, Sandborn WJ, Lindor KD. Inflammatory bowel disease in primary sclerosing cholangitis: a robust yet changing relationship. Inflamm Bowel Dis. 2013;19:1004-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 14. | Oshitani N, Kitano A, Nakamura S, Obata A, Hashimura H, Hiki M, Matsumoto T, Okawa K, Kobayashi K. Clinical and prognostic features of rectal sparing in ulcerative colitis. Digestion. 1989;42:39-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Horio Y, Uchino M, Bando T, Chohno T, Sasaki H, Hirata A, Takesue Y, Ikeuchi H. Rectal-sparing type of ulcerative colitis predicts lack of response to pharmacotherapies. BMC Surg. 2017;17:59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Yang SK, Hong WS, Min YI, Kim HY, Yoo JY, Rhee PL, Rhee JC, Chang DK, Song IS, Jung SA, Park EB, Yoo HM, Lee DK, Kim YK. Incidence and prevalence of ulcerative colitis in the Songpa-Kangdong District, Seoul, Korea, 1986-1997. J Gastroenterol Hepatol. 2000;15:1037-1042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 124] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 17. | Dignass A, Eliakim R, Magro F, Maaser C, Chowers Y, Geboes K, Mantzaris G, Reinisch W, Colombel JF, Vermeire S, Travis S, Lindsay JO, Van Assche G. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 1: definitions and diagnosis. J Crohns Colitis. 2012;6:965-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 602] [Cited by in RCA: 641] [Article Influence: 49.3] [Reference Citation Analysis (0)] |
| 18. | Silverberg MS, Satsangi J, Ahmad T, Arnott ID, Bernstein CN, Brant SR, Caprilli R, Colombel JF, Gasche C, Geboes K, Jewell DP, Karban A, Loftus EV Jr, Peña AS, Riddell RH, Sachar DB, Schreiber S, Steinhart AH, Targan SR, Vermeire S, Warren BF. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005;19 Suppl A:5A-36A. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2148] [Cited by in RCA: 2368] [Article Influence: 215.3] [Reference Citation Analysis (0)] |
| 19. | Rajwal SR, Puntis JW, McClean P, Davison SM, Newell SJ, Sugarman I, Stringer MD. Endoscopic rectal sparing in children with untreated ulcerative colitis. J Pediatr Gastroenterol Nutr. 2004;38:66-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 41] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Spiliadis CA, Spiliadis CA, Lennard-Jones JE. Ulcerative colitis with relative sparing of the rectum. Clinical features, histology, and prognosis. Dis Colon Rectum. 1987;30:334-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 37] [Article Influence: 1.0] [Reference Citation Analysis (0)] |