Published online Jan 16, 2020. doi: 10.4253/wjge.v12.i1.17
Peer-review started: May 20, 2019
First decision: August 2, 2019
Revised: August 30, 2019
Accepted: November 6, 2019
Article in press: November 6, 2019
Published online: January 16, 2020
Processing time: 216 Days and 9.9 Hours
We recently developed a new endoscopic closure technique using only conventional endo-clips for colorectal lesions. Little is known about the feasibility of the endoscopic mucosa-submucosa clip closure method for gastric lesions.
To elucidate the efficacy of the endoscopic mucosa-submucosa clip closure method after gastric endoscopic submucosal dissection (ESD).
Twenty-two patients who underwent gastric ESD and mucosa-submucosa clip closure were included in this study. In this method, endo-clips are placed at the edges of a mucosal defect. Additional endo-clips are then applied in the same way to facilitate reduction of the defect size. Additional endo-clips are applied to both sides of the mucosal defect. Complete closure can be achieved. We have also developed a “location score” and “closure difficulty index” for assessment purposes.
Complete closure was achieved in 68.2% of the patients (15/22). The location score in the failure group was significantly larger than that in the complete closure group (P = 0.023). The closure difficulty index in the failure group was significantly higher than that in the complete closure group (P = 0.007). When the cutoff value of the closure difficulty index was set at 99, the high closure difficulty index predicted failure with a sensitivity of 57.1%, specificity of 100%, and accuracy of 86.3%.
The endoscopic mucosa-submucosa clip closure method was unreliable after gastric ESD, especially in cases with a high closure difficulty index.
Core tip: The endoscopic mucosa-submucosa clip closure method is a simple closure method using only conventional clips. The success rate of the endoscopic mucosa-submucosa clip closure method was 68.2% (15/22) after gastric endoscopic submucosal dissection. The location and size of a mucosal defect were considered to be the main factors underlying difficulty in closure. Defects were relatively easy to close in the greater curvature of the upper or middle third stomach, because the gastric wall was relatively thin and soft and a front view approach could be taken.
- Citation: Kinoshita S, Nishizawa T, Fujimoto A, Mori H, Nakazato Y, Kikuchi M, Uraoka T. Efficacy of mucosa-submucosa clip closure method after gastric endoscopic submucosal dissection. World J Gastrointest Endosc 2020; 12(1): 17-22
- URL: https://www.wjgnet.com/1948-5190/full/v12/i1/17.htm
- DOI: https://dx.doi.org/10.4253/wjge.v12.i1.17
The introduction of endoscopic submucosal dissection (ESD) has led to great advances in the endoscopic treatment of gastric cancer. ESD has been adopted as an established standard treatment for early gastric tumors with the proven capacity to remove large lesions exceeding 2 cm in diameter[1,2]. However, this method sometimes causes complications such as bleeding and perforation. Even when ESD is successfully performed, the ESD-induced ulcers are exposed to gastric acid, pepsin, and mechanical stimuli. Exposure of the ulcers to these elements introduces a risk of delayed perforation or bleeding for several days after the ESD procedure. Patients, therefore, generally must remain in hospital for 5-7 d post-operation[3].
The endoscopic purse-string suture[4], “loop clip”[5], slip knot clip suturing method[6], and string clip suturing method[7] have been reported to be useful for closure of large mucosal defect. The success rates of these methods are over 90%. However, these methods require an endo-loop, double-channel endoscope, string, or supplemental devices. Our group previously developed a simple closure method using only conventional clips[8]. The endoscopic mucosa-submucosa clip closure method is effective in completely closing mucosal defects as large as 2-4 cm in diameter after colorectal ESD[9]. Here we report the results of a clinical pilot study to investigate the use of the endoscopic mucosa-submucosa clip closure method after gastric ESD.
Patients with early gastric cancers of less than 35 mm in diameter were selected for inclusion in this study. The exclusion criteria were as follows: (1) Specimen diameter of more than 50 mm; (2) Tumor extension to the cardia or pyloric ring; (3) Suspected submucosal invasion; (4) Tumor with indistinct borders; and (5) Judgment by the operator that the mucosal defect cannot be closed. Seventy patients underwent gastric ESD at Tokyo Medical Center between May 2018 and February 2019. Of these, 22 patients underwent mucosa-submucosa clip closure after gastric ESD. The protocol of this trial was approved by the in-facility review committee of the Tokyo Medical Center (registration number: R17-106). Written informed consent was obtained from all patients.
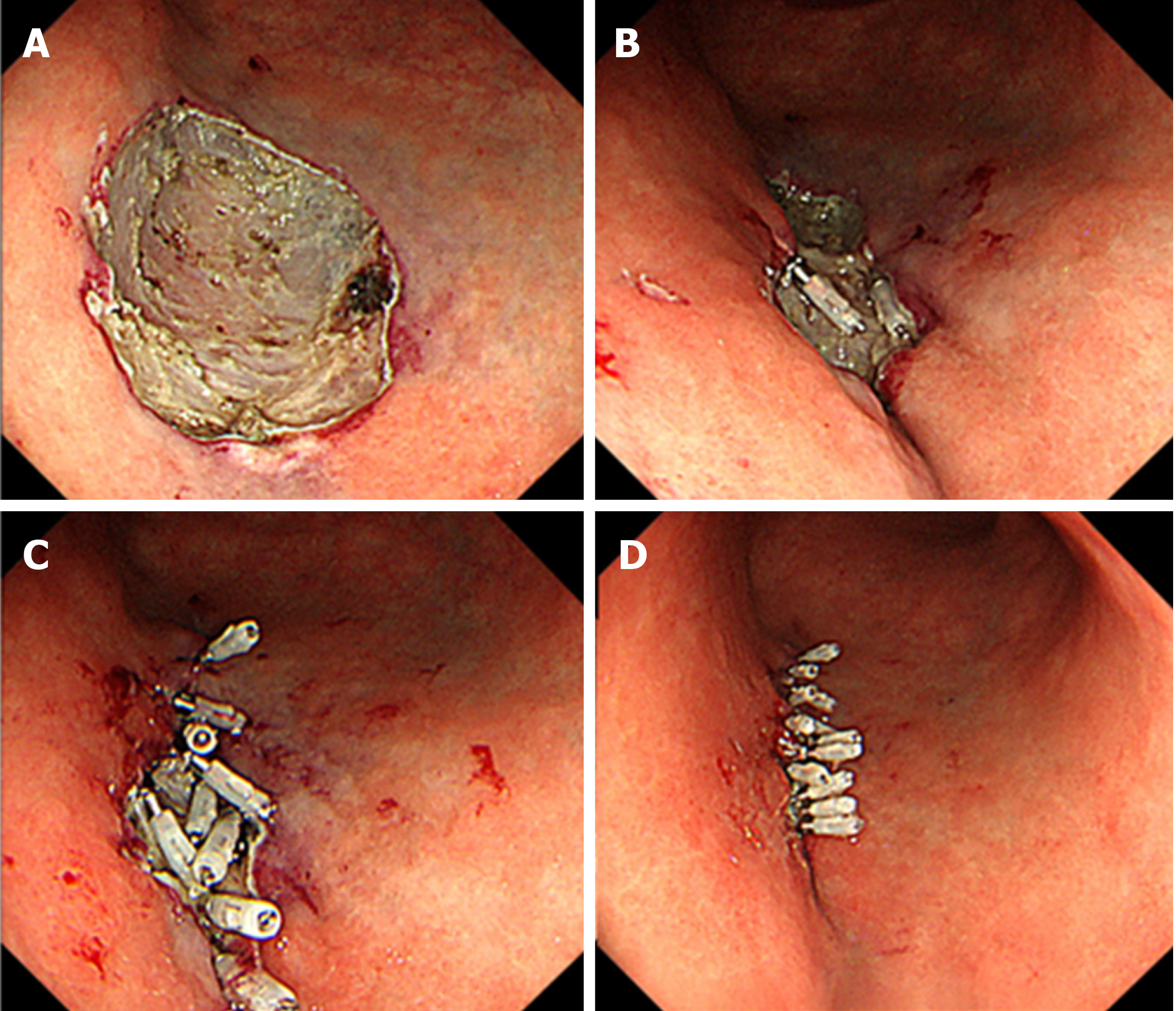
Several standard endo-clips [EZ ClipⓇ, HX-610-090L (long-type), Olympus, Tokyo, Japan] were placed at the edges of the mucosal defect[8]. In some cases, a Resolution™ Clip Device (Boston Scientific, Boston, MA, United States) was also occasionally used. The two arms of the endo-clips respectively gripped the mucosa and submucosa in the direction parallel to the short axis of the mucosal defect. Additional endo-clips were then applied in the same way to facilitate the gradual reduction in defect size. Additional endo-clips can then be applied to both sides of the mucosal defect. Complete closure is then achieved. Furthermore, endoscopic inspection was performed to visually confirm complete closure (Figure 1). The endoscopic procedure was carried out using a GIF-Q260J, GIF-H260Z, or GIF-2 TMQ260M (Olympus Co., Tokyo, Japan).
Outcomes: We evaluated the success rate, size of the resected specimen, location of the lesion, procedure time, number of clips, adverse events, and length of hospital stay. The areas of the resected specimens were measured using Image JⓇ software (National Institutes of Health, Unites States).
The success rate was defined as the percentage of successes (complete closure of mucosal defect) in the patients enrolled. “Complete closure of the mucosal defect” was defined as complete closure of the whole resection site with clips. The procedure time was measured from the insertion of the first clip to completion of the procedure.
Closure difficulty index: The difficulty in closing the defects was assessed by assigning a “closure difficulty index” defined as: The “size of the resected specimen (mm)” × “location score.” The location score was assigned as follows: The posterior wall of the stomach and anterior wall or lessor curvature of the upper third stomach were scored as 3; the greater curvature of the upper or middle third stomach was scored as 1; other areas were scored as 2. Mucosal defects were difficult to close in the posterior wall of the stomach and anterior wall or lessor curvature of the upper third stomach, because a lateral view approach had to be taken. Defects were relatively easy to close in the greater curvature of the upper or middle third stomach, because the gastric wall was relatively thin and soft and a front view approach could be taken.
Adverse events: Perforation during ESD was diagnosed if mesenteric fat or intra-abdominal space was observed during the ESD procedure or if free air was detected on chest and abdominal radiographs. Delayed perforation was defined when a patient manifested no signs of perforation during ESD and no symptoms immediately after tumor removal but later complained of sudden abdominal pain and manifested free air on X-ray. Delayed bleeding was defined as bleeding symptoms or hemoglobin loss (≥ 2 g/dL).
Each continuous variable was expressed as a mean ± standard deviation. Differences between the two groups were detected using the Student’s t-test or Welch's t-test for continuous data. Categorical secondary outcomes were compared using the chi-squared test. A P value of less than 0.05 was considered statistically significant. All statistical analyses were performed using Stat Mate IV software (ATOMS, Tokyo, Japan).
The characteristics of the complete closure group and failure group are summarized in Table 1. The success rate of the endoscopic mucosa-submucosa clip closure method was 68.2% (15/22). Of the 7 cases in the failure group, 3 had partial closure of more than 80% but failed to achieve complete closure. The specimens resected from the failure group were larger than those resected from the complete closure group, but not significantly (P = 0.087). The failure group had a significantly higher location score (P = 0.023) and closure difficulty index (P = 0.007) than the complete closure group.
| Complete closure | Failure | P value | |
| Patient | |||
| Number | 15 | 7 | |
| Male sex, n (%) | 12 (80) | 6 (85.7) | 0.787 |
| Age (years) | 71.5 ± 8.75 | 75.6 ± 13.1 | 0.392 |
| Use of antithrombotic agent | 3 | 2 | |
| Resected specimen | |||
| Size | 29.3 ± 4.75 | 34.4 ± 8.68 | 0.087 |
| Area | 6.68 ± 2.39 | 7.96 ± 4.21 | 0.37 |
| Location | |||
| L/M/U | 6/8/1 | 2/4/1 | 0.82 |
| A/P/L/G | 5/3/3/4 | 0/5/1/1 | 0.09 |
| Location score | 1.93 ± 0.704 | 2.71 ± 0.49 | 0.016 |
| Closure difficulty index | 56.8 ± 21.9 | 95.4 ± 35 | 0.005 |
| Closure | |||
| Procedure time (s) | 1005.5 ± 723 | 608.3 ± 358.9 | 0.22 |
| Number of clips | 11.8 ± 2.17 | 8.57 ± 3.87 | 0.018 |
| Adverse event | |||
| Perforation during ESD | 3 | 0 | 0.54 |
| Delayed perforation | 0 | 0 | - |
| Delayed bleeding | 0 | 1 | 0.69 |
| Length of hospital stay (days) | 7.36 ± 0.93 | 7.86 ± 2.27 | 0.59 |
There were no significant differences between the complete closure group and failure group in delayed perforation, delayed bleeding, and the length of hospital stay (Table 1). When the cutoff value of the closure difficulty index was set at 99, the high index (≥ 99) predicted failure with a sensitivity of 57.1%, specificity of 100%, positive predictive value of 100%, negative predictive value of 83.3%, and accuracy of 86.3% (Table 2). In cases with a high closure difficulty index (≥ 99), the success rate of the endoscopic mucosa-submucosa clip closure method was 0% (0/4).
| Failure | Success | |
| High closure difficulty index (≥ 99) | 4 | 0 |
| Low closure difficulty index (< 99) | 3 | 15 |
We hypothesized that the endoscopic mucosa-submucosa clip closure method would close gastric mucosal defects of around 2-4 cm in diameter. This study failed to confirm that this method could perform reliably after gastric ESD.
Endoscopic mucosa-submucosa clip closure was often unachieved, especially in cases with a high closure difficulty index (≥ 99). We developed the “closure difficulty index” in the belief that the location and size of a mucosal defect were the main factors underlying difficulty in closure. To the best of our knowledge, the present study is the first to report a useful predictor of failure of gastric mucosal defect closure. Endoscopists should consider other closure methods or forgo closing altogether in cases with a high closure difficulty index.
Few reports have described the closure of post-gastric ESD compared with post-colorectal ESD[4,10-14]. The lesser degree of closure of post-gastric ESD likely stems from the difficulty in closing a large mucosal defect, because the gastric wall is thick and hard. Li et al[10] reported that mucosal closure with a detachable snare and clips has a success rate of 61% (16/26). Maekawa et al[15] reported that a combined method using over-the-scope clips and through-the-scope clips had a success rate of 91.7% (11/12), but the patients selected for their study had gastric tumors of 3 cm in diameter or less. More effective methods are expected to be developed in the future for larger lesions.
The limitations of this study include its retrospective design. The study was also single-armed and did not compare the superiority of the mucosa-submucosa clip closure method with other methods. Furthermore, the small number of patients was also a limiting factor. These issues should be re-evaluated in larger prospective studies in the future. In conclusion, the endoscopic mucosa-submucosa clip closure method was unreliable after gastric ESD, especially in cases with a high closure difficulty index.
We recently developed the endoscopic mucosa-submucosa clip closure method for mucosal defects after endoscopic submucosal dissection (ESD). The method is a simple closure method using only conventional clips.
The endoscopic mucosa-submucosa clip closure method is feasible for colorectal mucosal defects. However, the feasibility for gastric mucosal defects is still unknown.
The aim of this retrospective study was to elucidate the efficacy of endoscopic mucosa-submucosa clip closure method for gastric mucosal defects.
Twenty-two patients who underwent gastric ESD and mucosa-submucosa clip closure were investigated in this study. The difficulty in closing the defects was assessed by the newly developed “location score” and “closure difficulty index”. “Closure difficulty index” was defined as: “size of the resected specimen (mm)” × “location score.” In the “location score”, the area with thick gastric wall and lateral view approach was scored as 3; the area with thin gastric wall and front view approach was scored as 1; other areas were scored as 2.
The success rate was 68.2% (15/22). The failure group had a significantly higher location score (P = 0.023) and closure difficulty index (P = 0.007) than the complete closure group. When the cutoff value of the closure difficulty index was set at 99, the high closure difficulty index predicted failure with a sensitivity of 57.1%, specificity of 100%, and accuracy of 86.3%.
The endoscopic mucosa-submucosa clip closure method after gastric ESD would fail in cases with a high closure difficulty index.
The endoscopic mucosa-submucosa clip closure method is effective in completely closing mucosal defects as large as 2-4 cm in diameter after colorectal ESD.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Goral V, Jonaitis LV, Lee CL, Zhu YL S-Editor: Yan JP L-Editor: Webster JR E-Editor: Ma YJ
| 1. | Nishizawa T, Yahagi N. Endoscopic mucosal resection and endoscopic submucosal dissection: technique and new directions. Curr Opin Gastroenterol. 2017;33:315-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 77] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 2. | Fujimoto A, Goto O, Nishizawa T, Ochiai Y, Horii J, Maehata T, Akimoto T, Kinoshita S, Sagara S, Sasaki M, Uraoka T, Yahagi N. Gastric ESD may be useful as accurate staging and decision of future therapeutic strategy. Endosc Int Open. 2017;5:E90-E95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Kim YJ, Park DK. Management of complications following endoscopic submucosal dissection for gastric cancer. World J Gastrointest Endosc. 2011;3:67-70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Zhang Y, Wang X, Xiong G, Qian Y, Wang H, Liu L, Miao L, Fan Z. Complete defect closure of gastric submucosal tumors with purse-string sutures. Surg Endosc. 2014;28:1844-1851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 53] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Sakamoto N, Beppu K, Matsumoto K, Shibuya T, Osada T, Mori H, Shimada Y, Konno A, Kurosawa A, Nagahara A, Otaka M, Ohkusa T, Ogihara T, Watanabe S. "Loop Clip", a new closure device for large mucosal defects after EMR and ESD. Endoscopy. 2008;40 Suppl 2:E97-E98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 45] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Nishizawa T, Ochiai Y, Uraoka T, Akimoto T, Mitsunaga Y, Goto O, Fujimoto A, Maehata T, Kanai T, Yahagi N. Endoscopic slip-knot clip suturing method: prospective pilot study (with video). Gastrointest Endosc. 2017;85:433-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Yahagi N, Nishizawa T, Akimoto T, Ochiai Y, Goto O. New endoscopic suturing method: string clip suturing method. Gastrointest Endosc. 2016;84:1064-1065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 8. | Banno S, Nishizawa T, Kinoshita S, Mori H, Uraoka T. Endoscopic mucosa-submucosal clip closure method. Endoscopy. 2017;49:E307-E308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Nishizawa T, Banno S, Kinoshita S, Mori H, Nakazato Y, Hirai Y, Kubosawa Y, Sunata Y, Matsushita M, Uraoka T. Feasibility of endoscopic mucosa-submucosa clip closure method (with video). Endosc Int Open. 2018;6:E1070-E1074. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Lee BI, Kim BW, Kim HK, Choi H, Ji JS, Hwang SM, Cho YS, Chae HS, Choi KY. Routine mucosal closure with a detachable snare and clips after endoscopic submucosal dissection for gastric epithelial neoplasms: a randomized controlled trial. Gut Liver. 2011;5:454-459. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 11. | Goto O, Sasaki M, Akimoto T, Ochiai Y, Kiguchi Y, Mitsunaga Y, Fujimoto A, Maehata T, Nishizawa T, Takeuchi H, Kitagawa Y, Yahagi N. Endoscopic hand-suturing for defect closure after gastric endoscopic submucosal dissection: a pilot study in animals and in humans. Endoscopy. 2017;49:792-797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 12. | Akimoto T, Goto O, Sasaki M, Ochiai Y, Maehata T, Fujimoto A, Nishizawa T, Yahagi N. "Hold-and-drag" closure technique using repositionable clips for large mucosal defects after colonic endoscopic submucosal dissection. Endosc Int Open. 2016;4:E1068-E1072. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 13. | Harada H, Suehiro S, Murakami D, Nakahara R, Ujihara T, Shimizu T, Miyama Y, Katsuyama Y, Hayasaka K, Tounou S. Clinical impact of prophylactic clip closure of mucosal defects after colorectal endoscopic submucosal dissection. Endosc Int Open. 2017;5:E1165-E1171. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 14. | Ogiyama H, Tsutsui S, Murayama Y, Maeda S, Satake S, Nasu A, Umeda D, Miura Y, Tominaga K, Horiki M, Sanomura T, Imanaka K, Iishi H. Prophylactic clip closure may reduce the risk of delayed bleeding after colorectal endoscopic submucosal dissection. Endosc Int Open. 2018;6:E582-E588. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 15. | Maekawa S, Nomura R, Murase T, Ann Y, Harada M. Complete closure of artificial gastric ulcer after endoscopic submucosal dissection by combined use of a single over-the-scope clip and through-the-scope clips (with videos). Surg Endosc. 2015;29:500-504. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |