Copyright
©The Author(s) 2016.
World J Gastrointest Endosc. Feb 10, 2016; 8(3): 192-197
Published online Feb 10, 2016. doi: 10.4253/wjge.v8.i3.192
Published online Feb 10, 2016. doi: 10.4253/wjge.v8.i3.192
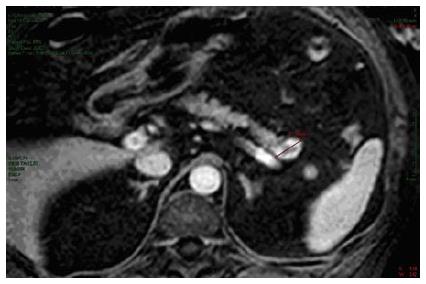
Figure 1 Abdominal magnetic resonance imaging demonstrating a round, well-demarcated nodule of the pancreatic tail.
The 22 mm lesion (calipers) shows highly vascularised peripheral tissue.
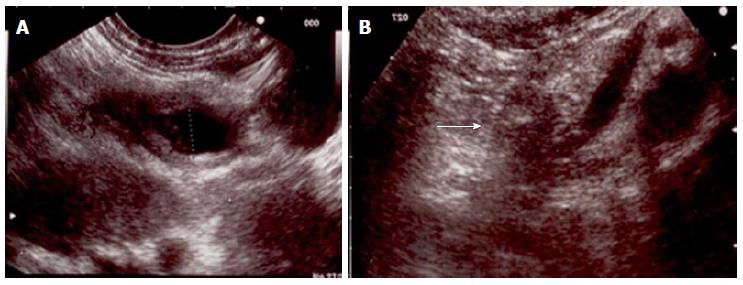
Figure 2 Endoscopic ultrasound appearances before (A) and after (B) treatment (white arrow).
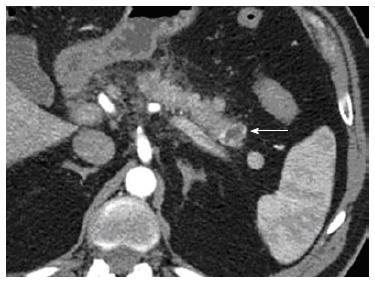
Figure 3 Computed tomography scan showing thin residual hypervascular tissue (white arrow) two months after the first treatment.
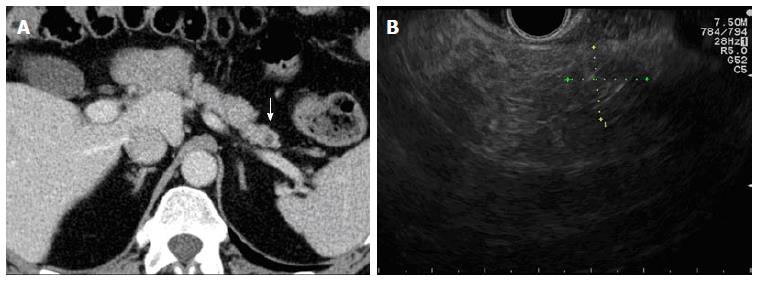
Figure 4 Twenty-four months follow-up.
A: Computed tomography scan showing absence of hypervascular tissue around a small hypodense area (white arrow); B: Endoscopic ultrasound scan of the pancreatic tail demonstrating poorly defined hyperechoic tissue (fibrosis) with posterior shadow (caliper).
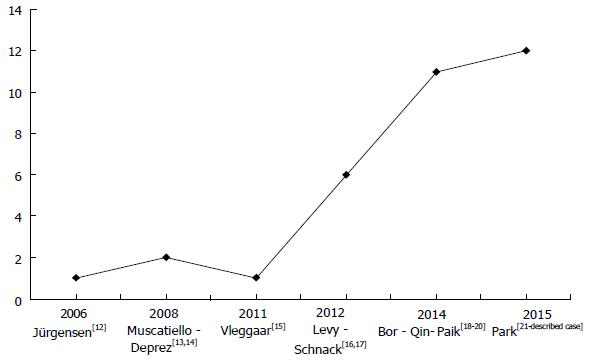
Figure 5 Reported endoscopic ultrasound-guided ethanol ablation procedures over time.
Literature review showed a progressive increase of performed procedures from 2006 to 2015. Cases described in abstract form by Paik et al[20] were not included in the final results analysis.
- Citation: Armellini E, Crinò SF, Ballarè M, Pallio S, Occhipinti P. Endoscopic ultrasound-guided ethanol ablation of pancreatic neuroendocrine tumours: A case study and literature review. World J Gastrointest Endosc 2016; 8(3): 192-197
- URL: https://www.wjgnet.com/1948-5190/full/v8/i3/192.htm
- DOI: https://dx.doi.org/10.4253/wjge.v8.i3.192