Published online Jul 18, 2016. doi: 10.4254/wjh.v8.i20.844
Peer-review started: March 18, 2016
First decision: April 18, 2016
Revised: May 29, 2016
Accepted: June 14, 2016
Article in press: June 16, 2016
Published online: July 18, 2016
Processing time: 119 Days and 2.2 Hours
AIM: To show that aluminum potassium sulfate and tannic acid (ALTA) sclerotherapy has a high success rate for Grade II and III hemorrhoids.
METHODS: This study was based on the clinical data of 604 patients with hemorrhoids who underwent ALTA sclerotherapy between January 2009 and February 2015. The objective of this study was to assess the efficacy of this treatment for Grades II and III hemorrhoids. Preoperative and postoperative symptoms, complications and success rate were all assessed retrospectively. Follow-up consisted of a simple questionnaire, physical examination and an anoscopy. Patients were followed-up at one day, one week, two weeks, one month, one year, two years, three years, four years and five years after the ALTA sclerotherapy.
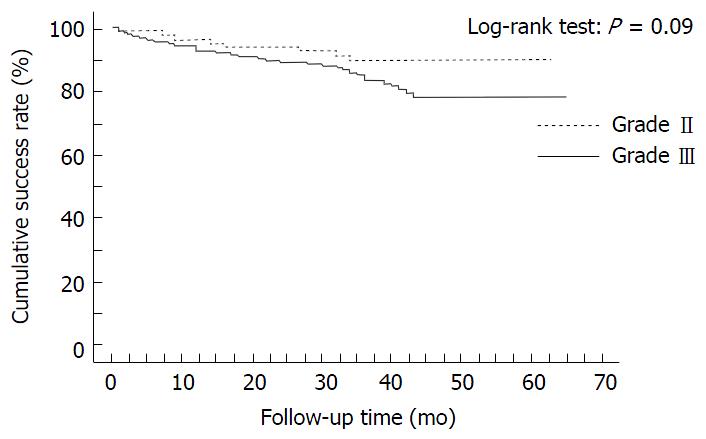
RESULTS: One hundred and sixty-nine patients were diagnosed with Grade II hemorrhoids and 435 patients were diagnosed with Grade III hemorrhoids. The one year, three year and five year cumulative success rates of ALTA sclerotherapy for Grades II and III hemorrhoids were 95.9% and 93.1%; 89.3% and 83.7%; and 89.3% and 78.2%, respectively. No significant differences were observed in the cumulative success rates after ALTA sclerotherapy between Grades II and III hemorrhoids (P = 0.09). There were forty-seven post-operative complications (low grade fever; anal pain; urinary retention; rectal ulcer; and others). No serious or life-threatening complications occurred and all cases improved through conservative treatment. At univariate analysis there were no predictive factors of failure.
CONCLUSION: ALTA sclerotherapy has had a high success rate for Grade II and III hemorrhoids during five years of post-operative treatment. However, additional studies are needed to evaluate the efficacy of this ALTA sclerotherapy in the management of hemorrhoidal disease.
Core tip: Since 2000, aluminum potassium sulfate and tannic acid (ALTA) sclerotherapy has been frequently performed in Japan for internal hemorrhoids as a minimally invasive treatment. This study affirms that ALTA sclerotherapy is an effective and safety treatment for Goligher Grades II and III hemorrhoids because of the high cumulative success rate and no serious complications during post-operative treatment.
- Citation: Miyamoto H, Hada T, Ishiyama G, Ono Y, Watanabe H. Aluminum potassium sulfate and tannic acid sclerotherapy for Goligher Grades II and III hemorrhoids: Results from a multicenter study. World J Hepatol 2016; 8(20): 844-849
- URL: https://www.wjgnet.com/1948-5182/full/v8/i20/844.htm
- DOI: https://dx.doi.org/10.4254/wjh.v8.i20.844
Hemorrhoids are the most common anorectal disease world-wide. The term “hemorrhoidal disease” can be employed when hemorrhoidal tissue gives rise to symptoms such as bleeding, prolapse, or pruritus[1]. Etiologic factors are multi-factorial and include prolonged straining, irregular bowel habits and heredity. Supporting connective tissue degenerates and hemorrhoidal cushions slide as a consequence.
Conservative treatment based on lifestyle changes such as dietary and exercise and laxatives can help the majority of patients, and rubber band ligation, sclerotherapy and phlebotonic drugs can effectively treat Grades I and II hemorrhoids[2]. Surgical treatment is required for the most advanced stages, Grade III or IV and bleeding. There are several methods of surgical treatment for hemorrhoids: Conventional hemorrhoidectomy (CH), stapled hemorrhoidopexy (PPH), and trans-anal hemorrhoidal dearterialization (THD)[1-4].
Among them, PPH and THD aim to correct the underlying pathophysiological mechanisms involved in the etiology of hemorrhoids. These treatments are painless treatment, because of the sparing of the anoderm. Although an increased risk of recurrence is the price to pay for these minimally invasive treatments, a rapid return to normal life without pain are greatly appreciated by patients[5].
On the other hand, new and effective sclerosant named aluminum potassium sulfate and tannic acid (ALTA) has been developed in Japan. ALTA sclerotherapy has been frequently performed in Japan for internal hemorrhoids as a minimally invasive treatment[6-9]. Nowadays in Japan, ALTA sclerotherapy for internal hemorrhoids has been performed in over 300000 cases.
In this report, we present effective results of ALTA sclerotherapy for Grades II and III hemorrhoids, according to the five year follow-up for this multi-center study.
ALTA sclerotherapy was performed on all patients with internal hemorrhoids except for the following: Patients with associated acute inflammatory internal hemorrhoids and acute irreducible hemorrhoids; patients with serious cardiac, hepatic, renal, and hematological diseases; pregnant women or women who may be pregnant; nursing mothers; and patients with a past history of hyper-sensitivity to local anesthetics.
The medical records of 604 patients with hemorrhoidal disease who underwent ALTA sclerotherapy at four institutions from January 2009 to February 2015 were analyzed. All patients underwent clinical evaluation and physical examination including digital examination and proctoscopy for diagnosis of hemorrhoid engorgement and easy-bleeding, prolapsing hemorrhoids. The severity of hemorrhoidal disease was graded according to Goligher’s classification.
Patients assumed the lithotomy position or Sims’ position. Zero point five percent Lidocaine 10 mL was injected around sphincter muscle. The concentration of ALTA solution is set by, Mitsubishi Tanabe Pharma Corporation, Osaka, Japan. Procedures were undertaken under local anesthesia using the Z-type proctoscope (ARAKAWA SEISAKUJO, Tokyo, Japan) with a distally opening window that allowed for the application of an injection into the rectal mucosa. An ALTA four-step injection was performed[7]. The method used for the ALTA four-step injection was to inject four times, once into each of the following parts of the primary hemorrhoid: The superior part; the central deep and slight parts; and the inferior part above the dentate line.
All data were retrospectively collected from medical record. Patients took oral analgesia (loxoprofen or acetaminophen) at three days post operation. They were followed-up at one day, one week, two weeks, one month, one year, two years, three years, four years and five years after the ALTA sclerotherapy. Follow-up consisted of a simple questionnaire, physical examination and an anoscopy. Effects were defined as follows: (1) cure (after bowel movement there is no prolapse of the hemorrhoids, hemorrhage or other discomfort; and on examination with an anoscope, atrophied internal hemorrhoids have disappeared); (2) improvement (after bowel movement, some hemorrhoids prolapse but return into the anal canal spontaneously; occasional blood or hemorrhage with bowel movements; and an anoscopic examination reveals some internal hemorrhoids still visible); and (3) failure (no improvement, or some hemorrhoids prolapsed and did not return into the anal canal spontaneously).
ALTA compounds with aluminum potassium sulfate and tannic acid. The aluminum ion induces a strong local inflammatory reaction, resulting in fibrosis[10,11]. Tannic acid has a strong astringent effect on tissue, promoting protein coagulation and the contraction of blood vessels, while reducing exudation into tissue from the inflammatory reaction[10,11]. These actions tend to prevent tissue necrosis, and promote sclerosis, adhesion of hemorrhoidal tissue and immediate hemostasis and are also effective for the prolapse and bleeding of internal hemorrhoids early after injection.
The characteristics of the patients involved in this study are shown in Table 1. From January 2009 until February 2015 ALTA sclerotherapy was performed on 604 patients with second or third degree hemorrhoids. There were three 334 men and 270 women. The age range (mean ± SD) of the patients with Grades II and III hemorrhoids was 58 ± 18 years and 59 ± 16 years, respectively. Overall, 169 patients had Grade II hemorrhoids and 435 had Grade III hemorrhoids. The total injection dose of ALTA (mean ± SD) for Grades II and III was 13.4 ± 5.2 mL and 21.5 ± 6.8 mL, respectively. The operative time (mean ± SD) of Grades II and III was 14 ± 8 min and 16 ± 7 min, respectively. All the operations were performed under local anesthesia during either day surgery or a one day hospital stay.
| Goligher classification | Grade II | Grade III | Statistical significance |
| Number | 169 | 435 | |
| Gender | |||
| Male | 103 | 231 | NS |
| Female | 66 | 204 | |
| Age (yr) | 58 ± 18 | 59 ± 16 | NS |
| Injection dose of ALTA (mL) | 13.4 ± 5.2 | 21.5 ± 6.8 | P < 0.0001 |
| Operative time | 14 ± 8 | 16 ± 7 | P = 0.0020 |
Prolapses and bleeding disappeared immediately after ALTA sclerotherapy. All cases with bleeding or prolapses were cured or there was improvement after the first post-operative month. At one year after treatment, the rate of successful resolution of bleeding or prolapse of Grades II and III was 95.9% and 93.1%, respectively. The three year and five year cumulative success rates of ALTA sclerotherapy for Grades II and III hemorrhoids were 89.3% and 83.7%; and 89.3% and 78.2%, respectively. At one year after treatment, the rate of failure of Grades II and III was 4.1% and 6.9%, respectively. The three year and five year cumulative failure rates of ALTA sclerotherapy for Grades II and III hemorrhoids were 10.7% and 16.3%; and 10.7% and 21.8%, respectively. No significant differences were observed in the cumulative success rates after ALTA sclerotherapy between Grades II and III hemorrhoids (P = 0.09) (Figure 1). There were 47 post-operative complications (low grade fever; anal pain; urinary retention; rectal ulcer; and others). No serious or life-threatening complications occurred and all cases improved through conservative treatment. At uni-variate analysis there were no predictive factors of failure (Table 2). However, the only factor associated with a recurrence may be the grade of hemorrhoids (P = 0.09).
| Prognostic factor | Relative risk (95%CI) | P value |
| Age | 0.997 (0.981-1.012) | 0.6567 |
| Gender | 0.800 (0.469-1.365) | 0.4124 |
| Goligher grade | 1.768 (0.897-3.483) | 0.0997 |
| Operation time | 0.974 (0.941-1.010) | 0.1542 |
| ALTA injection dose | 0.976 (0.941-1.012) | 0.1901 |
| Complication | 1.293 (0.469-3.564) | 0.6189 |
The ideal operation for hemorrhoids should be effective with a low rate of recurrence; minimal post-operative pain to allow early return to normal activities; and safe with minimal morbidity[12]. The treatment for internal hemorrhoids is gradually shifting to minimally invasive surgery. CH has been used to be the most widely performed surgical procedure till now. Although CH was very effective, it was painful and potentially affected the mechanism of anal continence. Over the years, alternative minimally invasive techniques have been developed including stapled hemorrhoidopexy, also known as PPH, and trans-anal hemorrhoidal dearterialization, also known as THD[1,3-5]. In Japan, new sclerosant, ALTA, has been developed. Takano et al[6] reported that ALTA (OC-108) sclerotherapy was effective for Grades II, III, and IV internal hemorrhoids. In recent years in Japan, ALTA sclerotherapy has become gradually recognized as minimally invasive treatment for internal hemorrhoids.
In Japan, ALTA sclerotherapy is popular with patients with symptomatic internal hemorrhoids, because unpleasant symptoms disappear immediately on the first post-operative day in almost all cases[7], and patients experience little post-operative pain and no serious complications[6-9]. ALTA sclerotherapy could be performed on patients with Grades II and III hemorrhoids in an outpatient clinic. Patients are highly satisfied with ALTA sclerotherapy as a treatment for internal hemorrhoids. Our previous study demonstrated that overall patient satisfaction at one month and one year after ALTA sclerotherapy was 97.7%[13]. In the Japanese literature, Matsuda et al[14] reported that the overall satisfaction of ALTA sclerotherapy was over 90% and concluded that ALTA sclerotherapy matched the needs of patients with symptomatic internal hemorrhoids. Minimally invasive treatments such as PPH, THD, or Doppler-guided hemorrhoidal arterial ligation (DGHAL) are acceptable treatments. But, if recurrence is the main consideration, CH is still considered the best[15]. A recent systematic review of 27 randomized controlled trials demonstrated that, compared with CH, PPH had less pain, shorter operative time, and quicker patient’s recovery of patient, but a significantly higher rate of prolapse and reintervention for prolapse[16]. The recurrence rate and additional operation rate related to each technique were summarized in Table 3. Although the follow-up time was different, the recurrence rate and/or additional operation rate of CH, stapled hemorrhoidopexy, THD, DGHAL with rectoanal repair and ALTA was 0%-2%, 7.5%-13%, 0%-14%, 4%-10.34% and 3.6%-16%, respectively[4-7,17-24]. In this study, the one year cumulative rate for the successful resolution of bleeding or prolapse of Grades II and III was 95.9% and 93.1%, respectively. The five year cumulative success rate of ALTA sclerotherapy for Grades II and III hemorrhoids was 89.3% and 78.2%, respectively. ALTA sclerotherapy has had a high success rate for Grades II and III hemorrhoids during the five years post treatment.
| Ref. | Grade | Technique | n | Follow-up | Recurrence rate and/or additional surgery rate (%) |
| Giordano et al[4] | II, III | THD | 28 | 3 yr | 14.00 |
| SH | 24 | 13.00 | |||
| Giordano et al[17] | IV | THD + targeted mucopexy | 31 | 32 mo | 6.40 |
| Ratto et al[18] | II, III, IV | THD | 170 | 11.5 mo | 4.10 |
| Ratto et al[19] | II, III, IV | THD | 803 | 11.1 mo | 10.20 |
| Zampieri et al[20] | III, IV | THD | 46 | 1-6 mo | 0 |
| Ligasure | 68 | 4.00 | |||
| Theodoropoulos et al[21] | III, IV | DGHAL + RAR | 147 | 15 mo | 4.00 |
| Walega et al[22] | III, IV | DGHAL + RAR | 29 | 3 mo | 10.34 |
| Gravié et al[23] | SH | 63 | 2 yr | 7.50 | |
| MMH | 63 | 1.80 | |||
| Ammaturo et al[24] | III | SH | 39 | 2 yr | 13.00 |
| MMH | 40 | 0 | |||
| Hachiro et al[8] | III, IV | ALTA | 448 | 29 mo | 3.60 |
| Takano et al[6] | III, IV | ALTA (OC-108) | 80 | 1 yr | 16.00 |
| CH | 85 | 2.00 | |||
| Miyamoto et al[7] | II, III, IV | ALTA | 28 | 5 mo | 10.70 |
Vidal et al[25] reported a new concept for the treatment of hemorrhoids with arterial embolization. Fourteen patients with disabling chronic rectal bleeding were treated using the emborrhoid technique. Although 10 patients had coagulation disorders (anticoagulants or cirrhosis), coil embolization of the superior rectal arteries is technically feasible, safe and well tolerated. Yano et al[26] reported that among patients with hemorrhoids receiving anticoagulant, ALTA sclerotherapy was recommended for those in whom it was difficult to discontinue anticoagulant. Miyamoto et al[27] reported the efficacy and safety of ALTA sclerotherapy for hemorrhoidal patients with liver cirrhosis.
In conclusion, ALTA sclerotherapy is an effective treatment for Grades II or III hemorrhoids. ALTA sclerotherapy might revolutionize the present state of hemorrhoid treatment and be the ideal method for symptomatic internal hemorrhoids needed surgery. However, additional studies are needed to evaluate the efficacy of this ALTA sclerotherapy in the management of hemorrhoidal disease.
Aluminum potassium sulfate and tannic acid (ALTA) sclerotherapy is intended to shrink and harden internal hemorrhoids to eliminate hemorrhoidal prolapse and bleeding. ALTA sclerotherapy has been recognized as minimally invasive treatment for symptomatic internal hemorrhoid in Japan. The effectiveness of ALTA sclerotherapy, which shrinks and hardens internal hemorrhoids, is permanent.
There are few reports of clarifying long time follow-up after ALTA sclerotherapy. The results of this study contribute to clarifying the effectiveness of ALTA sclerotherapy for Grade II or III hemorrhoids with five-year follow-up.
In this study, ALTA sclerotherapy is an effective treatment for Grades II or III hemorrhoids. The one-year, three-year and five-year cumulative success rates of ALTA sclerotherapy for Grades II and III hemorrhoids were 95.9% and 93.1%; 89.3% and 83.7%; and 89.3% and 78.2%, respectively. ALTA is an epoch-making sclerosant. ALTA sclerotherapy might be an effective sclerotherapy for symptomatic internal hemorrhoids needed surgery.
This study suggests that ALTA sclerotherapy is an effective treatment for Grades II or III hemorrhoids. If a patient is diagnosed with Grade II or IIIhemorrhoids, ALTA sclerotherapy can be chosen.
This is an interesting manuscript describing a relatively new minimally invasive treatment of haemorrhoids. The paper has a good number of cases and it is well designed.
Manuscript source: Invited manuscript
P- Reviewer: Milone M, Parellada CM, Tarazov PG S- Editor: Gong ZM L- Editor: A E- Editor: Li D
| 1. | Festen S, van Hoogstraten MJ, van Geloven AA, Gerhards MF. Treatment of grade III and IV haemorrhoidal disease with PPH or THD. A randomized trial on postoperative complications and short-term results. Int J Colorectal Dis. 2009;24:1401-1405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 56] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 2. | Acheson AG, Scholefield JH. Management of haemorrhoids. BMJ. 2008;336:380-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 67] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 3. | Dal Monte PP, Tagariello C, Sarago M, Giordano P, Shafi A, Cudazzo E, Franzini M. Transanal haemorrhoidal dearterialisation: nonexcisional surgery for the treatment of haemorrhoidal disease. Tech Coloproctol. 2007;11:333-338; discussion 338-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 100] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 4. | Giordano P, Nastro P, Davies A, Gravante G. Prospective evaluation of stapled haemorrhoidopexy versus transanal haemorrhoidal dearterialisation for stage II and III haemorrhoids: three-year outcomes. Tech Coloproctol. 2011;15:67-73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 95] [Cited by in RCA: 84] [Article Influence: 6.0] [Reference Citation Analysis (1)] |
| 5. | Altomare DF, Giuratrabocchetta S. Conservative and surgical treatment of haemorrhoids. Nat Rev Gastroenterol Hepatol. 2013;10:513-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (2)] |
| 6. | Takano M, Iwadare J, Ohba H, Takamura H, Masuda Y, Matsuo K, Kanai T, Ieda H, Hattori Y, Kurata S. Sclerosing therapy of internal hemorrhoids with a novel sclerosing agent. Comparison with ligation and excision. Int J Colorectal Dis. 2006;21:44-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 46] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Miyamoto H, Asanoma M, Miyamoto H, Shimada M. ALTA injection sclerosing therapy: non-excisional treatment of internal hemorrhoids. Hepatogastroenterology. 2012;59:77-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 8. | Hachiro Y, Kunimoto M, Abe T, Kitada M, Ebisawa Y. Aluminum potassium sulfate and tannic acid (ALTA) injection as the mainstay of treatment for internal hemorrhoids. Surg Today. 2011;41:806-809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Tokunaga Y, Sasaki H, Saito T. Evaluation of sclerotherapy with a new sclerosing agent and stapled hemorrhoidopexy for prolapsing internal hemorrhoids: retrospective comparison with hemorrhoidectomy. Dig Surg. 2010;27:469-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Ono T, Goto K, Takagi S, Iwasaki S, Komatsu H. Sclerosing effect of OC-108, a novel agent for hemorrhoids, is associated with granulomatous inflammation induced by aluminum. J Pharmacol Sci. 2005;99:353-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Ono T, Nakagawa H, Fukunari A, Hashimoto T, Komatsu H. Hemostatic action of OC-108, a novel agent for hemorrhoids, is associated with regional blood flow arrest induced by acute inflammation. J Pharmacol Sci. 2006;102:314-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Yeo D, Tan KY. Hemorrhoidectomy - making sense of the surgical options. World J Gastroenterol. 2014;20:16976-16983. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 60] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 13. | Miyamoto H. ALTA sclerotherapy: the new sclerotherapy for curing advanced internal hemorrhoids, in Sclerotherapy: Procedures, Potential Complications and Clinical Outcomes (editor Brown ER), Nova Science Publishers, Inc. New York, USA, 2014: 149-163. . |
| 14. | Matsuda Y, Kawakami K, Nakai K, Asano M, Tanaka S, Nonaka M, Yano T, Ishimaru K, Yano Y, Ishii S. Recent evidence for operation versus non-operation of the anal treatment. Geka. 2010;72:1515-1520. |
| 15. | Giordano P, Gravante G, Sorge R, Ovens L, Nastro P. Long-term outcomes of stapled hemorrhoidopexy vs conventional hemorrhoidectomy: a meta-analysis of randomized controlled trials. Arch Surg. 2009;144:266-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 101] [Article Influence: 6.3] [Reference Citation Analysis (1)] |
| 16. | Burch J, Epstein D, Sari AB, Weatherly H, Jayne D, Fox D, Woolacott N. Stapled haemorrhoidopexy for the treatment of haemorrhoids: a systematic review. Colorectal Dis. 2009;11:233-243; discussion 243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 57] [Article Influence: 3.6] [Reference Citation Analysis (1)] |
| 17. | Giordano P, Tomasi I, Pascariello A, Mills E, Elahi S. Transanal dearterialization with targeted mucopexy is effective for advanced haemorrhoids. Colorectal Dis. 2014;16:373-376. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 18. | Ratto C, Donisi L, Parello A, Litta F, Doglietto GB. Evaluation of transanal hemorrhoidal dearterialization as a minimally invasive therapeutic approach to hemorrhoids. Dis Colon Rectum. 2010;53:803-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 64] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 19. | Ratto C, Parello A, Veronese E, Cudazzo E, D’Agostino E, Pagano C, Cavazzoni E, Brugnano L, Litta F. Doppler-guided transanal haemorrhoidal dearterialization for haemorrhoids: results from a multicentre trial. Colorectal Dis. 2015;17:O10-O19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (1)] |
| 20. | Zampieri N, Castellani R, Andreoli R, Geccherle A. Long-term results and quality of life in patients treated with hemorrhoidectomy using two different techniques: Ligasure versus transanal hemorrhoidal dearterialization. Am J Surg. 2012;204:684-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Theodoropoulos GE, Sevrisarianos N, Papaconstantinou J, Panoussopoulos SG, Dardamanis D, Stamopoulos P, Bramis K, Spiliotis J, Datsis A, Leandros E. Doppler-guided haemorrhoidal artery ligation, rectoanal repair, sutured haemorrhoidopexy and minimal mucocutaneous excision for grades III-IV haemorrhoids: a multicenter prospective study of safety and efficacy. Colorectal Dis. 2010;12:125-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 22. | Walega P, Krokowicz P, Romaniszyn M, Kenig J, Sałówka J, Nowakowski M, Herman RM, Nowak W. Doppler guided haemorrhoidal arterial ligation with recto-anal-repair (RAR) for the treatment of advanced haemorrhoidal disease. Colorectal Dis. 2010;12:e326-e329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Gravié JF, Lehur PA, Huten N, Papillon M, Fantoli M, Descottes B, Pessaux P, Arnaud JP. Stapled hemorrhoidopexy versus milligan-morgan hemorrhoidectomy: a prospective, randomized, multicenter trial with 2-year postoperative follow up. Ann Surg. 2005;242:29-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 115] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 24. | Ammaturo C, Tufano A, Spiniello E, Sodano B, Iervolino EM, Brillantino A, Braccio B. Stapled haemorrhoidopexy vs. Milligan-Morgan haemorrhoidectomy for grade III haemorrhoids: a randomized clinical trial. G Chir. 2012;33:346-351. [PubMed] |
| 25. | Vidal V, Sapoval M, Sielezneff Y, De Parades V, Tradi F, Louis G, Bartoli JM, Pellerin O. Emborrhoid: a new concept for the treatment of hemorrhoids with arterial embolization: the first 14 cases. Cardiovasc Intervent Radiol. 2015;38:72-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 52] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 26. | Yano T, Nogaki T, Asano M, Tanaka S, Kawakami K, Matsuda Y. Outcomes of case-matched injection sclerotherapy with a new agent for hemorrhoids in patients treated with or without blood thinners. Surg Today. 2013;43:854-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 27. | Miyamoto H, Nakagawa T, Miyamoto H, Takata A. Sclerotherapy Using Aluminum Potassium Sulfate and Tannic Acid (ALTA) for Haemorrhoids in Patients With Liver Cirrhosis. Ann Colorectal Res. 2015;3:e32980. [DOI] [Full Text] |