Published online May 28, 2016. doi: 10.4254/wjh.v8.i15.644
Peer-review started: January 22, 2016
First decision: February 22, 2016
Revised: March 11, 2016
Accepted: May 7, 2016
Article in press: May 9, 2016
Published online: May 28, 2016
Processing time: 119 Days and 3.6 Hours
AIM: To review the outcomes of liver trauma in patients with hepatic injuries only and in patients with associated injuries outside the liver.
METHODS: Data of liver trauma patients presented to our center from January 2003 to October 2013 were reviewed. The patients were divided into two groups. Group 1 consisted of patients who had hepatic injuries only. Group 2 consisted of patients who also had associated injuries outside the liver.
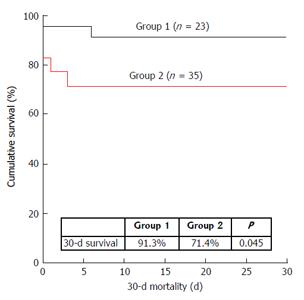
RESULTS: Seven (30.4%) patients in group 1 and 10 (28.6%) patients in group 2 received non-operative management; the rest underwent operation. Blunt trauma occurred in 82.8% (48/58) of the patients and penetrative trauma in 17.2% (10/58). A higher injury severity score (ISS) was observed in group 2 (median 45 vs 25, P < 0.0001). More patients in group 1 were hemodynamically stable (65.2% vs 37.1%, P = 0.036). Other parameters were comparable between groups. Group 1 had better 30-d survival (91.3% vs 71.4%, P = 0.045). On multivariate analysis using the logistic regression model, ISS was found to be associated with mortality (P = 0.004, hazard ratio = 1.035, 95%CI: 1.011-1.060).
CONCLUSION: Liver trauma patients with multiple injuries are relatively unstable on presentation. Despite a higher ISS in group 2, non-operative management was possible for selected patients. Associated injuries outside the liver usually account for morbidity and mortality.
Core tip: Liver trauma patients who have not only liver injury but also associated injury outside the liver usually have a high injury severity score (ISS) and a bigger chance of morbidity and death. Management of liver trauma features surgical and nonsurgical approaches. Choice of approach should depend on individual patients’ overall clinical condition rather than just ISS or imaging findings. The applicability of nonsurgical approach has extended to penetrative injuries with success.
- Citation: She WH, Cheung TT, Dai WC, Tsang SHY, Chan ACY, Tong DKH, Leung GKK, Lo CM. Outcome analysis of management of liver trauma: A 10-year experience at a trauma center. World J Hepatol 2016; 8(15): 644-648
- URL: https://www.wjgnet.com/1948-5182/full/v8/i15/644.htm
- DOI: https://dx.doi.org/10.4254/wjh.v8.i15.644
The liver is well known to be the most frequently injured internal organ in abdominal injury despite its relatively hidden location behind the subcostal region[1]. In liver trauma management, the widespread use of ultrasonography and computed tomography (CT) has facilitated decision-making, and non-operative management (NOM) has been shown to reduce mortality[2]. NOM is now the standard of care for blunt liver injury in hemodynamically stable patients[3-7]. A contrast CT scan of the abdomen can accurately identify the pathology, presence of complication and proper severity grade of injury in hemodynamically stable patients. For hemodynamically unstable patients, operative management (OM) may be necessary. Other considerations should also be taken into account as patients may suffer multiple injuries. Some injuries call for OM. In such cases, the liver injury can be dealt with in the laparotomy required by associated injuries. Treatment outcomes depend on the severity of injuries to organs. This study reviewed the management of liver trauma with or without associated injuries over 10 years at a level-1 trauma center in Hong Kong.
This is a retrospective study. The period for review is from January 2003 to October 2013. Patients at Department of Surgery, Queen Mary Hospital, the University of Hong Kong, who had liver trauma from blunt or penetrative injuries in the period were reviewed. Data of interest included demographic data, presentation, associated injury, mechanism of injury, grade of liver injury, injury severity score (ISS), and management outcome. The data were retrieved by a dedicated trauma nurse coordinator and then screened and reviewed by the authors.
The patients were divided into two groups. Group 1 consisted of patients who had hepatic injuries only. Group 2 was comprised of patients who also had associated injuries outside the liver. The presence of associated injuries was checked for either during the primary and the secondary surveys according to the Advanced Trauma Life Support principle and then by imaging (X-ray or CT scan) of various regions, or during operation. Patients (with or without initial fluid resuscitation) were regarded as hemodynamically stable if they had a patent airway, satisfactory oxygen saturation of > 95%, good volume pulse, heart rate of < 100 beats/min, and systolic blood pressure of > 90 mmHg.
The patients’ grade of liver injury was determined according to the Organ Injury Scaling developed by the Organ Injury Scaling Committee of the American Association for the Surgery of Trauma[8], with grade 1 being the least severe and Grade 6 being unsurvivable. For patients who received NOM, grade of liver injury was determined with a CT scan; for those who received OM, it was determined during operation.
The ISS is an anatomical scoring system that provides an overall score (0-75) for patients with multiple injuries. Calculation of each patient’s ISS was based on signs shown upon physical examination, results of investigation, and findings in operation. Each injury in the six body regions (head, face, chest, abdomen, extremities and external) was assigned an Abbreviated Injury Score (AIS) according to the Abbreviated Injury Scale, and only the highest AIS in each body region were used. Each patient’s three most severely injured body regions had their AIS squared and added together to produce an ISS for the patient. An AIS of 6 (unsurvivable injury) always entailed an ISS of 75 (fatality)[9].
NOM was adopted for hemodynamically stable patients whose abdominal examination showed no peritoneal signs and whose imaging scans (X-ray, CT or ultrasonography) showed no intraperitoneal, retroperitoneal or extra-abdominal injuries requiring operative intervention. OM was indicated otherwise and when NOM failed.
All patients were closely monitored in the intensive care unit. Reassessment measures included physical examination, daily blood tests, and reassessment CT scan. Reassessment CT scan of the abdomen was performed 3 to 5 d after initial insult. CT scan for other regions was performed if necessary.
At the Department of Surgery, The University of Hong Kong, we have our own statistical staff. The biostatistics in this study was performed by our own statistical staff. The computer software SPSS, version 21.0, from IBM SPSS Statistics was used for statistical analyses. Continuous variables were compared by the Mann-Whitney U test and expressed as median with interquartile range. Student's t-test and Pearson’s χ2 test were employed. Thirty-day survival was measured. The Kaplan-Meier method was used for survival estimation and the log-rank test was used for survival comparison. Multivariate analysis was performed to identify the risks for mortality. P values < 0.05 were considered statistically significant.
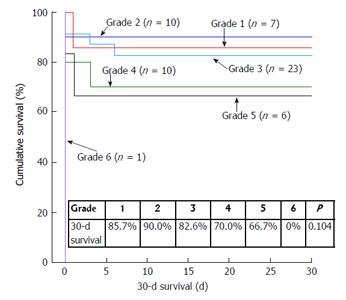
Fifty-eight patients were included in the study, with 23 patients in group 1 and 35 patients in group 2. Seven (30.4%) patients in group 1 and 10 (28.6%) patients in group 2 received NOM. No change in management plan occurred. The median age was 32 years in patients receiving NOM and 39 years in patients receiving OM (P = 0.140). Comparison of group 1 and group 2 is shown in Table 1. The amounts of blood loss in patients who received OM were similar in the two groups (300 mL vs 1250 mL, P = 0.133); the amounts of blood transfused were also similar (2700 mL vs 2880 mL, P = 0.799). However, significantly more patients in Group 2 required transfusion (70.6% vs 39.1%, P = 0.018). In the 58 patients, 48 (82.8%) suffered blunt trauma and 10 (17.2%) suffered penetrative trauma. Both group 1 and group 2 had road traffic accident as the commonest cause of injury. ISS (P < 0.0001) and hemodynamic stability (P = 0.036) were significantly different between the two groups. Group 1 had significantly better 30-d survival (91.3% vs 71.4%, P = 0.045), as shown in Figure 1. Figure 2 shows 30-d survival stratified by grade of liver injury (P = 0.104). On multivariate analysis using the logistic regression model, ISS was found to be associated with mortality (P = 0.004, hazard ratio = 1.035, 95%CI: 1.011-1.060) (Table 2).
| Group 1 (n = 23) | Group 2 (n = 35) | P value | |
| Age (yr) | 36 (4-79) | 36 (5-75) | 0.762 |
| Male:female | 16:7 | 23:12 | 0.760 |
| Health background | 0.208 | ||
| Good past health | 15 (65.2) | 28 (80.0) | |
| With comorbidity | 8 (34.8) | 7 (20.0) | |
| Type of trauma | 1 | ||
| Blunt | 19 (82.6) | 29 (82.9) | |
| Penetrative | 4 (17.4) | 6 (17.1) | |
| Mechanism of injury | 0.077 | ||
| Blunt injury | 5 (21.7) | 2 (5.7) | |
| Fall from a height | 2 (8.7) | 6 (17.1) | |
| Penetrative injury | 4 (17.4) | 3 (8.6) | |
| Road traffic accident | 9 (39.1) | 23 (65.7) | |
| Slip and fall | 3 (13.0) | 1 (2.9) | |
| With initial CT done | 17 (73.9) | 25 (71.4) | 1 |
| Reassessment CT | 0.367 | ||
| Not done | 8 (34.8) | 15 (42.9) | |
| Problem resolved | 15 (65.2) | 18 (51.4) | |
| Complication seen | 0 (0) | 2 (5.7) | |
| Hemodynamics | 0.036 | ||
| Stable | 15 (65.2) | 13 (37.1) | |
| Unstable | 8 (34.8) | 22 (62.9) | |
| Management | 0.879 | ||
| NOM | 7 (30.4) | 10 (28.6) | |
| OM | 16 (69.6) | 25 (71.4) | |
| Blood loss in OM (mL) | 300 (0-20000) | 1250 (0-24000) | 0.133 |
| Blood transfusion | 0.018 | ||
| No | 14 (60.9) | 10 (29.4) | |
| Yes | 9 (39.1) | 24 (70.6) | |
| Packed cells transfused (mL) | 0 (0-2390) | 1050 (0-10240) | 0.001 |
| Radiological intervention | 1 | ||
| No | 21 (91.3) | 30 (90.9) | |
| Yes | 2 (8.7) | 3 (9.1) | |
| ISS | 25 (16-75) | 45 (17-75) | < 0.0001 |
| Grade of liver injury1 | 0.354 | ||
| 1 | 4 (17.4) | 3 (8.8) | |
| 2 | 5 (21.8) | 5 (14.7) | |
| 3 | 11 (47.8) | 12 (35.3) | |
| 4 | 2 (8.7) | 8 (23.5) | |
| 5 | 1 (4.3) | 5 (14.7) | |
| 6 | 0 (0) | 1 (2.9) | |
| With complication | 4 (18.2) | 4 (11.4) | 0.747 |
| Follow-up duration (mo) | 6 (0-60) | 3 (0-128) | 0.339 |
| Dependent factor | |||
| Mortality | |||
| Variables put into the system for model selection | |||
| ISS | |||
| Location of injury (0: Liver only; 1: Liver and outside the liver) | |||
| Hemodynamics (0: Stable; 1: Unstable) | |||
| Variable remaining in the final logistic regression model | |||
| Factor | P | Hazard ratio | 95%CI |
| ISS | 0.004 | 1.035 | 1.011-1.060 |
The liver is the most commonly injured abdominal organ despite its well-protected position[1]. Management of liver injury depends on the patient’s condition, diagnosis, transfusion requirement and complications, as well as facilities for monitoring. NOM of liver injuries has gained wide support; it was adopted for approximately 60% of cases of liver injuries from low grades to high grades[8,10]. Its application has been extended to penetrative injuries[11].
At our center, liver trauma patients (with blunt or penetrative injuries) are subjected to CT for diagnostic purpose if they are hemodynamically stable; otherwise they are resuscitated and stabilized in the Accident and Emergency department, with a brief examination by a Focused Assessment with Sonography for Trauma scan, and then sent to the operation theater. Severity of injuries and presence of associated injuries are checked with CT or during laparotomy.
CT scan of the abdomen is widely used to evaluate intra-abdominal injuries in patients with stable hemodynamics; it should not be used if a patient has unstable hemodynamics since the patient’s condition may deteriorate rapidly during scanning. CT scan can present the precise grade of liver injury, thereby allowing formulation of a proper management plan. A high grade (Grade 3-5) represents relatively severe injury. Patients with a high grade of liver injury tend to be more unstable and require OM[12]. But NOM is becoming more applicable to these patients because of improvement in intensive clinical care and increased use of interventional radiology. If NOM is adopted, reassessment CT scan should be performed within 7 to 10 d after the initial CT scan to check if there are any delayed complications[5].
Grade of liver injury can reflect the degree of hepatic parenchymal damage, but it is not indicative of complication development or need for OM[13]. Grade-6 injuries are by definition not salvageable. In our present study, morbidity and mortality tended to worsen with a higher grade of liver injury. However, the presence of associated injuries also mattered; patients in group 2 with a high ISS fared the worst. Our 30-d survival curves by grade of liver injury reflected worsening survival with rising grades in both groups. However, further subgroup analysis showed that grade of liver injury did not make difference in survival (P = 0.104). In fact, if there are associated injuries outside the liver, grade of liver injury cannot reflect the overall severity of injuries.
Multiple injuries, which can be caused by more than one mechanism of injury, often lead to major trauma (or multi-trauma) and result in serious physical complications and physiological decompensation. Major trauma is defined as ISS > 15[14]. It is usually caused by a high impact of energy, and the commonest cause is road traffic accident[15]. The higher median ISS in group 2 was due to significant associated injuries outside the liver. And more patients in this group had transfusion need, a reflection of the severity of injury. It is not surprising that group 2 had a lower survival rate[16] as it has been reported that ISS could predict length of intensive care unit stay as well as mortality and survival[17]. Our multivariate analysis also found that patients with a higher ISS were more likely to have shorter survival.
Most of the patients who suffered blunt injuries in group 2 were unstable. At our center, the decision on management approach is based on individual patients’ clinical condition rather than ISS. Although ISS is used as an index for quality assurance at most trauma centers, it is not an accurate indicator and it does not reflect multiple injuries in the same body region. Hence, a high ISS should not be an indicator for OM. OM is required if a patient’s hemodynamics is unstable; it is also required in the presence of another operative indication (e.g., the need for thoracotomy, neurosurgery, orthopedic operation, repair of viscera, management of pelvic bleeding, etc). Decision on initial and subsequent management approaches should be based on clinical condition as well as mechanism and site of injury. Understanding the mechanism of the injury helps to identify potential life-threatening and limb-threatening conditions, which can maximize the chance of salvage and prevent functional deficit.
This study is not rid of the inherent limitations of a single-center retrospective study, and the patients were heterogeneous in terms of premorbid status, mechanism of injury and severity of injury. The use of ISS was to quantify severity of injuries for a more standardized representation.
In conclusion, liver trauma patients with multiple injuries are relatively unstable on presentation. Despite a significantly higher ISS in group 2, NOM was possible for selected patients. Associated injuries outside the liver usually account for morbidity and mortality.
In liver trauma management, the widespread use of ultrasonography and computed tomography (CT) has facilitated decision-making, and non-operative management (NOM) has been shown to reduce mortality. NOM is now the standard of care for blunt liver injury in hemodynamically stable patients.
This study reviewed the management of liver trauma with or without associated injuries over 10 years at a level-1 trauma center in Hong Kong.
Liver trauma patients with multiple injuries are relatively unstable on presentation. Despite a significantly higher injury severity score in group 2, NOM was possible for selected patients. Associated injuries outside the liver usually account for morbidity and mortality.
It is well written and documented and discussed paper, it has valuable points to stress the nonoperative management of liver trauma in addition to that on behalf of the scope of your journal this type of articles may increase the impact effect of it since the paper is discussed a huge number of cases even they collected them in 10 years but it is meaningful and it likes a review of liver trauma.
P- Reviewer: Guneren E, Ximenes RO S- Editor: Qi Y L- Editor: A E- Editor: Liu SQ
| 1. | Feliciano DV. Surgery for liver trauma. Surg Clin North Am. 1989;69:273-284. [PubMed] |
| 2. | David Richardson J, Franklin GA, Lukan JK, Carrillo EH, Spain DA, Miller FB, Wilson MA, Polk HC, Flint LM. Evolution in the management of hepatic trauma: a 25-year perspective. Ann Surg. 2000;232:324-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 228] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 3. | Croce MA, Fabian TC, Menke PG, Waddle-Smith L, Minard G, Kudsk KA, Patton JH, Schurr MJ, Pritchard FE. Nonoperative management of blunt hepatic trauma is the treatment of choice for hemodynamically stable patients. Results of a prospective trial. Ann Surg. 1995;221:744-753; discussion 753-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 351] [Cited by in RCA: 323] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 4. | Meredith JW, Young JS, Bowling J, Roboussin D. Nonoperative management of blunt hepatic trauma: the exception or the rule? J Trauma. 1994;36:529-534; discussion 534-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 143] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 5. | Pachter HL, Hofstetter SR. The current status of nonoperative management of adult blunt hepatic injuries. Am J Surg. 1995;169:442-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 125] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 6. | Malhotra AK, Fabian TC, Croce MA, Gavin TJ, Kudsk KA, Minard G, Pritchard FE. Blunt hepatic injury: a paradigm shift from operative to nonoperative management in the 1990s. Ann Surg. 2000;231:804-813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 201] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 7. | Coimbra R, Hoyt DB, Engelhart S, Fortlage D. Nonoperative management reduces the overall mortality of grades 3 and 4 blunt liver injuries. Int Surg. 2006;91:251-257. [PubMed] |
| 8. | Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA, Champion HR. Organ injury scaling: spleen and liver (1994 revision). J Trauma. 1995;38:323-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 872] [Cited by in RCA: 762] [Article Influence: 25.4] [Reference Citation Analysis (0)] |
| 9. | Baker SP, O’Neill B, Haddon W, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5970] [Cited by in RCA: 5975] [Article Influence: 117.2] [Reference Citation Analysis (0)] |
| 10. | Cachecho R, Clas D, Gersin K, Grindlinger GA. Evolution in the management of the complex liver injury at a Level I trauma center. J Trauma. 1998;45:79-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Petrowsky H, Raeder S, Zuercher L, Platz A, Simmen HP, Puhan MA, Keel MJ, Clavien PA. A quarter century experience in liver trauma: a plea for early computed tomography and conservative management for all hemodynamically stable patients. World J Surg. 2012;36:247-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Tinkoff G, Esposito TJ, Reed J, Kilgo P, Fildes J, Pasquale M, Meredith JW. American Association for the Surgery of Trauma Organ Injury Scale I: spleen, liver, and kidney, validation based on the National Trauma Data Bank. J Am Coll Surg. 2008;207:646-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 236] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 13. | Becker CD, Gal I, Baer HU, Vock P. Blunt hepatic trauma in adults: correlation of CT injury grading with outcome. Radiology. 1996;201:215-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 45] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Keel M, Trentz O. Pathophysiology of polytrauma. Injury. 2005;36:691-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 613] [Cited by in RCA: 573] [Article Influence: 28.7] [Reference Citation Analysis (0)] |
| 15. | von Rüden C, Woltmann A, Röse M, Wurm S, Rüger M, Hierholzer C, Bühren V. Outcome after severe multiple trauma: a retrospective analysis. J Trauma Manag Outcomes. 2013;7:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 16. | Pracht E. Inpatient hospital outcomes following injury in Suriname: lessons for prevention. Glob Health Promot. 2014;21:29-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Akhavan Akbari G, Mohammadian A. Comparison of the RTS and ISS scores on prediction of survival chances in multiple trauma patients. Acta Chir Orthop Traumatol Cech. 2012;79:535-539. [PubMed] |