Published online Dec 18, 2015. doi: 10.4254/wjh.v7.i29.2890
Peer-review started: May 5, 2015
First decision: June 25, 2015
Revised: November 9, 2015
Accepted: December 1, 2015
Article in press: December 2, 2015
Published online: December 18, 2015
Processing time: 225 Days and 21.6 Hours
Biliary complications (BC) currently represent a major source of morbidity after liver transplantation. Although refinements in surgical technique and medical therapy have had a positive influence on the reduction of postoperative morbidity, BC affect 5% to 25% of transplanted patients. Bile leak and anastomotic strictures represent the most common complications. Nowadays, a multidisciplinary approach is required to manage such complications in order to prevent liver failure and retransplantation.
Core tip: Biliary complications (BC) represent the downside of liver transplantation, impacting postoperative morbidity as well as patient and graft survival. In this paper, we will analyze the most common BC, along with diagnosis, management and treatment modalities.
- Citation: Memeo R, Piardi T, Sangiuolo F, Sommacale D, Pessaux P. Management of biliary complications after liver transplantation. World J Hepatol 2015; 7(29): 2890-2895
- URL: https://www.wjgnet.com/1948-5182/full/v7/i29/2890.htm
- DOI: https://dx.doi.org/10.4254/wjh.v7.i29.2890
Liver transplantation (LT) is the standard of care for end-stage liver disease. Although LT can currently be considered as a consolidate procedure and various refinements in surgical techniques are required, organ preservation and immunosuppressive management have reduced complications and contribute to better outcomes[1], biliary complications (BC) remain the main downside of this procedure, affecting 5% to 25% of transplanted patients[2]. The most common causes of BC are bile leakage, anastomotic and non-anastomotic strictures, and bile duct obstruction. According to the literature[3-8], the main risk factors are technical complications, ischemia/reperfusion injury, ABO mismatch, hepatic artery complications (thrombosis and stenosis), donor age and cytomegalovirus infection. The aim of this article is to review and focus on the treatment of BC after LT.
Two different types of biliary anastomoses can be performed in LT: Duct-to-duct (DD) and hepatojejunostomy (HJ). Different factors determine the choice of biliary reconstruction. In most cases, a DD anastomosis is preferred (90% of deceased donor LT[9,10] and 60% in living donor LT[11] due to its simpler technical feasibility, preserved function of Oddi’s sphincter, and endoscopic access preservation. In the literature, two kinds of DD anastomoses have been described: End-to-end and side-to-side. Davidson et al[12] have described an equal effectiveness of both reconstructions. HJ is preferred in case of size disparity between donor and recipient bile duct, recipient diseased duct or previous transplant or biliary surgery. In addition to the type of reconstruction, no evidence has been demonstrated regarding the suturing method (interrupted or continuous[13]) or materials. However, an inadequate surgical technique can be responsible for BC[14]. A T tube was routinely used after DD anastomosis to reduce the incidence of BC. Most retrospective studies cannot conclude in favor of the use of a T tube[15], and some of them point towards a potential negative effect[16-18] on anastomosis. Recently, a meta-analysis[19] including six prospective randomized trials demonstrated no benefit in terms of T tube, and consequently it could not be recommended.
The onset modality of BCs varied. In the presence of pain, abnormal liver function tests, increased levels of inflammatory markers, fever, and bilious secretion in the abdominal drain, further radiological examinations were necessary. In case of ongoing clinical suspicion, cholangiography remains the gold standard for the exploration of BCs. In the presence of a T tube, a simple cholangiography could reveal the origin of BCs. If a T tube is not used, endoscopic retrograde cholangiopancreatography (ERCP) is the method of choice in case of DD anastomosis. In case of HJ anastomosis, percutaneous transhepatic cholangiography is the first-line diagnostic exam. Recently, magnetic resonance cholangiopancreatography has guaranteed a good sensitivity and specificity in order to prevent invasive exploration. Ultrasonography may be helpful to detect the presence of biloma, biliary tree dilatation, and to explore all vascular anastomoses by means of a Doppler examination. Further procedures such as liver biopsy could be necessary in case of suspected graft dysfunction.
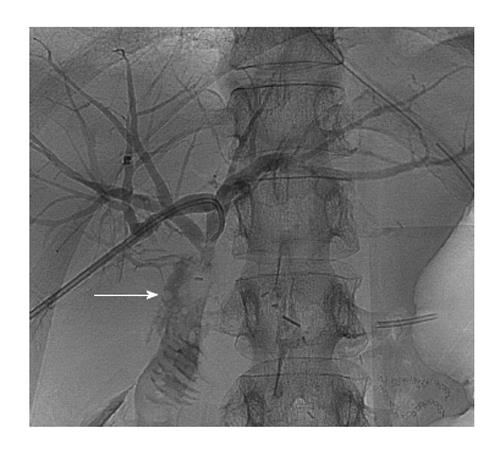
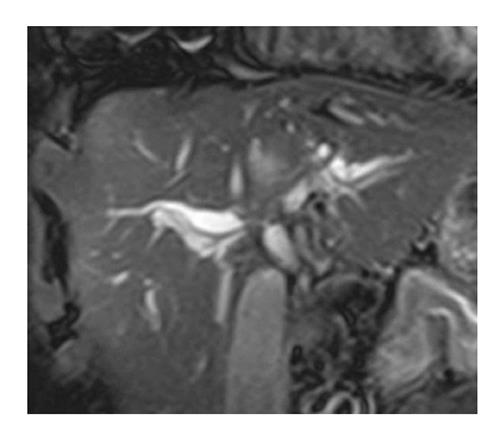
BC can be divided into several categories which are anastomotic leak (Figure 1), biliary strictures (Figure 2), non-anastomotic strictures (Figure 3), and biliary obstruction (stones, sludge and cast). Each complication usually occurs in different postoperative periods and requires different management options.
Anastomotic leaks: Bile leaks occur in 5% to 10% of deceased donor LT[20] and in 10% to 15% of living donor LT[21]. They can occur during the anastomosis, at T tube insertion, on the cystic duct stump and on the cut surface in case of partial graft. Early postoperative leak can be identified. They usually occur within one month after LT. Late bile leaks[22] rarely occur. In the early postoperative period, bile leak can originate directly from the anastomosis, and it is most likely due to technical problems or insufficient arterial bile duct vascularization. Other rare causes of bile leak are due to an incorrect suture of the cystic duct stump and may originate from the resection surface in case of living donor or split liver. In particular, caudate lobe biliary branches, which usually drain in the left liver are sometimes drained in the right liver, increasing the risk of leak either in donors or recipients[20,23]. Late bile leaks are related to T tube[24] removal in nearly 1% of cases, with a fistula arising directly from the insertion site. In some cases, especially in case of early accidental T tube removal, a biliary peritonitis can occur, due to the incomplete T tube tract scarring.
Biliary strictures: As described in the literature, biliary strictures represent a complication which can occur in 13% in deceased donor LT and in 19% in in living donor LT[9]. Biliary strictures can be divided into two categories, i.e., anastomotic strictures and non-anastomotic strictures. The main cause responsible for anastomotic strictures can be inadequate anastomoses, usually occurring in the early postoperative period and inflammatory strictures due to ischemic events or biliary fistulas. The mechanism of non-anastomotic strictures remains unclear, but it is often related to ischemic events. Non-anastomotic strictures are present in the entire biliary tree, especially in the hilum. Non-anastomotic strictures, also called ischemic cholangiopathies, can be caused by long-lasting cold ischemia times[25]. Generally, biliary strictures are considered as late complications, occurring within 6 mo[26,27] after LT, even though some cases may occur later, especially when associated with ischemic cholangitis for arterial thrombosis[28] or immunologic disorders[29].
Other complications: Bile leaks and anastomotic strictures represent the main BC. Liver test perturbation may be due to other causes. Outflow bile duct obstruction can be caused by Oddi’s sphincter dysfunction, as described in about 2% to 7% of patients[30]. It is often associated with a stump denervation of the recipient bile duct or with a chronic sphincter inflammation. Other causes of bile duct dilatation can be stones, sludge or cast. The formation of stones is often due to an underlying stenosis which induces an increased bile viscosity, occurring in 3% to 12% of cases[31]. Sludge is like a mixture of particles precipitated from the bile, often composed of cholesterol and calcium salt which generates a progressive bile duct lumen obstruction in 2% of cases[32]. Damage (ischemia, rejection, infection, obstruction) of the biliary tree mucosa can provoke a cast syndrome, defined as the presence of cast (desquamated epithelial cells mixed with bile products) within the intrahepatic and extrahepatic biliary system. Its incidence varies from 3% to 18% in the literature[33]. Mucoceles, an uncommon complication after LT occurring in 2% of patients[34], are defined as a collection of mucus present in the remnant cystic duct. This abnormal dilatation can cause extrinsic compression on the bile duct.
Even if its role is still debated[35], the T tube can be a useful tool for a rapid diagnosis of bile leak in case of early postoperative bile leak. A T tube cholangiogram could be used diagnostically and a simple drainage through the tube opening could be therapeutic, preventing any invasive treatment. Without the use of a T tube, endoscopic treatment is the standard of care[22,36,37]. A simple sphincterotomy could be therapeutic in case of small bile leak[38]. An endoscopic stent could be necessary for major bile leaks, with a short-term removal[27] of the prosthesis in case of successful treatment. In case of HJ anastomosis, in case of endoscopic treatment failure (even if expert teams substantiate the use of double-balloon enteroscopy[39]), transhepatic percutaneous[40] treatment becomes an alternative. Although percutaneous transanastomotic internal-external drainage guarantees good postoperative results, it is technically difficult due to the absence of leak-induced bile duct dilatation. Re-operation and re-transplantation[9] for bile leak, although described in the literature, become increasingly anecdotal due to improvements in radiology and endoscopy.
Biliary strictures are usually classified into anastomotic strictures and non-anastomotic strictures. Anastomotic strictures usually involve the anastomotic site whereas non-anastomotic strictures could be multiple and present either in the hilum and in the intrahepatic portion of the bile duct, with a guarded prognosis as compared to anastomotic strictures[41]. Concerning anastomotic strictures, the treatment aims to dilate the stenotic segment. Considering the access route, endoscopy is preferred to the percutaneous approach[42] due to a reduced morbidity, better efficacy, and increased comfort for the patient[43]. Endoscopic treatment, performed via ERCP, consists of sphincterotomy and several sessions of dilatation followed by placement of a plastic stent. Some studies compared simple balloon dilatation to balloon dilatation and simultaneous plastic stent placement, showing a lower recurrence rate and requiring fewer sessions in combined treatment[44,45]. The success rate of treatment is approximately 75%[45,46]. Multiple sessions are usually performed bimonthly and could be necessary to obtain satisfying results[47,48]. The necessity of a repetitive approach, entailed the increased use of metallic stents, which can achieve a higher diameter and develop less obstruction as compared to plastic stents. This concept is theoretically correct but has not found practical evidence neither with the use of partially nor fully covered stents as compared to plastic stents[41]. The percutaneous approach, mostly used in case of HJ anastomosis, guarantees goods results in terms of success and recurrence rates[29]. In case of endoscopic/percutaneous treatment failure, surgery represents a valid treatment alternative, considering the effect of prolonged biliary obstruction on liver function. Surgical revision was necessary in 10% to 20% of cases with anastomotic stricture[29].
Early arterial thrombosis represents the main risk factor for non-anastomotic strictures. Thrombosis associated with the absence of arterial collateral perfusion (otherwise present in late arterial thrombosis) is strongly associated with non-anastomotic strictures in 50% of cases[14]. Early detection could well reduce the rate of retransplantation[28], requiring a rapid revascularization in order to prevent graft loss. Ischemic-type lesions are difficult to manage, especially in case of multiple intrahepatic strictures. Medical treatment can be attempted, even if not evidence-based, with the use of ursodesoxicolic acid to increase bile flow and reduce lithogenicity. Considering the frequent association with cholangitis, a large use of antibiotic therapy and prophylaxis is often necessary[49]. Endoscopic treatment with multiple stent placement for non-anastomotic strictures usually requires long-term stenting, and despite encouraging results described in the literature[48,49], 30% to 50% of patients undergo re-transplantation[22,27,49] due to the progressive onset of liver dysfunction caused by chronic biliary cirrhosis. An immunomediate mechanism is responsible for late (> 1 year) non-anastomotic strictures[50,51], requiring the same management of ischemia-mediated strictures.
Most other pathological conditions are related to a difficult bile duct emptying. On radiological findings, they can be identified as common bile duct filling defects. Different causes contribute to this dysfunction, arising from the presence of stones, sludge, cast syndrome or cystic duct mucoceles[52]. Most of these complications are treated using an endoscopic approach, consisting of sphincterotomy and ERCP with balloon dilatation and basket extraction. In case of endoscopic treatment failure, surgery represents a valid alternative.
P- Reviewer: Kobayashi A S- Editor: Song XX L- Editor: A E- Editor: Liu SQ
| 1. | Adam R, Karam V, Delvart V, O’Grady J, Mirza D, Klempnauer J, Castaing D, Neuhaus P, Jamieson N, Salizzoni M. Evolution of indications and results of liver transplantation in Europe. A report from the European Liver Transplant Registry (ELTR). J Hepatol. 2012;57:675-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 606] [Cited by in RCA: 643] [Article Influence: 49.5] [Reference Citation Analysis (2)] |
| 2. | Gastaca M. Biliary complications after orthotopic liver transplantation: a review of incidence and risk factors. Transplant Proc. 2012;44:1545-1549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 81] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 3. | Memeo R, de’Angelis N, Salloum C, Compagnon P, Laurent A, Feray C, Duvoux C, Azoulay D. Clinical outcomes of right-lobe split-liver versus orthotopic liver transplants from donors more than 70 years old. Prog Transplant. 2015;25:243-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Seehofer D, Eurich D, Veltzke-Schlieker W, Neuhaus P. Biliary complications after liver transplantation: old problems and new challenges. Am J Transplant. 2013;13:253-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 215] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 5. | Yuan D, Wei YG, Lin HM, Li FQ, Yang M, Liu XL, Li B, Yan LN, Zeng Y, Wen TF. Risk factors of biliary complications following liver transplantation: retrospective analysis of a single centre. Postgrad Med J. 2009;85:119-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Qian YB, Liu CL, Lo CM, Fan ST. Risk factors for biliary complications after liver transplantation. Arch Surg. 2004;139:1101-1105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 124] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 7. | Ayoub WS, Esquivel CO, Martin P. Biliary complications following liver transplantation. Dig Dis Sci. 2010;55:1540-1546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 82] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 8. | Duailibi DF, Ribeiro MA. Biliary complications following deceased and living donor liver transplantation: a review. Transplant Proc. 2010;42:517-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 9. | Akamatsu N, Sugawara Y, Hashimoto D. Biliary reconstruction, its complications and management of biliary complications after adult liver transplantation: a systematic review of the incidence, risk factors and outcome. Transpl Int. 2011;24:379-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 275] [Cited by in RCA: 247] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 10. | Sharma S, Gurakar A, Jabbour N. Biliary strictures following liver transplantation: past, present and preventive strategies. Liver Transpl. 2008;14:759-769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 275] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 11. | Zhang S, Zhang M, Xia Q, Zhang JJ. Biliary reconstruction and complications in adult living donor liver transplantation: systematic review and meta-analysis. Transplant Proc. 2014;46:208-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Davidson BR, Rai R, Kurzawinski TR, Selves L, Farouk M, Dooley JS, Burroughs AK, Rolles K. Prospective randomized trial of end-to-end versus side-to-side biliary reconstruction after orthotopic liver transplantation. Br J Surg. 1999;86:447-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 62] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 13. | Castaldo ET, Pinson CW, Feurer ID, Wright JK, Gorden DL, Kelly BS, Chari RS. Continuous versus interrupted suture for end-to-end biliary anastomosis during liver transplantation gives equal results. Liver Transpl. 2007;13:234-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 34] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Koneru B, Sterling MJ, Bahramipour PF. Bile duct strictures after liver transplantation: a changing landscape of the Achilles’ heel. Liver Transpl. 2006;12:702-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 79] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 15. | Riediger C, Müller MW, Michalski CW, Hüser N, Schuster T, Kleeff J, Friess H. T-Tube or no T-tube in the reconstruction of the biliary tract during orthotopic liver transplantation: systematic review and meta-analysis. Liver Transpl. 2010;16:705-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Randall HB, Wachs ME, Somberg KA, Lake JR, Emond JC, Ascher NL, Roberts JP. The use of the T tube after orthotopic liver transplantation. Transplantation. 1996;61:258-261. [PubMed] |
| 17. | Ferraz-Neto BH, Mirza DF, Gunson BK, Ismail T, Mayer AD, Buckels JA, McMaster P. Bile duct splintage in liver transplantation: is it necessary? Transpl Int. 1996;9 Suppl 1:S185-S187. [PubMed] |
| 18. | Pratschke J, Weiss S, Neuhaus P, Pascher A. Review of nonimmunological causes for deteriorated graft function and graft loss after transplantation. Transpl Int. 2008;21:512-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 43] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 19. | Sun N, Zhang J, Li X, Zhang C, Zhou X, Zhang C. Biliary tract reconstruction with or without T-tube in orthotopic liver transplantation: a systematic review and meta-analysis. Expert Rev Gastroenterol Hepatol. 2015;9:529-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 20. | Kapoor VK. Bile duct injury repair - earlier is not better. Front Med. 2015;Epub ahead of print. [PubMed] |
| 21. | Iida T, Ogura Y, Oike F, Hatano E, Kaido T, Egawa H, Takada Y, Uemoto S. Surgery-related morbidity in living donors for liver transplantation. Transplantation. 2010;89:1276-1282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 103] [Article Influence: 6.9] [Reference Citation Analysis (1)] |
| 22. | Londoño MC, Balderramo D, Cárdenas A. Management of biliary complications after orthotopic liver transplantation: the role of endoscopy. World J Gastroenterol. 2008;14:493-497. [PubMed] |
| 23. | Jassem W, Heaton ND, Rela M. Reducing bile leak following segmental liver transplantation: understanding biliary anatomy of the caudate lobe. Am J Transplant. 2008;8:271-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Gastaca M, Matarranz A, Muñoz F, Valdivieso A, Aguinaga A, Testillano M, Bustamante J, Terreros I, Suarez MJ, Montejo M. Biliary complications in orthotopic liver transplantation using choledochocholedochostomy with a T-tube. Transplant Proc. 2012;44:1554-1556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 25. | Sanchez-Urdazpal L, Gores GJ, Ward EM, Maus TP, Wahlstrom HE, Moore SB, Wiesner RH, Krom RA. Ischemic-type biliary complications after orthotopic liver transplantation. Hepatology. 1992;16:49-53. [PubMed] |
| 26. | Mahajani RV, Cotler SJ, Uzer MF. Efficacy of endoscopic management of anastomotic biliary strictures after hepatic transplantation. Endoscopy. 2000;32:943-949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 67] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 27. | Thuluvath PJ, Pfau PR, Kimmey MB, Ginsberg GG. Biliary complications after liver transplantation: the role of endoscopy. Endoscopy. 2005;37:857-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 153] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 28. | Memeo R, Ciacio O, Pittau G, Cherqui D, Castaing D, Adam R, Vibert E. Systematic computer tomographic scans 7 days after liver transplantation surgery can lower rates of repeat-transplantation due to arterial complications. Transplant Proc. 2014;46:3536-3542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Verdonk RC, Buis CI, Porte RJ, van der Jagt EJ, Limburg AJ, van den Berg AP, Slooff MJ, Peeters PM, de Jong KP, Kleibeuker JH. Anastomotic biliary strictures after liver transplantation: causes and consequences. Liver Transpl. 2006;12:726-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 235] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 30. | Gholson CF, Zibari G, McDonald JC. Endoscopic diagnosis and management of biliary complications following orthotopic liver transplantation. Dig Dis Sci. 1996;41:1045-1053. [PubMed] |
| 31. | Thuluvath PJ, Atassi T, Lee J. An endoscopic approach to biliary complications following orthotopic liver transplantation. Liver Int. 2003;23:156-162. [PubMed] |
| 32. | Gor NV, Levy RM, Ahn J, Kogan D, Dodson SF, Cohen SM. Biliary cast syndrome following liver transplantation: Predictive factors and clinical outcomes. Liver Transpl. 2008;14:1466-1472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 54] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 33. | Shah JN, Haigh WG, Lee SP, Lucey MR, Brensinger CM, Kochman ML, Long WB, Olthoff K, Shaked A, Ginsberg GG. Biliary casts after orthotopic liver transplantation: clinical factors, treatment, biochemical analysis. Am J Gastroenterol. 2003;98:1861-1867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 75] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 34. | Caputo M, Piolanti M, Riccioli LA, Pazienza L, Fabbro E, Gruppioni F, Grazi G, Gavelli G. [Nonobstructive residual mucocele of the cystic duct. Reassessment of complications in our 13 years’ experience with liver transplantation]. Radiol Med. 2000;100:354-356. [PubMed] |
| 35. | Sankarankutty AK, Mente ED, Cardoso NM, Castro-E-Silva O. T-tube or no T-tube for bile duct anastomosis in orthotopic liver transplantation. Hepatobiliary Surg Nutr. 2013;2:171-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 36. | Rossi AF, Grosso C, Zanasi G, Gambitta P, Bini M, De Carlis L, Rondinara G, Arcidiacono R. Long-term efficacy of endoscopic stenting in patients with stricture of the biliary anastomosis after orthotopic liver transplantation. Endoscopy. 1998;30:360-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 67] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 37. | Sanna C, Saracco GM, Reggio D, Moro F, Ricchiuti A, Strignano P, Mirabella S, Ciccone G, Salizzoni M. Endoscopic retrograde cholangiopancreatography in patients with biliary complications after orthotopic liver transplantation: outcomes and complications. Transplant Proc. 2009;41:1319-1321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 38. | Llach J, Bordas JM, Elizalde JI, Enrico C, Ginès A, Pellisé M, Mondelo F, Piqué JM. Sphincterotomy in the treatment of biliary leakage. Hepatogastroenterology. 2012;49:1496-1498. [PubMed] |
| 39. | Gutierrez JP, Smith IB, Wilcox CM, Mönkemüller K. Bile leak from the duct of Luschka treated with double-balloon enteroscopy ERCP in a patient with Roux-en-Y gastric bypass. Endoscopy. 2013;45 Suppl 2 UCTN:E404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 40. | de Jong EA, Moelker A, Leertouwer T, Spronk S, Van Dijk M, van Eijck CH. Percutaneous transhepatic biliary drainage in patients with postsurgical bile leakage and nondilated intrahepatic bile ducts. Dig Surg. 2013;30:444-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 41. | Nacif LS, Bernardo WM, Bernardo L, Andraus W, Torres L, Chaib E, D’Albuquerque LC, Maluf-Filho F. Endoscopic treatment of post-liver transplantation anastomotic biliary stricture: systematic review and meta-analysis. Arq Gastroenterol. 2014;51:240-249. [PubMed] |
| 42. | Piardi T, Greget M, Audet M, Calandra G, Gheza F, Ellero B, Woehl-Jaegle ML, Cantu M, Portolani N, Wolf P. Biliary strictures after liver transplantation: is percutaneous treatment indicated? Ann Transplant. 2015;16:5-13. [PubMed] |
| 43. | Lee SH, Ryu JK, Woo SM, Park JK, Yoo JW, Kim YT, Yoon YB, Suh KS, Yi NJ, Lee JM. Optimal interventional treatment and long-term outcomes for biliary stricture after liver transplantation. Clin Transplant. 2015;22:484-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 44. | Zoepf T, Maldonado-Lopez EJ, Hilgard P, Malago M, Broelsch CE, Treichel U, Gerken G. Balloon dilatation vs. balloon dilatation plus bile duct endoprostheses for treatment of anastomotic biliary strictures after liver transplantation. Liver Transpl. 2006;12:88-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 128] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 45. | Kulaksiz H, Weiss KH, Gotthardt D, Adler G, Stremmel W, Schaible A, Dogan A, Stiehl A, Sauer P. Is stenting necessary after balloon dilation of post-transplantation biliary strictures? Results of a prospective comparative study. Endoscopy. 2008;40:746-751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 46. | Park JS, Kim MH, Lee SK, Seo DW, Lee SS, Han J, Min YI, Hwang S, Park KM, Lee YJ. Efficacy of endoscopic and percutaneous treatments for biliary complications after cadaveric and living donor liver transplantation. Gastrointest Endosc. 2003;57:78-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 161] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 47. | Tashiro H, Itamoto T, Sasaki T, Ohdan H, Fudaba Y, Amano H, Fukuda S, Nakahara H, Ishiyama K, Ohshita A. Biliary complications after duct-to-duct biliary reconstruction in living-donor liver transplantation: causes and treatment. World J Surg. 2007;31:2222-2229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 73] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 48. | Kochar K, Vallance K, Mathew G, Jadhav V. Intrahepatic perforation of the gall bladder presenting as liver abscess: case report, review of literature and Niemeier’s classification. Eur J Gastroenterol Hepatol. 2008;20:240-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 49. | Verdonk RC, Buis CI, van der Jagt EJ, Gouw AS, Limburg AJ, Slooff MJ, Kleibeuker JH, Porte RJ, Haagsma EB. Nonanastomotic biliary strictures after liver transplantation, part 2: Management, outcome, and risk factors for disease progression. Liver Transpl. 2007;13:725-732. [PubMed] |
| 50. | Guichelaar MM, Benson JT, Malinchoc M, Krom RA, Wiesner RH, Charlton MR. Risk factors for and clinical course of non-anastomotic biliary strictures after liver transplantation. Am J Transplant. 2003;3:885-890. [PubMed] |
| 51. | Buis CI, Verdonk RC, Van der Jagt EJ, van der Hilst CS, Slooff MJ, Haagsma EB, Porte RJ. Nonanastomotic biliary strictures after liver transplantation, part 1: Radiological features and risk factors for early vs. late presentation. Liver Transpl. 2007;13:708-718. [PubMed] |
| 52. | Piardi T, Panaro F, Gheza F, Wolf P. ‘Cystic’ lesion in the porta hepatis after liver transplantation. Liver Int. 2011;31:859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |