Published online Apr 27, 2022. doi: 10.4254/wjh.v14.i4.860
Peer-review started: January 10, 2022
First decision: January 22, 2022
Revised: January 22, 2022
Accepted: March 6, 2022
Article in press: March 6, 2022
Published online: April 27, 2022
Processing time: 101 Days and 11.8 Hours
Primary hepatic leiomyosarcoma is a very rare entity that originates from smooth muscle. Preoperative diagnosis requires a high degree of suspicion due to atypical clinical presentation and non-specific imaging features.
We report the case of a 42-year-old man, with no relevant past medical history, accidentally diagnosed with a nodular liver lesion on a routine abdominal ultrasound. Liver function tests and hematology parameters as well as tumor markers were normal. A contrast-enhanced abdominal computed tomography scan revealed a heterogenous hepatic lesion measuring 40 mm 30 mm, adjacent to the left branch of the portal vein and the round ligament. Due to the unclear diagnosis, the patient underwent surgical resection. Histopathological and immunohistochemical examinations confirmed complete (R0) resection of a hepatic leiomyosarcoma. The patient remains without any signs of tumor recurrence for more than 2 years.
We report a rare case of accidentally diagnosed primary hepatic leiomyosarcoma originating from the portal vein or the round ligament. Although this tumor has aggressive metastatic potential, a tumor-free resection margin is essential to improve survival.
Core Tip: Sarcomas comprise only 1%-2% of all primary liver malignancies, and leiomyosarcoma is even rarer. We report a rare case of primary hepatic leiomyosarcoma accidentally diagnosed and surgically treated. The diagnosis requires a high level of suspicion because the clinical scenario and cross-imaging are not specific. Thus, histological examination is the only way to reach the diagnosis. In our case, the tumor probably originated from the left branch of the portal vein or the round ligament. Radical hepatectomy is the cornerstone of treatment. However, this tumor has aggressive metastatic potential and is usually diagnosed in locally advanced or metastatic disease. Two years after surgical resection, our patient is alive and with no evidence of tumor recurrence, likely because the diagnosis was established at an early stage and the surgery achieved a tumor-free margin.
- Citation: Garrido I, Andrade P, Pacheco J, Rios E, Macedo G. Not all liver tumors are alike — an accidentally discovered primary hepatic leiomyosarcoma: A case report. World J Hepatol 2022; 14(4): 860-865
- URL: https://www.wjgnet.com/1948-5182/full/v14/i4/860.htm
- DOI: https://dx.doi.org/10.4254/wjh.v14.i4.860
Sarcomas comprise only 1%-2% of all primary liver malignancies, and leiomyosarcoma is even rarer[1]. In the vast majority of cases of primary hepatic leiomyosarcoma, the tumor originates in the inferior vena cava. Clinical presentation and imaging features are non-specific and can mimic the most frequent primary liver tumors, namely hepatocellular carcinoma and intrahepatic cholangiocarcinoma. This tumor has aggressive metastatic potential and is usually diagnosed in a locally advanced or metastatic disease[2]. We report a rare case of primary hepatic leiomyosarcoma originating from the portal vein or the round ligament, accidentally diagnosed and surgically treated.
The patient was asymptomatic.
A 42-year-old man was referred for gastroenterology consultation due to a nodular hepatic lesion identified in a routine abdominal ultrasound.
Healthy, with no specific diseases.
There was no family history of liver disease.
There were no relevant changes on physical examination.
Liver tests were normal. The metabolic, virological and autoimmune study was negative. Alpha-fetoprotein and cancer antigen 19-9 were also normal.
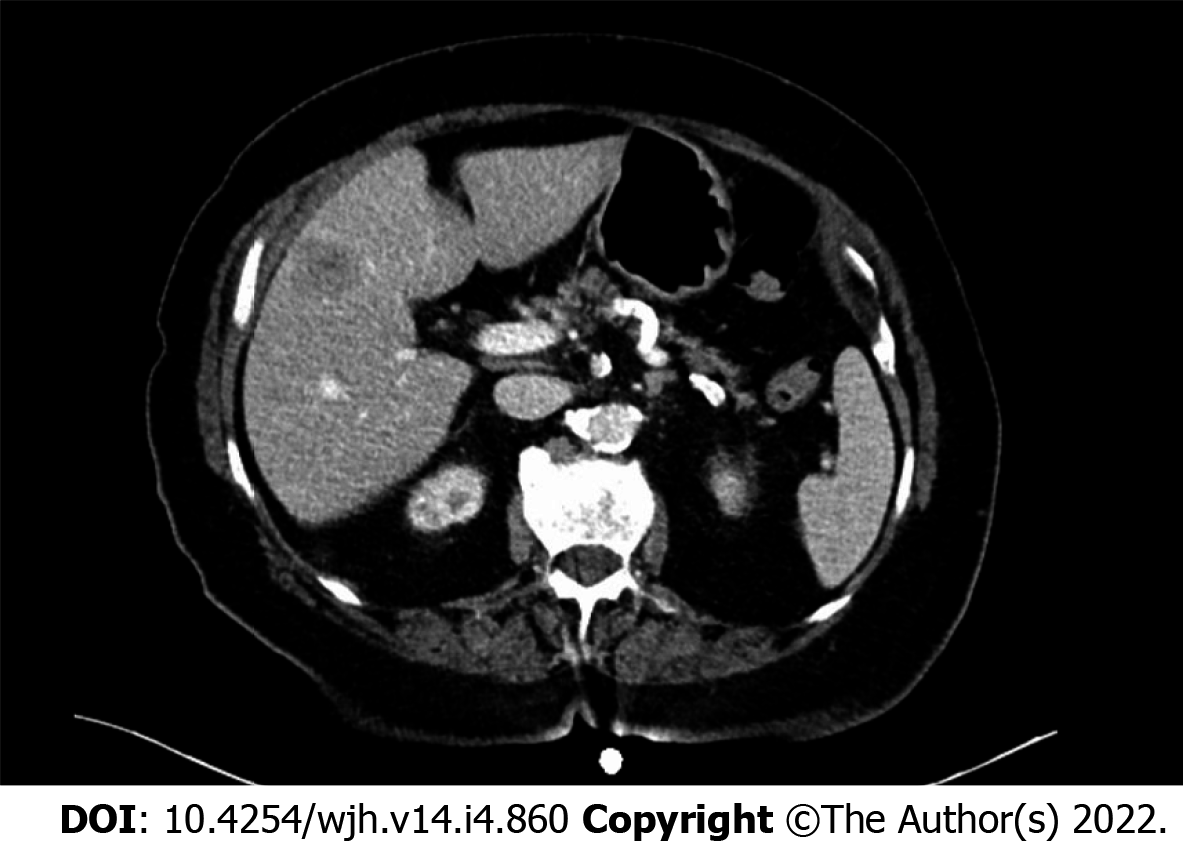
A contrast-enhanced abdominal computed tomography scan was performed, revealing a nodular hepatic lesion measuring 40 mm × 30 mm, adjacent to the left branch of the portal vein, in the transition from the right to the left lobe (Figure 1). The tumor was contrast-enhancing, with heterogeneous areas inside.
The imaging characteristics did not allow for a categorical distinction between hydatid cyst or other etiology. Therefore, it was decided at the multidisciplinary team meeting to perform surgical resection.
In the explored laparoscopy, an exophytic lesion in segment IV was identified, involving the left branch of the portal vein and the round ligament; non-anatomic resection was performed without complications.
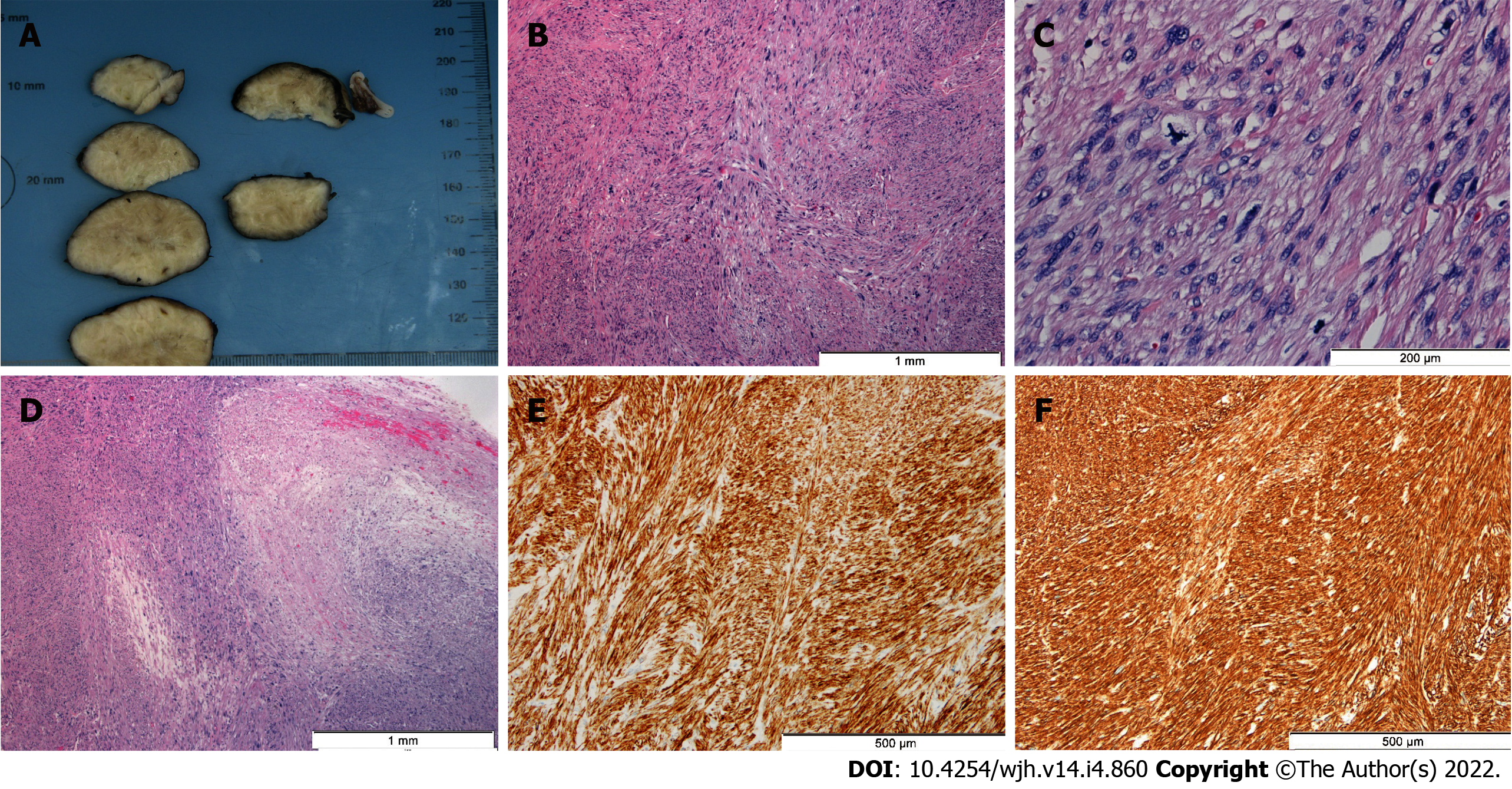
Histological examination showed complete resection of malignant mesenchymal neoplasia consisting of spindle cells with nuclei elongated to ovoid, with atypia and marked pleomorphism (Figure 2). In the immunohistochemical study, diffuse expression of actin and desmin was observed in neoplastic cells, in the absence of S100 expression. A chest-abdomen-pelvis computed tomography scan was performed in the postoperative period, with no evidence of residual or metastatic lesions. Moreover, this examination made it clear that it was a primary lesion. Thus, primary hepatic leiomyosarcoma was diagnosed with origin in the portal vein wall or the round ligament.
The patient remained under clinical surveillance. Two years after surgery, he is asymptomatic, with no evidence of tumor recurrence.
Primary hepatic leiomyosarcoma is a rare type of liver sarcoma; so far, less than 100 cases have been reported in the literature. Its diagnosis requires a high level of suspicion because the clinical scenario and cross-imaging are not specific[3]. In fact, patients are often asymptomatic or their symptoms are non-specific. Furthermore, alpha-fetoprotein and other serological markers are usually normal. Thus, histological examination is the only way to achieve the diagnosis, as in our case.
Primary hepatic leiomyosarcoma can arise from intrahepatic vascular structures, bile ducts or the round ligament. In our case, the tumor probably originated from the left branch of the portal vein or the round ligament. The first description of leiomyosarcoma by Perl in 1871 involved a tumor of the inferior vena cava[4]. Indeed, leiomyosarcoma of vascular origin often occurs in the inferior vena cava. On the other hand, those arising from portal vein are extremely rare and only 6 cases have been reported in the literature (Table 1)[5-10].
| Ref. | Wilson et al[5] | Sundaresan et al[6] | Boudjema et al[7] | Gohrbandt et al[8] | Gaignard et al[9] | Esposito et al[10] |
| Patient characteristics | Female, 28 yr | Female, 67 yr | Female, 44 yr | Female, 71 yr | Male, 53 yr | Male, 78 yr |
| Treatment | Operated - not resected | Left hepatectomy (R2) | Whipple with portal and biliary confluence reconstruction (R0) | Right hepatectomy with portal and biliary reconstruction (R0) | Right hepatectomy with portal and biliary reconstruction (R0) | Left hepatectomy (R0) |
| Outcome | Not available | Not available | Recurrence 27 mo after surgery. Died, 47 mo after surgery | Recurrence 36 mo after surgery. Alive | No recurrence. Alive | No recurrence. Alive |
No risk factors have been identified yet, although the increasing incidence of the tumor has been noted among immunosuppressed patients[11]. Nevertheless, more studies are needed to investigate the underlying pathogenetic mechanisms of this uncommon entity.
Due to the rarity of primary hepatic sarcomas in general and primary hepatic leiomyosarcoma in particular, the standard of care has not been defined. Radical R0 hepatectomy, in the form of wedge resection, segmentectomy, lobectomy or extended hepatectomy, is the cornerstone of successful management of primary hepatic leiomyosarcoma[12]. In our case, as the tumor was located in the liver, we were able to perform a surgical resection, obtaining a tumor-free margin. However, this tumor has aggressive metastatic potential and is usually diagnosed in locally advanced or metastatic disease. The role of adjuvant or neoadjuvant chemotherapy and radiotherapy regimens in these circumstances has not yet been established. Similarly, orthotopic liver transplantation remains controversial.
Little is known about the natural history of the disease. However, survival rates are relatively low, as the tumor is usually diagnosed in advanced stages. Chi et al[1] reported a median overall survival of 19 mo (range 0-181 mo) with 1-, 2- and 5-year survival rates of 61.2%, 41.1% and 14.5%, respectively. The smaller size of the lesion and tumor-free resection margin were identified as independent predictors of improved survival. Two years after surgical resection, our patient is alive and with no evidence of tumor recurrence, probably because the diagnosis was established at an early stage and the surgery achieved a tumor-free margin.
Primary hepatic leiomyosarcoma is a rare malignant disease with a poor prognosis. The authors report a rare case of resected primary hepatic leiomyosarcoma originating from the portal vein or the round ligament. Although there is no standard treatment due to the rarity of this disease, we showed that liver resection with a tumor-free resection margin could be an effective treatment in the early stages. Gastroenterologists should be alert to this unusual entity as early diagnosis requires a high degree of suspicion due to atypical clinical presentation and non-specific imaging features. We emphasize the need for a global database for these rare tumors to promote a better understanding and standardized treatment of these patients.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Portugal
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): E
P-Reviewer: Gupta V, India; Hien NX, Vietnam S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Gong ZM
| 1. | Chi M, Dudek AZ, Wind KP. Primary hepatic leiomyosarcoma in adults: analysis of prognostic factors. Onkologie. 2012;35:210-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Shivathirthan N, Kita J, Iso Y, Hachiya H, Kyunghwa P, Sawada T, Kubota K. Primary hepatic leiomyosarcoma: Case report and literature review. World J Gastrointest Oncol. 2011;3:148-152. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 32] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (1)] |
| 3. | Hamed MO, Roberts KJ, Merchant W, Lodge JP. Contemporary management and classification of hepatic leiomyosarcoma. HPB (Oxford). 2015;17:362-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Halyo V. Martin L. Perl (1927-2014). Nature. 2014;516:330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Wilson SR, Hine AL. Leiomyosarcoma of the portal vein. AJR Am J Roentgenol. 1987;149:183-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Sundaresan M, Kelly SB, Benjamin IS, Akosa AB. Primary hepatic vascular leiomyosarcoma of probable portal vein origin. J Clin Pathol. 1990;43:1036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Boudjema K, Sulpice L, Levi Sandri GB, Meunier B. Portal vein leiomyosarcoma, an unusual cause of jaundice. Dig Liver Dis. 2014;46:1053-1054. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Gohrbandt AE, Hansen T, Ell C, Heinrich SS, Lang H. Portal vein leiomyosarcoma: a case report and review of the literature. BMC Surg. 2016;16:60. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Gaignard E, Bergeat D, Stock N, Robin F, Boudjema K, Sulpice L, Rayar M, Meunier B. Portal vein leiomyosarcoma: A rare case of hepatic hilar tumor with review of the literature. Indian J Cancer. 2019;56:83-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Esposito F, Lim C, Baranes L, Salloum C, Feray C, Calderaro J, Azoulay D. Primary leiomyosarcoma of the liver: Two new cases and a systematic review. Ann Hepatobiliary Pancreat Surg. 2020;24:63-67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Brichard B, Smets F, Sokal E, Clapuyt P, Vermylen C, Cornu G, Rahier J, Otte JB. Unusual evolution of an Epstein-Barr virus-associated leiomyosarcoma occurring after liver transplantation. Pediatr Transplant. 2001;5:365-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 58] [Article Influence: 2.4] [Reference Citation Analysis (0)] |