Copyright
©The Author(s) 2015.
World J Hepatol. Jul 8, 2015; 7(13): 1735-1741
Published online Jul 8, 2015. doi: 10.4254/wjh.v7.i13.1735
Published online Jul 8, 2015. doi: 10.4254/wjh.v7.i13.1735
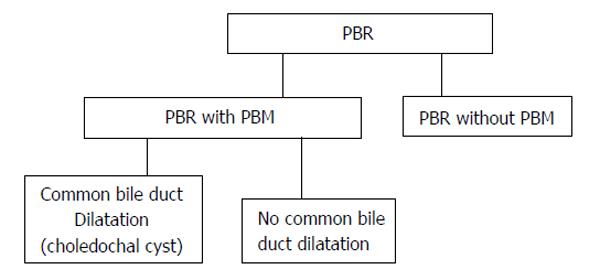
Figure 1 Classification of pancreaticobiliary reflux.
PBR: Pancreaticobiliary reflux; PBM: Panceraticobiliary maljunction.
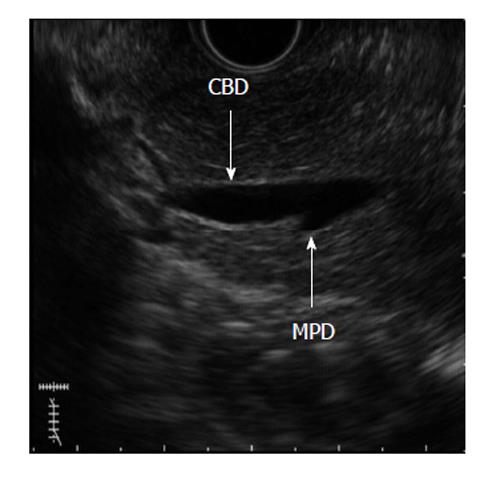
Figure 2 A 56-year-old female with pancreaticobiliary maljunction without choledochal cyst.
Endoscopic ultrasound image shows pancreaticobiliary maljunction. CBD: Common bile duct; MPD: Main pancreatic duct.
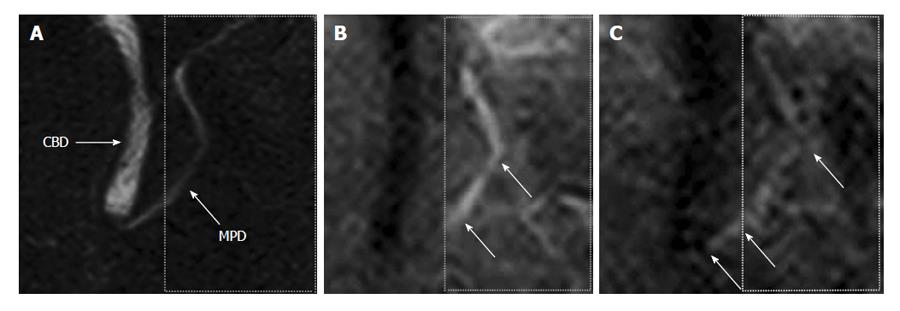
Figure 3 A 47-year-old male with normal volunteer.
A: Magnetic resonance cholangiopancreatography image. Labelling pulse of pancreas juice is applying to box surrounded by dotted lines on pancreas juice in body and caudal portion of the 3) main pancreatic duct; B: Time-SLIP image is not showing movement of pancreatic juice; C: Flow of pancreatic juice from body of the pancreas into head of pancreas is noted by high signal intensity (arrows). Reprinted from Sugita et al[43] (by permission of Wiley Periodicals, Inc). CBD: Common bile duct; MPD: Main pancreatic duct.
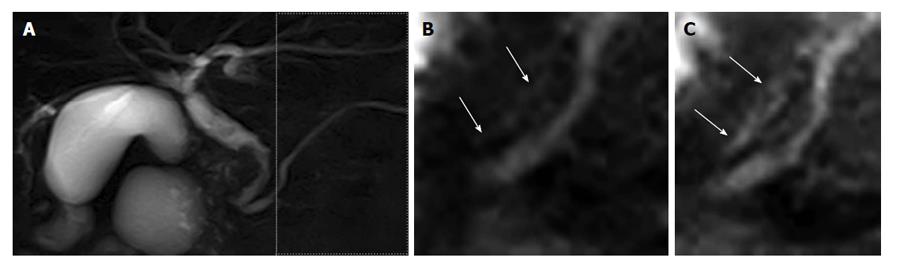
Figure 4 A 75-year-old male with common bile duct carcinoma without pancreaticobiliary maljunction.
A: Magnetic resonance cholangiopancreatography image shows the irregular wall throughout the entire common bile duct, with bile duct carcinoma revealed by biopsy. During endoscopic retrograde cholangiopancreatography, amylase level was measured in the bile. The amylase level in the collected bile was 1415 IU/L, higher than the upper limit of serum amylase of 130 IU/L; B and C: Labeled pancreatic juice in the main pancreatic duct refluxing into the common bile duct. Reprinted from Sugita et al[43] (by permission of Wiley Periodicals, Inc).
- Citation: Sugita R. Pancreaticobiliary reflux as a high-risk factor for biliary malignancy: Clinical features and diagnostic advancements. World J Hepatol 2015; 7(13): 1735-1741
- URL: https://www.wjgnet.com/1948-5182/full/v7/i13/1735.htm
- DOI: https://dx.doi.org/10.4254/wjh.v7.i13.1735