INTRODUCTION
The course of various pathological conditions depends on the recruitment of stem cells and partially differentiated progenitor cells[1,2]. Elevated systemic circulation of hematopoietic and endothelial precursors has been reported and these populations are believed to be implicated in progression of various diseases. In the past few years, it has become increasingly appreciated that mobilization of stem/progenitor cells from the endogenous pool may have tremendous clinical importance[3,4]. The notion that endogenous stem cells may be activated to mend damaged tissues during injury repair and organ regeneration has prompted efforts to identify stem cell mobilization factors for their potential use in regenerative medicine. Initially, approaches to cell mobilization have been developed as a strategy to induce the egress of hematopoietic stem cells (HSC) and hematopoietic progenitor cells (HPC) as an alternative to the highly invasive whole bone marrow transplantation[5].
Endothelial progenitor cells (EPC), giving rise to mature endothelial cells (EC), represent another mobile clinically important cell population[6]. New vessel formation in pathology/tissue repair depends on the local proliferation of EC in supporting microvasculature (angiogenesis)[7-9]. It has been realized that, in addition to angiogenesis, recruitment of circulating progenitors from the bone marrow into blood vessels (vasculogenesis) takes place in adulthood[10-12] in response to hypoxia and inflammation factors[13-15]. This paradigm shift has changed our view of how vascular composition is maintained in pathological tissues including tumors. Increased levels of circulating EPC are associated with a reduced risk of death from cardiovascular causes[16], indicating the benefit of their mobilization to ischemic tissues.
While bone marrow-derived progenitor cells may be implicated in cancer pathology, the full spectrum of circulating vascular progenitors, their individual roles, and the identity of the underlying stem cells is yet to be fully understood[17,18]. Endothelial and pericyte abnormalities observed in cancer suggest that endothelial mimicry plays an important role in tumor vascularization[19]. Several populations of circulating cells, other than EC and EPC, have been recently implicated in supporting tumor vasculogenesis. Tumor-associated dendritic cells (TADCs), a new leukocyte population expressing both DC and endothelial markers were shown to participate in the assembly of ovarian carcinoma neovasculature[20]. Recruited bone marrow-derived circulating cells (RBCCs), which express VEGFR1 but not VEGFR2, are transported to various organs where they engage in neovasculogenesis[21]. Moreover, identical to RBCCs, a population of TIE2-expressing monocytes (TEMs) was shown to be recruited to tumor sites and to promote cancer angiogenesis in a paracrine manner after adhering to newly forming blood vessels[22]. Some or all of these CD45+ circulating proangiogenic cell populations are likely to be identical to cells previously described as fibrocytes[23]. Interestingly, while fibrocytes are of myeloid origin, they have been proposed as progenitors of mesenchymal cells based on their in vivo differentiation into adipocytes[24].
MESENCHYMAL PROGENITOR CELLS AND THEIR CLINICAL IMPORTANCE
In the past few years, stromal mesenchymal progenitors, commonly referred to as mesenchymal stromal cells (MSC), have been identified as potentially important players in a number of pathological conditions[3,25]. Originally, MSC were isolated from the bone marrow stroma and termed fibroblast colony-forming units (CFU-F) based on their morphology[26]. The ability of this cell population to differentiate into cells of mesenchymal lineages, such as osteoblasts, chondrocytes, and adipocytes, has resulted in the term mesenchymal stem cells[27-29]. Recent studies in various organs by us and others have revealed that MSC function as perivascular cells maintaining vascular integrity (pericytes)[30-33]. Preclinical studies and clinical trials with allografted MSC, indicate the intrinsic therapeutic potential of these cells and suggest that they are activated in disease to engage in tissue repair[34]. It has been proposed that, upon injury, pericytes are mobilized and function as MSC that support the tissue regeneration process. This support involves trophic activity and the immunoprotection provided by the MSC. The trophic activity of MSC results from powerful bioactive molecules that they secrete to suppress apoptosis and scarring as well as to promote cell proliferation and vascularization[35,36]. In addition, MSC have immunomodulatory properties[37], and their capacity to mute T-cells is beneficial to autoimmune disease patients as it favors the outcome of bone marrow transplantation through the suppression of graft-versus-host-disease.
Candidate molecular pathways responsible for migration of mesenchymal stromal cells
Bone marrow transplantation studies in mice have demonstrated that a number of progenitor cell populations can undergo mobilization and migration[14,38-40]. Eukaryotic cells migrate in the body along external chemotactic gradients[1,41,42]. Chemotactic stimuli are sensed by heterotrimeric G-protein coupled receptors, the main class of which is the chemokine receptors[43]. There are multiple CCR-type and CXCR-type chemokine receptors characterized by their activation by cytokines called chemokines. Upon chemokine binding, activated chemokine receptors trigger G-protein subunit rearrangement allowing the exchange of GDP for GTP and activation of phospholipase C (PLC). At the same time, G-protein rearrangement upon chemokine binding can activate the protein tyrosine kinase, which phosphorylates the chemokine receptor and causes its desensitization. As a result of this transient activation, membrane-associated PLC carries out phosphatidylinositol phosphate cleavage, which produces diacylglycerol and leads to activation of protein kinase C, a flux in intracellular Ca2+ and downstream intracellular signaling transduced through the MAP kinase pathway[44]. Consistent with the role of chemokine gradients in MSC migration, there is evidence for the involvement of CXCR4 in mobilization of bone marrow MSC[45]. A number of chemokines and chemokine receptors have been identified as potential effector molecules upregulated in MSC that are activated to undergo migration. For example, expression of CCR1, CCR2, CCR3, CCR4, CCR7, CCR9, CXCR4, and CXCR5 was found to be upregulated on the surface of MSC in response to inflammation signals[46]. Further studies should be done to identify pathways governing migration of MSC in cancer.
The cell migration machinery triggered by chemotactic stimuli activates cell motility. This occurs via cell contraction coordinated with a cyclic gradient of reassembly of focal adhesions, through which the cell attaches to the extracellular matrix (ECM)[47,48]. Intracellular signaling initiated by chemokines induces changes in the clustering and avidity of cell adhesion molecules called integrins. Integrins are heterodimeric transmembrane cell-surface receptors, comprised of α and β chains, which act as the principle mediators of the interaction between the ECM environment and the cell[49,50]. The α5 and β1 integrin subunits are selectively overexpressed on MSC and are thought likely to control MSC migration. This is supported by data indicating that MSC utilize β1 (also known as CD29) for migration to and engraftment into ischemic myocardium[51]. The α5β1 integrin complex is known to be a receptor for the ECM protein fibronectin, the major substrate of stromal cells connected with collagen fibers. Recently, we identified β1 integrin as an MSC surface receptor for the matricellular protein SPARC (secreted protein, acidic and rich in cysteine)[52], and demonstrated that SPARC induces de-adhesion and migration of MSC derived from white adipose tissue (WAT)[53]. Further studies will be needed to test whether MSC migration in vivo is triggered by SPARC/α5β1 signaling.
White adipose tissue as a source of mesenchymal stromal cells
Because the ability of the bone marrow progenitors to respond to mobilization stimuli appears to decline with age[54], there is likely to be a progressively decreased capacity of the bone marrow-derived cells to engage in injury repair. The role of other organs in supplying stromal progenitor cells for neovessels is also beginning to emerge[55]. For example, experiments in rodents have demonstrated that non-bone marrow-derived cells contribute to vascularization during wound repair[56]. As we have recently proposed, WAT represents a potential source of mobilizable progenitor cells[3]. Clinically, expansion of WAT leading to obesity results from adipocyte hypertrophy, as well as hyperplasia resulting from progenitor cell proliferation[30,57]. Multipotent progenitors of preadipocytes in WAT have been identified in the stromal/vascular fraction (SFV)[58]. Recently, elegant attempts to classify multipotent subpopulations within the SVF of WAT have been reported[30,59]. In addition to adipocytes, WAT contains vascular adipose endothelial cells (AEC) and perivascular adipose stromal cells (ASC) as well as infiltrating hematopoietic cells such as macrophages and lymphocytes[60].
We and others have shown that WAT mesenchymal progenitors correspond to CD34-positive CD45-negative CD31-negative (CD34+CD45-CD31-) ASC that comprise the majority of cells in the SVF and display multipotency and proliferation capacity comparable to those of bone marrow MSC, while also having clear unique features[31,59,61]. Consistent with depot-specific roles of WAT in pathology, the content and properties of cells composing WAT have been found to differ between visceral and subcutaneous (e.g. interscapular and inguinal) WAT depots[62]. Interestingly, visceral adipose progenitors appear to have comparatively high self-renewal capacity, consistent with abdominal WAT remaining in old age when subcutaneous depots are depleted[63].
Interestingly, accumulating evidence indicates that ASC, in addition to serving as stem cells, display characteristics of pericytes (mural cells) and cooperate with the endothelium during vascularization[31], which has been confirmed by others[30,59]. ASC promote endothelial cell proliferation and blood vessel formation at least in part via trophic effects of secreted vascular endothelial growth factor (VEGF), hepatocyte growth factor (HGF), and other angiogenic molecules[59,64]. It has been shown, however, that systemically administered ASC[64] and endogenous AEC[65] can physically localize to sites of injury and contribute to revascularization of injured mouse tissues. The clinical potential of WAT-derived MSC is demonstrated, for example, by studies showing that patient-derived ASC contribute to repair of ischemia-induced injury in vivo via secretion of growth factors supporting neovascularization[64]. Moreover, human ASC can induce angiogenesis and nerve sprouting following myocardial infarction, resulting in potent preservation of cardiac function[66]. This ASC function is mediated at least in part though their capacity to cooperate with the endothelium in forming vascular networks[67].
Mesenchymal stromal cells and cancer progression
Cancer progression, the multi-step process that involves tumor growth, invasion, and metastasis[68], relies on neovascularization[7-9]. The importance of cancer vasculogenesis, involving inflammation-associated infiltration of endothelial and hematopoietic cells, has been revealed recently[39,40,69]. While marked quantitative differences between human cancers and experimental mouse models with respect to the mechanisms and clinical relevance of vasculogenesis still remain to be reconciled[70], it has been shown that levels of circulating progenitor cells (CPC) and of mature EC are elevated in human cancer[17,18,71], and that circulating EC do engraft into the tumor vasculature[72], suggesting a possible role in disease progression. The role of various leukocyte populations migrating to tumors and promoting cancer progression is also well recognized[14,38,73-76].
Because tumors secrete hypoxia and inflammation factors, it has been hypothesized that MSC may become recruited by tumors in cancer. Supporting this possibility, elevated circulation of CFU-F in cancer patients has been reported[77]. Recruitment of experimentally administered MSC by tumors has been demonstrated in animal models[78,79]. It has been proposed that MSC may be the progenitors of tumor stromal cells, which are also termed tumor-associated (or cancer-associated) fibroblasts (CAF)[78,80-83]. Upon tumor infiltration, MSC may re-establish the trophic microenvironment they normally maintain in the bone marrow[84,85]. Activation, and proliferation of stromal cells in tumors leads to their conversion into myofibroblasts/reactive stroma[83,86,87]. The resulting remodeling of the ECM, which the mesenchymal tumor cells execute, is an integral component of cancer progression[83,88,89]. There is evidence for epigenetically altered MSC cells driving both cancer initiation and progression[80,90,91]. The secretion of angiogenic and anti-apoptotic factors by MSC, as well as their ability to suppress T cell-mediated immune response has been proposed to account for the tumor-supporting role of MSC[37,42,79]. Consistent with the proposed importance of mesenchymal cells for cancer progression, experiments in animal models indicate that perivascular cells in tumors, supported by endogenously recruited mesenchymal progenitors[92] present a target complimentary to endothelial cells[93]. There is still no agreement in the field on the details of MSC localization upon homing. There are reports on both MSC incorporation into the endothelial cell layer and MSC perivascular engraftment[23,94,95]. It has been proposed that MSC incorporated into perivascular stroma might promote tumor growth via secretion of angiogenic factors, as previously demonstrated by tumor-associated fibroblasts[82,96]. Indeed, the ability of bone marrow MSC to favor tumor cell growth in rodent models has been demonstrated[97].
OBESITY AND CANCER: A PROGENITOR CELL LINK?
Identification of factors that can affect the clinical course of cancer is critical for strategizing the approaches to disease management. One such factor is obesity which is a progressively wide-spreading medical and social problem that has been reported to complicate a number of life-threatening pathologies[98]. Epidemiological studies have demonstrated that obesity, as measured by BMI (BMI= weight/height2) and waist-to-hip ratios, is associated with an increased risk of developing certain types of cancer[6,7]. Moreover, obesity has been shown to promote the progression of a number of cancers[2-5]. Increased physical activity and diet are the most logical measures against obesity although, unfortunately they have become increasingly insufficient given the lifestyle accepted in the modern world[99,100]. Thus, the prevalence of overweight and obese individuals which is increasing dramatically in most parts of the world, is likely to account for continuous changes in cancer epidemiology.
Colorectal cancer stands out as disease for which both risk and progression are positively associated with obesity. Anthropometric measures of adipose distribution have indicated an association between obesity and colon tumors and a similar association has also been noted for large or advanced adenomas, the proximate precursor to most colon cancers[101,102]. This risk of colon cancer in obese men may be as much as 2-fold that of leaner men. Interestingly, while body weight, and physical inactivity have been found to be positively related to risk of colon cancer in men, weaker or no associations have been reported for women. The lack of association between obesity and colorectal cancer in women[101] may be due to hormonal factors, since estrogens and hormone replacement therapy have been demonstrated to protect against colon cancer in both epidemiological and interventional studies. However, an alternative and unrecognized explanation is the difference of body fat distribution in men and women. Obesity in men is featured by comparatively high degree of visceral fat expansion, as compared to women typically showing outgrowth of subcutaneous hip fat, which suggest that the proximity of fat tissue to tumor site may be important. Interestingly, although a striking association between increased body mass index and colon cancer development has been found in numerous epidemiological studies, no consistent association has been found for rectal cancer[102].
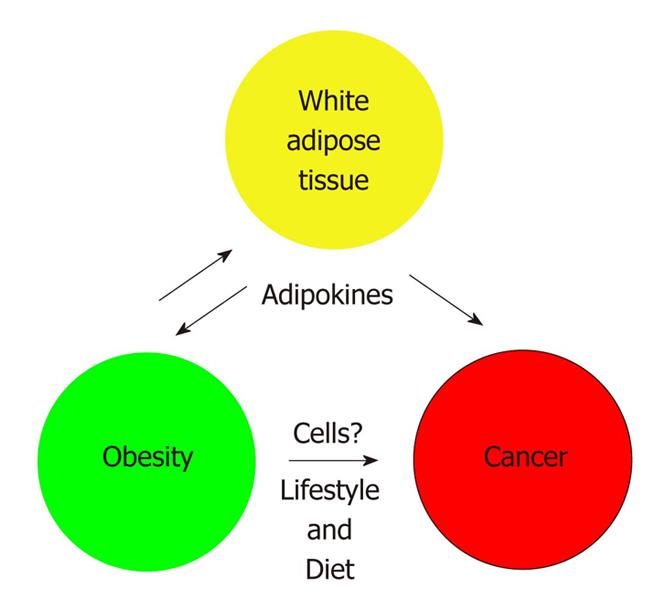
The pathophysiology underlying the association between obesity and cancer is unclear. The regulatory mechanisms associated with both obesity and cancer are influenced by lifestyle (including diet and physical activity) and genetic factors (Figure 1). The metabolic syndrome[103], featured by insulin resistance and subsequent hyperinsulinemia, may be a critical consequence of obesity. This possibility is supported by studies showing that subjects with type-2 diabetes are at increased risk of colon cancer. Hyperinsulinemia has also been proposed as an underlying biological mechanism for the observed associations between sedentary behaviour, obesity, and colorectal cancer. Consistent evidence indicates that metabolic aspects of central and abdominal adiposity contribute to the influence of obesity on cancer. The possible association between diabetes mellitus, diets high in sugar, refined grains, high glycemic load, and colorectal cancer supports these observations. Conversely, energy restriction and its consequent insulin lowering effects seem to inhibit carcinogenesis in animal models, although the corresponding studies in patient populations have produced controversial results. Besides having its own growth-promoting effects, hyperinsulinemia enhances the growth hormone–stimulated expression of insulin-like growth factors (IGFs) and increases their bioavailability via decreased synthesis of IGF-binding proteins IGFBP-1, IGFBP-2, and IGFBP-3. In addition to their important role in normal growth and development, IGF-1 and IGF-2, through autocrine, paracrine, and endocrine actions, can promote proliferation of tumor cells. The IGF-1 receptor mediates the proliferative activity of the IGFs. Both epidemiologic and in vitro studies have shown that endogenous and exogenous estrogens reduce serum IGF-1. Although higher concentrations of insulin are directly mitogenic for certain tumor cells in vitro, the clinical relevance of the metabolic syndrome in cancer etiology requires further study.
Figure 1 How does obesity promote cancer? In addition to obesity-associated lifestyle and diet which could influence cancer course, white adipose tissue (WAT) overgrowth may directly contribute to the pathogenesis of obesity and cancer progression.
Adipokines (soluble molecules secreted from WAT) have been proposed to play a role, but other mechanisms may also be important.
The fact that obesity is the consequence of WAT expansion provides clues to the mechanistic links between obesity and cancer progression. It has been hypothesized that WAT itself, in addition to the metabolic syndrome and a state of chronic low-grade inflammation associated with obesity, contributes to cancer progression[104]. WAT has been revealed as a potent endocrine organ, which secrets into circulation various growth factors (IGF-1, IGFBPs, and TGF-β), cytokines (such as TNF-α and interleukin-6), and hormones (such as leptin)[60,105]. Expression of these adipokines increases in obesity and affects lipid metabolism, insulin sensitivity, the alternative complement system, vascular haemostasis, angiogenesis and regulation of energy balance[106-108]. Some of these adipokines have been shown to promote cancer in various animal and in vivo models, and could potentially be implicated in the effect of WAT on colon cancer progression in patients[109,110]. For example, interleukin-6 is strongly linked to inflammation-associated colorectal cancers, such as those associated with inflammatory bowel disease (IBD). Therefore, the endocrine/paracrine signaling by WAT could provide a mechanism by which obesity-related metabolic disorders drive cancer. However, the identity of the key cancer-promoting systemically circulating WAT-derived factors has remained controversial, and there is still no conclusive clinical data reported to prove that specific WAT-derived adipokines promote cancer by enhancing proliferation of tumor cells in vivo[111]. Therefore, the possibility of paracrine effects of WAT-derived cells in the vicinity of the tumors should also be considered.
A role of adipose mesenchymal stromal cells in cancer?
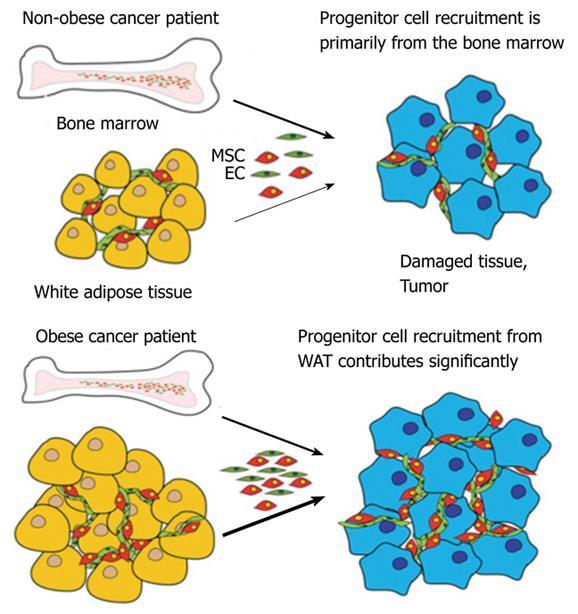
Despite the striking biological potency of WAT-resident progenitors[61], the possibility that MSC from WAT may undergo spontaneous mobilization and affect the progression of human disease has not so far been acknowledged. It is possible that adipose MSC can be mobilized in response to pathological signals and become recruited into the sites of disease, for instance serving as an extra CAF reserve in obese cancer patients (Figure 2). We have proposed that MSC from WAT (ASC) may become mobilized in obese patients in response to tumor signals and become recruited for tumor vasculogenesis[3]. Because the abundance of WAT cells is dramatically elevated in obese individuals, we hypothesize that high numbers of WAT-derived cells possibly mobilized and recruited by tumors in obese cancer patients may account for the epidemiological association between obesity and cancer progression.
Figure 2 A model for the role of mesenchymal stromal cells of obese patients in cancer progression.
Arrow thickness depicts relative contribution of progenitor cells from bone marrow and white adipose tissue. WAT: White adipose tissue; MSC: Mesenchymal stromal cells; EC: Endothelial cells.
Animal studies demonstrating the role of white adipose tissue-derived cells in cancer progression
The possibility that WAT cells may be mobilized in cancer and promote its progression has been tested for the first time in our recent work[112,113]. First, we tested whether mouse WAT cells can home to tumors. To analyze the short-term homing and engraftment capability of adipose cells, WAT SVF from mice expressing the green or red fluorescent proteins[114] (GFP or RFP) were iv-injected into mice bearing several types of model tumors[112]. Mice were sacrificed at 1 d and 3 d post-injection, and tissue sections were evaluated for the presence of GFP+ cells by immunofluorescence. At each time point, up to 50 GFP+ cells per cm2 were detected in tumor sections. Lungs, an established site of first-passage non-specific trapping of iv-injected cells, also contained occasional (1-5 per lung section) GFP+ cells, whereas no GFP+ cells were detected in control organs, including spleen, liver, and pancreas, as well as WAT. To assess recruitment of adipose cells by human tumors, we established xenografts of several human tumor cell lines in immunodeficient mice. Homing of adipose cells to tumors in these models similarly occurred within 1 d post-injection. Analysis of tissues with anti-Ki67 antibodies, demonstrated only rare proliferation of GFP+ cells.
To explore long-term engraftment of WAT cells, we injected 106 adipose SVF cells into mice bearing tumor grafts and analyzed tissues over 2 wk[112]. Over 80% of the GFP+ cells in tumors localized within the stroma, whereas the rest of the GFP+ cells appeared associated with blood vessels. At day 7, approximately 25% of tumor microvessels were found to contain threads of GFP+ cells, which at day 14 acquired morphology undistinguishable from the rest of the tumor blood microvessels. Confocal microscopy analysis showed that 5 to 10 % of the vessel-associated GFP+ expressed CD31, suggesting their endothelial identity. In many cases, endogenous GFP-/αSMA+ pericytes were observed as perivascular cells wrapped around GFP+ cells in capillaries, consistent with GFP+ cells being integrated into the lumen. Only about 1% of vessel-associated tumor-localized GFP+ cells were αSMA-positive, indicating that perivascular localization of donor cells is generally not related to αSMA expression. These data indicate that WAT-derived cells infiltrate different tumor compartments and suggest that both endothelial and stromal lineages are recruited by tumors.
Effect of adipose stem cells on tumor growth
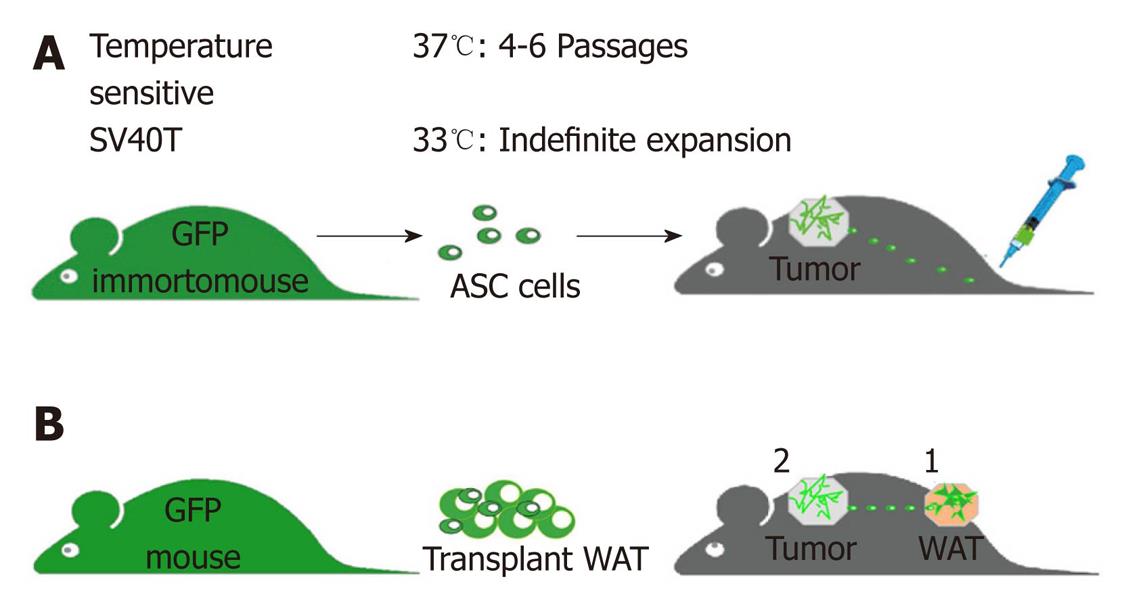
To generate a continuous ASC supply for metronomic cell administration in a long-term cancer progression study, we have developed a mouse model that has allowed us to establish a consistent source of readily available WAT-derived cells (Figure 3A). This new mouse strain termed ‘Immorto/GFP’, was created by crossing GFP mice[114] with ‘Immortomice’ that ubiquitously express a temperature-sensitive SV-40 T-antigen[115]. Cells from Immorto/GFP mice can be indefinitely cultured at permissive temperature (33°C), while at 37°C temperature the SV-40 T is degraded, thus rendering GFP+ cells physiologically normal in vivo. We have isolated ASC along with control stromal cells from lungs and bone marrow, immortalized and expanded them[112]. We reasoned that metronomically-repeated long-term treatment of experimental animals with low-doses of WAT cells would simulate the hypothetical chronic pathological recruitment of adipose cells by tumors[112]. To avoid invasive repetitive iv injections, we established that the sc administration route is compatible with migration of WAT cells to tumors. Analysis of peripheral blood mononuclear cells (PBMC) demonstrated that sc-injected WAT SVF cells were detectable in circulation as early as 15 min post-injection and began clearing the circulation after 6 h. Immunofluorescence analysis of tumors revealed comparable numbers of GFP+ cells in the stromal and perivascular compartments in sc-injected and iv-injected mice, indicating that sc-administered adipose cells efficiently home to tumors.
Figure 3 Design of experiments testing tumor homing of white adipose tissue cells and their effect on tumor growth.
A: metronomic green fluorescent proteins (GFP) + white adipose tissue (WAT) administration: cultured cells are sc-injected (lower back) using metronomic cell injection regimen (104 cells/d) into mice xenografted with human tumors (upper back). B: WAT transplants: GFP+ WAT is implanted (1) into lean mice prior to tumor grafting (2), which allows us to track recruitment of implant-derived cells by tumor and to measure the resulting effect on cancer progression. Tumor growth is compared to that in control mice.
To test the effect of ASC on tumor growth, we used immunodeficient Foxn1nu/nu mice, which have only residual endogenous WAT, as a model. Daily injections of 104 immortalized ASC or control cells were performed sc (distantly to tumor) for 6 wk starting 1 d after tumor grafting. After 2 wk of treatment, tumor growth rate accelerated in ASC-injected mice, but not in mice injected with control stromal cells. Analysis of tumors recovered from representative mice at week 6 revealed ASC accumulation in tumors, but not in control tissues.
Finally, we tested whether recruitment of endogenous WAT cells by tumors is associated with accelerated tumor growth. To determine whether migration of adipose cells to tumors could take place, we have developed an experimental model based on transplantation of traceable WAT cells into Foxn1nu/nu mice (Figure 3B). As a source of WAT for transplantation we used mice that ubiquitously express GFP.” To test whether WAT cells can be endogenously attracted by tumors, once GFP-labeled WAT implants had assimilated in the host 10 d post-implantation, we sc-grafted mouse tumor cells 2 cm away from the implant. For each model, tumors grew significantly faster in mice carrying WAT implants. Consistent with adipose cell mobilization into circulation, GFP+ cells were detected in blood by flow cytometry. Immunofluorescence analysis of tissues from WAT-grafted animals with anti-GFP and anti-CD31 antibodies demonstrated the presence of vascular and perivascular GFP+ cells within the tumors.
CONCLUSION
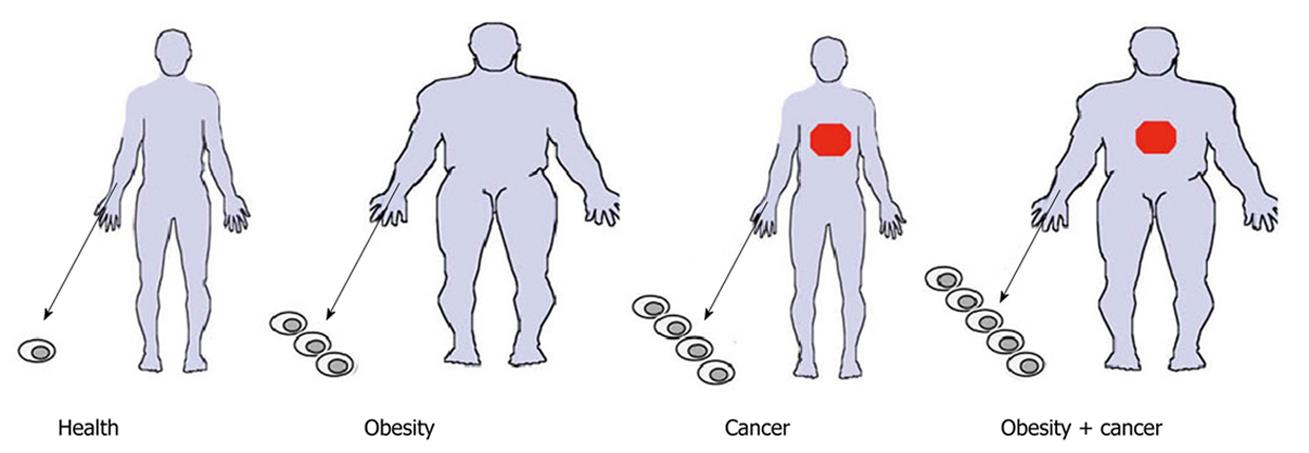
The studies outlined above suggest that advanced cancer progression is associated the recruitment of WAT-derived cells to tumors. These results are consistent with other reports indicating positive effect of ASC on tumor growth[116]. Collectively, data from these studies suggest that the recruitment of WAT-derived cells by tumors may at least partially account for advanced cancer progression in obese individuals (Figure 4). How exactly MSC (including ASC) are recruited to the diseased site is currently unclear. In theory, they could locally migrate to the sites of inflammation from the surrounding solid tissues (such as WAT), arrive through the systemic circulation, or both[42]. MSC are virtually absent in the peripheral circulation of healthy individuals although hypoxia and inflammation signals are believed to result in MSC mobilization and migration from their niche[94,117,118]. The possibility of spontaneous MSC mobilization in disease has been widely speculated upon, and could underlie their recruitment by tumors although this remains to be tested. Historically, quantification of tissue-resident progenitors has been performed based on the colony forming unit (CFU) assay based on the established ability of bone marrow-derived progenitors to attach to plastic[26,117]. Several groups have reported elevated CFU-F circulation in pathological conditions including cancer[77,119,120]. However, no careful immunophenotyping of freshly isolated cells was performed in some of these studies. It appears that in many cases hematopoietic cells, capable of EC and MSC mimicry in culture[121], may have been mistaken for MSC possibly accounting for conflicting published results. For example, based on CFU-F enumeration in blood, G-CSF treatment had been reported to mobilize MSC in humans[122], while in mice growth factors are incapable of mobilizing MSC without a perturbation in chemokine gradients[45]. Our unpublished results confirm that the abundance of attachable monocytes in blood is incompatible with the CFU assays for enumeration of MSC in circulation.
Figure 4 Increased circulation of white adipose tissue-derived cells in obese individuals? A hypothetical model predicts mobilization of adipose EC and MSC from residual adipose tissue into the peripheral blood, which may also occur in non-obese patients with cancer and is predicted to be the highest in obese cancer patients.
EC: Endothelial cells; MSC: Mesenchymal stromal cells.
It should be noted that plastic attachment is unlikely to be optimal for quantifying circulating stromal cells. This is because the CFU-F assay is designed to detect attachment of cells isolated from solid tissues, in which stromal cells maintain the state of firm adhesion. In contrast, cells undergoing mobilization are known to have key adhesion molecules, including β1[123], modulated to overcome matrix adherence and this is likely to reduce the ability of stromal cells to attach. More importantly, the dominating hematopoietic cells that attach to plastic upon PBMC plating for the CFU-F assay have been observed to inhibit MSC adherence and proliferation[124]. Therefore, capacity of MSC to undergo mobilization is still unclear and new methods are needed to quantify this phenomenon. Future studies will need to establish the identity of cell populations mobilized in obese cancer patients, compare the relative contribution of adipose and bone marrow-derived cells to tumors and investigate the mechanisms through which adipose cells promote cancer progression. This will allow us to determine whether cancer induces mobilization of cells from adipose tissue in obesity, to identify the populations of adipose cells that are recruited by tumors, and to determine functional contribution of ASC to tumor growth.