Published online Feb 26, 2024. doi: 10.4252/wjsc.v16.i2.64
Peer-review started: December 11, 2023
First decision: December 31, 2023
Revised: January 4, 2024
Accepted: January 19, 2024
Article in press: January 19, 2024
Published online: February 26, 2024
Processing time: 76 Days and 16 Hours
In this editorial, we comment on the article published in the recent issue of the World Journal of Stem Cells. They focus on stem cell preconditioning to prevent ferroptosis by modulating the cystathionine γ-lyase/hydrogen sulfide (H2S) pathway as a novel approach to treat vascular disorders, particularly pulmonary hypertension. Preconditioned stem cells are gaining popularity in regenerative medicine due to their unique ability to survive by resisting the harsh, unfavorable microenvironment of the injured tissue. They also secrete various paracrine factors against apoptosis, necrosis, and ferroptosis to enhance cell survival. Ferroptosis, a regulated form of cell death characterized by iron accumulation and oxidative stress, has been implicated in various pathologies encompassing dege
Core Tip: Ferroptosis is a regulated cell death mechanism entailing iron-dependent lipid peroxidation, accumulating reactive oxygen species, and subsequent cell damage. Like other cell-death mechanisms dominated by apoptosis and necrosis, ferroptosis significantly reduces the number of surviving donor cells post-engraftment, reducing the therapeutic effectiveness of cell-based therapy. Modulating ferroptosis mechanisms by preconditioning holds the therapeutic potential of stem cells by enhancing their survival and functionality.
- Citation: Zineldeen DH, Mushtaq M, Haider KH. Cellular preconditioning and mesenchymal stem cell ferroptosis. World J Stem Cells 2024; 16(2): 64-69
- URL: https://www.wjgnet.com/1948-0210/full/v16/i2/64.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v16.i2.64
The current understanding of stem cell biology, refinement of cell culture techniques, the progress in tissue engineering, and data emanating from clinical trials have provided new momentum to regenerative medicine and tissue repair. Notwithstanding the encouraging results and progress made therein, many issues in stem cell-based therapy necessitate resolution to ensure it can be established as a routine treatment option in clinical settings.
Massive donor cell death post-engraftment due to the uncongenial cytokine-rich host tissue microenvironment infiltrated by inflammatory cells is one of these issues that severely reduces the efficacy of the treatment. In some of the published studies, the reported survival of the transplanted cells is so low that the whole exercise of cell-based therapy becomes futile[1]. Hence, massive donor cell death is one crucial reason underlying the mixed data from clinical trials, leading to diverse approaches to enhance their survival post-engraftment[2]. Dominated by apoptosis, necrosis, and autophagy, donor cell death post-engraftment has multifarious mechanisms, with ferroptosis emerging as a novel programmed mechanism of cell death, morphologically and biochemically distinct from other cell death pathways[3].
Ferroptosis is a biological process that plays a vital role in the metabolism of amino acids, iron, and polyunsaturated fatty acids, as well as the production of glutathione (GSH), phospholipids, NADPH, and coenzyme Q10. It has been implicated in a subset of pathologies, including neurodegenerative diseases, cancer and stroke, vascular disorders, and pulmonary hypertension in mammals[4-7]. It is an iron-dependent form of regulated cell death that involves the accumulation of lipid peroxides and reactive oxygen species (ROS)[8,9].
The research interest in ferroptosis is gaining momentum as it is implicated in the poor engraftment of donor mesenchymal stem cells (MSCs), leading to the reduced efficiency of MSC-based treatment[6,10]. Ferroptosis can occur in response to diverse stimuli, such as starvation, exposure to toxins, ROS, etc, leading to intracellular iron accumulation[11]. Mechanistically, iron can react with hydrogen peroxide and lipid peroxides to form ROS with heightened lipid peroxidation and cell membrane injury death[11].
Signaling pathways involved in ferroptosis are complex and need to be better understood. However, recent research has shed light on some of the critical signaling pathways, such as p53, nuclear factor erythroid 2-related factor 2 (Nrf2), protein kinase R-like endoplasmic reticulum kinase[12], phospholipid remodeling pathway, GSH peroxidase 4 (GPX4), ferroptosis suppressor protein 1 and other emerging signaling pathways are considered to play a role therein[13,14]. This editorial aims to shed light on the pivotal role of the novel cystathionine γ-lyase (CSE)/hydrogen sulfide (H2S) pathway in ferroptosis, supported by the recent scientific evidence by Hu et al[10].
The CSE is an enzyme primarily expressed in the liver, kidney, and brain that critically regulates H2S production in the body[15]. It is a known cardio-protective enzyme detoxifying sulfur-containing amino acids, i.e. homocysteine, and requires pyridoxal phosphate as a prosthetic group. CSE has gained immense interest in the research as it produces a potent cell signaling gasotransmitter, H2S, an essential signaling molecule involved in several physiological and pathological processes such as inflammation, cell cycle, cell metabolism, cell death, and autophagy[15,16].
The CSE/H2S pathway has been implicated in various cellular events, including vasodilation, anti-proliferative, anti-inflammatory, and redox homeostasis[17,18]. Invariably, H2S production requires an appropriate concentration of cysteine and homocysteine in the presence of cystathionine-β-synthase and CSE, albeit CSE produces about 90% of the total H2S. H2S signals via protein sulfur hydration impart its pathologic effects on ischemia, myocardial fibrosis, metabolic disorder, traumatic brain injury, and bowel diseases[19,20]. In response to many stimuli, H2S orchestrates diverse molecular pathways to exert its effects on apoptosis and ferroptosis. The CSE/H2S pathway has been explicitly implicated in human melanoma progression and modulates tissue homeostasis implications in ophthalmic disease, angiogenesis, multiple sclerosis, and Parkinson’s disease[16,21,22].
H2S has been identified as a potent signaling molecule in various physiological processes, including neuromodulation within the brain and smooth muscle relaxation in the vascular system[20]. Additionally, it exhibits a remarkable cytoprotective effect by shielding neurons against oxidative stress and cardiac muscle from ischemia-reperfusion injury. Moreover, H2S can influence inflammation, insulin secretion, and angiogenesis[20]. The CSE/H2S pathway has also yielded novel biomarkers like homolanthionine and lanthionine, reported in the urine of homocystinuria patients and cardiovascular pathology[23].
Mechanistically, CSE catalyzes the cleavage of L-cysteine into pyruvate and NH3 and eliminates H2S, which plays a role in cellular signaling and has a cardiovascular protective role. Moreover, CSE is the critical enzyme for L-cysteine generation, a precursor of the antioxidant GSH[24].
Recently, gas-transmitters’ role in various physiological and pathological processes has intensified. H2S has become a key player in cellular signaling and regulation[16,24]. One of the critical mechanisms by which H2S regulates ferroptosis is its ability to scavenge ROS. ROS are known to induce lipid peroxidation, a hallmark of ferroptosis. H2S reacts with ROS to attenuate their damaging effects on lipids, preventing the initiation of a ferroptosis cascade[16,25]. In addition, H2S can indirectly activate antioxidant machinery, such as the Nrf2 pathway, which plays a crucial role in maintaining cellular redox homeostasis[25]. Furthermore, H2S has been shown to regulate iron metabolism by controlling cellular iron homeostasis through the modulation of ferroportin-1 and transferrin receptor-1 expression[26].
H2S and its effects on ROS and iron metabolism can also impact signaling pathways involved in ferroptosis. It can suppress MAPK signaling linked to ferroptosis activation[27]. H2S can also regulate the expression and activity of key molecules involved in ferroptosis, such as the cystine/glutamate antiporter system Xc-, GPX4, and the lipid repair enzyme GSH-S-transferase alpha 4[24,27]. The solute carrier family seven-member 11 (SLC7A11)/GPX4 pathway is a crucial defense mechanism against ferroptosis. SLC7A11 is a protein that helps synthesize reduced GSH and import cystine, which is then converted to cysteine for GSH synthesis[28].
GSH, in the presence of GPX4, converts toxic lipid peroxides to harmless lipid alcohols. Inhibiting SLC7A11 leads to GSH depletion, downregulation of GPX4, and the accumulation of damaging lipid peroxides. The SLC7A11/GPX4 axis is a target for potentially treating ferroptosis-related diseases[29,30]. Bioinformatic studies revealed multiple genes expressed in ferroptosis and other genes, and microRNAs can regulate ferroptosis and disease progression[30,31]. Given the significant role of the CSE/H2S pathway in cellular function, recent studies have revealed its crucial role in regulating ferroptosis in stem cells[10,32].
In their comprehensive investigation, Hu et al[10] investigated the therapeutic potential of human umbilical cord MSCs (hUCMSCs) in treating hypoxia-induced pulmonary arterial hypertension (PAH) in a murine model. They explored the impact of modulating the CSE/H2S pathway in preventing ferroptosis in hUCMSCs. Furthermore, the study demonstrated the capacity of hUCMSCs to homing towards injured lung tissue and protecting against pulmonary artery remodeling.
Remarkably, preconditioning hUCMSCs with a ferroptosis inhibitor, Fer-1, exhibited enhanced survival and efficacy in managing PAH, while ferroptosis induced low cellular viability and therapeutic effectiveness. These compelling findings imply a potential association between ferroptosis and the survival of hUCMSCs in hypoxia-induced PAH[10].
In this study, Hu et al[10] have shown that treatment of hUCMSCs with erastin, a ferroptosis inducer, significantly increases cell apoptosis and mitochondrial changes, with concomitant expression of ferroptosis markers, i.e. Fe2+, ROS, lipid peroxidation, and malondialdehyde, besides 4-hydroxynonenal, Fe3+-bound transferrin receptor, and nuclear receptor coactivator 4.
Conversely, the GSH/oxidized GSH ratio levels, cystine uptake, GPX4, ferritin heavy chain 1, and SLC7A11 expressions were significantly decreased[10]. These molecular changes were reversed when the cells were treated with Fer-1, a ferroptosis inhibitor, and further aggravated when CSE was inhibited, thus supporting the role of CSE/H2S signaling in preventing ferroptosis in hUMSCs and its efficiency as a therapeutic tool.
These data were further supported by a CSE-dependent decrease in H2S production in hUCMSCs while overexpressing CSE in the cells increased H2S levels[10]. CSE inhibition also reduced Nrf2 activation induced by Fer-1, while CSE overexpression upregulated Nrf2 inactivation caused by erastin. The expression of Nrf2 was also affected, with erastin treatment inhibiting its nuclear translocation. CSE inhibition upregulates Nrf2 expression in the cytoplasm and downregulates in the nucleus[10]. CSE overexpression-induced ferroptosis inhibition, which was eliminated by an Nrf2 inhibitor. Kelch-like ECH-associated protein 1 (Keap1) is the primary negative regulator of Nrf2 and mediates ubiquitylation and degradation of Nrf2[33,34].
Hu et al[10] have also reported that increased H2S-mediated sulfhydration of Keap1 in the hUCMSCs overexpressing CSE and decreased S-sulfhydration of CSE knockout cells treated with Fer-1, highlighting the role of CSE/H2S signaling in modulating ferroptosis in hUCMSCs.
MSCs hold immense potential in regenerative medicine, as they can differentiate into various cell types and replenish damaged tissues[35]. Stem cell preconditioning can effectively alleviate ferroptosis via several approaches. Hypoxic conditions increase the expression of heme oxygenase-1, which regulates iron metabolism and ferroptosis. Intriguingly, molecules like hydrogen peroxide or lipopolysaccharide can stimulate the secretion of protective paracrine factors from stem cells and modulate the expression of crucial ferroptosis genes, such as GPX4 and transferrin receptor 1, thereby mitigating ferroptosis-induced cell death[36].
Consequently, stem cell preconditioning has been extensively employed for therapeutic purposes in clinical settings and has progressed to advanced phases of clinical trials[37]. Recent research has shed light on the role of ferroptosis as a form of regulated cell death in stem cell biology, focusing on CSE/H2S signaling due to its cardinal physiological and pathological roles in cell death. The CSE/H2S pathway modulates and increases the viability of transplanted MSCs[38].
The underlying mechanism of improved survival has been attributed to the PI3K/Akt pathway activation to reduce cell death by mitochondrial and endoplasmic reticulum stress alleviation[19,38]. Moreover, ferroptosis of hUCMSCs is reduced by regulating the CSE/H2S pathway, which improves vascular remodeling in mice with hypoxia-induced PAH via maintaining the balance between stem cell maintenance and differentiation[10]. While genetic modification of stem cells for CSE expression is an efficient way of preconditioning the cells against ferroptosis, alternative preconditioning strategies may also be exploited[29,39,40].
These anti-ferroptosis strategies underscore their significance for potentially targeting ferroptosis signaling for therapeutic interventions in various diseases, including metabolic, inflammatory, and cancerous disorders[14]. As mitochondrial stress and ROS are integral parts of the molecular mechanism underlying ferroptosis, it would be interesting to assess the effectiveness of anti-apoptotic preconditioning strategies, i.e. physical, chemical, mechanical, genetic modulation, and growth factor treatment[41-47], either alone or in combination with anti-ferroptosis intervention to support improved cell survival. On the same note, combining sub-cellular preconditioning, i.e. mitochondrial targeting of Connexin-43[48] with anti-ferroptosis strategies to achieve their synergistic cytoprotective effect would be exciting.
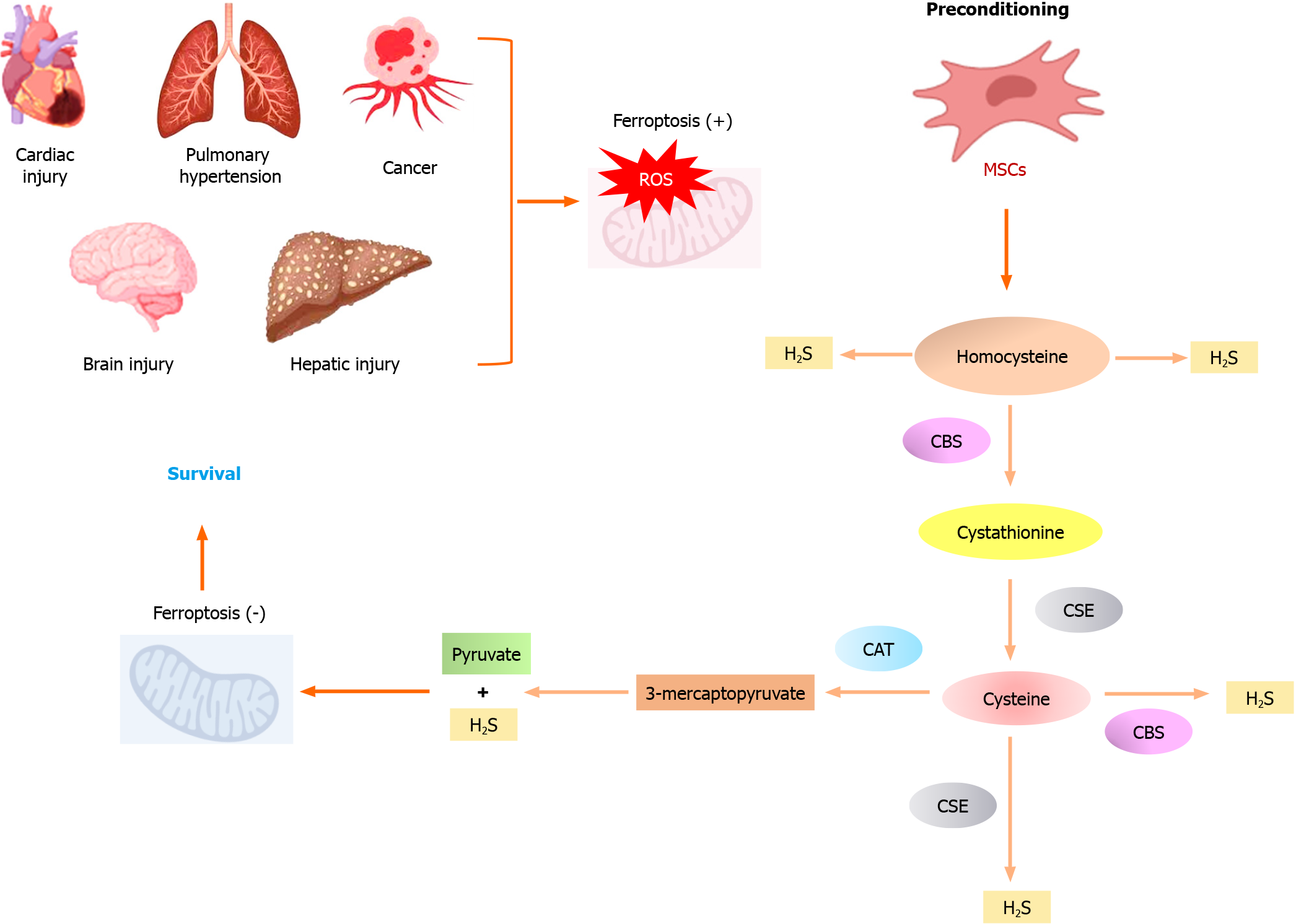
In conclusion, and as depicted in Figure 1, the emerging role of the CSE/H2S pathway in ferroptosis advocates that targeting this pathway could be a promising therapeutic approach for multiple diseases associated with ferroptosis. Developing CSE/H2S activators or H2S-releasing therapeutics may help attenuate ferroptosis and provide protective effects. Furthermore, understanding the specific mechanisms by which CSE/H2S signals in stem cells could enhance its therapeutic potential in various pathologies.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cell and tissue engineering
Country/Territory of origin: Saudi Arabia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Goebel WS, United States S-Editor: Wang JJ L-Editor: Filipodia P-Editor: Yuan YY
| 1. | Cinat D, Coppes RP, Barazzuol L. DNA Damage-Induced Inflammatory Microenvironment and Adult Stem Cell Response. Front Cell Dev Biol. 2021;9:729136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 43] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 2. | Haider HKh, Ashraf M. Strategies to promote donor cell survival: combining preconditioning approach with stem cell transplantation. J Mol Cell Cardiol. 2008;45:554-566. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 170] [Cited by in RCA: 168] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 3. | Abdelwahid E, Kalvelyte A, Stulpinas A, de Carvalho KA, Guarita-Souza LC, Foldes G. Stem cell death and survival in heart regeneration and repair. Apoptosis. 2016;21:252-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 89] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 4. | Hu Z, Liu C, Mao Y, Shi J, Xu J, Zhou G, Jiang F. Integration of transcriptomics reveals ferroptosis-related signatures and immune cell infiltration in bronchopulmonary dysplasia. Heliyon. 2023;9:e21093. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 5. | Liu S, Liu X, Xian J, Feng Z, Tian Y, Wang W, Tian X. Visualizing intracellular membrane interactions and cell type-specific differentiation in ferroptosis and apoptosis with Boranil-Carbazole derivative. Bioorg Chem. 2024;142:106949. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Liu X, Zhang J, Xie W. The role of ferroptosis in acute lung injury. Mol Cell Biochem. 2022;477:1453-1461. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 52] [Reference Citation Analysis (0)] |
| 7. | Stockwell BR, Friedmann Angeli JP, Bayir H, Bush AI, Conrad M, Dixon SJ, Fulda S, Gascón S, Hatzios SK, Kagan VE, Noel K, Jiang X, Linkermann A, Murphy ME, Overholtzer M, Oyagi A, Pagnussat GC, Park J, Ran Q, Rosenfeld CS, Salnikow K, Tang D, Torti FM, Torti SV, Toyokuni S, Woerpel KA, Zhang DD. Ferroptosis: A Regulated Cell Death Nexus Linking Metabolism, Redox Biology, and Disease. Cell. 2017;171:273-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4608] [Cited by in RCA: 4962] [Article Influence: 620.3] [Reference Citation Analysis (0)] |
| 8. | Liu C, Wang G, Han W, Tian Q, Li M. Ferroptosis: a potential therapeutic target for stroke. Neural Regen Res. 2024;19:988-997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 21] [Reference Citation Analysis (0)] |
| 9. | Feng S, Tang D, Wang Y, Li X, Bao H, Tang C, Dong X, Yang Q, Yan Y, Yin Z, Shang T, Zheng K, Huang X, Wei Z, Wang K, Qi S. The mechanism of ferroptosis and its related diseases. Mol Biomed. 2023;4:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 73] [Reference Citation Analysis (0)] |
| 10. | Hu B, Zhang XX, Zhang T, Yu WC. Dissecting molecular mechanisms underlying ferroptosis in human umbilical cord mesenchymal stem cells: Role of cystathionine γ-lyase/hydrogen sulfide pathway. World J Stem Cells. 2023;15:1017-1034. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 11. | Jiang T, Xiao Y, Zhou J, Luo Z, Yu L, Liao Q, Liu S, Qi X, Zhang H, Hou M, Miao W, Batsaikhan B, Damba T, Liang Y, Li Y, Zhou L. Corrigendum to "Arbutin alleviates fatty liver by inhibiting ferroptosis via FTO/ SLC7A11 pathway" [Redox Biol. 68 (2023) 102963]. Redox Biol. 2023;102974. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 12. | Hu W, Liang K, Zhu H, Zhao C, Hu H, Yin S. Ferroptosis and Its Role in Chronic Diseases. Cells. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 53] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 13. | Chu J, Li H, Yuan Z, Zhou W, Yu Y. Acetaminophen impairs ferroptosis in the hippocampus of septic mice by regulating glutathione peroxidase 4 and ferroptosis suppressor protein 1 pathways. Brain Behav. 2023;13:e3145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 14. | Yang D, Xia X, Xi S. Salvianolic acid A attenuates arsenic-induced ferroptosis and kidney injury via HIF-2α/DUOX1/GPX4 and iron homeostasis. Sci Total Environ. 2024;907:168073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 15. | Huang S, Li H, Ge J. A cardioprotective insight of the cystathionine γ-lyase/hydrogen sulfide pathway. Int J Cardiol Heart Vasc. 2015;7:51-57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 16. | Aroca A, Gotor C, Bassham DC, Romero LC. Hydrogen Sulfide: From a Toxic Molecule to a Key Molecule of Cell Life. Antioxidants (Basel). 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 80] [Cited by in RCA: 77] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 17. | Jin R, Yang R, Cui C, Zhang H, Cai J, Geng B, Chen Z. Ferroptosis due to Cystathionine γ Lyase/Hydrogen Sulfide Downregulation Under High Hydrostatic Pressure Exacerbates VSMC Dysfunction. Front Cell Dev Biol. 2022;10:829316. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 31] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 18. | Cunningham A, Oudejans LL, Geugien M, Pereira-Martins DA, Wierenga ATJ, Erdem A, Sternadt D, Huls G, Schuringa JJ. The nonessential amino acid cysteine is required to prevent ferroptosis in acute myeloid leukemia. Blood Adv. 2024;8:56-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 19. | Xiao T, Luo J, Wu Z, Li F, Zeng O, Yang J. Effects of hydrogen sulfide on myocardial fibrosis and PI3K/AKT1-regulated autophagy in diabetic rats. Mol Med Rep. 2016;13:1765-1773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 20. | Kimura H, Shibuya N, Kimura Y. Hydrogen sulfide is a signaling molecule and a cytoprotectant. Antioxid Redox Signal. 2012;17:45-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 228] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 21. | Panza E, De Cicco P, Armogida C, Scognamiglio G, Gigantino V, Botti G, Germano D, Napolitano M, Papapetropoulos A, Bucci M, Cirino G, Ianaro A. Role of the cystathionine γ lyase/hydrogen sulfide pathway in human melanoma progression. Pigment Cell Melanoma Res. 2015;28:61-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 103] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 22. | Sousa FBM, Souza LKM, Sousa NA, Araújo TSL, de Araújo S, Pacífico DM, Silva IS, Silva RO, Nicolau LAD, Souza FM, Filgueiras MC, Oliveira JS, Souza MHLP, Medeiros JVR. H(2)S is a key antisecretory molecule against cholera toxin-induced diarrhoea in mice: Evidence for non-involvement of the AC/cAMP/PKA pathway and AMPK. Nitric Oxide. 2018;76:152-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | DeRatt BN, Ralat MA, Lysne V, Tayyari F, Dhar I, Edison AS, Garrett TJ, Midttun Ø, Ueland PM, Nygård OK, Gregory JF 3rd. Metabolomic Evaluation of the Consequences of Plasma Cystathionine Elevation in Adults with Stable Angina Pectoris. J Nutr. 2017;147:1658-1668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 24. | Kimura H. Hydrogen Sulfide (H(2)S) and Polysulfide (H(2)S(n)) Signaling: The First 25 Years. Biomolecules. 2021;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 86] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 25. | Zou W, Yuan J, Tang ZJ, Wei HJ, Zhu WW, Zhang P, Gu HF, Wang CY, Tang XQ. Hydrogen sulfide ameliorates cognitive dysfunction in streptozotocin-induced diabetic rats: involving suppression in hippocampal endoplasmic reticulum stress. Oncotarget. 2017;8:64203-64216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 26. | Zhang MW, Yang G, Zhou YF, Qian C, Mu MD, Ke Y, Qian ZM. Regulating ferroportin-1 and transferrin receptor-1 expression: A novel function of hydrogen sulfide. J Cell Physiol. 2019;234:3158-3169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 27. | Rodkin S, Nwosu C, Sannikov A, Raevskaya M, Tushev A, Vasilieva I, Gasanov M. The Role of Hydrogen Sulfide in Regulation of Cell Death following Neurotrauma and Related Neurodegenerative and Psychiatric Diseases. Int J Mol Sci. 2023;24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 28. | Banerjee S, Sarkar R, Mukherjee A, Mitra S, Gope A, Chawla-Sarkar M. Rotavirus-induced lncRNA SLC7A11-AS1 promotes ferroptosis by targeting cystine/glutamate antiporter xCT (SLC7A11) to facilitate virus infection. Virus Res. 2024;339:199261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 29. | Huang L, Liu J, Jin Y, Qiu Y, Qin X, Wu S, Chen D, Bie C, Kuang W, Liu H. Niujiao Dihuang Jiedu decoction promotes SLC7A11 m5C methylation modification against ferroptosis in acute-on-chronic liver failure. Phytomedicine. 2024;122:155136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 30. | Wang HH, Fan SQ, Zhan YT, Peng SP, Wang WY. Suppression of the SLC7A11/glutathione axis causes ferroptosis and apoptosis and alters the mitogen-activated protein kinase pathway in nasopharyngeal carcinoma. Int J Biol Macromol. 2024;254:127976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 31. | Chen S, Jin X, He T, Zhang M, Xu H. Identification of ferroptosis-related genes in acute phase of temporal lobe epilepsy based on bioinformatic analysis. BMC Genomics. 2023;24:675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 32. | Markel TA, Drucker NA, Jensen AR, Olson KR. Human Mesenchymal Stem Cell Hydrogen Sulfide Production Critically Impacts the Release of Other Paracrine Mediators After Injury. J Surg Res. 2020;254:75-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 33. | Lee DH, Park JS, Lee YS, Bae SH. PERK prevents hepatic lipotoxicity by activating the p62-ULK1 axis-mediated noncanonical KEAP1-Nrf2 pathway. Redox Biol. 2022;50:102235. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 23] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 34. | Awuh JA, Haug M, Mildenberger J, Marstad A, Do CP, Louet C, Stenvik J, Steigedal M, Damås JK, Halaas Ø, Flo TH. Keap1 regulates inflammatory signaling in Mycobacterium avium-infected human macrophages. Proc Natl Acad Sci U S A. 2015;112:E4272-E4280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 35. | Hombach-Klonisch S, Panigrahi S, Rashedi I, Seifert A, Alberti E, Pocar P, Kurpisz M, Schulze-Osthoff K, Mackiewicz A, Los M. Adult stem cells and their trans-differentiation potential--perspectives and therapeutic applications. J Mol Med (Berl). 2008;86:1301-1314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 105] [Cited by in RCA: 98] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 36. | Wang Y, Sun Y, Wang F, Wang H, Hu J. Ferroptosis induction via targeting metabolic alterations in triple-negative breast cancer. Biomed Pharmacother. 2023;169:115866. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 37. | Al-Khani AM, Khalifa MA, Haider KH. Mesenchymal stem cells for cardiac repair. In: Haider KH Handbook of stem cell therapy. Singapore: Springer Nature, 2022: 1-53. |
| 38. | Guo Z, Li CS, Wang CM, Xie YJ, Wang AL. CSE/H2S system protects mesenchymal stem cells from hypoxia and serum deprivationinduced apoptosis via mitochondrial injury, endoplasmic reticulum stress and PI3K/Akt activation pathways. Mol Med Rep. 2015;12:2128-2134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 39. | Kang Y, Zhu R, Li S, Qin KP, Tang H, Shan WS, Yin ZS. Erythropoietin inhibits ferroptosis and ameliorates neurological function after spinal cord injury. Neural Regen Res. 2023;18:881-888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 26] [Reference Citation Analysis (0)] |
| 40. | Xie Q, Sun Y, Xu H, Chen T, Xiang H, Liu H, Wang R, Tan B, Yi Q, Tian J, Zhu J. Ferrostatin-1 improves BMSC survival by inhibiting ferroptosis. Arch Biochem Biophys. 2023;736:109535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 41. | Wang Y, Haider HK, Ahmad N, Ashraf M. Mechanisms by which K(ATP) channel openers produce acute and delayed cardioprotection. Vascul Pharmacol. 2005;42:253-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 42. | Niagara MI, Haider HKh, Jiang S, Ashraf M. Pharmacologically preconditioned skeletal myoblasts are resistant to oxidative stress and promote angiomyogenesis via release of paracrine factors in the infarcted heart. Circ Res. 2007;100:545-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 140] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 43. | Kim HW, Haider HK, Jiang S, Ashraf M. Ischemic preconditioning augments survival of stem cells via miR-210 expression by targeting caspase-8-associated protein 2. J Biol Chem. 2009;284:33161-33168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 270] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 44. | Konoplyannikov M, Haider KH, Lai VK, Ahmed RP, Jiang S, Ashraf M. Activation of diverse signaling pathways by ex-vivo delivery of multiple cytokines for myocardial repair. Stem Cells Dev. 2013;22:204-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 45. | Suzuki T, Yamamoto N, Choi JH, Takano T, Sasaki Y, Terashima Y, Ito A, Dohra H, Hirai H, Nakamura Y, Yano K, Kawagishi H. The biosynthetic pathway of 2-azahypoxanthine in fairy-ring forming fungus. Sci Rep. 2016;6:39087. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 46. | Lu G, Haider HK, Jiang S, Ashraf M. Sca-1+ stem cell survival and engraftment in the infarcted heart: dual role for preconditioning-induced connexin-43. Circulation. 2009;119:2587-2596. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 130] [Cited by in RCA: 116] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 47. | Tabeshmehr P, Husnain HK, Salmannejad M, Sani M, Hosseini SM, Khorraminejad Shirazi MH. Nicorandil potentiates sodium butyrate induced preconditioning of neurons and enhances their survival upon subsequent treatment with H(2)O(2). Transl Neurodegener. 2017;6:29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 48. | Lu G, Haider HKh, Porollo A, Ashraf M. Mitochondria-specific transgenic overexpression of connexin-43 simulates preconditioning-induced cytoprotection of stem cells. Cardiovasc Res. 2010;88:277-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 59] [Article Influence: 3.9] [Reference Citation Analysis (0)] |