Published online Oct 26, 2020. doi: 10.4252/wjsc.v12.i10.1097
Peer-review started: February 26, 2020
First decision: April 9, 2020
Revised: May 13, 2020
Accepted: August 25, 2020
Article in press: August 25, 2020
Published online: October 26, 2020
Processing time: 242 Days and 17.4 Hours
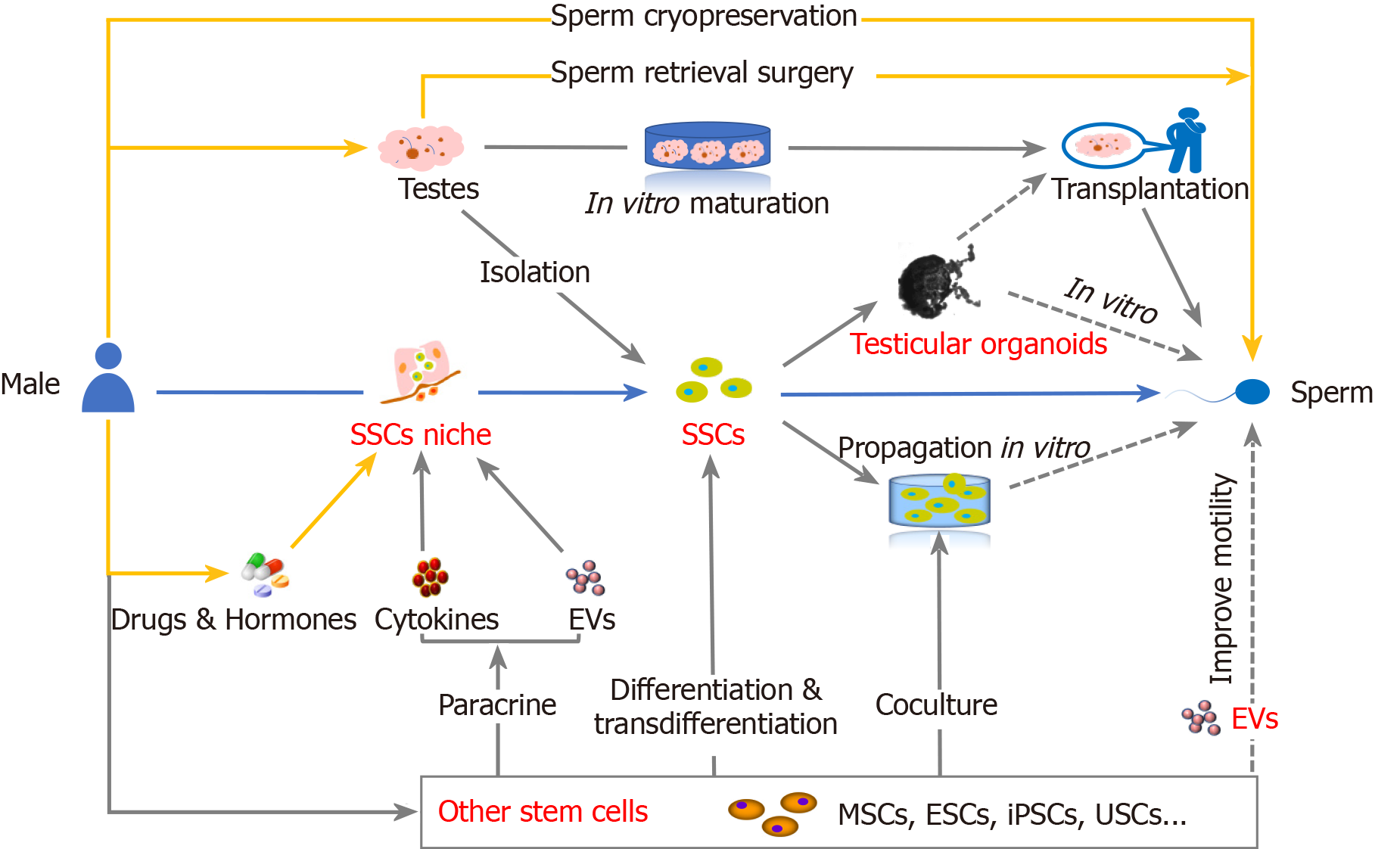
With the decline in male fertility in recent years, strategies for male fertility preservation have received increasing attention. In this study, by reviewing current treatments and recent publications, we describe research progress in and the future directions of stem cell-based therapies for male fertility preservation, focusing on the use of spermatogonial stem cells (SSCs), SSC niches, SSC-based testicular organoids, other stem cell types such as mesenchymal stem cells, and stem cell-derived extracellular vesicles. In conclusion, a more comprehensive understanding of the germ cell microenvironment, stem cell-derived extracellular vesicles, and testicular organoids will play an important role in achieving male fertility preservation.
Core Tip: With the decline in male fertility in recent years, strategies for male fertility preservation have received increasing attention. In this study, by reviewing current treatments and recent publications, we describe research progress in and the future directions of stem cell-based therapies for male fertility preservation, focusing on the use of spermatogonial stem cells (SSCs), SSC niches, SSC-based testicular organoids, other stem cell types such as mesenchymal stem cells, and extracellular vesicles derived from stem cells.
- Citation: Liu HC, Xie Y, Deng CH, Liu GH. Stem cell-based therapies for fertility preservation in males: Current status and future prospects. World J Stem Cells 2020; 12(10): 1097-1112
- URL: https://www.wjgnet.com/1948-0210/full/v12/i10/1097.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v12.i10.1097
The number of patients with cancer continues to increase due to population ageing and growth, and the age at cancer diagnosis is becoming younger[1]. Advances in the treatment of cancers prevalent in childhood, adolescence, and young adulthood have increased 5-year survival rates to greater than 80%[2,3]. Because of these increases in survival and other causes, such as environmental factors[4], immune diseases[5], genetic diseases[6], spermatogenic dysfunction[7], testicular injury[8,9], ageing[10], and delayed childbearing[11], male fertility preservation has gradually become an important issue in the field of human reproduction[12,13]. Male fertility preservation and assisted reproductive technology are medical fields that have attracted much attention in recent years[8,14]. At present, the available methods for preserving male fertility are limited to cryopreservation of sperm and testicular tissue[15,16]. To address all aspects of male fertility preservation, it is necessary to develop related techniques such as male germ cell transplantation, culture, and differentiation[6,17,18]. With the identification and characterization of stem cells, male fertility preservation research based on stem cells, especially spermatogonial stem cells (SSCs), has become popular[7]. This review will elaborate recent research achievements, key areas for the future development of current strategies that can be adopted for fertility preservation, and the role of SSCs, SSC niches, organoids, extracellular vesicles (EVs), and other kinds of stem cells in male fertility preservation (Figure 1).
At present, sperm cryopreservation, sperm retrieval surgery, and drug intervention are the most acceptable methods for fertility preservation[19,20]. The assisted reproductive technology methods of intracytoplasmic sperm injection and sperm cryopreservation have increased the chance of successful conception using stored sperm[21,22]. Testicular tissue cryopreservation is currently proposed to restore fertility in patients from whom mature sperm cannot be collected before puberty. Although this approach has been successful in mice and rhesus macaques, it remains in the experimental stage in humans[23-26].
Currently, hormone therapy is one of the most common drug treatments. Hypogonadism may be due to direct damage to testosterone-producing Leydig cells by chemotherapy, radiotherapy, or surgery and destruction of the hypothalamic-pituitary-adrenal axis by tumour invasion, central nervous system surgery, or radiotherapy[27,28]. Testosterone replacement therapy achieves the best outcomes in inducing or sustaining puberty-related growth, increased bone mass and mental health[29]. Although testosterone produced by Leydig cells mainly acts on Sertoli cells functioning as vegetative germ cells, it cannot induce sperm production[30,31]. In patients with hypogonadism, human chorionic gonadotropin or recombinant follicle-stimulating hormone (FSH) can be administered during puberty to stimulate testicular enlargement[32]. Some researchers have found that FSH use can increase SSC colonization in mammals[33,34].
Oxidative stress is one of the main causes of gonadal toxicity by anticancer therapy[35]. Oxidative stress also aggravates the effects of cell ageing on the male reproductive system[36,37]. Therefore, antioxidants are among the popular drugs under study for use in fertility preservation. The specific antioxidant pathway in SSCs or mesenchymal stem cells (MSCs) is not clear but may involve the inhibition of cellular necrosis and apoptosis. Previous studies have shown that necroptosis in the testis promotes the ageing-related deterioration of the male reproductive system in mice[38]. Our previous study identified a potential method for treating male late-onset hypogonadism by inhibiting the ageing of Leydig cells[39]. Whether fertility is improved by inhibiting testicular ageing or by promoting and maintaining SSC differentiation and proliferation through improvements in the state of the SSC niche requires further study. The roles of other stem cells in promoting growth and prolonging the life cycle have been previously reported[40,41]. Moreover, studies have shown that antioxidants and apoptosis inhibitors affect the enrichment of SSCs in cryopreserved mouse germ cells[42]. Our previous research suggested that suppressing necrotic apoptosis genes may help preserve SSCs and improve male fertility[43]. Vitamin E is also utilized to improve human sperm motility and concentration[44,45]. Levocarnitine is clinically administered to improve asthenospermia and azoospermia[46-48]. Astaxanthin, ellagic acid, lycopene, vitamin C (ascorbic acid), and other drugs have been proven to preserve fertility in animal experiments[49-52]. In addition, some cytoprotective agents have been proven to preserve fertility in animals[53-55].
SSCs are adult stem cells in the testis and the foundation of spermatogenesis; thus, they are essential for male fertility[56]. SSCs are located in the base of seminiferous tubules and are very rare among all male germ cells. They have the ability to differentiate and self-renew in the testis, but the development of appropriate methods for the stable culture and transplantation of isolated SSCs will be an important step in fertility preservation[57,58]. Spermatogenesis in the human testis occurs in a complex microenvironment in which various cells interact through different cytokines. SSCs and spermatogonial cells reside in the base of the seminiferous tubules, where they contact Sertoli cells and peritubular cells (PTCs). Sertoli cells are columnar cells extending from the basement membrane to the lumen of the seminiferous tubules that play a supporting role[59]; considered the most basic components of the testicular microenvironment, these cells secrete important cytokines such as fibroblast growth factor 2, glial cell line-derived neurotrophic factor, activin A, bone morphogenetic factor 4, and stem cell factor[60]. Among these cytokines, glial cell line-derived neurotrophic factor and fibroblast growth factor 2 are considered necessary for maintaining SSC proliferation and differentiation[61,62]. The basement membrane is composed of extracellular matrix proteins, which not only provide structural support but also regulate niches and mediate local cellular signaling by binding and releasing growth factors[63]. Mesenchymal tissue is another key component of the SSC niche, contributing various growth factors and signaling molecules. The stroma is composed of many cell types, including vascular cells, interstitial cells, macrophages, and PTCs. Periductal muscle-like cells are arranged on the outer side of the seminiferous basement membrane, providing structural support, mediating peristalsis, and secreting a variety of cytokines[64,65]. The blood-testis barrier, established by various cell contacts, creates a unique microenvironment and regulates SSC proliferation or differentiation by regulating access to secretions from testicular endothelial cells and interstitial cells[66,67]. Leydig cells and other interstitial cells are also involved in cellular communication within the niche[68-70]. This cell network responds to hormone signals and other signaling in the niche to drive spermatogenesis and testosterone production[7,71,72]. The differences in cellular interactions in the testicular microenvironments of different mammals have not yet been clarified[73], but the testicular microenvironment is essential for spermatogenesis[74].
Brinster et al[75] were the first to successfully use SSCs to restore fertility in mice with busulfan-induced infertility. Through our research, we found that busulfan can be used to generate an ideal animal model of azoospermia[76]. Wyns et al[77] proposed that spermatogenesis recovery can be achieved by injecting isolated SSCs into germ cell-free testes and transplanting testicle fragments containing SSCs. Germ cell-knockout models established with busulfan in bovines, pigs, and dogs show the ability to undergo complete spermatogenesis, but the function of the produced sperm needs to be further evaluated[78-81]. Studies have confirmed that SSC transplantation does not increase the risk of tumor formation or reduce longevity in mice and that the genome of offspring is unchanged[82,83]. Future studies should consider strategies to achieve further improvements in the efficiency of SSC transplantation and reductions in SSC loss[84]. Increasing research results support the potential use of SSCs to restore fertility in clinical applications[85]. At present, it is generally believed that providing a good microenvironment for SSCs can achieve the goal of using these cells for fertility preservation.
The successful and efficient culture of SSCs requires the accurate selection of cells and the implementation of conditions required for SSC growth, including the use of the appropriate medium containing factors such as cytokines and the inclusion of supporting cells[86,87]. In 2003, Kanatsu-Shinohara et al[88] first reported the long-term expansion (more than 5 mo) of mouse SSCs in specific medium and indicated that various specific cytokines were necessary for SSC proliferation and passaging in vitro. Related experiments have since proven that cytokines such as growth factors are indeed necessary to maintain SSC proliferation in vitro[89]. Although mouse SSCs have been successfully cultured, it has been difficult to achieve similar success with human SSCs[90]. Some researchers believe that the coculture of SSCs with isolated testicular cell suspensions enables human SSC proliferation in vitro. This culture method depends on the ability of somatic cells to adhere to the plate while some germ cells remain in suspension, allowing SSC enrichment after differentiation and culture[91,92]. Only a few studies have demonstrated the enrichment of SSCs by quantification in seminiferous tubules after the allotransplantation of in vitro-expanded SSCs[86]. In coculture, the ratio of somatic cells to SSCs affects the proliferation of SSCs[93-95]. Related studies have shown that Dulbecco's modified Eagle’s medium/F12 is a better culture medium[96]. Other researchers who studied the efficiency of selecting germ cells from testicular cells cultured under different conditions did not find any differences in the number of germ cells recovered[90]. Many phenotypic markers have been used to isolate SSCs, such as GPR125[97], CD9[98], SSEA-4[99], and ITGα6[100]. No long-term amplification system for human SSCs has been established; in related research, human SSCs have been cultured and propagated in vitro for just 4 mo[91].
The research and application of organoids remain at initial stages. Organoids have great potential in the study of a wide range of fields, including developmental biology, disease pathology, cell biology, regeneration, precision medicine, drug toxicity, and drug efficacy. These organoids, a kind of in vitro culture system, contain self-renewing stem cells that differentiate into various organ-specific cell types and tissues similar to those in the original organ and can recapitulate some organ functions[101,102]. The testicular microenvironment was originally reconstructed by culturing SSCs in two dimensions (2D) in vitro. Interactions between different cells are necessary to support germ cell development and achieve the culture of testicular structures and tissue. In 1980, Tung et al[103] promoted the reorganization of Sertoli cells and seminiferous tubule-like structures in vitro through the 2D coculture of Sertoli cells and myoid cells in rodents. Tubule formation in these cultures is driven by fibronectin, a component of the basement membrane synthesized by myoid cells that promotes Sertoli cell migration[104]. Some studies have shown that in coculture systems with Vero or Sertoli cells as a feeder layer, round spermatid cells can produce sperm cells with prolonged fertilization ability, and the production efficiency is increased when the cultures are supplemented with FSH[105-107]. Tanaka et al[108] confirmed the process of producing round spermatids from primary spermatocytes cultured with Vero cells. Although these findings indicate the achievement of basic structural reorganization, the development of germ cells is limited. In other words, the progression of spermatogenesis requires a complete system of testicular somatic cells. In 2018, von Kopylow et al[109] cultured various testicular somatic cells for more than 12 wk, but the structure was limited in its ability to support germ cells. Yang et al[110] produced haploid sperm cells in conventional single-cell cultures by stimulating isolated human SSCs with retinoic acid and stem cell factor. Through multidisciplinary cooperation, male reproductive biology research groups have begun to establish and characterize testicular organs. Such multidisciplinary research will be helpful for studying complex cell interactions, growth, preservation, and tissue development and generating drug and toxicity screening models[111].
Compared with 2D culture, 3D culture can meet the requirement of recapitulating the natural physical structure of the human body and the microenvironment with its network of cell-cell interactions[112]. In mammals, 3D culture models have been more effective than 2D culture models[113,114]. In 1954, Trowell et al[115] first immersed semisolid-supported tissue fragments in culture medium to balance nutrient transport with effective gas exchange. Based on this approach, Sato et al[116] achieved complete mouse spermatogenesis in vitro, and sperm with fertilization ability were differentiated from immature mouse testicle fragments and cultured, which proved that spermatozoa can be fully matured by maintaining the natural testicular microenvironment. Lambrot et al[117] also used the gas-liquid interface method to culture human fetal testes with membranes instead of an agar block. After treatment with retinoic acid, the number of germ cells in cultured human fetal testes decreased. In other studies, this semipermeable membrane has been used as a scaffold for the culture of human prepubertal testicular tissue. Although this approach can maintain the somatic microenvironment for testicular fragments, it leads to a decrease in the germ cell population after mitosis and meiosis[118,119].
Another culture method is the hanging drop technique, in which testicular tissue fragments are cultured in a small volume of medium placed on the lid of a culture plate. This method has been used to explore the effects of chemical treatments on human and mouse testes and to study fetal vascularization, morphogenesis, and organogenesis[120,121]. Pendergraft et al[122] used a hanging drop approach to produce a functional testicular organ system by coculture with adult SSCs. Some researchers used this method to observe the mechanism of Zika virus infection in the testis and showed that organ vitality and the expression of spermatogonial and somatic cell markers decreased after infection[123,124].
In conjunction with tissue engineering science, Perrard et al[125] reported a bioreactor system using chitosan water gel tubes in 2016. The system enabled the differentiation of germ cells into morphologically mature sperm. Komeya et al[126] developed a microfluidic device that can maintain mouse testicular tissue and complete spermatogenesis for 6 mo. The steady-state balance between tissue fragments and the culture medium may be a necessary condition for the mature somatic cell microenvironment to promote germ cell differentiation[112]. Alternatively, the cell aggregates themselves can function as a 3D scaffold to support the reorganization of cells into testicular-like structures. In 1981, Zenzes et al[127] cultured isolated rat testicular cells via a rotational culture method to explore the effects of specific cell populations and testicular maturation stages on new tissue formation. In 2013, Yokonishi et al[128] maintained germ cells in vitro and promoted their initial differentiation by using cellular pellets in an air-liquid interface method.
With the 3D culture approach, different support matrices have yielded different effects in testicular culture and organoid research. In 1985, Hadley et al[129] embedded testicular cells in a Matrigel matrix to explore the potential for cell recombination and germ cell differentiation in this 3D scaffold. Thereafter, a calcium alginate matrix[130], collagen matrix[131], poly (D, L-lactic-co-glycolic acid) matrix[132], methylcellulose culture system[133], soft agar culture system, and other soft matrices were used to culture isolated testicular cells[113,134]. In 2017, Alves-Lopes et al[135] used a three-layer gradient system based on the Matrigel matrix as a new platform for studying the microenvironment of SSCs in vitro and looked for novel factors related to germ cell proliferation and differentiation. In 2014, Reuter cultured cells with a collagen sponge and found that the cells colonized the whole scaffold for as long as 35 d, with signs of tubule formation. The cell mass was mainly composed of Sertoli cells and PTCs surrounded by undifferentiated spermatogonia, but no haploid cells were detected, confirming the lack of differentiation[136]. In 2017, Baert et al[137] cultured rat and human testicular cells using an acellular testicular matrix and found that primary human testicular cells formed organ-like organoids in a manner independent of the presence of scaffolding that did not recapitulate the testicular-specific cellular structure in organs.
MSCs, induced pluripotent stem cells (iPSCs), embryonic stem cells (ESCs), and other stem cells have been intensely studied in the field of male fertility preservation. MSCs can be isolated and identified from rodent and human tissues and are considered a potential source of Sertoli cells, Leydig cells, and PTCs in the developing adult testis[138]. Clinical studies on MSCs are relatively extensive and have proven better safety profiles with these cells[139]. MSCs derived from bone marrow, adipose tissue, the umbilical cord, and other fetal sources have been widely accepted as candidate cells for clinical cell therapy[140,141]. Stem cells from different sources are considered to differentiate into embryonic cell lines. In 2006, Nayernia et al[142] first reported that bone marrow-derived MSCs can differentiate towards germ cells in vitro. The injection of MSCs into the testes of busulfan-treated mice led to the production of more seminiferous tubules, which is helpful for rebuilding the SSC niche[143,144]. In 2018, Kadam et al[144] proved that co-transplantation with MSCs improves the transplantation efficiency of SSCs. Leydig cells and Sertoli cells in the testes of cancer patients are damaged to varying degrees after chemotherapy, so the application of MSCs as supporting cells and interstitial cells can improve the effects of SSC transplantation[145-148]. Therefore, it must be determined whether stem cells cocultured with SSCs produce functional sperm. The high self-renewal capacity, multilineage differentiation potential, and immunomodulatory properties of MSCs make them an attractive tool for research and clinical applications[149]. Other stem cells may also have great application potential, but this hypothesis needs to be supported by further experimental evidence. The paracrine effects of MSCs on cell survival, immune regulation, cell migration, angiogenesis, cell proliferation, and antioxidant effects are key issues related to the use of stem cells for the preservation and promotion of male fertility[150,151]. An article reviewing the role of human umbilical cord perivascular cells (HUCPVCs) in male fertility preservation suggests that HUCPVCs have broad development prospects[7]. First, the umbilical cord source is associated with high immunity[147,152,153]. These cells share characteristics with MSCs, including cell surface markers related to MSCs and pericytes; have the ability to differentiate into cartilage and undergo adipogenesis and osteogenesis in vitro; and show multidirectional differentiation potential[154]. Similar to other MSCs, HUCPVCs express and secrete many cytokines related to cell proliferation, survival, chemotaxis, angiogenesis, immune regulation, and the beneficial modulation of the local microenvironment[155-157].
In 2006, researchers discovered that pluripotent stem cells can be isolated and expanded via somatic cell reprogramming[158]. In the last decade, pluripotent stem cells have become the focus of medical research[159]. iPSCs and ESCs have shown great clinical potential[160]. In 2004, Clark et al[161] observed the expression of Ribonucleic Acid (RNAs) and proteins indicative of mature germ cells, providing evidence that ESCs can be transformed into germ cells. In 2006, Nayernia et al[162] bred offspring using spermatozoa differentiated from mouse ESCs. In 2016, Zhou et al[163] completely reproduced meiosis in vitro and produced euploid fertile offspring. Although these cells show good applicability, ethical and other considerations limit the further clinical development and application of ESCs[164]. Currently, some researchers believe that very small embryonic-like stem cells can undergo in vitro differentiation and assist in fertility preservation, but this has not been studied[165,166]. The methods for fertility promotion and preservation involving iPSCs include obtaining primordial germ cells from somatic cells of a patient and differentiating these cells into Sertoli cells and Leydig cells, as testicular microenvironment support, to promote the proliferation and differentiation of SSCs[167-169] into gametes in vitro[170,171]. In 2011, Eguizabal et al[172] obtained haploid cells that completed meiosis from iPSCs. In recent years, some researchers have differentiated human germ cells from iPSCs and ESCs, but the differentiation efficiency is low, and the resultant differentiation is still insufficient[173-175]. In addition, genetic and epigenetic mutations in iPSCs that arise during reprogramming and proliferation must be further explored[176].
Originally, terms such as EVs, exosomes, and microvesicles were not strictly defined in the literature and were often used as synonyms[177,178]. As important components of the paracrine system, these structures carry cargo such as microRNAs, mRNA, proteins, and lipids to target cells[179]. Subsequent publications established three categories of EVs: Apoptotic bodies (1–5 μm), shedding microvesicles (200–1000 nm), and exosomes (30–200 nm)[180]. Exosomes, with a diameter of approximately 30 nm to 200 nm, can more readily pass through the blood-brain barrier to play a therapeutic role[181]. Human semen contains a high concentration of EVs that promote sperm function in various ways, such as improving sperm motility, regulating acrosome activity, and affecting the fertilization process[182]. Related studies have proven that exosomes can affect semen quality and enter sperm, thereby enhancing sperm motor ability and capacitation after ejaculation[183]. Studies have shown that seminal plasma exosomes regulate sperm motility and mitochondrial metabolism in mammals[184]. The epididymis plays an important role in sperm maturation in the male reproductive tract, and male sperm rely heavily on interactions with epididymal epithelial secretions[185]. Epididymal and prostate exosomes are thought to be closely related to the later stages of sperm maturation[186-188]. Maturing sperm mix with the fluid secreted by each gonad throughout the ejaculation process[189]. Exosomes are also very important for cellular communication[190]. In 2014, Vojtech et al[191] demonstrated that small RNAs carried by exosomes in semen exhibit signal-regulating function. Related studies have shown that in genitourinary diseases, the biological information carried by exosomes can function as a biomarker of prostate cancer, bladder cancer, kidney cancer, and other diseases[192-195]. The relationship between sperm RNA and male infertility has been studied and proven to play a role in predicting health and individual outcomes of different fertility treatments[196,197]. Therefore, it is reasonable to consider that a patient’s semen quality can be determined by exosome analysis or that treatments for male infertility can involve exosomes[198,199]. Exosomes in the vascular, skeletal, and nervous systems have received widespread attention in relation to tissue reconstruction and regeneration, but there have been fewer studies on the preservation of male fertility[200]. Therapeutic drug delivery by MSC exosomes is an emerging research direction[201]. As the stem cell type with the most abundant in-depth research and most extensive sources, MSCs are widely used in many kinds of experiments[202]. MSC-derived exosomes have been shown to improve various diseases[203], for example, to protect against renal injury[204], repair the cornea[205], and improve some inflammatory diseases[206]. Exosomes derived from other types of stem cells, such as oral, adipose, and urine-derived stem cells, are increasingly being used in the study of diseases[207-209]. Our recent study showed that urine-derived stem cells can restore spermatogenesis in busulfan-induced nonobstructive azoospermic mouse models through paracrine exosomes[210]. Therefore, the role of exosomes secreted by various types of stem cells in preserving male fertility requires more in-depth study. With the rapid development of tissue engineering technology, one future focus is to improve sperm function and promote male fertility preservation through the use of exosomes[198].
The efficiency of SSC proliferation and culture remains low. The ability to rebuild the microenvironment, especially the SSC niche, will be key to promoting sustained SSC proliferation and differentiation into sperm. Further research is needed to ascertain how to promote SSC proliferation and maintain their original function after transplantation. There has been recent progress in understanding the testicular tissue microenvironment and recapitulating this microenvironment by growing different cells in a supporting matrix. Although considerable progress has been made, achieving full human spermatogenesis and mature sperm production with fertilization capability will require the creation of a complete testicular microenvironment in which immature testicular tissues can mature and SSCs can proliferate and differentiate into mature sperm. With the combination of testicular organoids and tissue engineering, the use of emerging technologies such as 3D printing to create functional human testicular substitutes is another potential direction of future development. A new type of micromodel, the “organoid-on-a-chip” concept, has been recently proposed[211]. This chip is used to simulate the smallest functional, structural unit of an organ and has potential use in drug screening and disease modelling[212,213]. Recent in vitro cell experiments have proven that the toxicity of various drugs to the testis imposes obvious limitations[122,214]. Further scientific efforts are needed to determine whether it is possible to simulate spermatogenic functional units in vivo by building a “testicular chip” to conduct drug screening and build disease models. The powerful role of stem cell differentiation and paracrine function in organoid formation and maintenance needs to be further explored. Paracrine exosomes have been proven to have beneficial therapeutic and diagnostic effects in other areas, but research on their use for male fertility preservation remains in the earliest stage. For this reason, it is necessary to further explore the supportive role of exosomes in the SSC niche, especially regarding whether exosomes can improve sperm motility and maturation in oligospermia or asthenospermia. Multidisciplinary cooperation will result in more diverse, stem cell-based experiments and provide strong support for future medical development.
The issues with fertility preservation based on stem cells have been widely studied. Research in this field has resulted in great achievements in testicular tissue cryopreservation and transplantation, SSC culture and transplantation, in vitro sperm production, and organoid generation. However, the efficiency, final outcomes, and safety of each experimental method need to be further evaluated. A more comprehensive understanding of the regulation of the germ cell microenvironment will play an important role in culturing SSCs and inducing their proliferation and differentiation in vitro. At the same time, the role of exosomes in sperm maturation and the testicular microenvironment is receiving increasing attention. Sperm maturation based on exosome approaches, the differentiation and proliferation of SSCs, and other fertility preservation-related topics may become popular in future research.
Manuscript source: Invited manuscript
Specialty type: Cell biology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Giménez-Bonafé P, Ku S S-Editor: Zhang L L-Editor: Wang TQ P-Editor: Li JH
| 1. | Miller KD, Nogueira L, Mariotto AB, Rowland JH, Yabroff KR, Alfano CM, Jemal A, Kramer JL, Siegel RL. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69:363-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2417] [Cited by in RCA: 3074] [Article Influence: 512.3] [Reference Citation Analysis (0)] |
| 2. | Skinner R, Mulder RL, Kremer LC, Hudson MM, Constine LS, Bardi E, Boekhout A, Borgmann-Staudt A, Brown MC, Cohn R, Dirksen U, Giwercman A, Ishiguro H, Jahnukainen K, Kenney LB, Loonen JJ, Meacham L, Neggers S, Nussey S, Petersen C, Shnorhavorian M, van den Heuvel-Eibrink MM, van Santen HM, Wallace WH, Green DM. Recommendations for gonadotoxicity surveillance in male childhood, adolescent, and young adult cancer survivors: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group in collaboration with the PanCareSurFup Consortium. Lancet Oncol. 2017;18:e75-e90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 114] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 3. | Gatta G, Zigon G, Capocaccia R, Coebergh JW, Desandes E, Kaatsch P, Pastore G, Peris-Bonet R, Stiller CA; EUROCARE Working Group. Survival of European children and young adults with cancer diagnosed 1995-2002. Eur J Cancer. 2009;45:992-1005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 413] [Cited by in RCA: 389] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 4. | Levine H, Jørgensen N, Martino-Andrade A, Mendiola J, Weksler-Derri D, Mindlis I, Pinotti R, Swan SH. Temporal trends in sperm count: a systematic review and meta-regression analysis. Hum Reprod Update. 2017;23:646-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 567] [Cited by in RCA: 823] [Article Influence: 117.6] [Reference Citation Analysis (0)] |
| 5. | Suehiro RM, Borba EF, Bonfa E, Okay TS, Cocuzza M, Soares PM, Silva CA. Testicular Sertoli cell function in male systemic lupus erythematosus. Rheumatology (Oxford). 2008;47:1692-1697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Giudice MG, Del Vento F, Wyns C. Male fertility preservation in DSD, XXY, pre-gonadotoxic treatments - Update, methods, ethical issues, current outcomes, future directions. Best Pract Res Clin Endocrinol Metab. 2019;33:101261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Gauthier-Fisher A, Kauffman A, Librach CL. Potential use of stem cells for fertility preservation. Andrology. 2020;8:862-878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 8. | Jensen JR, Morbeck DE, Coddington CC 3rd. Fertility preservation. Mayo Clin Proc. 2011;86:45-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 9. | Song SH, Chiba K, Ramasamy R, Lamb DJ. Recent advances in the genetics of testicular failure. Asian J Androl. 2016;18:350-355. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 10. | Stone BA, Alex A, Werlin LB, Marrs RP. Age thresholds for changes in semen parameters in men. Fertil Steril. 2013;100:952-958. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 132] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 11. | Harris ID, Fronczak C, Roth L, Meacham RB. Fertility and the aging male. Rev Urol. 2011;13:e184-e190. [PubMed] |
| 12. | Barratt CLR, Björndahl L, De Jonge CJ, Lamb DJ, Osorio Martini F, McLachlan R, Oates RD, van der Poel S, St John B, Sigman M, Sokol R, Tournaye H. The diagnosis of male infertility: an analysis of the evidence to support the development of global WHO guidance-challenges and future research opportunities. Hum Reprod Update. 2017;23:660-680. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 283] [Cited by in RCA: 299] [Article Influence: 37.4] [Reference Citation Analysis (0)] |
| 13. | Krausz C. Male infertility: pathogenesis and clinical diagnosis. Best Pract Res Clin Endocrinol Metab. 2011;25:271-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 389] [Cited by in RCA: 332] [Article Influence: 23.7] [Reference Citation Analysis (0)] |
| 14. | Nieschlag E, Lenzi A. The conventional management of male infertility. Int J Gynaecol Obstet. 2013;123 Suppl 2:S31-S35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 15. | Picton HM, Wyns C, Anderson RA, Goossens E, Jahnukainen K, Kliesch S, Mitchell RT, Pennings G, Rives N, Tournaye H, van Pelt AM, Eichenlaub-Ritter U, Schlatt S; ESHRE Task Force On Fertility Preservation In Severe Diseases. A European perspective on testicular tissue cryopreservation for fertility preservation in prepubertal and adolescent boys. Hum Reprod. 2015;30:2463-2475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 229] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 16. | García A, Herrero MB, Holzer H, Tulandi T, Chan P. Assisted reproductive outcomes of male cancer survivors. J Cancer Surviv. 2015;9:208-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 17. | Gassei K, Orwig KE. Experimental methods to preserve male fertility and treat male factor infertility. Fertil Steril. 2016;105:256-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 86] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 18. | Wyns C, Van Langendonckt A, Wese FX, Donnez J, Curaba M. Long-term spermatogonial survival in cryopreserved and xenografted immature human testicular tissue. Hum Reprod. 2008;23:2402-2414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 151] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 19. | Kenney LB, Antal Z, Ginsberg JP, Hoppe BS, Bober SL, Yu RN, Constine LS, van Santen HM, Skinner R, Green DM. Improving Male Reproductive Health After Childhood, Adolescent, and Young Adult Cancer: Progress and Future Directions for Survivorship Research. J Clin Oncol. 2018;36:2160-2168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 20. | Rabaça A, Sousa M, Alves MG, Oliveira PF, Sá R. Novel Drug Therapies for Fertility Preservation in Men Undergoing Chemotherapy: Clinical Relevance of Protector Agents. Curr Med Chem. 2015;22:3347-3369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Feldschuh J, Brassel J, Durso N, Levine A. Successful sperm storage for 28 years. Fertil Steril. 2005;84:1017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 59] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 22. | Podsiadly BT, Woolcott RJ, Stanger JD, Stevenson K. Pregnancy resulting from intracytoplasmic injection of cryopreserved spermatozoa recovered from testicular biopsy. Hum Reprod. 1996;11:1306-1308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Brinster RL, Zimmermann JW. Spermatogenesis following male germ-cell transplantation. Proc Natl Acad Sci USA. 1994;91:11298-11302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1102] [Cited by in RCA: 1082] [Article Influence: 34.9] [Reference Citation Analysis (0)] |
| 24. | Bahadur G, Chatterjee R, Ralph D. Testicular tissue cryopreservation in boys. Ethical and legal issues: case report. Hum Reprod. 2000;15:1416-1420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 69] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Brinster RL. Male germline stem cells: from mice to men. Science. 2007;316:404-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 202] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 26. | Fayomi AP, Peters K, Sukhwani M, Valli-Pulaski H, Shetty G, Meistrich ML, Houser L, Robertson N, Roberts V, Ramsey C, Hanna C, Hennebold JD, Dobrinski I, Orwig KE. Autologous grafting of cryopreserved prepubertal rhesus testis produces sperm and offspring. Science. 2019;363:1314-1319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 226] [Article Influence: 37.7] [Reference Citation Analysis (0)] |
| 27. | Mostoufi-Moab S, Seidel K, Leisenring WM, Armstrong GT, Oeffinger KC, Stovall M, Meacham LR, Green DM, Weathers R, Ginsberg JP, Robison LL, Sklar CA. Endocrine Abnormalities in Aging Survivors of Childhood Cancer: A Report From the Childhood Cancer Survivor Study. J Clin Oncol. 2016;34:3240-3247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 132] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 28. | Howell SJ, Shalet SM. Effect of cancer therapy on pituitary-testicular axis. Int J Androl. 2002;25:269-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 50] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 29. | Watson S, Fuqua JS, Lee PA. Treatment of hypogonadism in males. Pediatr Endocrinol Rev. 2014;11 Suppl 2:230-239. [PubMed] |
| 30. | Griswold MD. The central role of Sertoli cells in spermatogenesis. Semin Cell Dev Biol. 1998;9:411-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 560] [Cited by in RCA: 610] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 31. | Walker WH. Molecular mechanisms of testosterone action in spermatogenesis. Steroids. 2009;74:602-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 136] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 32. | Rohayem J, Hauffa BP, Zacharin M, Kliesch S, Zitzmann M; “German Adolescent Hypogonadotropic Hypogonadism Study Group”. Testicular growth and spermatogenesis: new goals for pubertal hormone replacement in boys with hypogonadotropic hypogonadism? Clin Endocrinol (Oxf). 2017;86:75-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 93] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 33. | Narenji Sani R, Tajik P, Yousefi MH, Movahedin M, Qasemi-Panahi B, Shafiei S, Ahmadi Hamedani M. Follicle stimulating hormone increases spermatogonial stem cell colonization during in vitro co-culture. Vet Res Forum. 2013;4:37-41. [PubMed] |
| 34. | Tajik P, Sani RN, Moezifar M, Yousefi MH, Movahedin M, Qasemi-Panahi B, Shafiei S, Fili PR. Effect of follicle-stimulating hormone and testosterone on colony formation of bovine spermatogonial stem cell. Comp Clin Path 2014; 23: 901-906. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 35. | Chen Y, Jungsuwadee P, Vore M, Butterfield DA, St Clair DK. Collateral damage in cancer chemotherapy: oxidative stress in nontargeted tissues. Mol Interv. 2007;7:147-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 281] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 36. | Noblanc A, Klaassen A, Robaire B. The Exacerbation of Aging and Oxidative Stress in the Epididymis of Sod1 Null Mice. Antioxidants (Basel). 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 37. | Terman A, Brunk UT. Oxidative stress, accumulation of biological 'garbage', and aging. Antioxid Redox Signal. 2006;8:197-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 269] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 38. | Li D, Meng L, Xu T, Su Y, Liu X, Zhang Z, Wang X. RIPK1-RIPK3-MLKL-dependent necrosis promotes the aging of mouse male reproductive system. Elife. 2017;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 70] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 39. | Zhang C, Xie Y, Chen H, Lv L, Yao J, Zhang M, Xia K, Feng X, Li Y, Liang X, Sun X, Deng C, Liu G. FOXO4-DRI alleviates age-related testosterone secretion insufficiency by targeting senescent Leydig cells in aged mice. Aging (Albany NY). 2020;12:1272-1284. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 40. | Lin TM, Tsai JL, Lin SD, Lai CS, Chang CC. Accelerated growth and prolonged lifespan of adipose tissue-derived human mesenchymal stem cells in a medium using reduced calcium and antioxidants. Stem Cells Dev. 2005;14:92-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 163] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 41. | Choi KM, Seo YK, Yoon HH, Song KY, Kwon SY, Lee HS, Park JK. Effect of ascorbic acid on bone marrow-derived mesenchymal stem cell proliferation and differentiation. J Biosci Bioeng. 2008;105:586-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 211] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 42. | Ha SJ, Kim BG, Lee YA, Kim YH, Kim BJ, Jung SE, Pang MG, Ryu BY. Effect of Antioxidants and Apoptosis Inhibitors on Cryopreservation of Murine Germ Cells Enriched for Spermatogonial Stem Cells. PLoS One. 2016;11:e0161372. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 43. | Xie Y, Chen H, Luo D, Yang X, Yao J, Zhang C, Lv L, Guo Z, Deng C, Li Y, Liang X, Deng C, Sun X, Liu G. Inhibiting Necroptosis of Spermatogonial Stem Cell as a Novel Strategy for Male Fertility Preservation. Stem Cells Dev. 2020;29:475-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 44. | Vézina D, Mauffette F, Roberts KD, Bleau G. Selenium-vitamin E supplementation in infertile men. Effects on semen parameters and micronutrient levels and distribution. Biol Trace Elem Res. 1996;53:65-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 47] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 45. | Moslemi MK, Tavanbakhsh S. Selenium-vitamin E supplementation in infertile men: effects on semen parameters and pregnancy rate. Int J Gen Med. 2011;4:99-104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 111] [Cited by in RCA: 128] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 46. | Khademi A, Alleyassin A, Safdarian L, Hamed EA, Rabiee E, Haghaninezhad H. The effects of L-carnitine on sperm parameters in smoker and non-smoker patients with idiopathic sperm abnormalities. J Assist Reprod Genet. 2005;22:395-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 47. | Zhou X, Liu F, Zhai S. Effect of L-carnitine and/or L-acetyl-carnitine in nutrition treatment for male infertility: a systematic review. Asia Pac J Clin Nutr. 2007;16 Suppl 1:383-390. [PubMed] |
| 48. | Cavallini G, Ferraretti AP, Gianaroli L, Biagiotti G, Vitali G. Cinnoxicam and L-carnitine/acetyl-L-carnitine treatment for idiopathic and varicocele-associated oligoasthenospermia. J Androl. 2004;25:761-70; discussion 771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 83] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 49. | Tripathi DN, Jena GB. Astaxanthin inhibits cytotoxic and genotoxic effects of cyclophosphamide in mice germ cells. Toxicology. 2008;248:96-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 101] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 50. | Türk G, Sönmez M, Ceribaşi AO, Yüce A, Ateşşahin A. Attenuation of cyclosporine A-induced testicular and spermatozoal damages associated with oxidative stress by ellagic acid. Int Immunopharmacol. 2010;10:177-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 51] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 51. | Ateşşahin A, Karahan I, Türk G, Gür S, Yilmaz S, Ceribaşi AO. Protective role of lycopene on cisplatin-induced changes in sperm characteristics, testicular damage and oxidative stress in rats. Reprod Toxicol. 2006;21:42-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 163] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 52. | Ahmed EA, Omar HM, elghaffar SKh, Ragb SM, Nasser AY. The antioxidant activity of vitamin C, DPPD and L-cysteine against Cisplatin-induced testicular oxidative damage in rats. Food Chem Toxicol. 2011;49:1115-1121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 54] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 53. | Carmely A, Meirow D, Peretz A, Albeck M, Bartoov B, Sredni B. Protective effect of the immunomodulator AS101 against cyclophosphamide-induced testicular damage in mice. Hum Reprod. 2009;24:1322-1329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 36] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 54. | Lirdi LC, Stumpp T, Sasso-Cerri E, Miraglia SM. Amifostine protective effect on cisplatin-treated rat testis. Anat Rec (Hoboken). 2008;291:797-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 69] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 55. | Vendramini V, Sasso-Cerri E, Miraglia SM. Amifostine reduces the seminiferous epithelium damage in doxorubicin-treated prepubertal rats without improving the fertility status. Reprod Biol Endocrinol. 2010;8:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 62] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 56. | Fayomi AP, Orwig KE. Spermatogonial stem cells and spermatogenesis in mice, monkeys and men. Stem Cell Res. 2018;29:207-214. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 143] [Cited by in RCA: 253] [Article Influence: 36.1] [Reference Citation Analysis (1)] |
| 57. | Clermont Y. Kinetics of spermatogenesis in mammals: seminiferous epithelium cycle and spermatogonial renewal. Physiol Rev. 1972;52:198-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 891] [Cited by in RCA: 853] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 58. | Vermeulen M, Giudice MG, Del Vento F, Wyns C. Role of stem cells in fertility preservation: current insights. Stem Cells Cloning. 2019;12:27-48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 59. | Mruk DD, Cheng CY. In vitro regulation of extracellular superoxide dismutase in sertoli cells. Life Sci. 2000;67:133-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 60. | de Rooij DG. The spermatogonial stem cell niche. Microsc Res Tech. 2009;72:580-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 132] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 61. | Meng X, Lindahl M, Hyvönen ME, Parvinen M, de Rooij DG, Hess MW, Raatikainen-Ahokas A, Sainio K, Rauvala H, Lakso M, Pichel JG, Westphal H, Saarma M, Sariola H. Regulation of cell fate decision of undifferentiated spermatogonia by GDNF. Science. 2000;287:1489-1493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1003] [Cited by in RCA: 985] [Article Influence: 39.4] [Reference Citation Analysis (0)] |
| 62. | Takashima S, Kanatsu-Shinohara M, Tanaka T, Morimoto H, Inoue K, Ogonuki N, Jijiwa M, Takahashi M, Ogura A, Shinohara T. Functional differences between GDNF-dependent and FGF2-dependent mouse spermatogonial stem cell self-renewal. Stem Cell Reports. 2015;4:489-502. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 130] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 63. | Hynes RO. The extracellular matrix: not just pretty fibrils. Science. 2009;326:1216-1219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2554] [Cited by in RCA: 2448] [Article Influence: 153.0] [Reference Citation Analysis (0)] |
| 64. | Mayerhofer A, Walenta L, Mayer C, Eubler K, Welter H. Human testicular peritubular cells, mast cells and testicular inflammation. Andrologia. 2018;50:e13055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 65. | Chen LY, Brown PR, Willis WB, Eddy EM. Peritubular myoid cells participate in male mouse spermatogonial stem cell maintenance. Endocrinology. 2014;155:4964-4974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 93] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 66. | Bhang DH, Kim BJ, Kim BG, Schadler K, Baek KH, Kim YH, Hsiao W, Ding BS, Rafii S, Weiss MJ, Chou ST, Kolon TF, Ginsberg JP, Ryu BY, Ryeom S. Testicular endothelial cells are a critical population in the germline stem cell niche. Nat Commun. 2018;9:4379. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 97] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 67. | Yoshida S, Sukeno M, Nabeshima Y. A vasculature-associated niche for undifferentiated spermatogonia in the mouse testis. Science. 2007;317:1722-1726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 366] [Cited by in RCA: 343] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 68. | Oatley JM, Oatley MJ, Avarbock MR, Tobias JW, Brinster RL. Colony stimulating factor 1 is an extrinsic stimulator of mouse spermatogonial stem cell self-renewal. Development. 2009;136:1191-1199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 237] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 69. | Hume DA, Halpin D, Charlton H, Gordon S. The mononuclear phagocyte system of the mouse defined by immunohistochemical localization of antigen F4/80: macrophages of endocrine organs. Proc Natl Acad Sci USA. 1984;81:4174-4177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 161] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 70. | Hutson JC. Physiologic interactions between macrophages and Leydig cells. Exp Biol Med (Maywood). 2006;231:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 92] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 71. | Sakib S, Goldsmith T, Voigt A, Dobrinski I. Testicular organoids to study cell-cell interactions in the mammalian testis. Andrology. 2020;8:835-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 72. | Li L, Xie T. Stem cell niche: structure and function. Annu Rev Cell Dev Biol. 2005;21:605-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 854] [Cited by in RCA: 815] [Article Influence: 42.9] [Reference Citation Analysis (0)] |
| 73. | Mayerhofer A. Human testicular peritubular cells: more than meets the eye. Reproduction. 2013;145:R107-R116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 102] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 74. | Ryu BY, Orwig KE, Oatley JM, Avarbock MR, Brinster RL. Effects of aging and niche microenvironment on spermatogonial stem cell self-renewal. Stem Cells. 2006;24:1505-1511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 194] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 75. | Brinster RL, Avarbock MR. Germline transmission of donor haplotype following spermatogonial transplantation. Proc Natl Acad Sci USA. 1994;91:11303-11307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 811] [Cited by in RCA: 767] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 76. | Xie Y, Deng CC, Ouyang B, Lv LY, Yao JH, Zhang C, Chen HC, Li XY, Sun XZ, Deng CH, Liu GH. Establishing a nonlethal and efficient mouse model of male gonadotoxicity by intraperitoneal busulfan injection. Asian J Androl. 2020;22:184-191. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 77. | Wyns C, Curaba M, Vanabelle B, Van Langendonckt A, Donnez J. Options for fertility preservation in prepubertal boys. Hum Reprod Update 2010; 16: 312-328. [RCA] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 207] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 78. | Izadyar F, Den Ouden K, Stout TA, Stout J, Coret J, Lankveld DP, Spoormakers TJ, Colenbrander B, Oldenbroek JK, Van der Ploeg KD, Woelders H, Kal HB, De Rooij DG. Autologous and homologous transplantation of bovine spermatogonial stem cells. Reproduction. 2003;126:765-774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 129] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 79. | Mikkola M, Sironen A, Kopp C, Taponen J, Sukura A, Vilkki J, Katila T, Andersson M. Transplantation of normal boar testicular cells resulted in complete focal spermatogenesis in a boar affected by the immotile short-tail sperm defect. Reprod Domest Anim. 2006;41:124-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 59] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 80. | Kim Y, Turner D, Nelson J, Dobrinski I, McEntee M, Travis AJ. Production of donor-derived sperm after spermatogonial stem cell transplantation in the dog. Reproduction. 2008;136:823-831. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 88] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 81. | Ganguli N, Wadhwa N, Usmani A, Kunj N, Ganguli N, Sarkar RK, Ghorai SM, Majumdar SS. An efficient method for generating a germ cell depleted animal model for studies related to spermatogonial stem cell transplantation. Stem Cell Res Ther. 2016;7:142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 82. | Mulder CL, Catsburg LAE, Zheng Y, de Winter-Korver CM, van Daalen SKM, van Wely M, Pals S, Repping S, van Pelt AMM. Long-term health in recipients of transplanted in vitro propagated spermatogonial stem cells. Hum Reprod. 2018;33:81-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 83. | Goossens E, de Vos P, Tournaye H. Array comparative genomic hybridization analysis does not show genetic alterations in spermatozoa and offspring generated after spermatogonial stem cell transplantation in the mouse. Hum Reprod. 2010;25:1836-1842. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 84. | Faes K, Lahoutte T, Hoorens A, Tournaye H, Goossens E. In search of an improved injection technique for the clinical application of spermatogonial stem cell transplantation. Reprod Biomed Online. 2017;34:291-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 85. | Kilcoyne KR, Mitchell RT. FERTILITY PRESERVATION: Testicular transplantation for fertility preservation: clinical potential and current challenges. Reproduction. 2019;158:F1-F14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 86. | Nickkholgh B, Mizrak SC, Korver CM, van Daalen SK, Meissner A, Repping S, van Pelt AM. Enrichment of spermatogonial stem cells from long-term cultured human testicular cells. Fertil Steril 2014; 102: 558-565. e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 87. | Nickkholgh B, Mizrak SC, van Daalen SK, Korver CM, Sadri-Ardekani H, Repping S, van Pelt AM. Genetic and epigenetic stability of human spermatogonial stem cells during long-term culture. Fertil Steril 2014; 102: 1700-7. e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 88. | Kanatsu-Shinohara M, Ogonuki N, Inoue K, Miki H, Ogura A, Toyokuni S, Shinohara T. Long-term proliferation in culture and germline transmission of mouse male germline stem cells. Biol Reprod. 2003;69:612-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 764] [Cited by in RCA: 758] [Article Influence: 34.5] [Reference Citation Analysis (0)] |
| 89. | Kubota H, Avarbock MR, Brinster RL. Growth factors essential for self-renewal and expansion of mouse spermatogonial stem cells. Proc Natl Acad Sci USA. 2004;101:16489-16494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 733] [Cited by in RCA: 716] [Article Influence: 34.1] [Reference Citation Analysis (0)] |
| 90. | Medrano JV, Rombaut C, Simon C, Pellicer A, Goossens E. Human spermatogonial stem cells display limited proliferation in vitro under mouse spermatogonial stem cell culture conditions. Fertil Steril 2016; 106: 1539-1549. e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 56] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 91. | Sadri-Ardekani H, Mizrak SC, van Daalen SK, Korver CM, Roepers-Gajadien HL, Koruji M, Hovingh S, de Reijke TM, de la Rosette JJ, van der Veen F, de Rooij DG, Repping S, van Pelt AM. Propagation of human spermatogonial stem cells in vitro. JAMA. 2009;302:2127-2134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 255] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 92. | Sadri-Ardekani H, Akhondi MA, van der Veen F, Repping S, van Pelt AM. In vitro propagation of human prepubertal spermatogonial stem cells. JAMA. 2011;305:2416-2418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 155] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 93. | Cai H, Wu JY, An XL, Zhao XX, Wang ZZ, Tang B, Yue ZP, Li ZY, Zhang XM. Enrichment and culture of spermatogonia from cryopreserved adult bovine testis tissue. Anim Reprod Sci. 2016;166:109-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 94. | Gat I, Maghen L, Filice M, Kenigsberg S, Wyse B, Zohni K, Saraz P, Fisher AG, Librach C. Initial germ cell to somatic cell ratio impacts the efficiency of SSC expansion in vitro. Syst Biol Reprod Med. 2018;64:39-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 95. | Gat I, Maghen L, Shlush E, Quach K, Gauthier-Fisher AS, Lo K, Librach C. In vitro testicular niche modelling: The ratio of spermatogonial stem cells (sscs) to supporting somatic cells is critical for optimal ssc proliferation in vitro. Fertil Steril 2015; 104: e91. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 96. | Gat I, Maghen L, Filice M, Wyse B, Zohni K, Jarvi K, Lo KC, Gauthier Fisher A, Librach C. Optimal culture conditions are critical for efficient expansion of human testicular somatic and germ cells in vitro. Fertil Steril 2017; 107: 595-605. e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 97. | Guo Y, Liu L, Sun M, Hai Y, Li Z, He Z. Expansion and long-term culture of human spermatogonial stem cells via the activation of SMAD3 and AKT pathways. Exp Biol Med (Maywood). 2015;240:1112-1122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 98. | Lim JJ, Sung SY, Kim HJ, Song SH, Hong JY, Yoon TK, Kim JK, Kim KS, Lee DR. Long-term proliferation and characterization of human spermatogonial stem cells obtained from obstructive and non-obstructive azoospermia under exogenous feeder-free culture conditions. Cell Prolif. 2010;43:405-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 88] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 99. | Kokkinaki M, Djourabtchi A, Golestaneh N. Long-term Culture of Human SSEA-4 Positive Spermatogonial Stem Cells (SSCs). J Stem Cell Res Ther. 2011;2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 100. | Shiva R, Ghasem S, Masoud H, Sadat KL, Ali K, Reza DM. Comparison of colony formation of human spermatogonial stem cells (SSCs) with and without collagen. J Pak Med Assoc. 2016;66:285-291. [PubMed] |
| 101. | Sato T, Clevers H. Growing self-organizing mini-guts from a single intestinal stem cell: mechanism and applications. Science. 2013;340:1190-1194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 803] [Cited by in RCA: 878] [Article Influence: 73.2] [Reference Citation Analysis (0)] |
| 102. | Huch M, Koo BK. Modeling mouse and human development using organoid cultures. Development. 2015;142:3113-3125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 349] [Cited by in RCA: 366] [Article Influence: 36.6] [Reference Citation Analysis (0)] |
| 103. | Tung PS, Fritz IB. Interactions of sertoli cells with myoid cells in vitro. Biol Reprod. 1980;23:207-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 79] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 104. | Richardson LL, Kleinman HK, Dym M. Basement membrane gene expression by Sertoli and peritubular myoid cells in vitro in the rat. Biol Reprod. 1995;52:320-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 75] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 105. | Cremades N, Bernabeu R, Barros A, Sousa M. In-vitro maturation of round spermatids using co-culture on Vero cells. Hum Reprod. 1999;14:1287-1293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 78] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 106. | Tesarik J, Greco E, Rienzi L, Ubaldi F, Guido M, Cohen-Bacrie P, Mendoza C. Differentiation of spermatogenic cells during in-vitro culture of testicular biopsy samples from patients with obstructive azoospermia: effect of recombinant follicle stimulating hormone. Hum Reprod. 1998;13:2772-2781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 62] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 107. | Sousa M, Cremades N, Alves C, Silva J, Barros A. Developmental potential of human spermatogenic cells co-cultured with Sertoli cells. Hum Reprod. 2002;17:161-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 97] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 108. | Tanaka A, Nagayoshi M, Awata S, Mawatari Y, Tanaka I, Kusunoki H. Completion of meiosis in human primary spermatocytes through in vitro coculture with Vero cells. Fertil Steril. 2003;79 Suppl 1:795-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 62] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 109. | von Kopylow K, Schulze W, Salzbrunn A, Schaks M, Schäfer E, Roth B, Schlatt S, Spiess AN. Dynamics, ultrastructure and gene expression of human in vitro organized testis cells from testicular sperm extraction biopsies. Mol Hum Reprod. 2018;24:123-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 110. | Yang S, Ping P, Ma M, Li P, Tian R, Yang H, Liu Y, Gong Y, Zhang Z, Li Z, He Z. Generation of haploid spermatids with fertilization and development capacity from human spermatogonial stem cells of cryptorchid patients. Stem Cell Reports. 2014;3:663-675. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 72] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 111. | Sakib S, Voigt A, Goldsmith T, Dobrinski I. Three-dimensional testicular organoids as novel in vitro models of testicular biology and toxicology. Environ Epigenet. 2019;5:dvz011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 112. | Alves-Lopes JP, Stukenborg JB. Testicular organoids: a new model to study the testicular microenvironment in vitro? Hum Reprod Update. 2018;24:176-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 62] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 113. | Huleihel M, Nourashrafeddin S, Plant TM. Application of three-dimensional culture systems to study mammalian spermatogenesis, with an emphasis on the rhesus monkey (Macaca mulatta). Asian J Androl. 2015;17:972-980. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 77] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 114. | Abofoul-Azab M, AbuMadighem A, Lunenfeld E, Kapelushnik J, Shi Q, Pinkas H, Huleihel M. Development of Postmeiotic Cells In Vitro from Spermatogonial Cells of Prepubertal Cancer Patients. Stem Cells Dev. 2018;27:1007-1020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 115. | TROWELL OA. A modified technique for organ culture in vitro. Exp Cell Res. 1954;6:246-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 169] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 116. | Sato T, Katagiri K, Gohbara A, Inoue K, Ogonuki N, Ogura A, Kubota Y, Ogawa T. In vitro production of functional sperm in cultured neonatal mouse testes. Nature. 2011;471:504-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 493] [Cited by in RCA: 527] [Article Influence: 37.6] [Reference Citation Analysis (0)] |
| 117. | Lambrot R, Coffigny H, Pairault C, Donnadieu AC, Frydman R, Habert R, Rouiller-Fabre V. Use of organ culture to study the human fetal testis development: effect of retinoic acid. J Clin Endocrinol Metab. 2006;91:2696-2703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 78] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 118. | de Michele F, Poels J, Weerens L, Petit C, Evrard Z, Ambroise J, Gruson D, Wyns C. Preserved seminiferous tubule integrity with spermatogonial survival and induction of Sertoli and Leydig cell maturation after long-term organotypic culture of prepubertal human testicular tissue. Hum Reprod. 2017;32:32-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 119. | Roulet V, Denis H, Staub C, Le Tortorec A, Delaleu B, Satie AP, Patard JJ, Jégou B, Dejucq-Rainsford N. Human testis in organotypic culture: application for basic or clinical research. Hum Reprod. 2006;21:1564-1575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 65] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 120. | Jørgensen A, Young J, Nielsen JE, Joensen UN, Toft BG, Rajpert-De Meyts E, Loveland KL. Hanging drop cultures of human testis and testis cancer samples: a model used to investigate activin treatment effects in a preserved niche. Br J Cancer. 2014;110:2604-2614. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 67] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 121. | Potter SJ, DeFalco T. Using Ex Vivo Upright Droplet Cultures of Whole Fetal Organs to Study Developmental Processes during Mouse Organogenesis. J Vis Exp. 2015;(105):e53262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 122. | Pendergraft SS, Sadri-Ardekani H, Atala A, Bishop CE. Three-dimensional testicular organoid: a novel tool for the study of human spermatogenesis and gonadotoxicity in vitro. Biol Reprod. 2017;96:720-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 137] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 123. | Siemann DN, Strange DP, Maharaj PN, Shi PY, Verma S. Zika Virus Infects Human Sertoli Cells and Modulates the Integrity of the In Vitro Blood-Testis Barrier Model. J Virol. 2017;91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 103] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 124. | Strange DP, Zarandi NP, Trivedi G, Atala A, Bishop CE, Sadri-Ardekani H, Verma S. Human testicular organoid system as a novel tool to study Zika virus pathogenesis. Emerg Microbes Infect. 2018;7:82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 125. | Perrard MH, Sereni N, Schluth-Bolard C, Blondet A, D Estaing SG, Plotton I, Morel-Journel N, Lejeune H, David L, Durand P. Complete Human and Rat Ex Vivo Spermatogenesis from Fresh or Frozen Testicular Tissue. Biol Reprod. 2016;95:89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 83] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 126. | Komeya M, Kimura H, Nakamura H, Yokonishi T, Sato T, Kojima K, Hayashi K, Katagiri K, Yamanaka H, Sanjo H, Yao M, Kamimura S, Inoue K, Ogonuki N, Ogura A, Fujii T, Ogawa T. Long-term ex vivo maintenance of testis tissues producing fertile sperm in a microfluidic device. Sci Rep. 2016;6:21472. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 148] [Cited by in RCA: 130] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 127. | Zenzes MT, Engel W. The capacity of testicular cells of the postnatal rat to reorganize into histotypic structures. Differentiation. 1981;20:157-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 128. | Yokonishi T, Sato T, Katagiri K, Komeya M, Kubota Y, Ogawa T. In Vitro Reconstruction of Mouse Seminiferous Tubules Supporting Germ Cell Differentiation. Biol Reprod. 2013;89:15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 129. | Hadley MA, Byers SW, Suárez-Quian CA, Kleinman HK, Dym M. Extracellular matrix regulates Sertoli cell differentiation, testicular cord formation, and germ cell development in vitro. J Cell Biol. 1985;101:1511-1522. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 365] [Cited by in RCA: 367] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 130. | Lee DR, Kaproth MT, Parks JE. In vitro production of haploid germ cells from fresh or frozen-thawed testicular cells of neonatal bulls. Biol Reprod. 2001;65:873-878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 65] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 131. | Lee JH, Kim HJ, Kim H, Lee SJ, Gye MC. In vitro spermatogenesis by three-dimensional culture of rat testicular cells in collagen gel matrix. Biomaterials. 2006;27:2845-2853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 96] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 132. | Lee JH, Oh JH, Lee JH, Kim MR, Min CK. Evaluation of in vitro spermatogenesis using poly(D,L-lactic-co-glycolic acid) (PLGA)-based macroporous biodegradable scaffolds. J Tissue Eng Regen Med. 2011;5:130-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 133. | Stukenborg JB, Schlatt S, Simoni M, Yeung CH, Elhija MA, Luetjens CM, Huleihel M, Wistuba J. New horizons for in vitro spermatogenesis? Mol Hum Reprod. 2009;15:521-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 127] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 134. | Stukenborg JB, Wistuba J, Luetjens CM, Elhija MA, Huleihel M, Lunenfeld E, Gromoll J, Nieschlag E, Schlatt S. Coculture of spermatogonia with somatic cells in a novel three-dimensional soft-agar-culture-system. J Androl. 2008;29:312-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 105] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 135. | Alves-Lopes JP, Söder O, Stukenborg JB. Testicular organoid generation by a novel in vitro three-layer gradient system. Biomaterials. 2017;130:76-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 115] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 136. | Reuter K, Ehmcke J, Stukenborg JB, Simoni M, Damm OS, Redmann K, Schlatt S, Wistuba J. Reassembly of somatic cells and testicular organogenesis in vitro. Tissue Cell. 2014;46:86-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 137. | Baert Y, De Kock J, Alves-Lopes JP, Söder O, Stukenborg JB, Goossens E. Primary Human Testicular Cells Self-Organize into Organoids with Testicular Properties. Stem Cell Reports. 2017;8:30-38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 110] [Cited by in RCA: 110] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 138. | Kumar DL, DeFalco T. A perivascular niche for multipotent progenitors in the fetal testis. Nat Commun. 2018;9:4519. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 139. | Galipeau J, Sensébé L. Mesenchymal Stromal Cells: Clinical Challenges and Therapeutic Opportunities. Cell Stem Cell. 2018;22:824-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1009] [Cited by in RCA: 1208] [Article Influence: 172.6] [Reference Citation Analysis (0)] |
| 140. | Guadix JA, Zugaza JL, Gálvez-Martín P. Characteristics, applications and prospects of mesenchymal stem cells in cell therapy. Med Clin (Barc). 2017;148:408-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 141. | Samsonraj RM, Raghunath M, Nurcombe V, Hui JH, van Wijnen AJ, Cool SM. Concise Review: Multifaceted Characterization of Human Mesenchymal Stem Cells for Use in Regenerative Medicine. Stem Cells Transl Med. 2017;6:2173-2185. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 510] [Cited by in RCA: 518] [Article Influence: 64.8] [Reference Citation Analysis (0)] |
| 142. | Nayernia K, Lee JH, Drusenheimer N, Nolte J, Wulf G, Dressel R, Gromoll J, Engel W. Derivation of male germ cells from bone marrow stem cells. Lab Invest. 2006;86:654-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 222] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 143. | Kadam P, Van Saen D, Goossens E. Can mesenchymal stem cells improve spermatogonial stem cell transplantation efficiency? Andrology. 2017;5:2-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 144. | Kadam P, Ntemou E, Baert Y, Van Laere S, Van Saen D, Goossens E. Co-transplantation of mesenchymal stem cells improves spermatogonial stem cell transplantation efficiency in mice. Stem Cell Res Ther. 2018;9:317. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 145. | Anand S, Bhartiya D, Sriraman K, Mallick A. Underlying Mechanisms that Restore Spermatogenesis on Transplanting Healthy Niche Cells in Busulphan Treated Mouse Testis. Stem Cell Rev Rep. 2016;12:682-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 81] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 146. | Bar-Shira Maymon B, Yogev L, Marks A, Hauser R, Botchan A, Yavetz H. Sertoli cell inactivation by cytotoxic damage to the human testis after cancer chemotherapy. Fertil Steril. 2004;81:1391-1394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 27] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 147. | Shinohara T, Orwig KE, Avarbock MR, Brinster RL. Restoration of spermatogenesis in infertile mice by Sertoli cell transplantation. Biol Reprod. 2003;68:1064-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 102] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 148. | Howell SJ, Radford JA, Ryder WD, Shalet SM. Testicular function after cytotoxic chemotherapy: evidence of Leydig cell insufficiency. J Clin Oncol. 1999;17:1493-1498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 95] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 149. | Mushahary D, Spittler A, Kasper C, Weber V, Charwat V. Isolation, cultivation, and characterization of human mesenchymal stem cells. Cytometry A. 2018;93:19-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 397] [Article Influence: 49.6] [Reference Citation Analysis (0)] |
| 150. | Maumus M, Jorgensen C, Noël D. Mesenchymal stem cells in regenerative medicine applied to rheumatic diseases: role of secretome and exosomes. Biochimie. 2013;95:2229-2234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 191] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 151. | Liang X, Ding Y, Zhang Y, Tse HF, Lian Q. Paracrine mechanisms of mesenchymal stem cell-based therapy: current status and perspectives. Cell Transplant. 2014;23:1045-1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 513] [Cited by in RCA: 683] [Article Influence: 68.3] [Reference Citation Analysis (0)] |
| 152. | Hong SH, Maghen L, Kenigsberg S, Teichert AM, Rammeloo AW, Shlush E, Szaraz P, Pereira S, Lulat A, Xiao R, Yie SM, Gauthier-Fisher A, Librach CL. Ontogeny of human umbilical cord perivascular cells: molecular and fate potential changes during gestation. Stem Cells Dev. 2013;22:2425-2439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 153. | Szaraz P, Librach M, Maghen L, Iqbal F, Barretto TA, Kenigsberg S, Gauthier-Fisher A, Librach CL. In Vitro Differentiation of First Trimester Human Umbilical Cord Perivascular Cells into Contracting Cardiomyocyte-Like Cells. Stem Cells Int. 2016;2016:7513252. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 154. | Baksh D, Yao R, Tuan RS. Comparison of proliferative and multilineage differentiation potential of human mesenchymal stem cells derived from umbilical cord and bone marrow. Stem Cells. 2007;25:1384-1392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 719] [Cited by in RCA: 740] [Article Influence: 41.1] [Reference Citation Analysis (0)] |
| 155. | de Witte SFH, Luk F, Sierra Parraga JM, Gargesha M, Merino A, Korevaar SS, Shankar AS, O'Flynn L, Elliman SJ, Roy D, Betjes MGH, Newsome PN, Baan CC, Hoogduijn MJ. Immunomodulation By Therapeutic Mesenchymal Stromal Cells (MSC) Is Triggered Through Phagocytosis of MSC By Monocytic Cells. Stem Cells. 2018;36:602-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 266] [Cited by in RCA: 373] [Article Influence: 53.3] [Reference Citation Analysis (0)] |
| 156. | Maghen L, Shlush E, Gat I, Filice M, Barretto T, Jarvi K, Lo K, Gauthier-Fisher AS, Librach CL. Human umbilical perivascular cells: a novel source of MSCs to support testicular niche regeneration. Reproduction. 2016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 157. | Shlush E, Maghen L, Swanson S, Kenigsberg S, Moskovtsev S, Barretto T, Gauthier-Fisher A, Librach CL. In vitro generation of Sertoli-like and haploid spermatid-like cells from human umbilical cord perivascular cells. Stem Cell Res Ther. 2017;8:37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 158. | Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126:663-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17989] [Cited by in RCA: 18204] [Article Influence: 958.1] [Reference Citation Analysis (0)] |
| 159. | Aoi T. 10th anniversary of iPS cells: the challenges that lie ahead. J Biochem. 2016;160:121-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 160. | Ilic D, Devito L, Miere C, Codognotto S. Human embryonic and induced pluripotent stem cells in clinical trials. Br Med Bull. 2015;116:19-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 161. | Clark AT, Bodnar MS, Fox M, Rodriquez RT, Abeyta MJ, Firpo MT, Pera RA. Spontaneous differentiation of germ cells from human embryonic stem cells in vitro. Hum Mol Genet. 2004;13:727-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 369] [Cited by in RCA: 356] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 162. | Nayernia K, Nolte J, Michelmann HW, Lee JH, Rathsack K, Drusenheimer N, Dev A, Wulf G, Ehrmann IE, Elliott DJ, Okpanyi V, Zechner U, Haaf T, Meinhardt A, Engel W. In vitro-differentiated embryonic stem cells give rise to male gametes that can generate offspring mice. Dev Cell. 2006;11:125-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 390] [Cited by in RCA: 343] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 163. | Zhou Q, Wang M, Yuan Y, Wang X, Fu R, Wan H, Xie M, Liu M, Guo X, Zheng Y, Feng G, Shi Q, Zhao XY, Sha J, Zhou Q. Complete Meiosis from Embryonic Stem Cell-Derived Germ Cells In Vitro. Cell Stem Cell. 2016;18:330-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 313] [Cited by in RCA: 268] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 164. | Hu J, Wang J. From embryonic stem cells to induced pluripotent stem cells-Ready for clinical therapy? Clin Transplant. 2019;33:e13573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 165. | Kurkure P, Prasad M, Dhamankar V, Bakshi G. Very small embryonic-like stem cells (VSELs) detected in azoospermic testicular biopsies of adult survivors of childhood cancer. Reprod Biol Endocrinol. 2015;13:122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 166. | Bhartiya D, Kasiviswanathan S, Unni SK, Pethe P, Dhabalia JV, Patwardhan S, Tongaonkar HB. Newer insights into premeiotic development of germ cells in adult human testis using Oct-4 as a stem cell marker. J Histochem Cytochem. 2010;58:1093-1106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 87] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 167. | Yang Y, Li Z, Wu X, Chen H, Xu W, Xiang Q, Zhang Q, Chen J, Ge RS, Su Z, Huang Y. Direct Reprogramming of Mouse Fibroblasts toward Leydig-like Cells by Defined Factors. Stem Cell Reports. 2017;8:39-53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 168. | Chen X, Li C, Chen Y, Xi H, Zhao S, Ma L, Xu Z, Han Z, Zhao J, Ge R, Guo X. Differentiation of human induced pluripotent stem cells into Leydig-like cells with molecular compounds. Cell Death Dis. 2019;10:220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 169. | Buganim Y, Itskovich E, Hu YC, Cheng AW, Ganz K, Sarkar S, Fu D, Welstead GG, Page DC, Jaenisch R. Direct reprogramming of fibroblasts into embryonic Sertoli-like cells by defined factors. Cell Stem Cell. 2012;11:373-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 128] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 170. | Mishra S, Kacin E, Stamatiadis P, Franck S, Van der Jeught M, Mertes H, Pennings G, De Sutter P, Sermon K, Heindryckx B, Geens M. The role of the reprogramming method and pluripotency state in gamete differentiation from patient-specific human pluripotent stem cells. Mol Hum Reprod. 2018;24:173-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 171. | Nagamatsu G, Hayashi K. Stem cells, in vitro gametogenesis and male fertility. Reproduction. 2017;154:F79-F91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 172. | Eguizabal C, Montserrat N, Vassena R, Barragan M, Garreta E, Garcia-Quevedo L, Vidal F, Giorgetti A, Veiga A, Izpisua Belmonte JC. Complete meiosis from human induced pluripotent stem cells. Stem Cells. 2011;29:1186-1195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 152] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 173. | Panula S, Medrano JV, Kee K, Bergström R, Nguyen HN, Byers B, Wilson KD, Wu JC, Simon C, Hovatta O, Reijo Pera RA. Human germ cell differentiation from fetal- and adult-derived induced pluripotent stem cells. Hum Mol Genet. 2011;20:752-762. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 185] [Cited by in RCA: 180] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 174. | Easley CA 4th, Phillips BT, McGuire MM, Barringer JM, Valli H, Hermann BP, Simerly CR, Rajkovic A, Miki T, Orwig KE, Schatten GP. Direct differentiation of human pluripotent stem cells into haploid spermatogenic cells. Cell Rep. 2012;2:440-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 184] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 175. | Medrano JV, Ramathal C, Nguyen HN, Simon C, Reijo Pera RA. Divergent RNA-binding proteins, DAZL and VASA, induce meiotic progression in human germ cells derived in vitro. Stem Cells. 2012;30:441-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 127] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 176. | Turinetto V, Orlando L, Giachino C. Induced Pluripotent Stem Cells: Advances in the Quest for Genetic Stability during Reprogramming Process. Int J Mol Sci. 2017;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 177. | Théry C, Ostrowski M, Segura E. Membrane vesicles as conveyors of immune responses. Nat Rev Immunol. 2009;9:581-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2703] [Cited by in RCA: 3109] [Article Influence: 194.3] [Reference Citation Analysis (0)] |
| 178. | Taylor DD, Shah S. Methods of isolating extracellular vesicles impact down-stream analyses of their cargoes. Methods. 2015;87:3-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 350] [Cited by in RCA: 476] [Article Influence: 47.6] [Reference Citation Analysis (0)] |
| 179. | Ibrahim A, Marbán E. Exosomes: Fundamental Biology and Roles in Cardiovascular Physiology. Annu Rev Physiol. 2016;78:67-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 234] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 180. | Cunnane EM, Weinbaum JS, O'Brien FJ, Vorp DA. Future Perspectives on the Role of Stem Cells and Extracellular Vesicles in Vascular Tissue Regeneration. Front Cardiovasc Med. 2018;5:86. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 181. | Mulvihill JJ, Cunnane EM, Ross AM, Duskey JT, Tosi G, Grabrucker AM. Drug delivery across the blood-brain barrier: recent advances in the use of nanocarriers. Nanomedicine (Lond). 2020;15:205-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 105] [Article Influence: 21.0] [Reference Citation Analysis (1)] |
| 182. | Poliakov A, Spilman M, Dokland T, Amling CL, Mobley JA. Structural heterogeneity and protein composition of exosome-like vesicles (prostasomes) in human semen. Prostate. 2009;69:159-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 254] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 183. | Murdica V, Giacomini E, Alteri A, Bartolacci A, Cermisoni GC, Zarovni N, Papaleo E, Montorsi F, Salonia A, Viganò P, Vago R. Seminal plasma of men with severe asthenozoospermia contain exosomes that affect spermatozoa motility and capacitation. Fertil Steril 2019; 111: 897-908. e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 84] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 184. | Guo H, Chang Z, Zhang Z, Zhao Y, Jiang X, Yu H, Zhang Y, Zhao R, He B. Extracellular ATPs produced in seminal plasma exosomes regulate boar sperm motility and mitochondrial metabolism. Theriogenology. 2019;139:113-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 185. | Sullivan R, Mieusset R. The human epididymis: its function in sperm maturation. Hum Reprod Update. 2016;22:574-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 220] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 186. | Sullivan R. Epididymosomes: Role of extracellular microvesicles in sperm maturation. Front Biosci (Schol Ed). 2016;8:106-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 56] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 187. | Saez F, Frenette G, Sullivan R. Epididymosomes and prostasomes: their roles in posttesticular maturation of the sperm cells. J Androl. 2003;24:149-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 142] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 188. | Sullivan R, Frenette G, Girouard J. Epididymosomes are involved in the acquisition of new sperm proteins during epididymal transit. Asian J Androl. 2007;9:483-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 206] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 189. | Sullivan R, Saez F. Epididymosomes, prostasomes, and liposomes: their roles in mammalian male reproductive physiology. Reproduction. 2013;146:R21-R35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 229] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 190. | Mathivanan S, Ji H, Simpson RJ. Exosomes: extracellular organelles important in intercellular communication. J Proteomics. 2010;73:1907-1920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1718] [Cited by in RCA: 1946] [Article Influence: 129.7] [Reference Citation Analysis (0)] |
| 191. | Vojtech L, Woo S, Hughes S, Levy C, Ballweber L, Sauteraud RP, Strobl J, Westerberg K, Gottardo R, Tewari M, Hladik F. Exosomes in human semen carry a distinctive repertoire of small non-coding RNAs with potential regulatory functions. Nucleic Acids Res. 2014;42:7290-7304. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 446] [Cited by in RCA: 446] [Article Influence: 40.5] [Reference Citation Analysis (0)] |
| 192. | Nawaz M, Camussi G, Valadi H, Nazarenko I, Ekström K, Wang X, Principe S, Shah N, Ashraf NM, Fatima F, Neder L, Kislinger T. The emerging role of extracellular vesicles as biomarkers for urogenital cancers. Nat Rev Urol. 2014;11:688-701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 236] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 193. | Welton JL, Khanna S, Giles PJ, Brennan P, Brewis IA, Staffurth J, Mason MD, Clayton A. Proteomics analysis of bladder cancer exosomes. Mol Cell Proteomics. 2010;9:1324-1338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 323] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 194. | Raimondo F, Morosi L, Corbetta S, Chinello C, Brambilla P, Della Mina P, Villa A, Albo G, Battaglia C, Bosari S, Magni F, Pitto M. Differential protein profiling of renal cell carcinoma urinary exosomes. Mol Biosyst. 2013;9:1220-1233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 131] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 195. | Barceló M, Castells M, Bassas L, Vigués F, Larriba S. Semen miRNAs Contained in Exosomes as Non-Invasive Biomarkers for Prostate Cancer Diagnosis. Sci Rep. 2019;9:13772. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 107] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 196. | Jodar M, Sendler E, Moskovtsev SI, Librach CL, Goodrich R, Swanson S, Hauser R, Diamond MP, Krawetz SA. Absence of sperm RNA elements correlates with idiopathic male infertility. Sci Transl Med. 2015;7:295re6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 110] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 197. | Burl RB, Clough S, Sendler E, Estill M, Krawetz SA. Sperm RNA elements as markers of health. Syst Biol Reprod Med. 2018;64:25-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 198. | Barkalina N, Jones C, Wood MJ, Coward K. Extracellular vesicle-mediated delivery of molecular compounds into gametes and embryos: learning from nature. Hum Reprod Update. 2015;21:627-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 199. | Foster BP, Balassa T, Benen TD, Dominovic M, Elmadjian GK, Florova V, Fransolet MD, Kestlerova A, Kmiecik G, Kostadinova IA, Kyvelidou C, Meggyes M, Mincheva MN, Moro L, Pastuschek J, Spoldi V, Wandernoth P, Weber M, Toth B, Markert UR. Extracellular vesicles in blood, milk and body fluids of the female and male urogenital tract and with special regard to reproduction. Crit Rev Clin Lab Sci. 2016;53:379-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 70] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 200. | Ma Z, Wang Y, Li H. Applications of extracellular vesicles in tissue regeneration. Biomicrofluidics. 2020;14:011501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 201. | Lai RC, Yeo RW, Tan KH, Lim SK. Exosomes for drug delivery - a novel application for the mesenchymal stem cell. Biotechnol Adv. 2013;31:543-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 321] [Cited by in RCA: 403] [Article Influence: 31.0] [Reference Citation Analysis (0)] |
| 202. | Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284:143-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15372] [Cited by in RCA: 15203] [Article Influence: 584.7] [Reference Citation Analysis (0)] |
| 203. | Borgovan T, Crawford L, Nwizu C, Quesenberry P. Stem cells and extracellular vesicles: biological regulators of physiology and disease. Am J Physiol Cell Physiol. 2019;317:C155-C166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 204. | Bruno S, Grange C, Deregibus MC, Calogero RA, Saviozzi S, Collino F, Morando L, Busca A, Falda M, Bussolati B, Tetta C, Camussi G. Mesenchymal stem cell-derived microvesicles protect against acute tubular injury. J Am Soc Nephrol. 2009;20:1053-1067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 931] [Cited by in RCA: 1027] [Article Influence: 64.2] [Reference Citation Analysis (0)] |
| 205. | Tao H, Chen X, Cao H, Zheng L, Li Q, Zhang K, Han Z, Han ZC, Guo Z, Li Z, Wang L. Mesenchymal Stem Cell-Derived Extracellular Vesicles for Corneal Wound Repair. Stem Cells Int. 2019;2019:5738510. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 206. | Harrell CR, Jovicic N, Djonov V, Arsenijevic N, Volarevic V. Mesenchymal Stem Cell-Derived Exosomes and Other Extracellular Vesicles as New Remedies in the Therapy of Inflammatory Diseases. Cells. 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 225] [Cited by in RCA: 535] [Article Influence: 89.2] [Reference Citation Analysis (0)] |
| 207. | Trubiani O, Marconi GD, Pierdomenico SD, Piattelli A, Diomede F, Pizzicannella J. Human Oral Stem Cells, Biomaterials and Extracellular Vesicles: A Promising Tool in Bone Tissue Repair. Int J Mol Sci. 2019;20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 86] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 208. | Figliolini F, Ranghino A, Grange C, Cedrino M, Tapparo M, Cavallari C, Rossi A, Togliatto G, Femminò S, Gugliuzza MV, Camussi G, Brizzi MF. Extracellular Vesicles From Adipose Stem Cells Prevent Muscle Damage and Inflammation in a Mouse Model of Hind Limb Ischemia: Role of Neuregulin-1. Arterioscler Thromb Vasc Biol. 2020;40:239-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 60] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 209. | Yang Q, Chen X, Zheng T, Han D, Zhang H, Shi Y, Bian J, Sun X, Xia K, Liang X, Liu G, Zhang Y, Deng C. Transplantation of Human Urine-Derived Stem Cells Transfected with Pigment Epithelium-Derived Factor to Protect Erectile Function in a Rat Model of Cavernous Nerve Injury. Cell Transplant. 2016;25:1987-2001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 210. | Deng C, Xie Y, Zhang C, Ouyang B, Chen H, Lv L, Yao J, Liang X, Zhang Y, Sun X, Deng C, Liu G. Urine-Derived Stem Cells Facilitate Endogenous Spermatogenesis Restoration of Busulfan-Induced Nonobstructive Azoospermic Mice by Paracrine Exosomes. Stem Cells Dev. 2019;28:1322-1333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 211. | Park SE, Georgescu A, Huh D. Organoids-on-a-chip. Science. 2019;364:960-965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 484] [Cited by in RCA: 521] [Article Influence: 86.8] [Reference Citation Analysis (0)] |
| 212. | Skardal A, Shupe T, Atala A. Organoid-on-a-chip and body-on-a-chip systems for drug screening and disease modeling. Drug Discov Today. 2016;21:1399-1411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 302] [Cited by in RCA: 321] [Article Influence: 35.7] [Reference Citation Analysis (0)] |
| 213. | Karzbrun E, Kshirsagar A, Cohen SR, Hanna JH, Reiner O. Human Brain Organoids on a Chip Reveal the Physics of Folding. Nat Phys. 2018;14:515-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 281] [Article Influence: 40.1] [Reference Citation Analysis (0)] |
| 214. | Ghaemmaghami AM, Hancock MJ, Harrington H, Kaji H, Khademhosseini A. Biomimetic tissues on a chip for drug discovery. Drug Discov Today. 2012;17:173-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 261] [Article Influence: 18.6] [Reference Citation Analysis (0)] |