Published online Mar 26, 2019. doi: 10.4252/wjsc.v11.i3.167
Peer-review started: January 14, 2019
First decision: January 26, 2019
Revised: February 7, 2019
Accepted: February 27, 2019
Article in press: February 28, 2019
Published online: March 26, 2019
Processing time: 73 Days and 3.1 Hours
Mesenchymal stem cells (MSCs) are a subset of multipotent stroma cells residing in various tissues of the body. Apart from supporting the hematopoietic stem cell niche, MSCs possess strong immunoregulatory ability and multiple differentiation potentials. These powerful capacities allow the extensive application of MSCs in clinical practice as an effective treatment for diseases. Therefore, illuminating the functional mechanism of MSCs will help to improve their curative effect and promote their clinical use. Long noncoding RNA (LncRNA) is a novel class of noncoding RNA longer than 200 nt. Recently, multiple studies have demonstrated that LncRNA is widely involved in growth and development through controlling the fate of cells, including MSCs. In this review, we highlight the role of LncRNA in regulating the functions of MSCs and discuss their participation in the pathogenesis of diseases and clinical use in diagnosis and treatment.
Core tip: Mesenchymal stem cells (MSCs) are an important kind of multipotent stroma cells in vivo. The various and powerful functions of MSCs are under the control of long non-coding RNA (LncRNA). Previously, many studies have been conducted to illustrate the role of LncRNA in the functions of MSCs. In this review, we highlight LncRNA as a great functional regulator of MSCs and discuss their participation in the pathogenesis of diseases and clinical use in diagnosis and treatment.
- Citation: Xie ZY, Wang P, Wu YF, Shen HY. Long non-coding RNA: The functional regulator of mesenchymal stem cells. World J Stem Cells 2019; 11(3): 167-179
- URL: https://www.wjgnet.com/1948-0210/full/v11/i3/167.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v11.i3.167
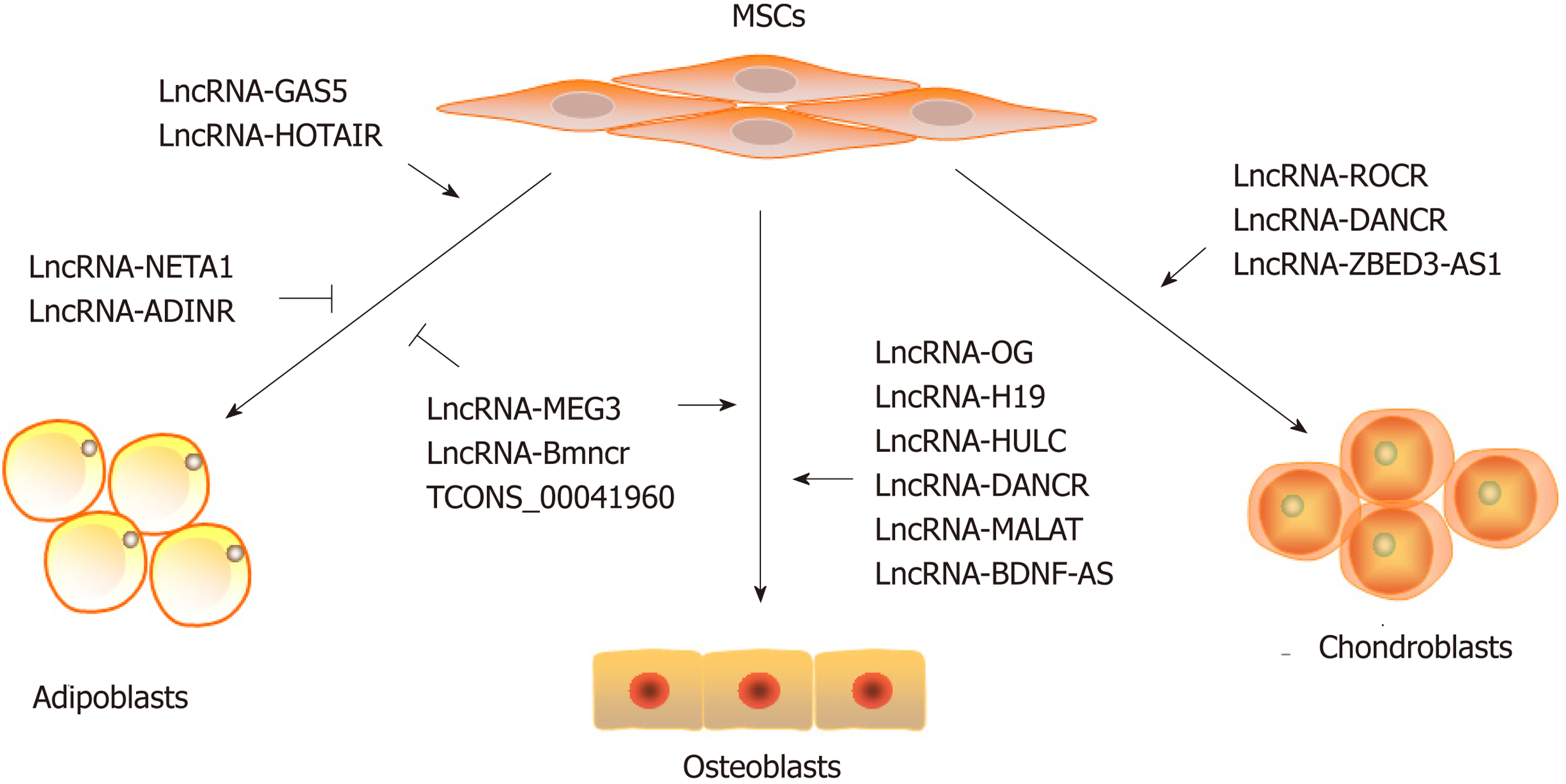
First identified by Friedenstein et al[1] in 1974, mesenchymal stem cells (MSCs) were found to support the hematopoietic stem cell niche in the bone marrow microenvironment. With the advancement of research through these years, it has been established that MSCs are multipotent progenitor cells located in various tissues in vivo. Moreover, MSCs possess two critical capacities, immunoregulation and multilineage differentiation[2]. On the one hand, MSCs modulate the functions of different kinds of immunocytes, such as T cells, B cells and dendritic cells, which greatly contribute to the homeostasis of the immune system[3,4]. On the other hand, under different circumstances, MSCs could differentiate into osteoblasts, chondroblasts or adipoblasts, which play an important role in body development and tissue repair[5,6]. Benefiting from self-renewal and low immunogenicity characteristics, MSCs with these powerful capacities have been widely used in clinical practice[7-9].
MSCs exhibit diverse capacities under various circumstances (i.e., inflammation, stress or other factors)[10-12]. These external stimuli induce changes in transcriptional regulation in the cells, which modulate the activation of signaling pathways and finally determine the immunoregulatory ability and differentiation direction of MSCs. On the other hand, abnormal transcriptional regulation causes MSC dysfunction, which is also involved in disease progression. Therefore, illuminating the mechanism of the transcriptional regulation of MSCs could not only elucidate the pathogenesis of diseases but also improve their curative effects. Recently, many studies on the mechanism of transcriptional regulation in MSCs have been conducted, and the importance of long noncoding RNA (LncRNA) is coming into focus.
General cell function is under the precise control of various epigenetic mechanisms, including DNA methylation, histone methylation and noncoding RNA[13,14]. Noncoding RNA, although spanning more than 98% of DNA transcripts, is not translated into proteins. Rather, these molecules spatiotemporally regulate protein-coding gene expression. Noncoding RNA is defined into two classes, those less than 200 nt, including microRNA, small nuclear RNA and small interfering RNA, and those larger than 200 nt, called lncRNA[14].
LncRNA used to be considered as dark matter. Recently, more evidence has indicated a role for LncRNA as a new player in the functional regulation of various eukaryotes[15]. According to its different characteristics, LncRNA is divided into several categories, including sense, antisense, intronic, intergenic and bidirectional LncRNA. These LncRNAs are mainly located in the cell nucleus or cytoplasm, affecting the status and fate of cells through different transcriptional and posttranscriptional mechanisms[16]. Nuclear LncRNA guides chromatin modifiers, such as DNA methyltransferase, histone methyltransferase and heteronuclear ribosome protein, to a specific genetic locus and induces chromatin structure remodeling, which in turn regulates gene expression either positively or negatively[17]. In addition, some nuclear LncRNAs bind to specific genetic loci by complementary sequences and affect their expression. Moreover, the location and transcriptional status of other nuclear LncRNAs will directly affect their nearby or partial overlapping gene expression mainly through bringing transcriptional enhancers closer to the promoters of a specific gene. Based on the difference in action range, these nuclear LncRNAs are distinguished into cis-acting LncRNAs, which affect the gene expression in the vicinity of the same chromosome, and trans-acting LncRNAs, which function over great distances as “intercontinental missiles”[17]. For cytoplasmic LncRNA, the regulation mechanisms are fundamentally different[18]. The most common and widely studied mechanism of cytoplasmic LncRNA is to act as a competitive endogenous RNA (ceRNA). MicroRNA, another type of noncoding RNA, negatively controls the translation of mRNA into protein. LncRNA can act as a microRNA sponge through binding to specific complementary sequences and competitively protect the target mRNA being repressed by microRNA[19]. In addition, cytoplasmic LncRNA can act as a decoy for cytoplasmic mRNA by base pairing and then degrading or conversely stabilizing these specific mRNAs. This mode of action may also function at the mRNA translation level when cytoplasmic LncRNA binds to translationally controlled proteins and indirectly modulates target mRNA translation[18]. Recently, a novel mechanism of cytoplasmic LncRNA was identified. These cytoplasmic LncRNAs can either block the functional site or alter the structure and modification of specific proteins, thereby regulating the function and stabilization of these proteins. This process leads to the up- or downregulation of signaling pathways and ultimately alters the fate and function of cells[20]. These protean and powerful functions allow the wide involvement of LncRNA in all aspects of cell processes.
A number of studies have indicated that LncRNA modulates various functions of multiple cells. In stem cells, LncRNA contributes not only to stemness maintenance but also to multilineage differentiation and other aspects[21-24]. In recent years, the role of LncRNA in MSCs has been widely studied, and several critical LncRNAs have been identified with regard to differentiation, immunoregulation, proliferation and apoptosis. In this review, we provide a systematic overview of these studies to provide new insights on the functional role of LncRNA in MSC regulation.
MSCs are the major origins of osteoblasts in vivo[25]. Under specific conditions or in specific microenvironments, MSCs perform osteogenic differentiation, and this process is under the precise control of a series of transcriptional and posttranscriptional mechanisms. To date, investigation into the expression and regulatory function of LncRNA during MSC osteogenic differentiation has provided the most insight into the role of LncRNA in MSCs. Song et al[26] was the first to detect the LncRNA expression profile of immortalized MSCs on day 28 of osteogenic differentiation with RNA sequencing. Hundreds of differentially expressed mRNAs and LncRNAs and several signaling pathways have been identified. However, the genome of immortalized MSCs has been artificially reconstructed by gene editing technology to infinite multiplication. Therefore, compared to normal MSCs, immortalized MSCs may have partially different transcriptomes. Several studies on bone marrow MSCs undergoing osteogenic differentiation were then conducted to study the LncRNA expression profile using a microarray[27,28]. The results using MSCs directly isolated from human bone marrow may reflect the real LncRNA expression profile during osteogenic differentiation. However, studies with microarrays mainly detect identified LncRNAs, while RNA sequencing assays could detect larger changes to identify unknown LncRNAs. Considering that a large number of LncRNAs have not yet been identified, RNA sequencing technology has a better prospect of application in further studies of LncRNA.
Osteogenesis is a dynamic process that results in inconsistent changes in LncRNA expression profiles at any time point. Therefore, the continuous monitoring of LncRNA profiles during the osteogenic differentiation of MSCs is commanded. Recently, Qiu et al[29] reported the global LncRNA expression on days 7, 14 and 21 of osteogenic differentiation and identified 665 LncRNAs that were continuously differentially expressed. This result provides a more comprehensive view of LncRNA expression patterns and is helpful in identifying critical LncRNAs. Notably, either the number or the category of the differentially expressed LncRNAs in these described studies is different. This discrepancy could result from the different experimental conditions in these studies. It is necessary to determine the mutual differentially expressed genes in these results, which could represent critical LncRNAs in the osteogenesis of MSCs.
Although the expression profile provides a comprehensive view, identifying the functional LncRNAs that function during the osteogenesis of MSCs is of great importance. H19, a paternally imprinted noncoding DNA, positively regulates the osteogenic differentiation of MSCs via microRNA-657. This complex inhibits TGF-β1 and the phosphorylation of Smad3, therefore promoting MSC osteogenesis[30]. This mechanism as a ceRNA to microRNA is common in MSCs during osteogenic differentiation. Jiang et al[31] demonstrated that LncRNA-HULC, acting as a ceRNA to microRNA-195, promoted the osteogenic differentiation of MSCs. Moreover, another well-known LncRNA, MALAT1, also up-regulates the critical osteogenic transcription factor Osterix by targeting microRNA-143, which eventually promotes MSC osteogenesis[32]. Other regulatory mechanisms also function during the osteogenic differentiation of MSCs, such as DANCR and BDNF-AS[33,34]. However, several questions still exist. First, most studies focus on the regulatory mechanisms and downstream targets of these LncRNAs. The upstream regulator that induces expression changes in these LncRNAs during the osteogenic differentiation of MSCs is still unknown. Moreover, a myriad of LncRNAs are related to the osteogenesis of MSCs to a certain degree; nevertheless, vital LncRNAs need to be identified. Last, whether and how these LncRNAs function in bone metabolism in vivo are also unclear. Recently, we determined that LncRNA-OG interacted with hnRNPK and accelerated MSC osteogenesis in vitro and vivo by modulating the BMP signaling pathway. Surprisingly, hnRNPK promoted the transcription of LncRNA-OG by affecting its H3K27 acetylation, therefore forming a positive feedback loop[35]. This result indicates that specific proteins, such as hnRNPK, could be both upstream regulators and downstream targets of LncRNA, suggesting a novel mechanism of LncRNA.
The osteogenic differentiation of MSCs is affected by many factors[36]. It is very likely that these factors influence MSCs by regulating their LncRNA expression. Osteogenic growth peptide, a short and linear tetradecapeptide in serum, enhances the osteogenic differentiation of MSCs through lncRNA-AK141205[37]. In addition, MSCs undergoing osteogenic differentiation in an inflammatory microenvironment caused by Staphylococcal protein A have the specific expression profile of LncRNAs, among which LncRNA-NONHSAT009968 may play a leading role[38]. In addition, high glucose conditions inhibit LncRNA-AK028326 expression and therefore prevent MSC osteogenic differentiation[39]. Therefore, the conclusion could be made that not only the nutrient content but also the osteo-inductive and inflammatory factor in the culture microenvironment could affect LncRNA expression, leading to a subsequent change in MSC osteogenesis. However, even when different stimulations result in the same tendency of differentiation, these factors still exhibit functions through various LncRNAs and different mechanisms.
Apart from the culture medium, culture materials influence the osteogenic differentiation of MSCs. A large number of biomaterials, including nanomaterials, piezoelectric materials and hydrogels, could enhance the osteogenic differentiation ability of MSCs, some of which have been widely used in the clinic[40,41]. Recently, Lv et al[42] found that TiO2 nanotube materials could alter the epigenetic profile, including the LncRNA expression of MSCs during osteogenic differentiation. Moreover, nanofibers modulated the LncRNA network to accelerate MSCs osteogenesis[43]. These studies confirm that the differentially expressed LncRNA in the culture materials mediate the osteogenic differentiation of MSCs. Clarifying the concrete mechanisms of these LncRNAs can allow us to precisely control the osteogenic ability of MSCs and help to improve their curative effect in bone reconstruction.
Adipose tissue comprises a substantial amount of biologically active tissues, and nonobese men and women have approximately 12 kg and 14 kg of adipose tissue, respectively[44]. Previously, some studies have demonstrated that LncRNA contributes to the process of adipogenesis[45,46]. The objects of these studies were adipocytes, indicating that these LncRNAs may function in the later phase of adipogenic differentiation. Adipocytes are the basic components of adipose tissue, and MSCs are a main source of adipocytes in many tissues. It could be more important to focus on the LncRNAs that initiate the adipogenic differentiation process. Recently, we found that lncRNA-GAS5 expression decreased gradually during the adipogenesis of MSCs. GAS5 negatively regulated adipogenic differentiation through the microRNA-18a-CTGF axis as a ceRNA, forming a negative feedback loop to prevent excessive adipogenesis[47]. In addition, Kalwa et al[48] reported that LncRNA-HOTAIR formed a triple helix structure to impact the adipogenic differentiation of MSCs through DNA methylation. These studies revealed the precise mechanism of adipogenesis, even though their roles in vivo need to be further discussed.
In regard to research on MSC differentiation, an unavoidable question is the balance between osteogenesis and adipogenesis. Although MSCs can undergo both osteogenic and adipogenic differentiation, one differentiation direction inhibits the other[49,50]. Similarly, osteo-inductive factors always accelerate MSC osteogenic differentiation but inhibit adipogenic differentiation and vice versa as lipogenic factors[51]. Determining the balance point and regulatory mechanisms of this process is the focus academic research in recent years. Recent studies suggest that LncRNAs can control this process. To promote osteogenesis, LncRNA-H19 was proven to inhibit adipocyte differentiation through a histone deacetylase mechanism in MSCs[30,52]. These results suggested that H19 could be one of the critical points in this differentiation balance. In addition to LncRNA-H19, a newly identified LncRNA named TCONS_00041960 could also enhance osteogenic differentiation but inhibit adipogenic differentiation. This LncRNA interacted with two competitive microRNAs, thereby modulating the balance between osteogenesis and adipogenesis of MSCs isolated from rats[53]. It could be assumed that the regulatory mechanism mediated by LncRNA is common and relatively conserved in many different species. Nevertheless, a challenge to these results is that all these studies are only performed in vitro. Recently, Li et al[54] identified LncRNA-BMNCR in MSCs and then constructed overexpressed and depleted transgenic mice. The results showed that the BMNCR-depleted mice had decreased bone mass but increased bone marrow adiposity, and overexpressed transgenic mice had completely opposite features[54]. To our knowledge, this study is the first concerning lncRNA in controlling the osteogenic and adipogenic differentiation direction in vivo. Nevertheless, it is worth noting that the complete knock-in or out of a gene in mice could possibly affect the functions of other cells, except the target cells, so conclusions regarding this phenotypic feature of MSCs alone should not be made at this time. Conditional knock-in/out transgenic mice targeting MSCs may help to illustrate the function of lncRNA in MSCs in vivo in the future.
As MSCs can be isolated from many different tissues in vivo, such as bone marrow, adipose tissue and Wharton’s jelly, the differentiation capacities of MSCs from various tissues are explicitly different[55]. Briefly, bone marrow-derived MSCs have stronger potential in osteogenic differentiation, but adipose-derived MSCs tend to undergo adipogenic differentiation. The reason and mechanism of this tissue specificity remain unknown. Interestingly, a recent study showed that bone marrow-derived MSCs preferred osteogenic differentiation, and LncRNA-MEG3 inhibited their osteogenic differentiation[56]. However, another study showed that LncRNA-MEG3 inhibited adipogenesis but promoted the osteogenesis of adipose-derived MSCs[57]. In addition, the expression profile of LncRNA-MEG3 in these two kinds of MSCs was distinctly different during differentiation. Therefore, we suggest that on the one hand, the difference in the differentiation potential of MSCs from various sources may result from the expression and function of LncRNA, and on the other hand, the same LncRNA could exhibit different functions in MSCs from various origins.
Apart from osteogenic and adipogenic differentiation, studies on LncRNA functions in the chondrogenic differentiation of MSCs have been widely carried out. The process of MSCs differentiating into chondrocytes contains two steps, chondrogenic and hypertrophic phases[58]. On day 14 of induction, as the chondrogenic phase, Wang et al[59] detected the expression profiles of LncRNA in MSCs and identified a total of 3638 differentially expressed LncRNA. Furthermore, Cao et al[60] determined the LncRNA expression profiles at the hypertrophic phase and found three critical LncRNAs that exerted functions from the chondrogenic phase to the hypertrophic phase. SOX9 is one of the most important transcription factors in chondrogenesis. Focused on SOX9 expression, Barter et al[61] identified that LncRNA-LOC102723505, termed ROCR, participated in the differentiation of MSCs into chondrocytes. However, the underlying mechanism of ROCR in modulating SOX9 expression is still unclear.
MSCs from joint tissues, including synovium and synovial fluid, are considered to have a stronger capacity for chondrogenic differentiation. This kind of MSC in the joint can directly take part in cartilage repair regeneration. A recent study reported that divergent LncRNA-ZBED3-AS1 promoted the chondrogenic differentiation of synovial fluid-derived MSCs by activating the Wnt/β-catenin signaling pathway[62]. Another LncRNA-DANCR, which is also the positive regulator of MSC osteogenesis, accelerated the chondrogenesis of MSCs isolated from synovium through a microRNA-1305/Smad4 axis as a ceRNA[34,63]. Notably, these LncRNAs and their mechanism can help to improve the therapeutic effect of MSCs in osteoarthritis.
As the major origins of mesodermal lineage, MSCs possess multipotent differentiation ability. Other than their well-known osteogenic, adipogenic and chondrogenic differentiation, MSCs could also differentiate into endotheliocytes and myocytes in the mesoderm under conditional induction[2]. Compared to the research performed in the field of osteogenesis, adipogenesis and chondrogenesis described above, studies on the concrete roles of LncRNAs in the endothelial and myogenic differentiation of MSCs are relatively rare.
Endothelial cells, forming a monolayer endothelium, are an important part of the vessels in vivo that separates the circulating blood from the tissues[64]. The regular quantity and function of endothelial cells guarantee angiogenesis; otherwise, their dysfunction results in the development of many pathological disorders. Therefore, it is of great importance to investigate, in depth, the mechanism of MSC differentiation into endotheliocytes. LncRNA-MIAT, which was considered to contribute greatly to development and disease, facilitated the endothelial differentiation of MSCs by targeting microRNA200a and vascular endothelial growth factor (VEGF)[65,66]. Moreover, MEG3, a well-studied LncRNA in MSCs as described above, was also found to participate in the endothelial differentiation of MSCs. This LncRNA facilitated the ubiquitination and subsequent degradation of FOXM1, which therefore reduced angiogenic VEGF expression and finally promoted the endothelial differentiation of bone marrow-derived MSCs[67]. This result suggests that in the same kind of cells, an LncRNA, such as MEG3, could possess various regulatory functions. Under specific stimulation, this LncRNA exhibits different functions through different mechanisms, which in turn regulate the different capacities of MSCs to meet various needs in vivo. This precise regulation is mediated by LncRNA, making MSCs universally functional from development to disease.
Myocytes contain skeletal muscle cells, myocardial cells and smooth muscle cells, which perform different functions in vivo. Although previous studies have claimed that MSCs could differentiate into all kinds of myocytes, only studies concerning LncRNA in the smooth muscle differentiation of MSCs have been reported thus far[68-70]. Li et al[71] reported that LncRNA-HULC is a promoter of the smooth muscle differentiation of adipose-derived MSCs through BMP9 expression and the activation balance between the Wnt/β-catenin/Notch signaling pathways. Several other LncRNAs, including H19, MEG3 and MALAT1, were also considered to be related to the myogenic differentiation of MSCs, although some of these studies were performed using C2C12 cells, an immortalized mouse myoblast cell line[72]. Since there is a vast difference between MSCs and C2C12 cells, the role of these LncRNAs in the myogenic differentiation of MSCs needs to be further confirmed.
Neural cells, derived from an ectoderm lineage, are the foundation of the nervous system but have relatively weaker regeneration capacity in vivo. Therefore, treatment for neurological disorders and nerve injury remains a worldwide problem. In recent years, studies have suggested that MSCs could be used as a novel and effective therapy for nervous system disease[73,74]. This therapeutic effect, on the one hand, is due to the immunoregulatory ability of MSCs and neuroprotective factor secretion from these cells, while on the other hand, this effect may result from MSCs differentiating into neural cells. Although whether MSCs can transdifferentiate into neural cells of other lineages in vivo is still controversial, many studies have demonstrated that MSCs could gradually differentiate into neural-like cells in vitro under specific induction conditions[75,76]. To study the in-depth mechanism, Wu et al[77] detected the LncRNA expression pattern of MSCs during their neurogenesis differentiation. Moreover, Farzi-Molan further reported that the neural-like differentiation of MSCs was under the regulation of LncRNA-H19, which functioned through the miRNA-675/IGFR axis[78]. In vivo experiments should be performed to confirm MSC neurogenesis and these mechanisms, which could help to improve their therapeutic effect on nervous system disease.
Similar to other cells, MSCs have other capacities, such as proliferation and antiapoptosis. As we suggest that LncRNA could affect various aspects of cells, Li et al[79] reported that LncRNA-HULC promoted MSC proliferation and inhibited apoptosis. In addition, this LncRNA also accelerated the migration of MSCs. Other LncRNAs, including H19 and MALAT1, were determined to regulate proliferation and apoptosis simultaneously. Moreover, these two LncRNAs affect the angiogenesis of MSCs[80,81]. However, detailed regulatory mechanisms were not clarified in these studies. The Wnt/β-catenin signaling pathway contributes to cell proliferation and differentiation. LncRNA-LET was proven to negatively modulate the proliferation of MSCs by inhibiting TGF-β expression and subsequent Wnt/β-catenin signal pathway activation[82]. In addition, LncRNA-p21 devitalized the Wnt/β-catenin signaling pathway and therefore participated in MSC senescence[83]. In another study, LncRNA-p21 was involved in the apoptosis of MSCs through the Wnt/β-catenin signal pathway[84].
A lingering issue in our mind is the question of why fewer studies about LncRNA in the immunoregulatory abilities of MSCs were performed. Except for a study of LncRNA-MALAT1-overexpressing MSCs that promote M2 macrophage polarization, no other studies have been reported to date[80]. Considering that the immunoregulatory ability of a series of immune cells is one of the most critical functions of MSCs, it is of great importance to investigate the role of LncRNA in this function, which could improve the clinical use of MSCs in the treatment of inflammatory disease.
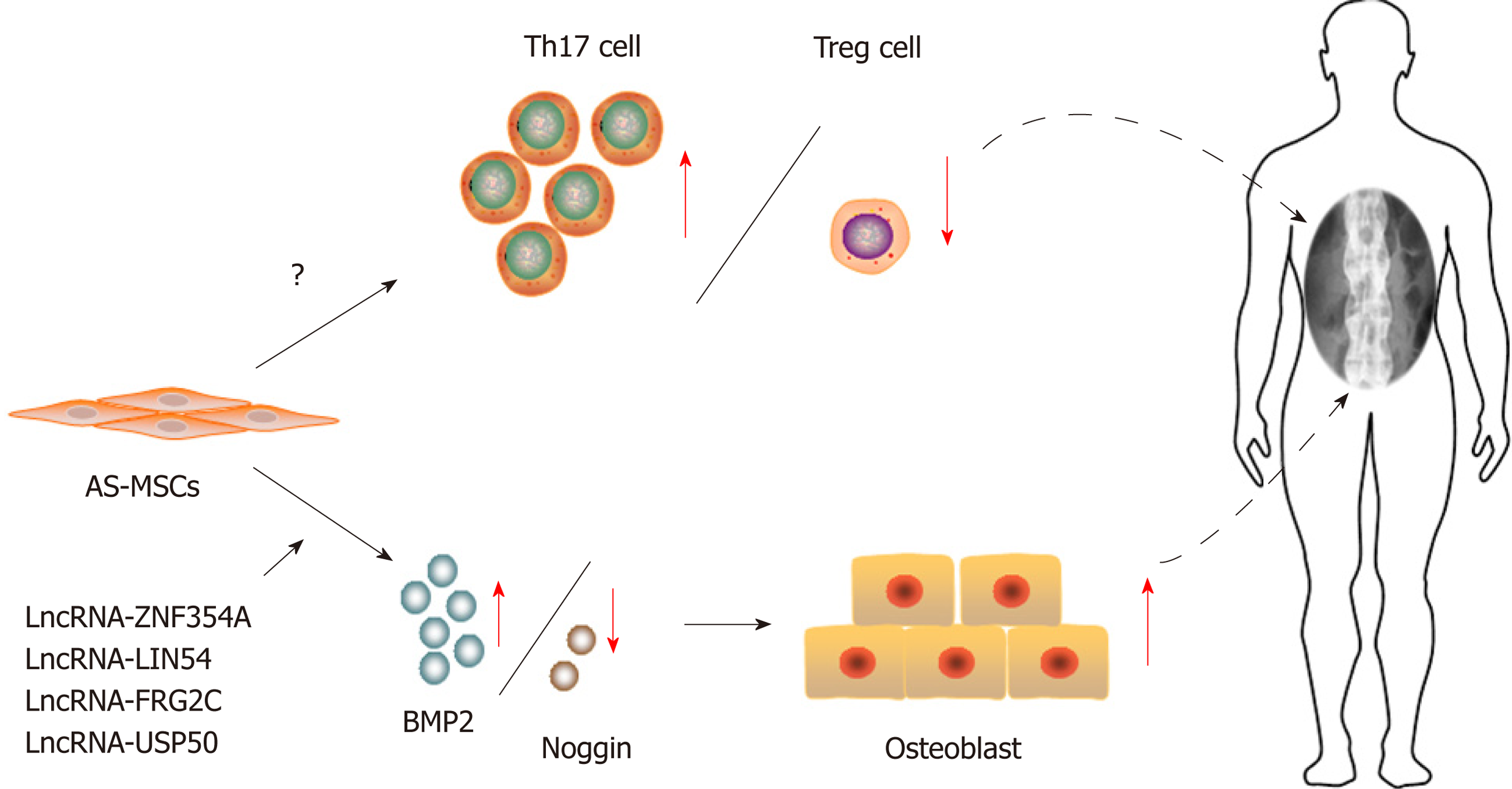
As MSCs greatly contribute to every physiological process through their powerful capacities, the regular functions of MSCs are critical to maintaining homeostasis in vivo. Therefore, it is not surprising that the abnormal function of MSCs has a great effect on our body or even leads to diseases. To date, MSC dysfunction has been demonstrated to be the critical pathogenesis in several diseases. For example, disorders in the immunoregulatory capacity of MSCs are related to autoimmune diseases, such as systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA)[85,86]. Additionally, the dysfunction in MSC differentiation contributes to diseases with structural abnormalities, including osteoporosis and ectopic ossification[87]. Ankylosing spondylitis (AS) is a kind of autoimmune disease characterized by chronic inflammation and pathological osteogenesis[88]. Through our studies, we demonstrate for the first time that MSCs from AS patients have reduced immunoregulation ability, which leads to disproportionality between Th17 cells and Treg cells. This dysfunction of MSCs contributes to the pathogenesis of chronic inflammation in AS[89]. Furthermore, we further determined that enhanced osteogenic differentiation ability was observed in the MSCs from AS patients, which is a critical reason for pathological osteogenesis in AS[90] (Figure 1). As LncRNA is a major regulator of MSC functions, it could be speculated that LncRNA may also participate in these processes.
Many studies have proven that LncRNA contributes to various diseases[14]. To confirm this hypothesis specifically in the MSC setting, we first detected and compared the LncRNA expression profiles between AS patient MSCs and normal MSCs during osteogenic differentiation and found that 520 LncRNAs were abnormally expressed during the osteogenesis of MSCs from AS patients. Among these 520 LncRNAs, Lnc-ZNF354A, Lnc-LIN54, Lnc-FRG2C, and Lnc-USP50 had tight relationships with the imbalance between BMP2 and Noggin, which leads to enhanced osteogenic differentiation ability and the subsequent pathological new bone formation[91] (Figure 2). In contrast, several other studies showed that abnormal LncRNA expression resulted in reduced osteogenic differentiation and related diseases. Zhuang et al[92] determined that LncRNA-MEG3 expression, an LncRNA that modulates MSC osteogenesis, as reported in a previous study, was downregulated in MSCs from patients with multiple myeloma. This downregulation of MEG3 inactivated the transcriptional activity of BMP4 and then led to the reduced osteogenic differentiation of MSCs from multiple myeloma patients. MSC dysfunction was a critical mechanism of osteoporosis, one of the pathological features in multiple myeloma[92]. Consistent with this study, a recent study demonstrated that LncRNA-MEG3 participated in the pathogenesis of osteoporosis through the same mechanism[93]. In addition, Wang et al[94] identified that the impaired osteogenic differentiation of MSCs from periodontitis patients resulted from the lower expression of LncRNA-POIR through a ceRNA mechanism. These results indicated that the abnormal expression of LncRNA resulted in disorder in MSC osteogenic differentiation, therefore contributing to abnormal bone metabolism in diseases. As other MSC dysfunctions have been tightly related to the pathological features of several diseases, especially the abnormal immunoregulatory ability of MSCs in inflammatory diseases, further research should be performed to identify critical LncRNAs and illustrate their mechanisms. These studies could help us to gain a deeper understanding of the occurrence and development of diseases.
A recent study showed that the exosomes from lung cancer altered the LncRNA expression profile of MSCs[95]. As MSCs interact with tumor cells and affect tumor progression, LncRNA is very likely to participate in this process[96]. In addition, this study emphasized that under the specific microenvironment of diseases, MSCs could be educated and their LncRNA expression profiles could be unique to specific conditions. Circulating MSCs have been found in peripheral blood and could be used as an auxiliary diagnosis method[97]. Therefore, we suggest that these educated MSCs with special LncRNA in blood circulation could be treated as a natural diagnostic kit for diseases. Detecting the specific LncRNA or distinct LncRNA groups in educated circulating MSCs in peripheral blood will be a novel and accurate method to diagnose these diseases.
To date, clinical studies of MSCs have been carried out extensively, and these results demonstrated that MSCs could be an effective treatment for some autoimmune diseases, including SLE and graft-versus-host disease[98,99]. Moreover, MSCs with differentiation potential could be used as seed cells in tissue and regeneration engineering such as fracture repair and osteoarthritis[100,101]. In 2011, we performed clinical research on AS and demonstrated that the intravenous infusion of allogenic MSCs was an effective and safe treatment for active AS patients who failed nonsteroidal anti-inflammatory drug treatment[102]. However, the clinical efficacy of MSC treatment could be further improved by enhancing the capacities of MSCs. Recently, a study determined that LncRNA was involved in MSC treatment for airway allergic inflammation in mice[103]. In addition, lncRNA MEG3 and MIAT could affect MSC treatment for erectile dysfunction[66,67]. As LncRNA is a critical functional regulator of MSCs, regulating specific LncRNA expression through gene editing technology may be a novel way to improve the clinical efficacy of MSCs. In autoimmune diseases, upregulating or downregulating LncRNA could induce the secretion of specific anti-inflammatory cytokines that target key pathogenic factors and then promote the immunoregulatory capacity of MSCs. On the other hand, modulating specific LncRNA could guide the directional differentiation of MSCs into specific cells, which may be committed to special use in tissue and regeneration engineering.
In this review, we highlight the critical role of LncRNA in the function of MSCs. Based on the discoveries described above, we conclude that LncRNA is an important functional regulator of MSCs, including their immunoregulation and differentiation capacities, which can greatly improve the clinical use of MSCs in the diagnosis and treatment of diseases. However, limitations still exist in these current studies. First, the detailed mechanism of LncRNA in MSCs warrants further study. What does control the LncRNA expression profile when MSCs exhibit functions? Several studies have reported that RNA modifications may be critical to this question, but the detailed mechanisms remain unknown. In addition, how does an LncRNA affect the ability of MSCs? Or does the LncRNA have tissue specificity in MSCs from various sources? Although many LncRNAs have been identified, their spatiotemporal specificities and functional mechanisms need to be clarified in the future. Second, in vivo experiments should be performed to ensure the actual function of these LncRNAs. Benefiting from the development of CRISPR/Cas9 technology, it is now possible to construct conditional knock-out (CKO) mice, which precisely inhibits the target LncRNA in MSCs. These CKO mice will help to illustrate the role of LncRNA in vivo. Finally, clinical research should be conducted to confirm the clinical application value of LncRNA. Clinical-based studies can help us to not only understand the actual pathogenesis of diseases but also improve the clinical application of MSCs in disease diagnosis and treatment.
Manuscript source: Invited manuscript
Specialty type: Cell and tissue engineering
Country of origin: South Korea
Peer-review report classification
Grade A (Excellent): A, A
Grade B (Very good): B
Grade C (Good): C, C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Andrukhov O, Castoria G, Garg M, Perez-Campo FM, Rui YF, Scuteri A, Ventura C S-Editor: Ji FF L-Editor: A E-Editor: Song H
| 1. | Friedenstein AJ, Chailakhyan RK, Latsinik NV, Panasyuk AF, Keiliss-Borok IV. Stromal cells responsible for transferring the microenvironment of the hemopoietic tissues. Cloning in vitro and retransplantation in vivo. Transplantation. 1974;17:331-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 998] [Cited by in RCA: 948] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 2. | Uccelli A, Moretta L, Pistoia V. Mesenchymal stem cells in health and disease. Nat Rev Immunol. 2008;8:726-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2360] [Cited by in RCA: 2698] [Article Influence: 168.6] [Reference Citation Analysis (0)] |
| 3. | Castro-Manrreza ME, Montesinos JJ. Immunoregulation by mesenchymal stem cells: biological aspects and clinical applications. J Immunol Res. 2015;2015:394917. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 239] [Cited by in RCA: 281] [Article Influence: 28.1] [Reference Citation Analysis (0)] |
| 4. | Wang Y, Chen X, Cao W, Shi Y. Plasticity of mesenchymal stem cells in immunomodulation: pathological and therapeutic implications. Nat Immunol. 2014;15:1009-1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 830] [Cited by in RCA: 1059] [Article Influence: 105.9] [Reference Citation Analysis (0)] |
| 5. | Barry F, Murphy M. Mesenchymal stem cells in joint disease and repair. Nat Rev Rheumatol. 2013;9:584-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 299] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 6. | Collas P. Programming differentiation potential in mesenchymal stem cells. Epigenetics. 2010;5:476-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Pistoia V, Raffaghello L. Mesenchymal stromal cells and autoimmunity. Int Immunol. 2017;29:49-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 8. | Karantalis V, Hare JM. Use of mesenchymal stem cells for therapy of cardiac disease. Circ Res. 2015;116:1413-1430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 287] [Cited by in RCA: 326] [Article Influence: 32.6] [Reference Citation Analysis (0)] |
| 9. | Djouad F, Bouffi C, Ghannam S, Noël D, Jorgensen C. Mesenchymal stem cells: innovative therapeutic tools for rheumatic diseases. Nat Rev Rheumatol. 2009;5:392-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 237] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 10. | Shi Y, Hu G, Su J, Li W, Chen Q, Shou P, Xu C, Chen X, Huang Y, Zhu Z, Huang X, Han X, Xie N, Ren G. Mesenchymal stem cells: a new strategy for immunosuppression and tissue repair. Cell Res. 2010;20:510-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 380] [Cited by in RCA: 435] [Article Influence: 29.0] [Reference Citation Analysis (0)] |
| 11. | Fahy N, Alini M, Stoddart MJ. Mechanical stimulation of mesenchymal stem cells: Implications for cartilage tissue engineering. J Orthop Res. 2018;36:52-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 116] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 12. | Almalki SG, Agrawal DK. Key transcription factors in the differentiation of mesenchymal stem cells. Differentiation. 2016;92:41-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 307] [Article Influence: 34.1] [Reference Citation Analysis (0)] |
| 13. | Rinaldi L, Benitah SA. Epigenetic regulation of adult stem cell function. FEBS J. 2015;282:1589-1604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Batista PJ, Chang HY. Long noncoding RNAs: cellular address codes in development and disease. Cell. 2013;152:1298-1307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1761] [Cited by in RCA: 2112] [Article Influence: 176.0] [Reference Citation Analysis (0)] |
| 15. | Fatica A, Bozzoni I. Long non-coding RNAs: new players in cell differentiation and development. Nat Rev Genet. 2014;15:7-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2002] [Cited by in RCA: 2315] [Article Influence: 192.9] [Reference Citation Analysis (0)] |
| 16. | Chen LL. Linking Long Noncoding RNA Localization and Function. Trends Biochem Sci. 2016;41:761-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 587] [Cited by in RCA: 782] [Article Influence: 86.9] [Reference Citation Analysis (0)] |
| 17. | Sun Q, Hao Q, Prasanth KV. Nuclear Long Noncoding RNAs: Key Regulators of Gene Expression. Trends Genet. 2018;34:142-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 427] [Cited by in RCA: 435] [Article Influence: 62.1] [Reference Citation Analysis (0)] |
| 18. | Noh JH, Kim KM, McClusky WG, Abdelmohsen K, Gorospe M. Cytoplasmic functions of long noncoding RNAs. Wiley Interdiscip Rev RNA. 2018;9:e1471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 301] [Article Influence: 43.0] [Reference Citation Analysis (0)] |
| 19. | Thomson DW, Dinger ME. Endogenous microRNA sponges: evidence and controversy. Nat Rev Genet. 2016;17:272-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1116] [Cited by in RCA: 1589] [Article Influence: 176.6] [Reference Citation Analysis (0)] |
| 20. | Liu B, Sun L, Liu Q, Gong C, Yao Y, Lv X, Lin L, Yao H, Su F, Li D, Zeng M, Song E. A cytoplasmic NF-κB interacting long noncoding RNA blocks IκB phosphorylation and suppresses breast cancer metastasis. Cancer Cell. 2015;27:370-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 661] [Cited by in RCA: 736] [Article Influence: 73.6] [Reference Citation Analysis (0)] |
| 21. | Liu J, Li Y, Lin B, Sheng Y, Yang L. HBL1 Is a Human Long Noncoding RNA that Modulates Cardiomyocyte Development from Pluripotent Stem Cells by Counteracting MIR1. Dev Cell. 2017;42:333-348.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 22. | Wang X, Sun W, Shen W, Xia M, Chen C, Xiang D, Ning B, Cui X, Li H, Li X, Ding J, Wang H. Long non-coding RNA DILC regulates liver cancer stem cells via IL-6/STAT3 axis. J Hepatol. 2016;64:1283-1294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 247] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 23. | Xu C, Zhang Y, Wang Q, Xu Z, Jiang J, Gao Y, Gao M, Kang J, Wu M, Xiong J, Ji K, Yuan W, Wang Y, Liu H. Long non-coding RNA GAS5 controls human embryonic stem cell self-renewal by maintaining NODAL signalling. Nat Commun. 2016;7:13287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 84] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 24. | Ramos AD, Andersen RE, Liu SJ, Nowakowski TJ, Hong SJ, Gertz C, Salinas RD, Zarabi H, Kriegstein AR, Lim DA. The long noncoding RNA Pnky regulates neuronal differentiation of embryonic and postnatal neural stem cells. Cell Stem Cell. 2015;16:439-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 274] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 25. | Deschaseaux F, Pontikoglou C, Sensébé L. Bone regeneration: the stem/progenitor cells point of view. J Cell Mol Med. 2010;14:103-115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 46] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 26. | Song WQ, Gu WQ, Qian YB, Ma X, Mao YJ, Liu WJ. Identification of long non-coding RNA involved in osteogenic differentiation from mesenchymal stem cells using RNA-Seq data. Genet Mol Res. 2015;14:18268-18279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 27. | Wang L, Wang Y, Li Z, Li Z, Yu B. Differential expression of long noncoding ribonucleic acids during osteogenic differentiation of human bone marrow mesenchymal stem cells. Int Orthop. 2015;39:1013-1019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 28. | Zhang W, Dong R, Diao S, Du J, Fan Z, Wang F. Differential long noncoding RNA/mRNA expression profiling and functional network analysis during osteogenic differentiation of human bone marrow mesenchymal stem cells. Stem Cell Res Ther. 2017;8:30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 115] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 29. | Qiu X, Jia B, Sun X, Hu W, Chu H, Xu S, Zhao J. The Critical Role of Long Noncoding RNA in Osteogenic Differentiation of Human Bone Marrow Mesenchymal Stem Cells. Biomed Res Int. 2017;2017:5045827. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 30. | Huang Y, Zheng Y, Jia L, Li W. Long Noncoding RNA H19 Promotes Osteoblast Differentiation Via TGF-β1/Smad3/HDAC Signaling Pathway by Deriving miR-675. Stem Cells. 2015;33:3481-3492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 247] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 31. | Jiang XR, Guo N, Li XQ, Yang HY, Wang K, Zhang CL, Li GS, Li GD. Long non-coding RNA HULC promotes proliferation and osteogenic differentiation of bone mesenchymal stem cells via down-regulation of miR-195. Eur Rev Med Pharmacol Sci. 2018;22:2954-2965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 32. | Gao Y, Xiao F, Wang C, Wang C, Cui P, Zhang X, Chen X. Long noncoding RNA MALAT1 promotes osterix expression to regulate osteogenic differentiation by targeting miRNA-143 in human bone marrow-derived mesenchymal stem cells. J Cell Biochem. 2018;119:6986-6996. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 91] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 33. | Feng X, Lin T, Liu X, Yang C, Yang S, Fu D. Long non-coding RNA BDNF-AS modulates osteogenic differentiation of bone marrow-derived mesenchymal stem cells. Mol Cell Biochem. 2018;445:59-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 34. | Zhang J, Tao Z, Wang Y. Long non‑coding RNA DANCR regulates the proliferation and osteogenic differentiation of human bone-derived marrow mesenchymal stem cells via the p38 MAPK pathway. Int J Mol Med. 2018;41:213-219. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 54] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 35. | Tang S, Xie Z, Wang P, Li J, Wang S, Liu W, Li M, Wu X, Su H, Cen S, Ye G, Zheng G, Wu Y, Shen H. LncRNA-OG Promotes the Osteogenic Differentiation of Bone Marrow-Derived Mesenchymal Stem Cells Under the Regulation of hnRNPK. Stem Cells. 2019;37:270-283. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 71] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 36. | Liu J, Chen B, Yan F, Yang W. The Influence of Inflammatory Cytokines on the Proliferation and Osteoblastic Differentiation of MSCs. Curr Stem Cell Res Ther. 2017;12:401-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 37. | Li H, Zhang Z, Chen Z, Zhang D. Osteogenic growth peptide promotes osteogenic differentiation of mesenchymal stem cells mediated by LncRNA AK141205-induced upregulation of CXCL13. Biochem Biophys Res Commun. 2015;466:82-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 38. | Cui Y, Lu S, Tan H, Li J, Zhu M, Xu Y. Silencing of Long Non-Coding RNA NONHSAT009968 Ameliorates the Staphylococcal Protein A-Inhibited Osteogenic Differentiation in Human Bone Mesenchymal Stem Cells. Cell Physiol Biochem. 2016;39:1347-1359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 39. | Cao B, Liu N, Wang W. High glucose prevents osteogenic differentiation of mesenchymal stem cells via lncRNA AK028326/CXCL13 pathway. Biomed Pharmacother. 2016;84:544-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 40. | Barradas AM, Monticone V, Hulsman M, Danoux C, Fernandes H, Tahmasebi Birgani Z, Barrère-de Groot F, Yuan H, Reinders M, Habibovic P, van Blitterswijk C, de Boer J. Molecular mechanisms of biomaterial-driven osteogenic differentiation in human mesenchymal stromal cells. Integr Biol (Camb). 2013;5:920-931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 76] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 41. | Chun C, Lim HJ, Hong KY, Park KH, Song SC. The use of injectable, thermosensitive poly(organophosphazene)-RGD conjugates for the enhancement of mesenchymal stem cell osteogenic differentiation. Biomaterials. 2009;30:6295-6308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 73] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 42. | Lv L, Liu Y, Zhang P, Bai X, Ma X, Wang Y, Li H, Wang L, Zhou Y. The epigenetic mechanisms of nanotopography-guided osteogenic differentiation of mesenchymal stem cells via high-throughput transcriptome sequencing. Int J Nanomedicine. 2018;13:5605-5623. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 43. | Izadpanahi M, Seyedjafari E, Arefian E, Hamta A, Hosseinzadeh S, Kehtari M, Soleimani M. Nanotopographical cues of electrospun PLLA efficiently modulate non-coding RNA network to osteogenic differentiation of mesenchymal stem cells during BMP signaling pathway. Mater Sci Eng C Mater Biol Appl. 2018;93:686-703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 44. | Parker R, Kim SJ, Gao B. Alcohol, adipose tissue and liver disease: mechanistic links and clinical considerations. Nat Rev Gastroenterol Hepatol. 2018;15:50-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 132] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 45. | Gernapudi R, Wolfson B, Zhang Y, Yao Y, Yang P, Asahara H, Zhou Q. MicroRNA 140 Promotes Expression of Long Noncoding RNA NEAT1 in Adipogenesis. Mol Cell Biol. 2015;36:30-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 96] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 46. | Xiao T, Liu L, Li H, Sun Y, Luo H, Li T, Wang S, Dalton S, Zhao RC, Chen R. Long Noncoding RNA ADINR Regulates Adipogenesis by Transcriptionally Activating C/EBPα. Stem Cell Reports. 2015;5:856-865. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 124] [Cited by in RCA: 138] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 47. | Li M, Xie Z, Wang P, Li J, Liu W, Tang S, Liu Z, Wu X, Wu Y, Shen H. The long noncoding RNA GAS5 negatively regulates the adipogenic differentiation of MSCs by modulating the miR-18a/CTGF axis as a ceRNA. Cell Death Dis. 2018;9:554. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 68] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 48. | Kalwa M, Hänzelmann S, Otto S, Kuo CC, Franzen J, Joussen S, Fernandez-Rebollo E, Rath B, Koch C, Hofmann A, Lee SH, Teschendorff AE, Denecke B, Lin Q, Widschwendter M, Weinhold E, Costa IG, Wagner W. The lncRNA HOTAIR impacts on mesenchymal stem cells via triple helix formation. Nucleic Acids Res. 2016;44:10631-10643. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 127] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 49. | Yuan Z, Li Q, Luo S, Liu Z, Luo D, Zhang B, Zhang D, Rao P, Xiao J. PPARγ and Wnt Signaling in Adipogenic and Osteogenic Differentiation of Mesenchymal Stem Cells. Curr Stem Cell Res Ther. 2016;11:216-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 165] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 50. | Kim M, Kim C, Choi YS, Kim M, Park C, Suh Y. Age-related alterations in mesenchymal stem cells related to shift in differentiation from osteogenic to adipogenic potential: implication to age-associated bone diseases and defects. Mech Ageing Dev. 2012;133:215-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 149] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 51. | van Zoelen EJ, Duarte I, Hendriks JM, van der Woning SP. TGFβ-induced switch from adipogenic to osteogenic differentiation of human mesenchymal stem cells: identification of drug targets for prevention of fat cell differentiation. Stem Cell Res Ther. 2016;7:123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 58] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 52. | Huang Y, Zheng Y, Jin C, Li X, Jia L, Li W. Long Non-coding RNA H19 Inhibits Adipocyte Differentiation of Bone Marrow Mesenchymal Stem Cells through Epigenetic Modulation of Histone Deacetylases. Sci Rep. 2016;6:28897. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 105] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 53. | Shang G, Wang Y, Xu Y, Zhang S, Sun X, Guan H, Zhao X, Wang Y, Li Y, Zhao G. Long non-coding RNA TCONS_00041960 enhances osteogenesis and inhibits adipogenesis of rat bone marrow mesenchymal stem cell by targeting miR-204-5p and miR-125a-3p. J Cell Physiol. 2018;233:6041-6051. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 67] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 54. | Li CJ, Xiao Y, Yang M, Su T, Sun X, Guo Q, Huang Y, Luo XH. Long noncoding RNA Bmncr regulates mesenchymal stem cell fate during skeletal aging. J Clin Invest. 2018;128:5251-5266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 170] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 55. | Strioga M, Viswanathan S, Darinskas A, Slaby O, Michalek J. Same or not the same? Comparison of adipose tissue-derived versus bone marrow-derived mesenchymal stem and stromal cells. Stem Cells Dev. 2012;21:2724-2752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 540] [Cited by in RCA: 602] [Article Influence: 46.3] [Reference Citation Analysis (0)] |
| 56. | Wang Q, Li Y, Zhang Y, Ma L, Lin L, Meng J, Jiang L, Wang L, Zhou P, Zhang Y. LncRNA MEG3 inhibited osteogenic differentiation of bone marrow mesenchymal stem cells from postmenopausal osteoporosis by targeting miR-133a-3p. Biomed Pharmacother. 2017;89:1178-1186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 160] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 57. | Li Z, Jin C, Chen S, Zheng Y, Huang Y, Jia L, Ge W, Zhou Y. Long non-coding RNA MEG3 inhibits adipogenesis and promotes osteogenesis of human adipose-derived mesenchymal stem cells via miR-140-5p. Mol Cell Biochem. 2017;433:51-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 93] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 58. | Yu DA, Han J, Kim BS. Stimulation of chondrogenic differentiation of mesenchymal stem cells. Int J Stem Cells. 2012;5:16-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 63] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 59. | Wang L, Li Z, Li Z, Yu B, Wang Y. Long noncoding RNAs expression signatures in chondrogenic differentiation of human bone marrow mesenchymal stem cells. Biochem Biophys Res Commun. 2015;456:459-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 60. | Cao Z, Huang S, Li J, Bai Y, Dou C, Liu C, Kang F, Gong X, Ding H, Hou T, Dong S. Long noncoding RNA expression profiles in chondrogenic and hypertrophic differentiation of mouse mesenchymal stem cells. Funct Integr Genomics. 2017;17:739-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 61. | Barter MJ, Gomez R, Hyatt S, Cheung K, Skelton AJ, Xu Y, Clark IM, Young DA. The long non-coding RNA ROCR contributes to SOX9 expression and chondrogenic differentiation of human mesenchymal stem cells. Development. 2017;144:4510-4521. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 60] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 62. | Ou F, Su K, Sun J, Liao W, Yao Y, Zheng Y, Zhang Z. The LncRNA ZBED3-AS1 induces chondrogenesis of human synovial fluid mesenchymal stem cells. Biochem Biophys Res Commun. 2017;487:457-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 63. | Zhang L, Sun X, Chen S, Yang C, Shi B, Zhou L, Zhao J. Long noncoding RNA DANCR regulates miR-1305-Smad 4 axis to promote chondrogenic differentiation of human synovium-derived mesenchymal stem cells. Biosci Rep. 2017;37:pii: BSR20170347. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 64. | Pantsulaia Ia, Ciszewski Ciszewski, Niewiarowska J. Senescent endothelial cells: Potential modulators of immunosenescence and ageing. Ageing Res Rev. 2016;29:13-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 54] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 65. | Sun C, Huang L, Li Z, Leng K, Xu Y, Jiang X, Cui Y. Long non-coding RNA MIAT in development and disease: a new player in an old game. J Biomed Sci. 2018;25:23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 88] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 66. | Wang H, Ding XG, Yang JJ, Li SW, Zheng H, Gu CH, Jia ZK, Li L. LncRNA MIAT facilitated BM-MSCs differentiation into endothelial cells and restored erectile dysfunction via targeting miR-200a in a rat model of erectile dysfunction. Eur J Cell Biol. 2018;97:180-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 67. | Sun X, Luo LH, Feng L, Li DS. Down-regulation of lncRNA MEG3 promotes endothelial differentiation of bone marrow derived mesenchymal stem cells in repairing erectile dysfunction. Life Sci. 2018;208:246-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 68. | Li N, Sanyour H, Remund T, Kelly P, Hong Z. Vascular extracellular matrix and fibroblasts-coculture directed differentiation of human mesenchymal stem cells toward smooth muscle-like cells for vascular tissue engineering. Mater Sci Eng C Mater Biol Appl. 2018;93:61-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 69. | Sridhar S, Venugopal JR, Sridhar R, Ramakrishna S. Cardiogenic differentiation of mesenchymal stem cells with gold nanoparticle loaded functionalized nanofibers. Colloids Surf B Biointerfaces. 2015;134:346-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 64] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 70. | Chan J, O'Donoghue K, Gavina M, Torrente Y, Kennea N, Mehmet H, Stewart H, Watt DJ, Morgan JE, Fisk NM. Galectin-1 induces skeletal muscle differentiation in human fetal mesenchymal stem cells and increases muscle regeneration. Stem Cells. 2006;24:1879-1891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 109] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 71. | Li Y, Shan Z, Yang B, Yang D, Men C, Cui Y, Wu J. LncRNA HULC promotes epithelial and smooth-muscle-like differentiation of adipose-derived stem cells by upregulation of BMP9. Pharmazie. 2018;73:49-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 72. | Tye CE, Gordon JA, Martin-Buley LA, Stein JL, Lian JB, Stein GS. Could lncRNAs be the missing links in control of mesenchymal stem cell differentiation? J Cell Physiol. 2015;230:526-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 72] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 73. | Harris VK, Stark J, Vyshkina T, Blackshear L, Joo G, Stefanova V, Sara G, Sadiq SA. Phase I Trial of Intrathecal Mesenchymal Stem Cell-derived Neural Progenitors in Progressive Multiple Sclerosis. EBioMedicine. 2018;29:23-30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 117] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 74. | Xu P, Yang X. The Efficacy and Safety of Mesenchymal Stem Cell Transplantation for Spinal Cord Injury Patients: A Meta-Analysis and Systematic Review. Cell Transplant. 2019;28:36-46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 69] [Cited by in RCA: 65] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 75. | Harris VK, Faroqui R, Vyshkina T, Sadiq SA. Characterization of autologous mesenchymal stem cell-derived neural progenitors as a feasible source of stem cells for central nervous system applications in multiple sclerosis. Stem Cells Transl Med. 2012;1:536-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 71] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 76. | Fu L, Zhu L, Huang Y, Lee TD, Forman SJ, Shih CC. Derivation of neural stem cells from mesenchymal stemcells: evidence for a bipotential stem cell population. Stem Cells Dev. 2008;17:1109-1121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 102] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 77. | Wu AM, Ni WF, Huang ZY, Li QL, Wu JB, Xu HZ, Yin LH. Analysis of differentially expressed lncRNAs in differentiation of bone marrow stem cells into neural cells. J Neurol Sci. 2015;351:160-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 78. | Farzi-Molan A, Babashah S, Bakhshinejad B, Atashi A, Fakhr Taha M. Down-regulation of the non-coding RNA H19 and its derived miR-675 is concomitant with up-regulation of insulin-like growth factor receptor type 1 during neural-like differentiation of human bone marrow mesenchymal stem cells. Cell Biol Int. 2018;42:940-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 79. | Li X, Wang J, Pan Y, Xu Y, Liu D, Hou Y, Zhao G. Long non-coding RNA HULC affects the proliferation, apoptosis, migration, and invasion of mesenchymal stem cells. Exp Biol Med (Maywood). 2018;243:1074-1082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 80. | Li X, Song Y, Liu F, Liu D, Miao H, Ren J, Xu J, Ding L, Hu Y, Wang Z, Hou Y, Zhao G. Long Non-Coding RNA MALAT1 Promotes Proliferation, Angiogenesis, and Immunosuppressive Properties of Mesenchymal Stem Cells by Inducing VEGF and IDO. J Cell Biochem. 2017;118:2780-2791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 84] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 81. | Hou J, Wang L, Wu Q, Zheng G, Long H, Wu H, Zhou C, Guo T, Zhong T, Wang L, Chen X, Wang T. Long noncoding RNA H19 upregulates vascular endothelial growth factor A to enhance mesenchymal stem cells survival and angiogenic capacity by inhibiting miR-199a-5p. Stem Cell Res Ther. 2018;9:109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 77] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 82. | Jin X, Zhang Z, Lu Y, Fan Z. Suppression of long non-coding RNA LET potentiates bone marrow-derived mesenchymal stem cells (BMSCs) proliferation by up-regulating TGF-β1. J Cell Biochem. 2018;119:2843-2850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 83. | Xia W, Zhuang L, Deng X, Hou M. Long noncoding RNA‑p21 modulates cellular senescence via the Wnt/β‑catenin signaling pathway in mesenchymal stem cells. Mol Med Rep. 2017;16:7039-7047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 84. | Xia W, Zhuang L, Hou M. Role of lincRNA‑p21 in the protective effect of macrophage inhibition factor against hypoxia/serum deprivation‑induced apoptosis in mesenchymal stem cells. Int J Mol Med. 2018;42:2175-2184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 85. | Sun LY, Zhang HY, Feng XB, Hou YY, Lu LW, Fan LM. Abnormality of bone marrow-derived mesenchymal stem cells in patients with systemic lupus erythematosus. Lupus. 2007;16:121-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 139] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 86. | Bocelli-Tyndall C, Bracci L, Spagnoli G, Braccini A, Bouchenaki M, Ceredig R, Pistoia V, Martin I, Tyndall A. Bone marrow mesenchymal stromal cells (BM-MSCs) from healthy donors and auto-immune disease patients reduce the proliferation of autologous- and allogeneic-stimulated lymphocytes in vitro. Rheumatology (Oxford). 2007;46:403-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 147] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 87. | You L, Pan L, Chen L, Gu W, Chen J. MiR-27a is Essential for the Shift from Osteogenic Differentiation to Adipogenic Differentiation of Mesenchymal Stem Cells in Postmenopausal Osteoporosis. Cell Physiol Biochem. 2016;39:253-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 90] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 88. | Taurog JD, Chhabra A, Colbert RA. Ankylosing Spondylitis and Axial Spondyloarthritis. N Engl J Med. 2016;375:1303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 55] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 89. | Wu Y, Ren M, Yang R, Liang X, Ma Y, Tang Y, Huang L, Ye J, Chen K, Wang P, Shen H. Reduced immunomodulation potential of bone marrow-derived mesenchymal stem cells induced CCR4+CCR6+ Th/Treg cell subset imbalance in ankylosing spondylitis. Arthritis Res Ther. 2011;13:R29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 69] [Cited by in RCA: 73] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 90. | Xie Z, Wang P, Li Y, Deng W, Zhang X, Su H, Li D, Wu Y, Shen H. Imbalance Between Bone Morphogenetic Protein 2 and Noggin Induces Abnormal Osteogenic Differentiation of Mesenchymal Stem Cells in Ankylosing Spondylitis. Arthritis Rheumatol. 2016;68:430-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 93] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 91. | Xie Z, Li J, Wang P, Li Y, Wu X, Wang S, Su H, Deng W, Liu Z, Cen S, Ouyang Y, Wu Y, Shen H. Differential Expression Profiles of Long Noncoding RNA and mRNA of Osteogenically Differentiated Mesenchymal Stem Cells in Ankylosing Spondylitis. J Rheumatol. 2016;43:1523-1531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 92. | Zhuang W, Ge X, Yang S, Huang M, Zhuang W, Chen P, Zhang X, Fu J, Qu J, Li B. Upregulation of lncRNA MEG3 Promotes Osteogenic Differentiation of Mesenchymal Stem Cells From Multiple Myeloma Patients By Targeting BMP4 Transcription. Stem Cells. 2015;33:1985-1997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 221] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 93. | Chen S, Jia L, Zhang S, Zheng Y, Zhou Y. DEPTOR regulates osteogenic differentiation via inhibiting MEG3-mediated activation of BMP4 signaling and is involved in osteoporosis. Stem Cell Res Ther. 2018;9:185. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 94. | Wang L, Wu F, Song Y, Li X, Wu Q, Duan Y, Jin Z. Long noncoding RNA related to periodontitis interacts with miR-182 to upregulate osteogenic differentiation in periodontal mesenchymal stem cells of periodontitis patients. Cell Death Dis. 2016;7:e2327. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 143] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 95. | Wang S, Li X, Zhu R, Han Q, Zhao RC. Lung cancer exosomes initiate global long non-coding RNA changes in mesenchymal stem cells. Int J Oncol. 2016;48:681-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 96. | Ridge SM, Sullivan FJ, Glynn SA. Mesenchymal stem cells: key players in cancer progression. Mol Cancer. 2017;16:31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 288] [Cited by in RCA: 414] [Article Influence: 51.8] [Reference Citation Analysis (0)] |
| 97. | van der Velden DL, Houthuijzen JM, Roodhart JML, van Werkhoven E, Voest EE. Detection of endogenously circulating mesenchymal stem cells in human cancer patients. Int J Cancer. 2018;143:2516-2524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 98. | Introna M, Lucchini G, Dander E, Galimberti S, Rovelli A, Balduzzi A, Longoni D, Pavan F, Masciocchi F, Algarotti A, Micò C, Grassi A, Deola S, Cavattoni I, Gaipa G, Belotti D, Perseghin P, Parma M, Pogliani E, Golay J, Pedrini O, Capelli C, Cortelazzo S, D'Amico G, Biondi A, Rambaldi A, Biagi E. Treatment of graft versus host disease with mesenchymal stromal cells: a phase I study on 40 adult and pediatric patients. Biol Blood Marrow Transplant. 2014;20:375-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 168] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 99. | Wang D, Wang S, Huang S, Zhang Z, Yuan X, Feng X, Lu L, Sun L. Serum IFN-γ Predicts the Therapeutic Effect of Mesenchymal Stem Cells Transplantation in Systemic Lupus Erythematosus Patients. Stem Cells Transl Med. 2017;6:1777-1785. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 100. | Rapp AE, Bindl R, Heilmann A, Erbacher A, Müller I, Brenner RE, Ignatius A. Systemic mesenchymal stem cell administration enhances bone formation in fracture repair but not load-induced bone formation. Eur Cell Mater. 2015;29:22-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 101. | Saulnier N, Viguier E, Perrier-Groult E, Chenu C, Pillet E, Roger T, Maddens S, Boulocher C. Intra-articular administration of xenogeneic neonatal Mesenchymal Stromal Cells early after meniscal injury down-regulates metalloproteinase gene expression in synovium and prevents cartilage degradation in a rabbit model of osteoarthritis. Osteoarthritis Cartilage. 2015;23:122-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 69] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 102. | Wang P, Li Y, Huang L, Yang J, Yang R, Deng W, Liang B, Dai L, Meng Q, Gao L, Chen X, Shen J, Tang Y, Zhang X, Hou J, Ye J, Chen K, Cai Z, Wu Y, Shen H. Effects and safety of allogenic mesenchymal stem cell intravenous infusion in active ankylosing spondylitis patients who failed NSAIDs: a 20-week clinical trial. Cell Transplant. 2014;23:1293-1303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 53] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 103. | Wang SY, Fan XL, Yu QN, Deng MX, Sun YQ, Gao WX, Li CL, Shi JB, Fu QL. The lncRNAs involved in mouse airway allergic inflammation following induced pluripotent stem cell-mesenchymal stem cell treatment. Stem Cell Res Ther. 2017;8:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |