Copyright
©2014 Baishideng Publishing Group Co.
World J Stem Cells. Apr 26, 2014; 6(2): 213-229
Published online Apr 26, 2014. doi: 10.4252/wjsc.v6.i2.213
Published online Apr 26, 2014. doi: 10.4252/wjsc.v6.i2.213
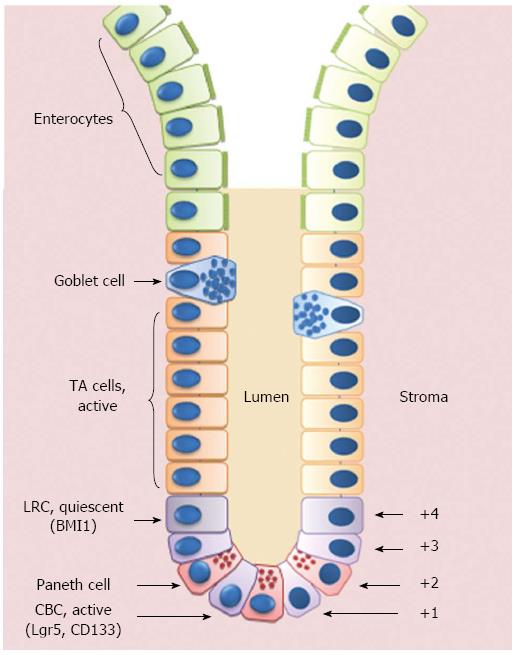
Figure 1 Schematic representation of the crypt/villus axis.
Putative intestinal stem cells (ISCs) reside either at the crypt base, between Paneth cells, as Crypt Base Columnar Cells (CBCs), or in position +4 from the bottom of the crypt, as Label Retaining Cells (LRCs). ISCs give rise to Transit Amplifying (TA) cells that are able to migrate upwards and progressively maturate losing their proliferative capability to become fully-differentiated villous epithelial cells.
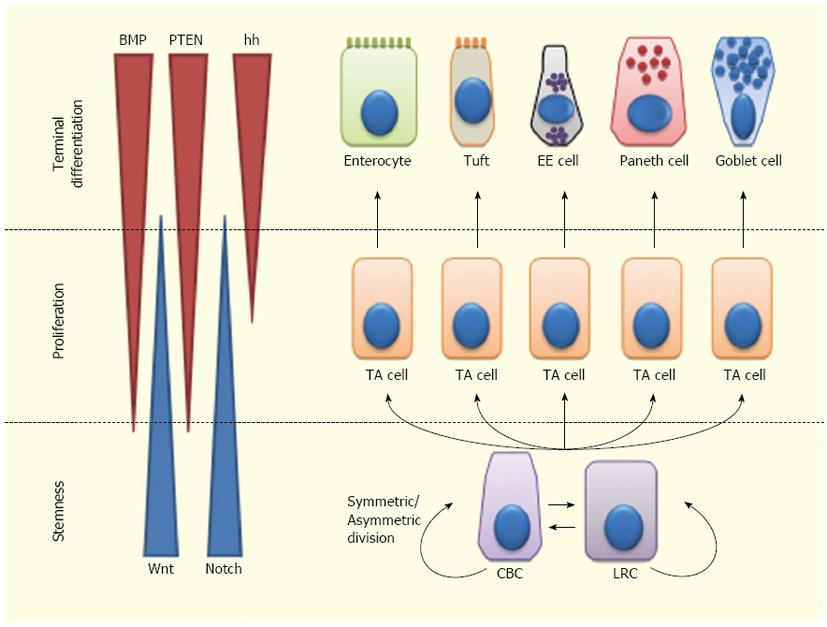
Figure 2 Lineage specification of intestinal stem cells.
Intestinal stem cells (ISCs)-Crypt Columnar Cells (CBCs) and Label Retaining Cells (LRCs)-can divide asymmetrically or symmetrically to maintain the stem cell compartment. ISCs give rise to Transit Amplifying (TA) cells which actively proliferate and can further differentiate into enterocytes, tuft cells, enteroendocrine (EE) cells or goblet cells. Wnt signaling maintains the stem-like phenotype of ISCs, while Notch signaling maintains the proliferation of progenitor cells. In the upper crypt region, hedgehog (hh) triggers BMP expression in stromal cells which activates PTEN expression; all these factors inhibit Wnt signaling in the ISC niche.
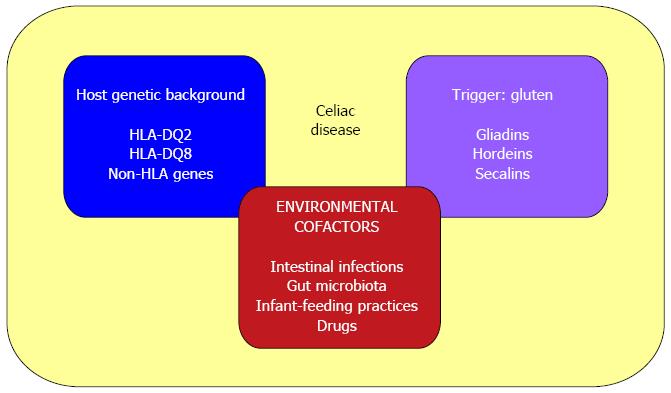
Figure 3 Causative factors in celiac disease.
The pathogenesis of celiac disease involves: (1) host genetic background (HLA-DQ2 or DQ8 and other non-HLA genes); (2) an external trigger (gluten); and (3) environmental cofactors (such as intestinal pathogens, altered gut microbiota composition, infant-feeding practices and some immune-modulatory drugs).
- Citation: Piscaglia AC. Intestinal stem cells and celiac disease. World J Stem Cells 2014; 6(2): 213-229
- URL: https://www.wjgnet.com/1948-0210/full/v6/i2/213.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v6.i2.213