Copyright
©The Author(s) 2024.
World J Stem Cells. Apr 26, 2024; 16(4): 375-388
Published online Apr 26, 2024. doi: 10.4252/wjsc.v16.i4.375
Published online Apr 26, 2024. doi: 10.4252/wjsc.v16.i4.375
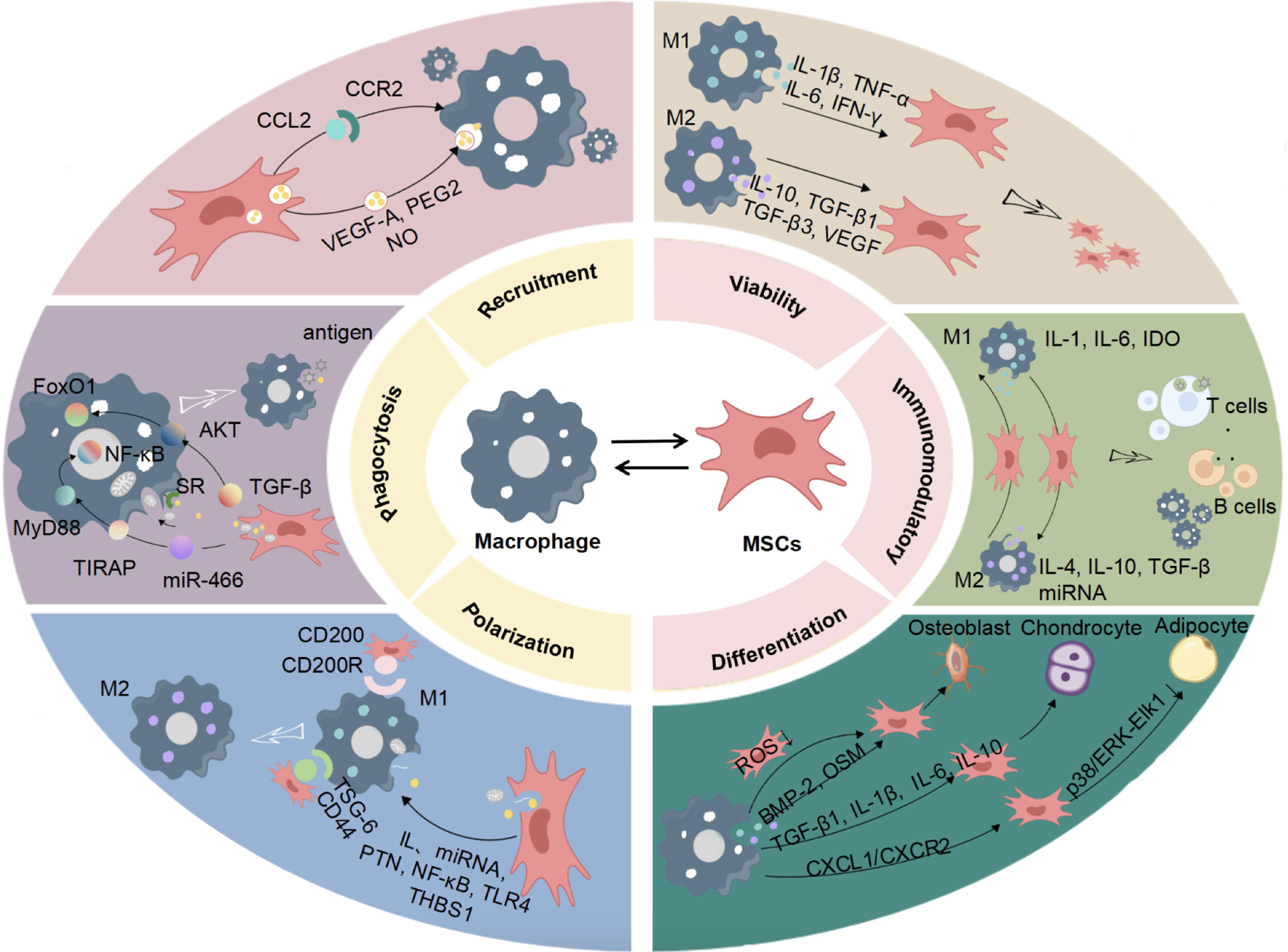
Figure 1 Bidirectional interaction between mesenchymal stem cells and macrophages.
Mesenchymal stem cells (MSCs) can facilitate the proliferation and infiltration of macrophages, enhance their phagocytic capabilities, and promote the polarization of macrophages phenotypes. Macrophages are capable of activating MSCs, boosting their proliferation and migration abilities, influencing the immune regulatory microenvironment of MSCs, and promoting the multilineage differentiation of MSCs through the secretion of inflammatory-related factors, chemokines, and osteogenic-related factors. MSC: Mesenchymal stem cell; CCL2: C-C motif chemokine ligand 2; CCR2: C-C motif chemokine receptor 2; VEGF-A: Vascular endothelial growth factor-A; PEG2: Prostaglandin E2; IL: Interleukin; IFN: Interferon; TGF-β: Transforming growth factor beta; FoxO1: Forkhead box transcription factor O1; NF-κB: Nuclear factor kappa-B; MyD88: Myeloid differentiation primary response gene 88; TIRAP: Toll-interleukin-1 receptor domain-containing adaptor protein; TIR: Toll-interleukin-1 receptor; SR: Scavenger receptor; AKT: Protein kinase B; PTN: Pleiotropic hormones; TLR4: Toll-like receptor 4; THBS-1: Thrombospondin-1; BMP-2: Bone morphogenetic protein-2; OSM: Oncostatin-M; IDO: Indoleamine 2,3-dioxygenase; HGF: Hepatocyte growth factor; miRNA: MicroRNA; ROS: Reactive oxygen species; NO: Nitric oxide.
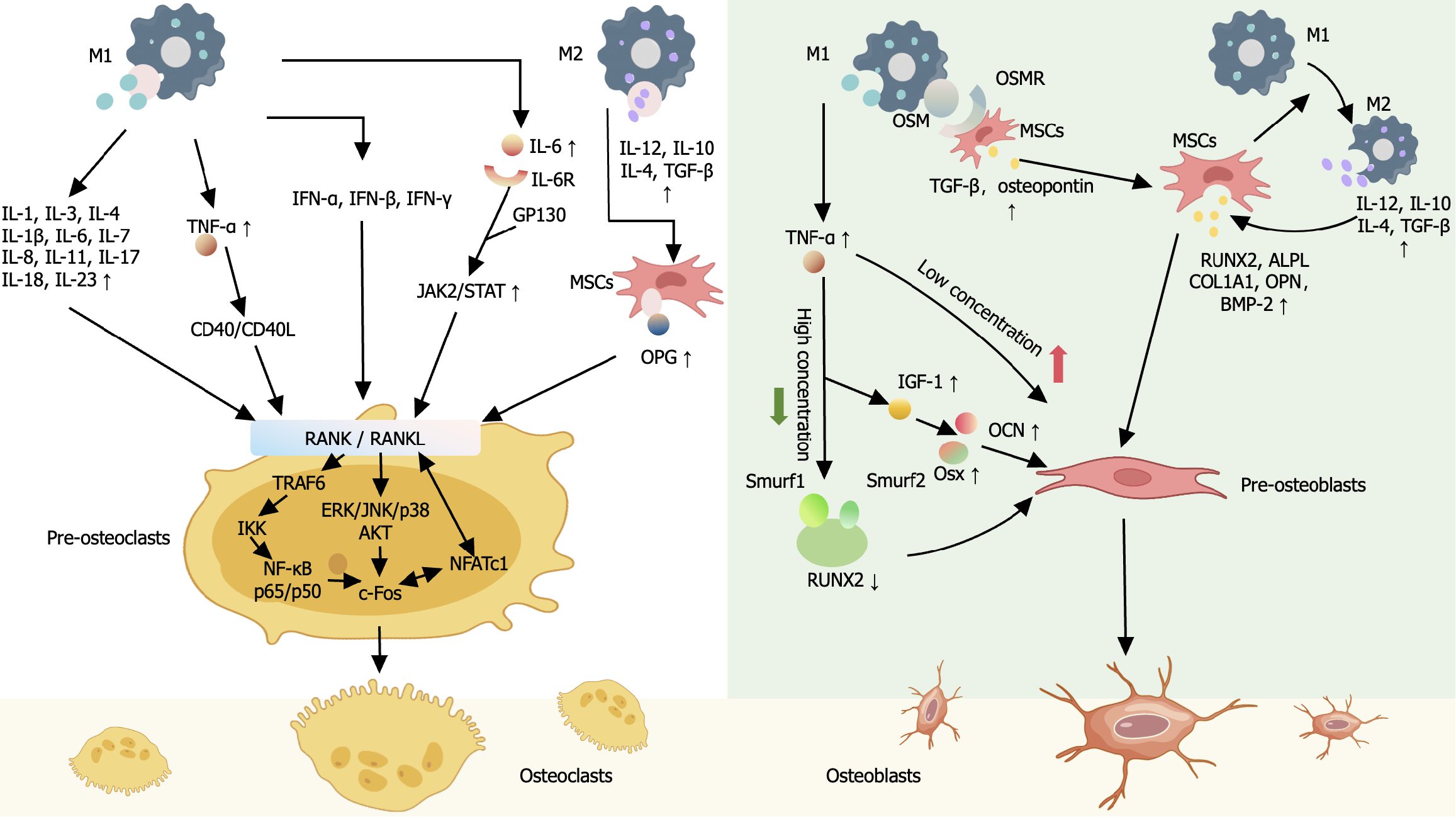
Figure 2 The dialogue between mesenchymal stem cells and macrophages in mediating the immune environment and bone tissue.
Multiple inflammatory factors secreted by M1 macrophages can promote the differentiation of osteoclast precursors into osteoclasts. When the inflammatory factors accumulate to a certain extent, the differentiation of osteoclasts is inhibited by the action of osteogenic factors secreted by M2 macrophages and mesenchymal stem cells (MSCs). Macrophages can promote the secretion of various osteogenic induction factors by MSCs through direct contact or by secreting various bioactive factors indirectly, inducing further differentiation of osteogenic precursor cells into osteoblasts. MSC: Mesenchymal stem cell; RANK: Receptor activator of nuclear factor kappa-B; RANKL: Receptor activator of nuclear factor kappa-B ligand; NF-κB: Nuclear factor kappa-B; TRAF6: Tumor necrosis factor receptor-associated factor 6; NFATc1: Transcription factor nuclear factor of activated T cells; OPG: Osteoprotegerin; OSM: Oncostatin-M; OSMR: Oncostatin-M receptor; RUNX2: Runt-related transcription factor 2; OCN: Osteocalcin; Osx: Osterix; OPN: Osteopontin; ALPL: Alkaline phosphatase; BMP-2: Bone morphogenetic protein-2; TNF: Tumor necrosis factor; IL: Interleukin; IFN: Interferon; TGF-β: Transforming growth factor beta; IGF-1: Insulin-like growth factor-1.
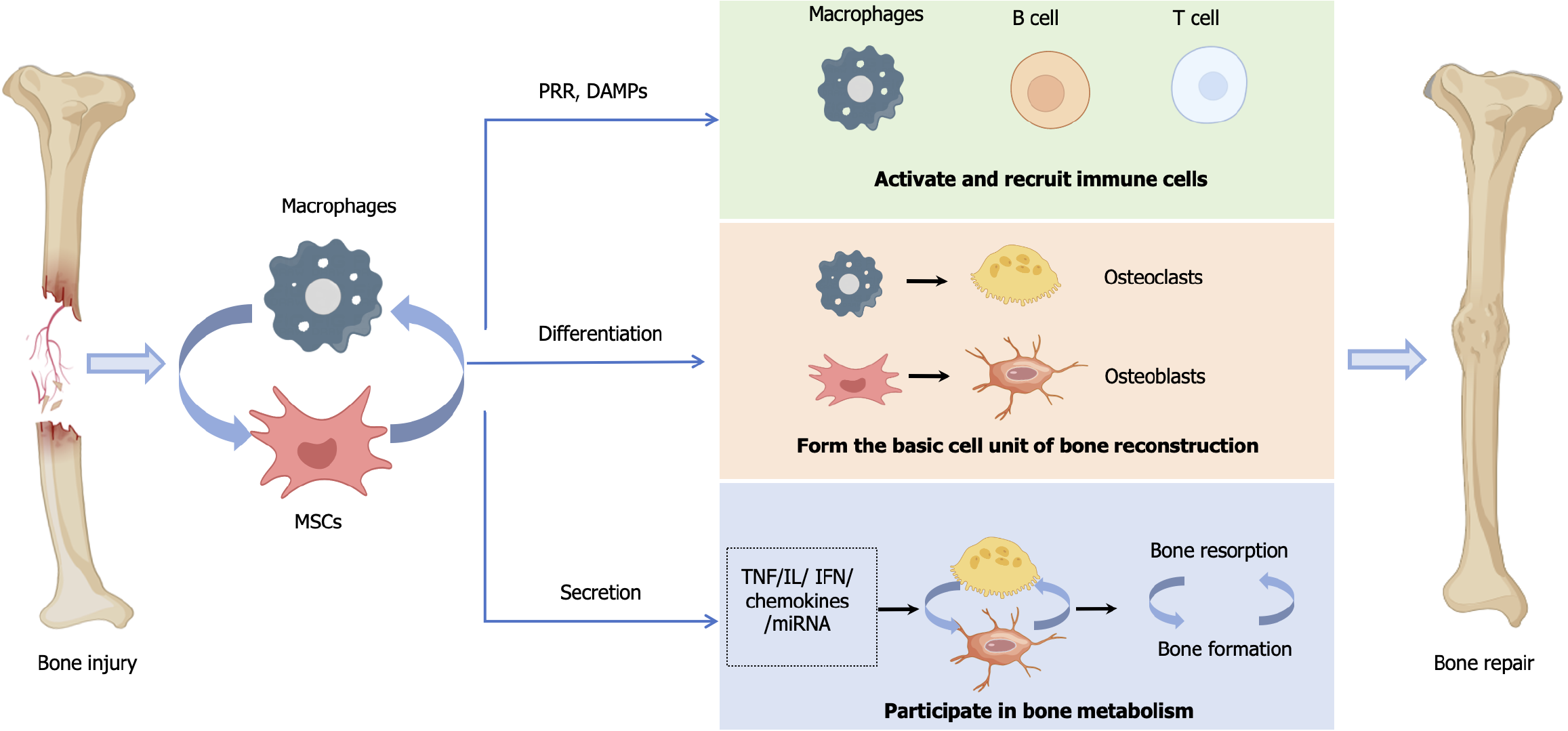
Figure 3 Mesenchymal stem cells and macrophages promote bone tissue repair.
The inflammatory microenvironment after injury promotes the activation of mesenchymal stem cells (MSCs) and macrophages. Through immune response patterns such as pattern recognition receptors and damage associated molecular patterns, the interaction between MSCs and macrophages further activates immune cells such as B cells and T cells, enhancing the immune response in the damaged microenvironment. MSCs and macrophages are precursor cells for osteoblasts (OBs) and osteoclasts (OCs), respectively, and play an important role in bone tissue reconstruction. At the same time, MSCs and macrophages also affect the formation of OBs and OCs by secreting chemokines, tumor necrosis factor, interferon, interferon and other bioactive factors, regulating the balance between bone resorption and bone formation, and promoting the repair of bone tissue. MSC: Mesenchymal stem cell; PRR: Pattern recognition receptor; DAMPs: Damage associated molecular patterns; TNF: Tumor necrosis factor; IL: Interleukin; IFN: Interferon; miRNA: MicroRNA.
- Citation: Zhang FF, Hao Y, Zhang KX, Yang JJ, Zhao ZQ, Liu HJ, Li JT. Interplay between mesenchymal stem cells and macrophages: Promoting bone tissue repair. World J Stem Cells 2024; 16(4): 375-388
- URL: https://www.wjgnet.com/1948-0210/full/v16/i4/375.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v16.i4.375