Copyright
©The Author(s) 2019.
World J Stem Cells. Sep 26, 2019; 11(9): 604-617
Published online Sep 26, 2019. doi: 10.4252/wjsc.v11.i9.604
Published online Sep 26, 2019. doi: 10.4252/wjsc.v11.i9.604
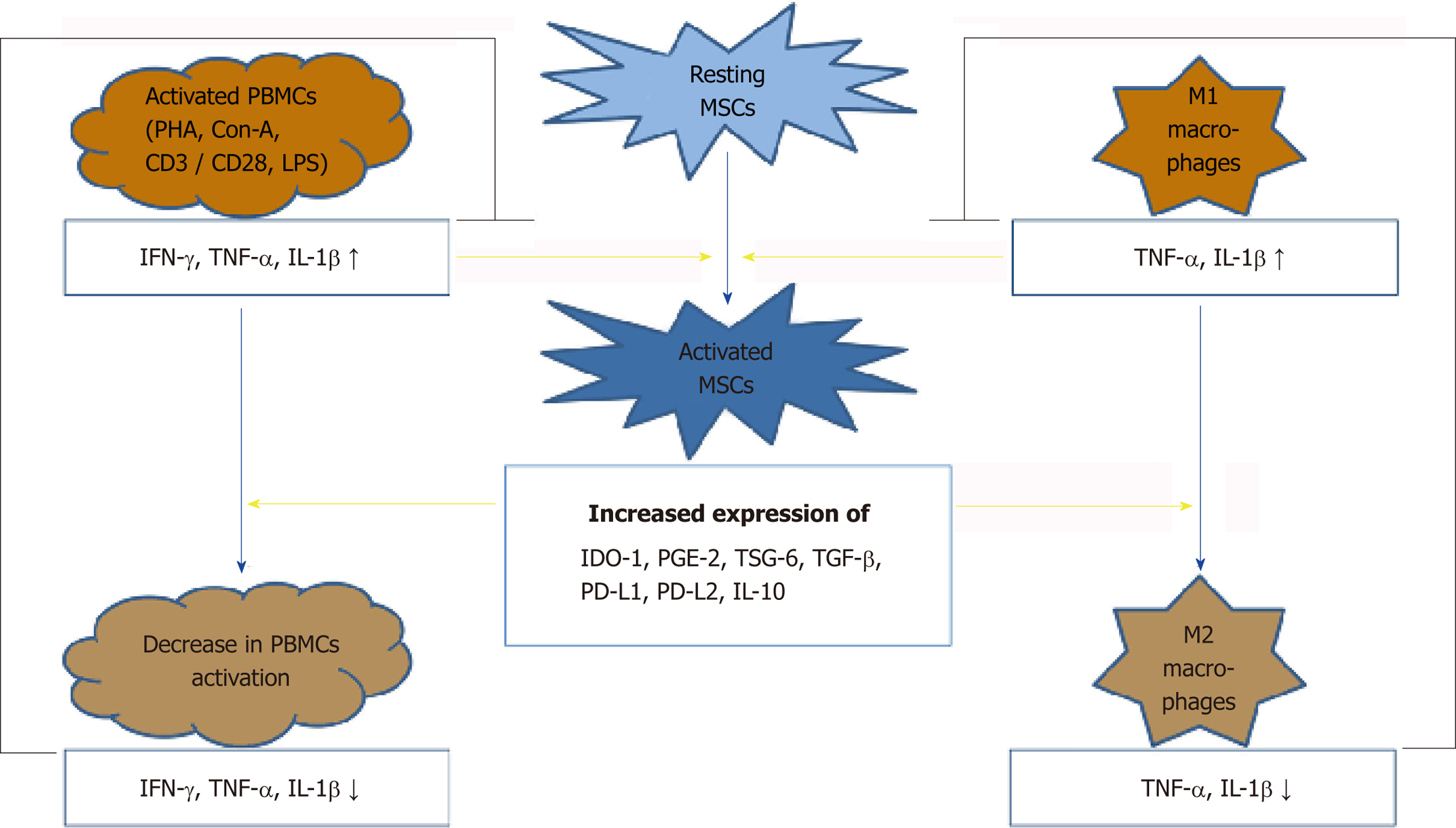
Figure 1 Reciprocal interaction between dental tissue-derived mesenchymal stem cells and immune cells.
While the immunomodulatory ability of resting mesenchymal stem cells (MSCs) is usually low, inflammatory cytokines such as interferon-γ, tumour necrosis factor-α, and interleukin-1β lead to strong activation of this ability. Large amounts of these cytokines are produced by immune cells, such as peripheral blood mononuclear cells (PBMCs) or macrophages, under inflammatory conditions. In vitro cytokine production can be activated by either mitotic stimuli or bacterial pathogens. Inflammatory cytokines increase the expression of different immunomodulatory proteins in MSCs, which leads to the suppression of the activity of PBMCs or directs macrophage polarization towards the M2 phenotype via paracrine mechanisms or direct cell-to-cell contact. The resulting lower levels of the inflammatory cytokines produced by PBMCs or macrophages diminish the ability of these cells to activate MSC-dependent immunosuppression. Thus, the continuous interaction between immune cells and dental tissue-derived MSCs determines the intensity of the immune response and hypothetically plays an important role in tissue homeostasis.
- Citation: Andrukhov O, Behm C, Blufstein A, Rausch-Fan X. Immunomodulatory properties of dental tissue-derived mesenchymal stem cells: Implication in disease and tissue regeneration. World J Stem Cells 2019; 11(9): 604-617
- URL: https://www.wjgnet.com/1948-0210/full/v11/i9/604.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v11.i9.604