修回日期: 2025-02-11
接受日期: 2025-02-20
在线出版日期: 2025-02-28
三期增强计算机断层扫描(computed tomography, CT)是肝占位病变诊断常用检查方法, 微小RNA是能调控细胞增殖、凋亡的重要生物标志物. 伴脂肪肝的肝占位病变病情复杂, 因此探究三期增强CT定量参数与血清微小RNA-122、微小RNA-224联合应用对伴脂肪肝的肝占位病变的诊断价值.
探究CT增强扫描联合血清miRNA-122(miR-122)、miRNA-224(miR-224)对伴脂肪肝的肝占位病变性质诊断效能, 为临床诊疗提供参考.
前瞻性选取2021-06/2024-06淳安县中医院收治的80例伴脂肪肝的肝占位病变患者为研究对象, 经手术或肝穿刺活检病理结果作为"金标准", 确诊伴脂肪肝的肝占位病变良恶性. 病理检查前均行CT增强扫描, 并测定血清miR-122、miR-224水平. 比较不同性质伴脂肪肝的肝占位病变的三期增强CT值、增强指数及血清miR-122、miR-224水平, 分析三期增强CT联合血清miR-122、miR-224诊断伴脂肪肝的肝占位恶性病变的效能.
80例伴脂肪肝的肝占位病变患者中良性病变46例, 恶性病变34例. 恶性病变CT增强扫描有包膜、强化方式快进快出占比均高于良性病变, 密度均匀、有中央瘢痕占比均低于良性病变(P<0.05); 恶性病变动脉期、门静脉期、延迟期的CT值、增强指数均低于良性病变(P<0.05); 伴脂肪肝的恶性病变血清miR-122水平低于良性病变, miR-224水平高于良性病变(P<0.05); 绘制增强CT定量参数、血清miR-122、miR-224联合诊断伴脂肪肝的肝占位恶性病变的受试者工作特征曲线, 结果显示增强CT定量参数、miR-122、miR-224联合的曲线下面积最大, 为0.946(95%CI: 0.972-0.984)(P<0.05).
伴脂肪肝的良性、恶性肝占位病变患者增强CT定量参数存在显著差异, 增强CT参数联合血清miR-122、miR-224对于伴脂肪肝的肝占位恶性病变有较高诊断效能.
核心提要: 伴脂肪肝的肝占位病变诊断中易受到其他因素干扰, 影像学联合血清学在占位性病变临床诊断中有一定优势. 文中提出三期增强计算机断层扫描联合血清微小RNA-122、微小RNA-224用于伴脂肪肝的肝占位病变性质诊断中, 取得了良好诊断效能, 建议临床推广.
引文著录: 章艳飞, 刘文华. 三期增强CT定量参数联合血清miR-122、miR-224对伴脂肪肝的肝占位病变性质诊断效能研究. 世界华人消化杂志 2025; 33(2): 131-139
Revised: February 11, 2025
Accepted: February 20, 2025
Published online: February 28, 2025
Three-phase contrast-enhanced computed tomography (CT) is a commonly used diagnostic method for liver space-occupying lesions, and microRNA is an important biomarker that can regulate cell proliferation and apoptosis. The condition of liver space-occupying lesions with fatty liver is complex, so we explored the diagnostic value of combining quantitative parameters of three-phase contrast-enhanced CT with serum microRNA-122 and microRNA-224 for liver space-occupying lesions with fatty liver.
To explore the efficacy of contrast-enhanced CT scanning combined with serum miRNA-122 (miR-122) and miRNA-224 (miR-224) in the diagnosis of liver space-occupying lesions with fatty liver, to provide a reference for their clinical diagnosis and treatment.
A prospective study was conducted on 80 patients with liver space-occupying lesions accompanied by fatty liver who were admitted to the Chun'an County Traditional Chinese Medicine Hospital from June 2021 to June 2024. The surgical or liver biopsy pathology results were used as the "gold standard" to determine the benign or malignant nature of the liver space-occupying lesions accompanied by fatty liver. Before pathological examination, all patients underwent contrast-enhanced CT scanning and the levels of serum miR-122 and miR-224 were measured. The CT values, enhancement indexes, and serum levels of miR-122 and miR-224 were compared in patients with different types of liver space-occupying lesions accompanied by fatty liver, and the efficacy of three-phase contrast-enhanced CT combined with serum levels of miR-122 and miR-224 in diagnosing malignant liver space-occupying lesions accompanied by fatty liver was evaluated.
Among the 80 patients with liver space-occupying lesions accompanied by fatty liver, 46 had benign lesions and 34 had malignant lesions. On contrast-enhanced CT, malignant lesions exhibited a higher probability of presence of capsules and fast-in and fast-out pattern compared to benign lesions. Additionally, the probability of uniform density and central scarring was lower in malignant lesions than in benign lesions (P < 0.05). The CT values and enhancement indexes of malignant lesions in the arterial phase, portal venous phase, and delayed phase were lower than those of benign lesions (P < 0.05). The serum level of miR-122 in malignant lesions with fatty liver was lower than that in benign lesions, while the level of miR-224 was higher than that in benign lesions (P < 0.05). The receiver operating characteristic curves of enhanced CT quantitative parameters, serum miR-122, and miR-224, alone or in combination, for the diagnosis of malignant lesions with fatty liver were drawn. The results showed that the area under curve of the combination of enhanced CT quantitative parameters, miR-122, and miR-224 was the largest at 0.946 (95% confidence interval: 0.972-0.984) (P < 0.05).
There are significant differences in quantitative parameters of contrast-enhanced CT between patients with benign and malignant liver space-occupying lesions with fatty liver. The combination of enhanced CT parameters and serum miR-122 and miR-224 has high diagnostic efficiency for malignant liver space-occupying lesions with fatty liver.
- Citation: Zhang YF, Liu WH. Efficacy of quantitative parameters of three-phase contrast-enhanced computed tomography combined with serum miR-122 and miR-224 in diagnosis of liver space-occupying lesions with fatty liver. Shijie Huaren Xiaohua Zazhi 2025; 33(2): 131-139
- URL: https://www.wjgnet.com/1009-3079/full/v33/i2/131.htm
- DOI: https://dx.doi.org/10.11569/wcjd.v33.i2.131
脂肪肝是肝脏常见的弥漫性病变. 肝占位病变为各种因素引起的增生结节、肝脏肿瘤等多种病变[1,2]. 计算机断层扫描(computed tomography, CT)增强扫描是肝脏疾病诊断常用影像学方式, 在肝占位病变性质诊断中具有重要作用[3]. 但伴脂肪肝的肝占位病变诊断中易受到肥胖、气体、声窗等因素干扰, 使诊断特异性下降而导致漏诊; 且此类患者病情复杂, 易出现误诊, 增加伴脂肪肝的肝占位病变性质的诊断难度[4,5]. 现阶段肝癌筛查常采用甲胎蛋白等生物标志物, 是进展期肝癌的有效诊断标志物, 但其在早期阶段敏感性、特异性欠佳, 检测小肿瘤(<3 cm)易漏诊. 微小RNA(microRNA, miRNA)可参与调控细胞增殖、凋亡及生物体发育等的生理病理过程, 已被临床作为肝癌等实体瘤诊断有潜力的生物标志物[6,7]. 研究表明[8], miRNA-122(microRNA-122, miR-122)、miRNA-224(microRNA-224, miR-224)在肝癌的发病机制中显著异常. 为进一步探究伴脂肪肝的肝占位恶性病变诊断方式, 本研究尝试联合应用三期增强CT、血清miR-122、miR-224, 为临床诊断提供新思路. 现报道如下.
本研究前瞻性选取2021-06/2024-06淳安县中医院收治的80例伴脂肪肝的肝占位病变患者为研究对象, 其中男53例, 女27例, 年龄46-67岁, 平均(56.43±4.37)岁; 体质量指数(23-28) kg/m2, 平均(25.17±1.03) kg/m2; 基础疾病: 高血压18例, 糖尿病24例; 脂肪肝程度: 轻度42例, 中度38例. 病灶位置: 28例(35.00%)右前叶, 24例(30.00%)右后叶, 8例(10.00%)左内叶, 15例(18.75%)左外叶, 5例(6.25%)尾状叶; 病灶直径(0.80-3.90) cm, 平均(2.35±0.77) cm.
纳入标准: (1)肝占位病变经手术或肝穿刺活检病理诊断确诊; (2)合并脂肪肝[9]; (3)年龄>18岁; (4)未接受放、化疗和靶向治疗; (5)接受CT增强扫描, 图像质量良好; (6)征得患者和家属签字同意. 排除标准: (1)对CT增强扫描对比剂过敏; (2)伴有心、肺、肾等其他脏器功能严重障碍; (3)存在其他良恶性肿瘤疾病; (4)妊娠或哺乳期女性; (5)凝血功能异常; (6)语言障碍; (7)精神异常.
1.2.1 CT增强扫描: 采用64层螺旋CT扫描仪(菲利普16排, 型号Ingenuity Flex), 行仰卧位扫描, 自膈顶扫描至肾脏下缘; 增强扫描时以(3-4) mL/s速率经肘静脉注射对比剂碘海醇(300 mg/mL), 剂量1.5 mL/kg, 延迟6 s开始动脉期扫描, 动脉期后延迟30 s行门静脉期扫描, 注射对比剂后120 s行延迟期扫描. 将图像导入后处理工作站, 观察病灶包膜、供血动脉征、密度、中央瘢痕及强化方式. 于动脉期在病灶最大层面勾画感兴趣区(ROI)(约40 mm2), 并勾画与病灶同层面腹主动脉的ROI(约25 mm2-45 mm2). 计算各期平均CT值、增强指数, 增强指数 = 病灶CT值/腹主动脉CT值. 由2位高年资腹部影像诊断医师进行双盲法独立阅片, 若意见不统一, 经与第3位高年资腹部影像诊断医师讨论达成共识.
1.2.2 miR-122、miR-224检测: 入组后采集3 mL外周静脉血, 离心取血清, 提取总RNA(美国Invitrogen公司TRIzol试剂盒), 进行反转录(日本TaKaRa公司反转录试剂盒)合成cDNA; 以cDNA作为模板, U6引物作为内参, 采用实时荧光定量PCR仪(美国ABI公司)检测miR-122、miR-224相对表达, 以2-△△Ct法表示.
统计伴脂肪肝的肝占位病变性质病理结果及不同性质病变患者临床资料; 比较不同性质伴脂肪肝的肝占位性病变CT增强扫描特征、图像表现; 比较不同性质伴脂肪肝的肝占位病变的三期增强CT值、增强指数及血清miR-122、miR-224; 分析增强CT定量参数、血清miR-122、miR-224单独及联合诊断伴脂肪肝的肝占位恶性病变的效能.
统计学处理 采用SPSS 27.0对数据进行分析, 计量资料以(mean±SD)表示, 差异行t检验, 计数资料以n(%)表示, 差异行χ2检验, 采用受试者工作特征(receiver operating characteristic, ROC)曲线分析三期增强CT联合血清miR-122、miR-224对伴脂肪肝的肝占位病变性质的诊断效能, 获取曲线下面积(area under the curve, AUC)值、置信区间(95%CI)、截断值、敏感度及特异度, 以AUC评价诊断效果, AUC<0.5表示无诊断价值, 0.5-<0.7表示诊断准确性较低, 0.7-0.9表示有一定诊断价值, >0.9表示准确性较高. 检验水准: α = 0.05.
80例伴脂肪肝的肝占位病变患者中良性病变46例, 其中19例(23.75%)局灶性结节增生, 18例(22.50%)肝囊肿, 9例(11.25%)肝腺瘤; 恶性病变34例, 其中25例(32.25%)肝细胞癌, 9例(11.25%)胆管细胞癌.
不同病变患者性别、年龄、体质量指数、脂肪肝程度、基础疾病、病灶位置、病灶直径比较差异均无统计学意义, 见表1.
| 指标 | 恶性病变(34例) | 良性病变(46例) | χ2/t | P值 |
| 性别(男/女) | 24(70.59)/10(29.41) | 29(63.04)/17(36.96) | 0.498 | 0.481 |
| 年龄(岁) | 57.24±4.12 | 55.83±3.87 | 1.567 | 0.121 |
| 体质量指数(kg/m2) | 24.96±0.91 | 25.33±0.95 | 1.753 | 0.084 |
| 高血压 | 8(23.53) | 10(21.74) | 0.036 | 0.850 |
| 糖尿病 | 13(38.24) | 11(23.91) | 1.910 | 0.167 |
| 脂肪肝程度 | ||||
| 轻度 | 16(47.06) | 26(56.52) | 0.702 | 0.402 |
| 中度 | 18(52.94) | 20(43.48) | ||
| 病灶位置 | ||||
| 右前叶 | 13(38.24) | 15(32.61) | 1.306 | 0.086 |
| 右后叶 | 10(29.41) | 14(30.43) | ||
| 左外叶 | 7(20.59) | 8(17.39) | ||
| 左内叶 | 2(5.88) | 6(13.04) | ||
| 尾状叶 | 2(5.88) | 3(6.52) | ||
| 病灶直径(cm) | 2.31±0.72 | 2.38±0.75 | 0.420 | 0.676 |
不同性质伴脂肪肝的肝占位性病变供血动脉征比较差异无统计学意义, 恶性病变CT增强扫描有包膜、强化方式快进快出占比均高于良性病变, 密度均匀、有中央瘢痕占比均低于良性病变(P<0.05), 见表2.
| 指标 | 恶性病变(34例) | 良性病变(46例) | χ2 | P值 |
| 包膜 | ||||
| 有 | 14(41.18) | 8(17.39) | 5.547 | 0.019 |
| 无 | 20(58.82) | 38(82.61) | ||
| 供血动脉征 | ||||
| 有 | 15(44.12) | 30(65.22) | 3.537 | 0.060 |
| 无 | 19(55.88) | 16(34.78) | ||
| 密度 | ||||
| 均匀 | 7(20.59) | 44(95.65) | 47.667 | <0.001 |
| 不均匀 | 27(79.41) | 2(4.35) | ||
| 中央瘢痕 | ||||
| 有 | 3(8.82) | 25(54.35) | 17.810 | <0.001 |
| 无 | 31(91.18) | 21(45.65) | ||
| 强化方式 | ||||
| 缓升缓降 | 1(2.94) | 5(10.87) | 36.200 | <0.001 |
| 速升平台 | 13(38.24) | 41(89.13) | ||
| 快进快出 | 20(58.82) | 0(0.00) |
良性病变: (1)肝囊肿: 为边缘光滑的类圆形影, 呈低密度, 增强扫描动脉期呈点状强化; (2)局灶性结节增生: 17例CT平扫呈低密度, 增强扫描中实质区域明显强化; 2例存在环形强化, 门静脉、延迟期密度较低; (3)肝腺瘤: 多为类圆形肿块, 密度混杂, 其中5例存在脂肪变性, 动脉期均匀强化; 3例可见包膜影.
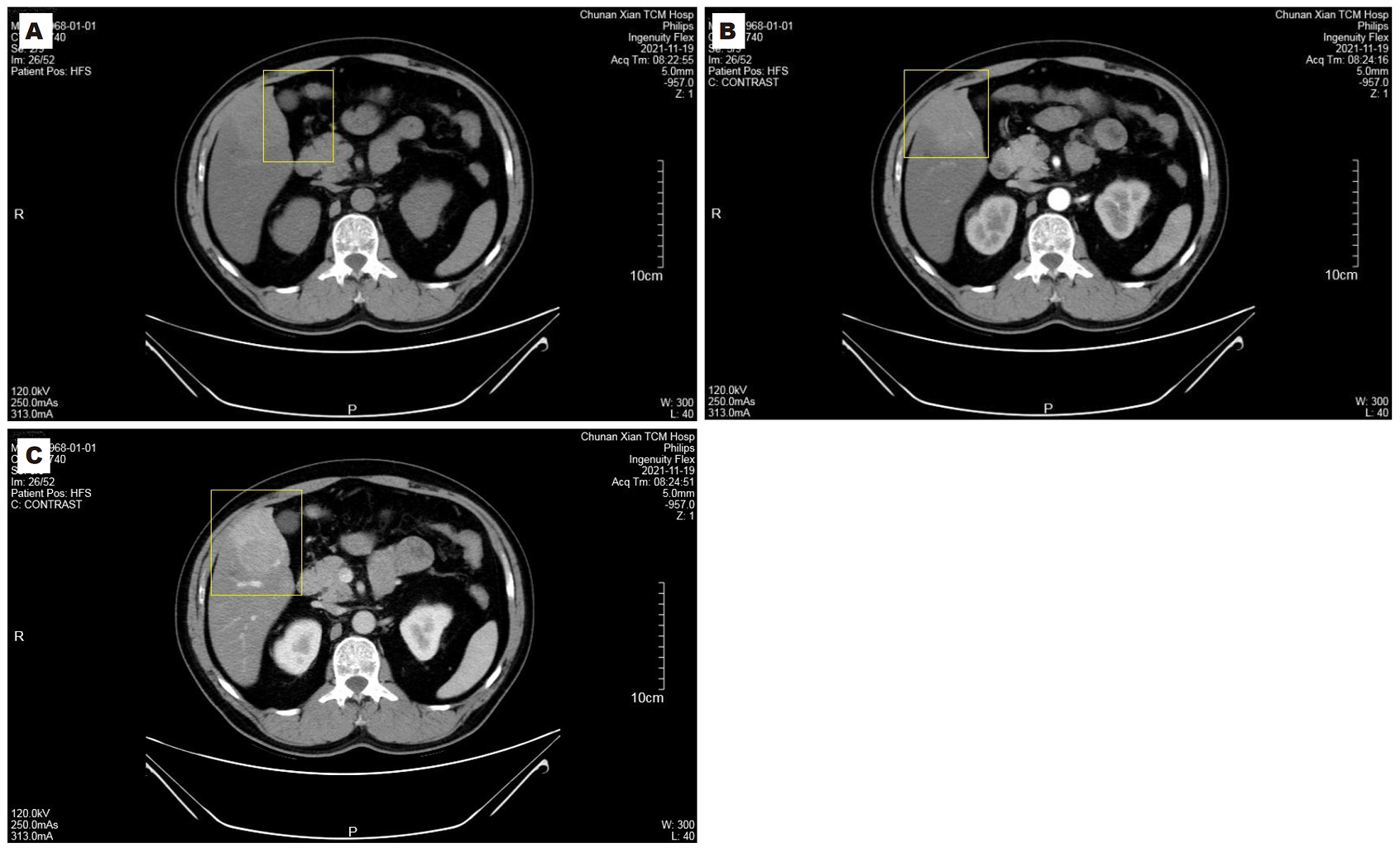
恶性病变: (1)肝细胞癌: 病灶内存在囊变或坏死, 多为低或等密度影, 动脉期明显增强, 门静脉期轻、中度强化, 呈"快进快出"模式; (2)胆管细胞癌: 边界不清且不规则, 呈低密度影, 胆管存在扩张, 动脉期边缘明显强化, 门静脉期不规则强化, 管腔变窄. 见图1.
恶性病变动脉期、门静脉期、延迟期的CT值、增强指数均低于良性病变(P<0.05), 见表3.
| 病变性质 | n | CT值 | 增强指数 | ||||
| 动脉期 | 门静脉期 | 延迟期 | 动脉期 | 门静脉期 | 延迟期 | ||
| 恶性病变 | 34 | 93.75±23.58 | 99.72±18.14 | 83.62±14.41 | 0.35±0.11 | 0.69±0.14 | 0.75±0.12 |
| 良性病变 | 46 | 136.23±28.65 | 125.37±24.41 | 98.82±18.05 | 0.51±0.90 | 0.87±0.12 | 0.85±0.13 |
| t | 7.055 | 5.161 | 4.047 | 9.433 | 6.177 | 3.513 | |
| P值 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
伴脂肪肝的恶性病变血清miR-122水平低于良性病变, miR-224水平高于良性病变(P<0.05), 见表4.
| 病变性质 | n | miR-122 | miR-224 |
| 恶性病变 | 34 | 39.11±4.18 | 72.18±9.42 |
| 良性病变 | 46 | 73.62±7.27 | 40.27±3.35 |
| t | 24.791 | 21.266 | |
| P值 | <0.001 | <0.001 |
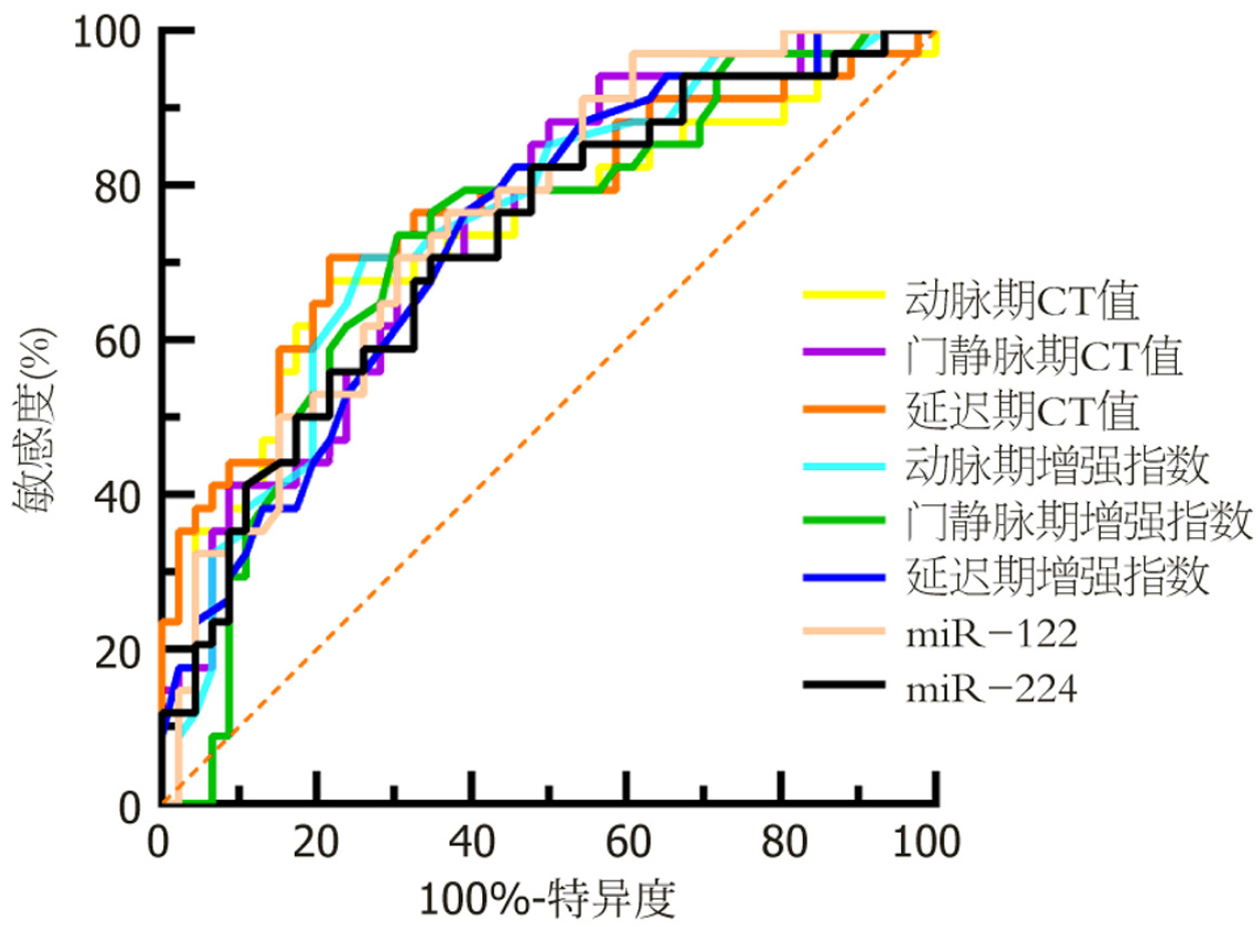
以伴脂肪肝的肝占位恶性病变患者、良性病变患者分别为阳性样本、阴性样本, 绘制增强CT定量参数、血清miR-122、miR-224单独诊断伴脂肪肝的肝占位恶性病变的ROC曲线. 见表5、图2.
| 指标 | AUC | 95%CI | 截断值 | 敏感度(%) | 特异度(%) | P值 |
| 动脉期CT值 | 0.760 | 0.651-0.848 | 106.22 | 70.59 | 73.91 | <0.001 |
| 门静脉期CT值 | 0.751 | 0.642-0.841 | 111.25 | 73.53 | 73.91 | <0.001 |
| 延迟期CT值 | 0.778 | 0.671-0.863 | 93.86 | 70.59 | 71.74 | <0.001 |
| 动脉期增强指数 | 0.779 | 0.672-0.864 | 0.43 | 70.59 | 73.91 | <0.001 |
| 门静脉期增强指数 | 0.754 | 0.645-0.844 | 0.78 | 79.41 | 65.22 | <0.001 |
| 延迟期增强指数 | 0.743 | 0.633-0.834 | 0.81 | 70.59 | 78.26 | <0.001 |
| miR-122 | 0.754 | 0.644-0.843 | 40.84 | 70.59 | 69.57 | <0.001 |
| miR-224 | 0.723 | 0.612-0.817 | 66.85 | 70.59 | 65.22 | <0.001 |
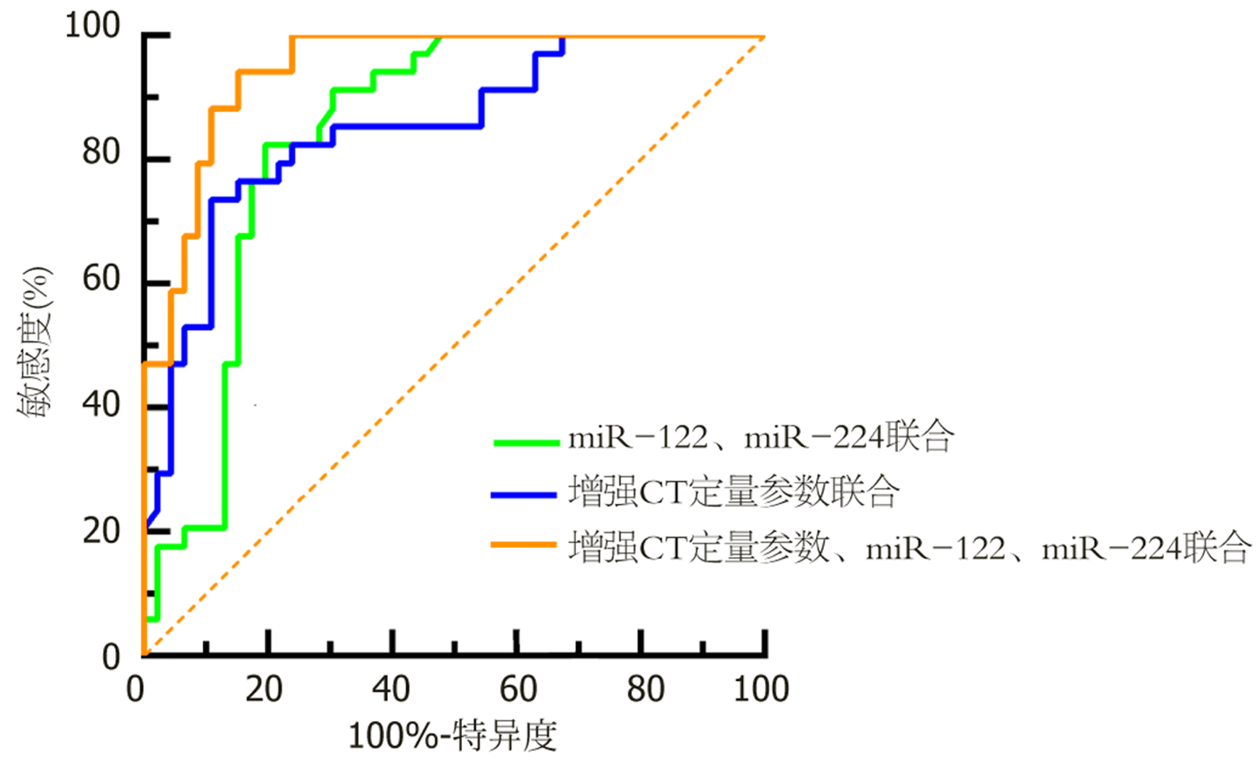
绘制增强CT定量参数、血清miR-122、miR-224联合诊断伴脂肪肝的肝占位恶性病变的ROC曲线, 结果显示增强CT定量参数、miR-122、miR-224联合的AUC最大, 为0.946(95%CI: 0.972-0.984)(P<0.05). 见表6、表7和图3.
| 指标 | AUC | 95%CI | 敏感度(%) | 特异度(%) | P值 |
| miR-122、miR-224联合 | 0.840 | 0.740-0.912 | 82.35 | 80.43 | <0.001 |
| 增强CT定量参数联合 | 0.849 | 0.751-0.919 | 73.53 | 89.13 | <0.001 |
| 增强CT定量参数、miR-122、miR-224联合 | 0.946 | 0.872-0.984 | 94.12 | 84.78 | <0.001 |
| 成对对比 | AUC差异 | 标准误差 | 95%CI | Z | P值 |
| 联合1 vs 联合3 | 0.107 | 0.054 | 0.001-0.212 | 1.987 | 0.047 |
| 联合2 vs 联合3 | 0.0975 | 0.049 | 0.002-0.193 | 2.010 | 0.045 |
影像征象是诊断肝脏占位性病变的基础, 本研究从包膜、密度、中央瘢痕、强化方式等方面进行分析, 显示伴脂肪肝的肝占位恶性病变CT增强扫描有包膜、强化方式快进快出占比均高于良性病变, 密度均匀、有中央瘢痕占比均低于良性病变. 包膜的存在高度提示肝细胞癌[10,11]. 本研究结果显示, 恶性病变多为"快进快出"式强化. 陈启全等[12]研究显示, 77.8%肝细胞癌病灶呈"快进快出"表现, 与本研究相似. 伴脂肪肝的肝占位恶性病变部分血供由门静脉转为肝动脉, 血管基底膜受损, 碘海醇快速进出血管, 强化呈现"快进快出"式. 伴脂肪肝的肝占位病变多存在脂肪变性, 肝细胞癌等富血供病变的病灶血供达不到其生长所需, 病灶内部分细胞坏死, 且可能伴有自发破裂出血, 造成密度不均匀[13,14]. 而良性病变密度较均匀, 钙化、出血等情况较少见[15,16]. 中央瘢痕是局灶性结节增生等良性肝脏占位性病变的典型征象[17,18]. 本研究显示良性病变患者中有54.35%存在中央瘢痕, 明显高于恶性病变患者. CT增强扫描强化方式是鉴别诊断肝占位病变性质的重要指标.
肝细胞癌等恶性病变多为富血供病变, 动脉期强化明显, 三期增强CT中的CT值、强化指数为强化程度判断提供了量化标准. 本研究显示, 恶性病变动脉期、门静脉期、延迟期的CT值、增强指数均低于良性病变, 可见三期增强CT定量参数对伴脂肪肝的肝占位病变良恶性有一定评估作用. 分析原因可能在于病理基础不同, 不同性质肝占位病变均存在肝动脉供血, 但由于良性病变肝实质细胞组织结构正常, 血管基底膜相对完整, 供血动脉管径相比于恶性病变较大[19,20]. 脂肪肝患者肝细胞内脂肪过多沉积, 多存在不同程度的脂肪浸润, 整个肝脏实质密度下降, 对于伴脂肪肝的肝占位病变, 影像学检查难以准确诊断微小病灶或隐性病灶.
miRNAs在肝癌组织和细胞中呈异常表达, 已有研究表明, miR-122、miR-224在早期肝细胞癌中有显著的诊断效能, 可能参与肝细胞癌变的病理过程[21-23]. 王海溥等[8]研究显示, miR-224高表达、miR-122低表达与肝细胞癌肿瘤直径、病理分期相关. 本研究结果发现, 伴脂肪肝的恶性病变血清miR-122水平低于良性病变, miR-224水平高于良性病变, 提示miR-122、miR-224在伴脂肪肝的管占位性病变中有一定鉴别作用. 马珊等[24]、An等[25]研究显示, miR-122可靶向作用于沉默信息调节因子1, 发挥负调控作用抑制肝癌细胞增殖、侵袭; miR-224可能通过白介素-6/转录信号转导子与激活子3/Smad同源物4通路调节肝细胞癌的侵袭、发展. 随着临床逐步阐明血清miR-224的生物学功能与疾病之间的关系, 有望在更多类型的肝占位病变中发挥诊疗价值. 本研究ROC曲线显示, 三期增强CT定量参数、miR-122、miR-224联合的AUC最大, 敏感度、特异度均较高, 可见此联合诊断方式针对伴脂肪肝的肝占位恶性病变诊断有较高临床价值.
综上所述, 伴脂肪肝的肝占位病变良、恶性的三期增强CT表现有显著差异, 三期增强CT与血清miR-122、miR-224联合对伴脂肪肝的肝占位恶性病变有较高诊断效能, 可为此类患者的针对性诊疗提供可靠依据.
三期增强计算机断层扫描(computed tomography, CT)是肝占位病变诊断常用检查方法, 微小RNA是能调控细胞增殖、凋亡的重要生物标志物. 伴脂肪肝的肝占位病变病情复杂, 因此探究三期增强CT定量参数与血清微小RNA-122、微小RNA-224联合应用对伴脂肪肝的肝占位病变的诊断价值. 微小RNA(miRNA)可参与调控细胞增殖、凋亡及生物体发育等的生理病理过程, 已被临床作为肝癌等实体瘤诊断有潜力的生物标志物[6,7]. 研究表明, miRNA-122(miR-122)、miRNA-224(miR-224)在肝癌的发病机制中显著异常[8]. 为进一步探究伴脂肪肝的肝占位恶性病变诊断方式, 本研究尝试联合应用三期增强CT、血清miR-122、miR-224, 为临床诊断提供新思路.
CT增强扫描是肝脏疾病诊断常用影像学方式, 在肝占位病变性质诊断中具有重要作用. 但伴脂肪肝的肝占位病变诊断中易受到肥胖、气体、声窗等因素干扰, 使诊断特异性下降而导致漏诊; 且此类患者病情复杂, 易出现误诊, 增加伴脂肪肝的肝占位病变性质的诊断难度.
为进一步探究伴脂肪肝的肝占位恶性病变诊断方式, 本研究尝试联合应用三期增强CT、血清miR-122、miR-224, 为临床诊断提供新思路.
前瞻性选取2021-06/2024-06淳安县中医院收治的80例伴脂肪肝的肝占位病变患者为研究对象, 经手术或肝穿刺活检病理结果作为"金标准", 确诊伴脂肪肝的肝占位病变良恶性. 病理检查前均行CT增强扫描, 并测定血清miR-122、miR-224水平. 比较不同性质伴脂肪肝的肝占位病变的三期增强CT值、增强指数及血清miR-122、miR-224水平, 分析三期增强CT联合血清miR-122、miR-224诊断伴脂肪肝的肝占位恶性病变的效能.
恶性病变CT增强扫描有包膜、强化方式快进快出占比均高于良性病变, 密度均匀、有中央瘢痕占比均低于良性病变(P<0.05); 恶性病变动脉期、门静脉期、延迟期的CT值、增强指数均低于良性病变(P<0.05); 伴脂肪肝的恶性病变血清miR-122水平低于良性病变, miR-224水平高于良性病变(P<0.05); 绘制增强CT定量参数、血清miR-122、miR-224联合诊断伴脂肪肝的肝占位恶性病变的ROC曲线, 结果显示增强CT定量参数、miR-122、miR-224联合的曲线下面积最大, 为0.946(95%CI: 0.972-0.984)(P<0.05).
伴脂肪肝的良性、恶性肝占位病变患者增强CT定量参数存在显著差异, 增强CT参数联合血清miR-122、miR-224对于伴脂肪肝的肝占位恶性病变有较高诊断效能.
伴脂肪肝的肝占位病变良、恶性的三期增强CT表现有显著差异, 三期增强CT与血清miR-122、miR-224联合对伴脂肪肝的肝占位恶性病变有较高诊断效能, 可为此类患者的针对性诊疗提供可靠依据.
学科分类: 胃肠病学和肝病学
手稿来源地: 浙江省
同行评议报告学术质量分类
A级 (优秀): 0
B级 (非常好): 0
C级 (良好): C, C, C
D级 (一般): 0
E级 (差): 0
科学编辑: 张砚梁 制作编辑:张砚梁
| 1. | Menon J, Shanmugam N, Madathil S, Vij M, Rammohan A, Rela M. Mature Cystic Teratoma of the Gall Bladder Masquerading a "Hepatic Space Occupying Lesion". J Pediatr Hematol Oncol. 2023;45:207-208. [PubMed] [DOI] |
| 2. | Vasireddy R, Bilalaga MM, Iding J, Sankineni A. Challenges in Diagnosis: Primary Hepatic Lymphoma Presenting as a Space-Occupying Liver Lesion. ACG Case Rep J. 2024;11:e01443. [PubMed] [DOI] |
| 3. | Tong AK, Tham WY, Too CW, Tai DW, Chow PK, Ng DC. Molecular Imaging and Therapy of Liver Tumors. Semin Nucl Med. 2020;50:419-433. [PubMed] [DOI] |
| 4. | Ota T, Hori M, Sasaki K, Onishi H, Nakamoto A, Tatsumi M, Fukui H, Ogawa K, Tomiyama N. Multimaterial decomposition algorithm for quantification of fat in hepatocellular carcinoma using rapid kilovoltage-switching dual-energy CT: A comparison with chemical-shift MR imaging. Medicine (Baltimore). 2021;100:e26109. [PubMed] [DOI] |
| 6. | Li Y, Li D, Yang Y, Wang J. miR-15a-5p Regulates Liver Cancer Cell Migration, Apoptosis and Cell Cycle Progression by Targeting Transcription Factor E2F3. Crit Rev Eukaryot Gene Expr. 2022;32:1-10. [PubMed] [DOI] |
| 7. | Feng Y, Jiang W, Zhao W, Lu Z, Gu Y, Dong Y. miR-124 regulates liver cancer stem cells expansion and sorafenib resistance. Exp Cell Res. 2020;394:112162. [PubMed] [DOI] |
| 11. | 易 建生, 梁 贻篇, 许 慧敏, 李 孔香, 江 求海, 吴 其叶, 徐 兆谋. 基于肝脏影像报告和数据系统的LR-5类与LR-TIV-肝细胞癌病变强化包膜的比较研究. 海南医学. 2022;33:1987-1990. [DOI] |
| 13. | Tan DJH, Ng CH, Lin SY, Pan XH, Tay P, Lim WH, Teng M, Syn N, Lim G, Yong JN, Quek J, Xiao J, Dan YY, Siddiqui MS, Sanyal AJ, Muthiah MD, Loomba R, Huang DQ. Clinical characteristics, surveillance, treatment allocation, and outcomes of non-alcoholic fatty liver disease-related hepatocellular carcinoma: a systematic review and meta-analysis. Lancet Oncol. 2022;23:521-530. [PubMed] [DOI] |
| 14. | Villena Salinas J, Montellano Fenoy AJ, Sanz Viedma S, Suárez Muñoz MÁ. Steatotic hepatocellular adenoma: an unusual cause of a hypermetabolic liver lesion. Rev Esp Enferm Dig. 2023;115:452-453. [PubMed] [DOI] |
| 15. | Wei Y, Yang M, Zhang M, Gao F, Zhang N, Hu F, Zhang X, Zhang S, Huang Z, Xu L, Zhang F, Liu M, Deng J, Cheng X, Xie T, Wang X, Liu N, Gong H, Zhu S, Song B, Liu M. Focal liver lesion diagnosis with deep learning and multistage CT imaging. Nat Commun. 2024;15:7040. [PubMed] [DOI] |
| 16. | Berbís MÁ, Godino FP, Rodríguez-Comas J, Nava E, García-Figueiras R, Baleato-González S, Luna A. Radiomics in CT and MR imaging of the liver and pancreas: tools with potential for clinical application. Abdom Radiol (NY). 2024;49:322-340. [PubMed] [DOI] |
| 18. | Rudolphi-Solero T, Triviño-Ibáñez EM, Medina-Benítez A, Fernández-Fernández J, Rivas-Navas DJ, Pérez-Alonso AJ, Gómez-Río M, Aroui-Luquin T, Rodríguez-Fernández A. Differential Diagnosis of Hepatic Mass with Central Scar: Focal Nodular Hyperplasia Mimicking Fibrolamellar Hepatocellular Carcinoma. Diagnostics (Basel). 2021;12:44. [PubMed] [DOI] |
| 19. | Wang DC, Jang HJ, Kim TK. Characterization of Indeterminate Liver Lesions on CT and MRI With Contrast-Enhanced Ultrasound: What Is the Evidence? AJR Am J Roentgenol. 2020;214:1295-1304. [PubMed] [DOI] |
| 20. | Matteini F, Cannella R, Garzelli L, Dioguardi Burgio M, Sartoris R, Brancatelli G, Vilgrain V, Ronot M, Vernuccio F. Benign and malignant focal liver lesions displaying rim arterial phase hyperenhancement on CT and MRI. Insights Imaging. 2024;15:178. [PubMed] [DOI] |
| 21. | Wu M, Deng X, Zhong Y, Hu L, Zhang X, Liang Y, Li X, Ye X. MafF Is Regulated via the circ-ITCH/miR-224-5p Axis and Acts as a Tumor Suppressor in Hepatocellular Carcinoma. Oncol Res. 2020;28:299-309. [PubMed] [DOI] |
| 22. | 张 黎然, 刘 媛, 王 珍子. GDF15、miR-122、AFP和PIVKA-Ⅱ联合评估在HBV感染肝硬化患者肝细胞癌发生风险中的预测价值. 临床和实验医学杂志. 2024;23:121-126. [DOI] |
| 23. | Yang L, Wei C, Li Y, He X, He M. miR-224 is an early-stage biomarker of hepatocellular carcinoma with miR-224 and miR-125b as prognostic biomarkers. Biomark Med. 2020;14:1485-1500. [PubMed] [DOI] |
| 25. | An F, Wu X, Zhang Y, Chen D, Lin Y, Wu F, Ding J, Xia M, Zhan Q. miR-224 Regulates the Aggressiveness of Hepatoma Cells Through the IL-6/STAT3/SMAD4 Pathway. Turk J Gastroenterol. 2021;32:532-542. [PubMed] [DOI] |