修回日期: 2007-03-01
接受日期: 2007-03-17
在线出版日期: 2007-06-18
目的: 探讨磁共振(MRI)水成像(MRH)对直肠癌术前诊断和分期的价值.
方法: 对临床确诊为直肠癌的患者34例进行MRI水成像检查, 检查前经直肠注入生理盐水300 mL左右, 先作盆腔常规轴位平扫, 再作磁共振直肠水成像扫描, 扫描完后再作轴位、矢状位和冠状位增强扫描.
结果: 34例直肠癌均能显示原发病灶, 三维成像病变部位肠腔内不规则充盈缺损32例, 19例病变远侧端呈"袖口征"及"截断征". 轴位30例表现为腔内软组织肿块, 26例表现为肠壁不规则增厚, 肠腔环形狭窄. MRI水成像检查对T1, T2, T3, T4期肿瘤的准确度分别为66.7%(2/3), 76.9%(10/13), 86.7%(13/15), 100%(3/3), 总准确性为82.4%(28/34); 判断淋巴结转移的敏感性、特异性和准确性分别为69.2%(18/26), 62.5%(5/8), 67.6%(23/34); 对邻近组织脏器浸润、远处转移判断的准确度分别为94.1%(32/34)、97.1%(33/34).
结论: MRI水成像加常规平扫加增强扫描对直肠癌的诊断和分期有较大价值, 可以较准确地判断肿瘤在肠壁的浸润深度及盆腔内淋巴结的转移.
引文著录: 涂小煌, 黎成金, 马明, 王烈, 宋京翔. 直肠癌术前磁共振水成像检查的意义. 世界华人消化杂志 2007; 15(17): 1928-1933
Revised: March 1, 2007
Accepted: March 17, 2007
Published online: June 18, 2007
AIM: To explore the value of rectal magnetic resonance hydrography (MRH) in rectal carcinoma.
METHODS: Thirty-four patients with rectal carcinoma were included in the study. All underwent plain scan, three-planar enhanced scan and hydrography.
RESULTS: All foci were correctly detected by rectal MRH, which showed that there were irregular intraluminal filling defects (n = 32), and that "cuff" or "sawn-off" signs were seen at the distal end of the tumor (n = 19). Main MRH findings were: intraluminal soft tissue mass (n = 30), irregular thickening of the rectal wall and partial or circumferential stenosis of the rectal lumen (n = 26). The accuracy of rectal MRH for T staging was 82.4% (28/34). The accuracy for T1, T2, T3, and T4 staging was 66.7% (2/3), 76.9% (10/13), 86.7% (13/15) and 100% (3/3), respectively. The sensitivity, specificity, and accuracy for lymph node metastases were 69.2% (18/26), 62.5% (5/8) and 67.6% (23/34), respectively. The accuracy for adjacent organ invasion and liver metastasis was 94.1% (32/34) and 97.1% (33/34), respectively.
CONCLUSION: The combination of MRI plain scan, three-planar enhanced scan and hydrography could accurately stage rectal carcinomas and determine the invasive depth of local lesions. This method has direct applicability for clinical treatment.
- Citation: Tu XH, Li CJ, Ma M, Wang L, Song JX. Value of rectal magnetic resonance hydrography for diagnosis and staging of rectal carcinoma. Shijie Huaren Xiaohua Zazhi 2007; 15(17): 1928-1933
- URL: https://www.wjgnet.com/1009-3079/full/v15/i17/1928.htm
- DOI: https://dx.doi.org/10.11569/wcjd.v15.i17.1928
直肠癌为消化道常见恶性肿瘤, 在我国发病率呈上升趋势, 准确的术前诊断并分期直接关系到治疗方案的制订、术式的选择和评估预后. 传统的诊断方法如指诊、内镜、钡灌肠等, 用于直肠癌分期的准确性较低, 随着近年影像学的发展, 开始较多地运用经直肠超声检查(TRUS)、CT、MRI等对其进行诊断, MRI检查不仅对直肠癌患者的预后有参考意义, 对术前分期方面也有重要价值, 但单一的MRI检查对肿瘤的侵犯及淋巴结转移的判断其敏感性较低[1-13]. 用水使直肠充盈后, 可提高肿瘤的诊断率[14]. 为了探讨磁共振水成像在直肠癌术前分期的意义, 我们对34例确诊为直肠癌的患者于术前行MRI水成像检查, 分析其表现并分期, 与术后病理分期进行对比, 结果报告如下.
本组共34例, 其中男21例, 女13例, 年龄27-72(平均54.6±12.8)岁, 均为病理诊断为直肠癌的患者, 术前未行放疗或化疗, 术前1 wk内行MRI水成像检查. 根据肛门指诊及内窥镜检查, 肿瘤距肛门口的距离小于3 cm的5例, 距肛门口3-6 cm的肿瘤16例, 距肛门口6-12 cm的肿瘤13例. 病理显示: 黏液腺癌11例, 低分化腺癌6例, 中分化腺癌9例, 高分化腺癌8例.
检查前禁食, 禁水, 清洁灌肠, 扫描前患者右侧卧于扫描床, 用双腔气囊导尿管经肛门插入, 先将所囊管注空气20 mL, 让气囊充气, 以防导尿管脱出; 再经导尿管注入生理盐水300 mL左右, 以患者能耐受为度, 扩张直肠; 注水结束后, 患者取仰卧位, 脚先进; 先作常规盆腔轴位平扫, 再作MRI直肠水成像扫描, T2WI采用FSE序列, T1WI采用SE序列, 水成像扫描参数: TR5000-9000 ms, TE352 ms, Nex: 1次, Etl: 48, TA 1800, FOV: 36×36, 距阵192×256, 层厚3 mm, 层间隔0 mm, 平扫完后作增强扫描, 增强扫描前经肘静脉推注顺磁性对比剂Gd-DTPA(钆-二乙烯三胺五乙酸)15 mL, 以带脂肪抑制T1WI序列行轴位、矢状位、冠状位扫描, 以清楚显示直肠壁, 平扫及增强扫描观察直肠周围组织浸润与淋巴结转移情况. 图像后处理: 对直肠水成像扫描的原始图像用最大信号强度投影法, 作任意方向重建, 获得直肠水成像的图像, 利用Navigator软件对扫描数据进行三维重建进行仿真内窥镜检查, 应用Fly-through Sequence软件沿直肠管腔中轴方向进行观察病变在肠腔内的形态及邻近肠段的腔内表面情况.
MRI诊断标准[1]: 直肠癌MRI诊断标准如下: 肠壁局限性或弥漫性增厚(>6 mm), 肠腔内偏心性软组织肿块, 平扫呈等T1、长T2信号, 增强扫描明显强化, 肠腔不规则狭窄; MR水成像肠腔内不规则充盈缺损, 病变远侧端呈"袖口征"或"截断征". MRI分期标准: MRI上T1期指肿瘤浸润至黏膜层, 不论黏膜是否受累, 但肌层完整; T2期指肿瘤破坏黏膜下层, 肌层部分中断, 但肌层的外缘和周围脂肪完整; T3期指肌层完全中断, 与周围脂肪界限不清; T4期指肿瘤侵犯周围脏器和盆壁结构. 鉴别T1、T2期的关键是看环形肌有无受累, 鉴别T2和T3期的关键是看直肠周围脂肪有无浸润. 病理分期采用国际TNM分期方法(表1).
| 分期 | 肿瘤侵犯范围 |
| Tis | 原位癌 |
| T1期 | 肿瘤侵犯黏膜下层 |
| T2期 | 肿瘤侵犯直肠壁的环形或纵型肌层 |
| T3期 | 肿瘤侵犯浆膜或纤维外直肠周围脂肪组织 |
| T4期 | 肿瘤直接侵犯周围组织器官 |
| N0期 | 无区域淋巴结转移 |
| N1期 | 直肠周围有1-3个淋巴结转移 |
| N2期 | 直肠周围有4个以上淋巴结转移 |
| M0期 | 无远处转移 |
| M1期 | 有远处转移 |
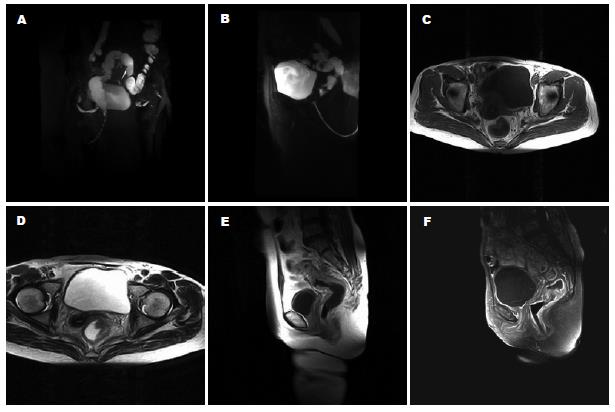
34例直肠癌均能显示原发病灶, 三维成像病变部位肠腔内不规则充盈缺损32例(图1A), 19例病变远侧端呈"袖口征"及"截断征"(图1B). 轴位像30例表现为腔内软组织肿块(图1C), 26例表现为肠壁不规则增厚, 肠腔环形狭窄(图1D). 平扫T1WI上呈等信号, 31例T2WI上呈略高信号, 3例呈明显高信号; 增强扫描病灶均明显强化. 7例平扫SE序列T1WI上病灶周围脂肪间隙内见斑片状低信号. 病变段肠壁外缘光滑20例(图1E), 不光滑或有结节影向外突出14例(图1F).
本组34例手术病理诊断T1, T2, T3, T4期肿瘤中, MRI检查的准确性分别为66.7%, 76.9%, 86.7%, 100%, 总准确性为82.4%. 低估4例, 高估2例(表2). 3例肝转移, 正确诊断2例(表3).
| MRI水成像 | 组织学 | 准确度[%(n/N)] | |||
| T1 | T2 | T3 | T4 | ||
| T1 | 2 | 1 | 66.7(2/3) | ||
| T2 | 1 | 10 | 2 | 76.9(10/13) | |
| T3 | 1 | 13 | 1 | 86.7(13/15) | |
| T4 | 3 | 100(3/3) | |||
| 总准确度 | 82.4(28/34) | ||||
| MRI | 组织学 | 敏感性[%(n/N)] | 特异性[%(n/N)] | 准确性[%(n/N)] | ||
| 阳性 | 阴性 | |||||
| 淋巴结 | ||||||
| 阳性 | 18 | 3 | 69.2(18/26) | 62.5(5/8) | 67.6(23/34) | |
| 阴性 | 8 | 5 | ||||
| 周围脂肪浸润 | ||||||
| 阳性 | 13 | 2 | 76.5(13/17) | 88.2(15/17) | 82.4(28/34) | |
| 阴性 | 4 | 15 | ||||
| 临近器官及骨盆浸润 | ||||||
| 阳性 | 3 | 0 | 60.0(3/5) | 100.0(29/29) | 94.1(32/34) | |
| 阴性 | 2 | 29 | ||||
| 远处转移 | ||||||
| 阳性 | 2 | 0 | 66.7(2/3) | 100.0(31/31) | 97.1(33/34) | |
| 阴性 | 1 | 31 | ||||
基因治疗等综合疗法是直肠癌治疗的方向[15-16], 手术切除是治疗直肠癌效果最明确的方法, 而手术方式的选择必须基于术前对肿瘤浸润深度与范围的准确判断. 直肠属空腔器官, 由于直肠解剖位置特殊, 被盆腔内脂肪固定, 蠕动较弱, 使之成为消化道MRI检查最成功的器官[17-18]. MR水成像是利用长TR加特长TE获得重T2WI的效果, 使含水器官显影[19], 我们体会, 采用人为的方法使肠腔充水, 增厚的肠壁或腔内肿块及周围结构发生信号的减弱, 含水的肠腔以明显的高信号显示出来, 再对其进行MIP重建, 肠腔的狭窄特征显示更清楚. 肠道灌水量主要取决于患者的承受能力, 本组平均灌水量300 mL, 34例原发病灶均能显影, 我们分析除检查前应作充分的肠道准备外, 与检查前已确诊, 病变较晚有关. T1WI轴位平扫采用SE序列, SE序列不进行脂肪抑制, 可以显示肠管周围脂肪, 有助于对T1, T2, T3, T4期肿瘤进行鉴别. Gd-DTPA增强扫描可以清楚显示病变段肠壁的外缘, 有助于判断肿瘤的浸润深度, 提高T分期的准确率[20-24].目前常用的对结直肠肿瘤术前分期的方法包括TRUS、CT及MRI, TRUS和MRI可显示肠壁的分层, MRI判断肠壁侵犯程度的能力和直肠内超声基本相当, 均优于盆腔CT. 直肠狭窄与上段直肠病变是直肠超声的主要局限因素, 对瘤边缘的炎性浸润与肿瘤侵犯难以区分, 肌层收缩导致肌层外缘形态改变也可误诊为肿瘤已突破肌层[25-33]. 本组T分期的总准确度为82.4%, 从T1到T4期分期的准确度呈上升趋势, 表明MRI水成像对中晚期直肠癌T分期更有价值. 本组对肠壁和直肠周围脂肪组织中大于0.5 cm的淋巴结设定为有转移, 但敏感性、特异性和准确性均较低, 分别为69.2%(18/26)、62.5%(5/8)、67.6%(23/34), 部分病例可见淋巴结, 但没有转移, 部分病例则未见淋巴结, 病理显示已有转移, 小于5 mm的淋巴结假阴性率高, 位于直肠上段病变的淋巴结转移常因超越病变水平而造成假阴性. MRI和CT、超声检查一样, 均无法对淋巴结有无转移作出准确判断, 对淋巴结转移的判断仅仅是通过大小、形态以及他和原发肿瘤的分离性来定性的, 因而常常不能发现淋巴结内部结构与微小转移, 或区别增大的炎性淋巴结与转移, 从而对淋巴结分期过高或过低[34-36].
钡灌肠和纤维内窥镜是检查直肠癌的主要方法, 但两者对肿瘤分期价值有限. 与钡灌肠相比较, MRI水成像可以解决钡灌肠梗阻近侧段及腔外情况不能显示的问题, MRI水成像由于具有多参数成像的特点及良好的软组织分辨率, 且扫描范围广, 因而并不存在空间限制的约束, 不仅能显示肠壁病灶、邻近器官的浸润及较大范围淋巴结转移外, 还能显示肝、骨等远处转移的种种优点, 本组邻近组织脏器浸润、远处转移判断的准确度分别为94.1%(32/34)、97.1%(33/34). MRI检查也克服了钡灌肠检查的不适和操作者依赖性, 以及CT检查的较大辐射量和碘过敏反应的不足, 随着检查技术的进展, 将成为对直肠癌术前诊断并分期的一种十分有效的手段[37-40].
直肠癌准确的术前诊断并分期直接关系到治疗方案的制订、术式的选择和评估预后. 为了提高磁共振成像在术前诊断和分期的准确率, 目前主要采用不同的对比剂、mAb体技术及高分辨磁共振技术等.
磁共振水成像是利用体内的液体-水作为天然对比剂, 在重度T2加权序列的MR图像上, 静态或缓慢流动的液体呈高信号, 而实质脏器或快速流动的血液呈低或无信号, 白色高信号的液体在黑色低信号背景的衬托下清晰显示, 因此称为MR水成像. 如:MR胰胆管造影(MRCP)、MR尿路造影(MRU)、MR脊髓造影(MRM)、肠梗阻MR水成像、MR输卵管成像等
本文以人为的方法使肠腔充水, 再采用磁共振水成像技术, 使含水的肠腔以明显的高信号显示出来, 肠腔的狭窄特征显示更清楚, 并与临床病理结果做对比分析, 对提高磁共振成像术前分期的准确率有指导意义, 有一定的学术价值和现实指导意义.
编辑: 张焕兰 电编:何基才
| 1. | Diagnostic accuracy of preoperative magnetic resonance imaging in predicting curative resection of rectal cancer: prospective observational study. BMJ. 2006;333:779. [PubMed] |
| 2. | Panzironi G, De Vargas Macciucca M, Manganaro L, Ballesio L, Ricci F, Casale A, Campagnano D. Preoperative locoregional staging of rectal carcinoma: comparison of MR, TRUS and Multislice CT. Personal experience. Radiol Med (Torino). 2004;107:344-355. [PubMed] |
| 3. | Brown G, Davies S, Williams GT, Bourne MW, Newcombe RG, Radcliffe AG, Blethyn J, Dallimore NS, Rees BI, Phillips CJ. Effectiveness of preoperative staging in rectal cancer: digital rectal examination, endoluminal ultrasound or magnetic resonance imaging? Br J Cancer. 2004;91:23-29. [PubMed] |
| 4. | Bianchi PP, Ceriani C, Rottoli M, Torzilli G, Pompili G, Malesci A, Ferraroni M, Montorsi M. Endoscopic ultrasonography and magnetic resonance in preoperative staging of rectal cancer: comparison with histologic findings. J Gastrointest Surg. 2005;9:1222-1227; discussion 1227-1228. [PubMed] |
| 5. | Bianchi P, Ceriani C, Palmisano A, Pompili G, Passoni GR, Rottoli M, Cappellani A, Montorsi M. A prospective comparison of endorectal ultrasound and pelvic magnetic resonance in the preoperative staging of rectal cancer. Ann Ital Chir. 2006;77:41-46. [PubMed] |
| 6. | Chun HK, Choi D, Kim MJ, Lee J, Yun SH, Kim SH, Lee SJ, Kim CK. Preoperative staging of rectal cancer: comparison of 3-T high-field MRI and endorectal sonography. AJR Am J Roentgenol. 2006;187:1557-1562. [PubMed] |
| 7. | Sinha R, Verma R, Rajesh A, Richards CJ. Diagnostic value of multidetector row CT in rectal cancer staging: comparison of multiplanar and axial images with histopathology. Clin Radiol. 2006;61:924-931. [PubMed] |
| 8. | Hoeffel C, Arrive L, Mourra N, Azizi L, Lewin M, Tubiana JM. Anatomic and pathologic findings at external phased-array pelvic MR imaging after surgery for anorectal disease. Radiographics. 2006;26:1391-1407. [PubMed] |
| 9. | Stollfuss JC, Becker K, Sendler A, Seidl S, Settles M, Auer F, Beer A, Rummeny EJ, Woertler K. Rectal carcinoma: high-spatial-resolution MR imaging and T2 quantification in rectal cancer specimens. Radiology. 2006;241:132-141. [PubMed] |
| 10. | Hama Y, Makita K, Yamana T, Dodanuki K. Mucinous adenocarcinoma arising from fistula in ano: MRI findings. AJR Am J Roentgenol. 2006;187:517-521. [PubMed] |
| 11. | Kuriu Y, Otsuji E, Kin S, Nakase Y, Fukuda K, Okamoto K, Hagiwara A, Yamagishi H. Monoclonal antibody conjugated to gadolinium as a contrast agent for magnetic resonance imaging of human rectal carcinoma. J Surg Oncol. 2006;94:144-148. [PubMed] |
| 12. | Salerno G, Daniels IR, Brown G. Magnetic resonance imaging of the low rectum: defining the radiological anatomy. Colorectal Dis. 2006;8 Suppl 3:10-13. [PubMed] |
| 13. | Skandarajah AR, Tjandra JJ. Preoperative loco-regional imaging in rectal cancer. ANZ J Surg. 2006;76:497-504. [PubMed] |
| 14. | Kim MJ, Lim JS, Oh YT, Kim JH, Chung JJ, Joo SH, Kim NK, Lee KY, Kim WH, Kim KW. Preoperative MRI of rectal cancer with and without rectal water filling: an intraindividual comparison. AJR Am J Roentgenol. 2004;182:1469-1476. [PubMed] |
| 15. | 黎 成金, 马 庆久, 赖 大年, 鲁 建国, 王 小军, 王 青, 潘 伯荣, 武 永忠, 李 金茂. CD/5-FC系统对结肠癌细胞的杀伤作用. 世界华人消化杂志. 2003;11:535-539. [DOI] |
| 17. | Slater A, Halligan S, Taylor SA, Marshall M. Distance between the rectal wall and mesorectal fascia measured by MRI: Effect of rectal distension and implications for preoperative prediction of a tumour-free circumferential resection margin. Clin Radiol. 2006;61:65-70. [PubMed] |
| 18. | Brown G, Kirkham A, Williams GT, Bourne M, Radcliffe AG, Sayman J, Newell R, Sinnatamby C, Heald RJ. High-resolution MRI of the anatomy important in total mesorectal excision of the rectum. AJR Am J Roentgenol. 2004;182:431-439. [PubMed] |
| 19. | Poon FW, McDonald A, Anderson JH, Duthie F, Rodger C, McCurrach G, McKee RF, Horgan PG, Foulis AK, Chong D. Accuracy of thin section magnetic resonance using phased-array pelvic coil in predicting the T-staging of rectal cancer. Eur J Radiol. 2005;53:256-262. [PubMed] |
| 20. | Brown G. Thin section MRI in multidisciplinary pre-operative decision making for patients with rectal cancer. Br J Radiol. 2005;78 Spec No 2:S117-127. [PubMed] |
| 21. | Kim CK, Kim SH, Chun HK, Lee WY, Yun SH, Song SY, Choi D, Lim HK, Kim MJ, Lee J. Preoperative staging of rectal cancer: accuracy of 3-Tesla magnetic resonance imaging. Eur Radiol. 2006;16:972-980. [PubMed] |
| 22. | Tatli S, Mortele KJ, Breen EL, Bleday R, Silverman SG. Local staging of rectal cancer using combined pelvic phased-array and endorectal coil MRI. J Magn Reson Imaging. 2006;23:534-540. [PubMed] |
| 23. | Iafrate F, Laghi A, Paolantonio P, Rengo M, Mercantini P, Ferri M, Ziparo V, Passariello R. Preoperative staging of rectal cancer with MR Imaging: correlation with surgical and histopathologic findings. Radiographics. 2006;26:701-714. [PubMed] |
| 24. | Burton S, Brown G, Daniels I, Norman A, Swift I, Abulafi M, Wotherspoon A, Tait D. MRI identified prognostic features of tumors in distal sigmoid, rectosigmoid, and upper rectum: treatment with radiotherapy and chemotherapy. Int J Radiat Oncol Biol Phys. 2006;65:445-451. [PubMed] |
| 25. | Koh DM, Brown G, Temple L, Raja A, Toomey P, Bett N, Norman AR, Husband JE. Rectal cancer: mesorectal lymph nodes at MR imaging with USPIO versus histopathologic findings--initial observations. Radiology. 2004;231:91-99. [PubMed] |
| 26. | Brown G, Radcliffe AG, Newcombe RG, Dallimore NS, Bourne MW, Williams GT. Preoperative assessment of prognostic factors in rectal cancer using high-resolution magnetic resonance imaging. Br J Surg. 2003;90:355-364. [PubMed] |
| 27. | Kim MJ, Park JS, Park SI, Kim NK, Kim JH, Moon HJ, Park YN, Kim WH. Accuracy in differentiation of mucinous and nonmucinous rectal carcinoma on MR imaging. J Comput Assist Tomogr. 2003;27:48-55. [PubMed] |
| 28. | Roach SC, Hulse PA, Moulding FJ, Wilson R, Carrington BM. Magnetic resonance imaging of anal cancer. Clin Radiol. 2005;60:1111-1119. [PubMed] |
| 29. | Lahaye MJ, Engelen SM, Nelemans PJ, Beets GL, van de Velde CJ, van Engelshoven JM, Beets-Tan RG. Imaging for predicting the risk factors--the circumferential resection margin and nodal disease--of local recurrence in rectal cancer: a meta-analysis. Semin Ultrasound CT MR. 2005;26:259-268. [PubMed] |
| 30. | Beets-Tan RG, Lettinga T, Beets GL. Pre-operative imaging of rectal cancer and its impact on surgical performance and treatment outcome. Eur J Surg Oncol. 2005;31:681-688. [PubMed] |
| 31. | Oberholzer K, Junginger T, Kreitner KF, Krummenauer F, Simiantonaki N, Trouet S, Thelen M. Local staging of rectal carcinoma and assessment of the circumferential resection margin with high-resolution MRI using an integrated parallel acquisition technique. J Magn Reson Imaging. 2005;22:101-108. [PubMed] |
| 32. | Ferri M, Laghi A, Mingazzini P, Iafrate F, Meli L, Ricci F, Passariello R, Ziparo V. Pre-operative assessment of extramural invasion and sphincteral involvement in rectal cancer by magnetic resonance imaging with phased-array coil. Colorectal Dis. 2005;7:387-393. [PubMed] |
| 33. | Taylor A, Sheridan M, McGee S, Halligan S. Preoperative staging of rectal cancer by MRI; results of a UK survey. Clin Radiol. 2005;60:579-586. [PubMed] |
| 34. | Koh DM, Brown G, Temple L, Blake H, Raja A, Toomey P, Bett N, Farhat S, Norman AR, Daniels I. Distribution of mesorectal lymph nodes in rectal cancer: in vivo MR imaging compared with histopathological examination. Initial observations. Eur Radiol. 2005;15:1650-1657. [PubMed] |
| 35. | Kim DW, Kim DY, Kim TH, Jung KH, Chang HJ, Sohn DK, Lim SB, Choi HS, Jeong SY, Park JG. Is T classification still correlated with lymph node status after preoperative chemoradiotherapy for rectal cancer? Cancer. 2006;106:1694-1700. [PubMed] |
| 36. | Matsuoka H, Nakamura A, Sugiyama M, Hachiya J, Atomi Y, Masaki T. MRI diagnosis of mesorectal lymph node metastasis in patients with rectal carcinoma. what is the optimal criterion? Anticancer Res. 2004;24:4097-4101. [PubMed] |
| 37. | Burton S, Brown G, Daniels IR, Norman AR, Mason B, Cunningham D. MRI directed multidisciplinary team preoperative treatment strategy: the way to eliminate positive circumferential margins? Br J Cancer. 2006;94:351-357. [PubMed] |
| 38. | Kim YH, Kim DY, Kim TH, Jung KH, Chang HJ, Jeong SY, Sohn DK, Choi HS, Ahn JB, Kim DH. Usefulness of magnetic resonance volumetric evaluation in predicting response to preoperative concurrent chemoradiotherapy in patients with resectable rectal cancer. Int J Radiat Oncol Biol Phys. 2005;62:761-768. [PubMed] |
| 39. | Oh YT, Kim MJ, Lim JS, Kim JH, Lee KY, Kim NK, Kim WH, Kim KW. Assessment of the prognostic factors for a local recurrence of rectal cancer: the utility of preoperative MR imaging. Korean J Radiol. 2005;6:8-16. [PubMed] |