修回日期: 2007-01-10
接受日期: 2007-02-08
在线出版日期: 2007-04-08
目的: 探讨螺旋CT多平面重建(MPR)对无典型临床表现阑尾炎的诊断价值.
方法: 搜集临床首次诊断未确诊为阑尾炎, 手术和病理证实为阑尾炎者19例, 回顾性分析比较螺旋CT轴扫和MPR两种方法的诊断符合率.
结果: 单纯采用螺旋CT轴扫法图像分析, 诊断符合率84.2%, 8例表现为阑尾增粗、壁增厚并有明显强化, 其中4例阑尾内见结石; 盲肠和(或)周围炎10例; 右下腹局限性脓肿5例, 其中2例伴有斑点状钙化. 误诊为回盲部及升结肠肿瘤2例, 盆腔炎1例, 误诊率15.8%. 采用螺旋CT MPR图像分析, 诊断符合率94.7%, 误诊为回盲部及升结肠肿瘤1例, 误诊率5.3%.
结论: 症状和体征不典型的阑尾炎临床诊断困难, 易误诊, 螺旋CT MPR方法简单, 可从不同角度观察病变部位及其周围情况, 有利于鉴别诊断, 提高诊断符合率, 具有较高的临床价值.
引文著录: 鲁际, 戴洪修, 谭光喜, 张安莹, 王洁兵, 肖治明. 螺旋CT多平面重建在急性阑尾炎诊断和鉴别诊断中的临床应用. 世界华人消化杂志 2007; 15(10): 1165-1170
Revised: January 10, 2007
Accepted: February 8, 2007
Published online: April 8, 2007
AIM: To investigate the value of spiral computed tomography (CT) multiple planar reconstruction (MPR) in the diagnosis of acute appendicitis with atypical clinical features.
METHODS: A total of 19 patients with acute appendicitis, who were not initially diagnosed according to clinical presentations, were confirmed surgically and pathologically, and CT manifestations were respectively analyzed. The diagnostic accordance rate was compared between CT axial scan and MPR.
RESULTS: The diagnostic accordance rate was 84.2% when CT axial scan was used alone. Eight cases (4 with stones) were found with increased diameters and walls of appendix, and 10 cases were found with appendicitis or peripheral inflammation. Localized abscess was observed in the right lower abdomen of 5 cases, of which 2 cases were found with calcified appendicitis. Two cases were misdiagnosed with the tumor of ascending colon, and another case with pelvic inflammation. The misdiagnosis rate was 15.8%. The diagnostic accordance rate was 94.7% when CT MPR was used alone. One case was misdiagnosed with the tumor of ascending colon, and the misdiagnosis rate was 5.3%.
CONCLUSION: It is rather difficult to diagnose acute appendicitis with atypical clinical features. Spiral CT MPR, operated simply, can be used to observe the lesion site and peripheral conditions from different angles, which benefits the differential diagnosis and improvement of accordance rates.
- Citation: Lu J, Dai HX, Tan GX, Zhang AY, Wang JB, Xiao ZM. Value of spiral computed tomography multiple planar reconstruction in the diagnosis and differential diagnosis of acute appendicitis with atypical clinical features. Shijie Huaren Xiaohua Zazhi 2007; 15(10): 1165-1170
- URL: https://www.wjgnet.com/1009-3079/full/v15/i10/1165.htm
- DOI: https://dx.doi.org/10.11569/wcjd.v15.i10.1165
目前CT轴位扫描诊断阑尾炎的已有较多报道[1-10], 但应用螺旋CT多平面重建诊断阑尾炎, 在国内尚未见文献报道, 本文比较CT轴位扫描与螺旋CT多平面重建两种方法对临床表现不典型阑尾炎的诊断效果, 着重探讨螺旋CT多平面重建对临床不典型阑尾炎的诊断价值.
收集了2003-05/2006-07经手术及病理证实的不典型急性阑尾炎病例19例, 其中, 男8例, 女11例, 年龄16-74(平均45)岁. 术前患者均有腹痛病史, 就诊时部分病例无发热及白细胞升高, 7例扪及右下腹部包块, 术前临床疑诊为腹腔肿瘤6例, 盆腔炎4例, 胰腺炎1例, 胆石症1例, 其他7例.
使用GE Lightspeed QX/I四层螺旋CT机. 扫描范围从脐部至耻骨联合, 扫描参数: 120 kV, 220 mA. 层厚5 mm, 层距5 mm, 进床速度为15 mm/s, 视野36 cm, 原始图像传至CT工作站(Advantage Windows 4.0), 进行MPR重建, CT图像用软组织窗进行观察, 以利于显示阑尾及其周围脂肪间隙. 窗位为-13~-40 Hu, 窗宽260-300 Hu. 12例作螺旋CT平扫, 不口服或结肠灌注造影剂. 4例作了增强扫描, 扫描前2-3 h口服碘水约500 mL以充盈回盲部. 增强时用高压注射器经肘静脉注入碘海醇注射液100 mL, 注射速率为2.2 mL/s.
我们回顾性阅读了19位患者的CT资料, 首先采用MPR的方法, 由两名有经验的诊断医师进行诊断, 计算出诊断符合率, 再和术前单纯采用CT轴扫方法的诊断符合率相比较, 分析这两种方法对病灶观察情况的优势和不足, 并将其与相关文献报道的诊断符合率相对比.
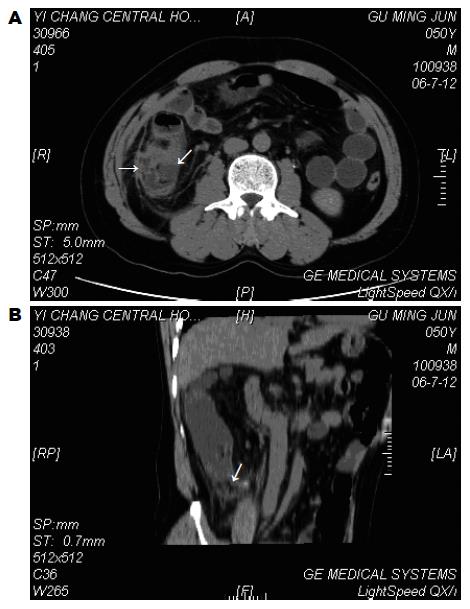
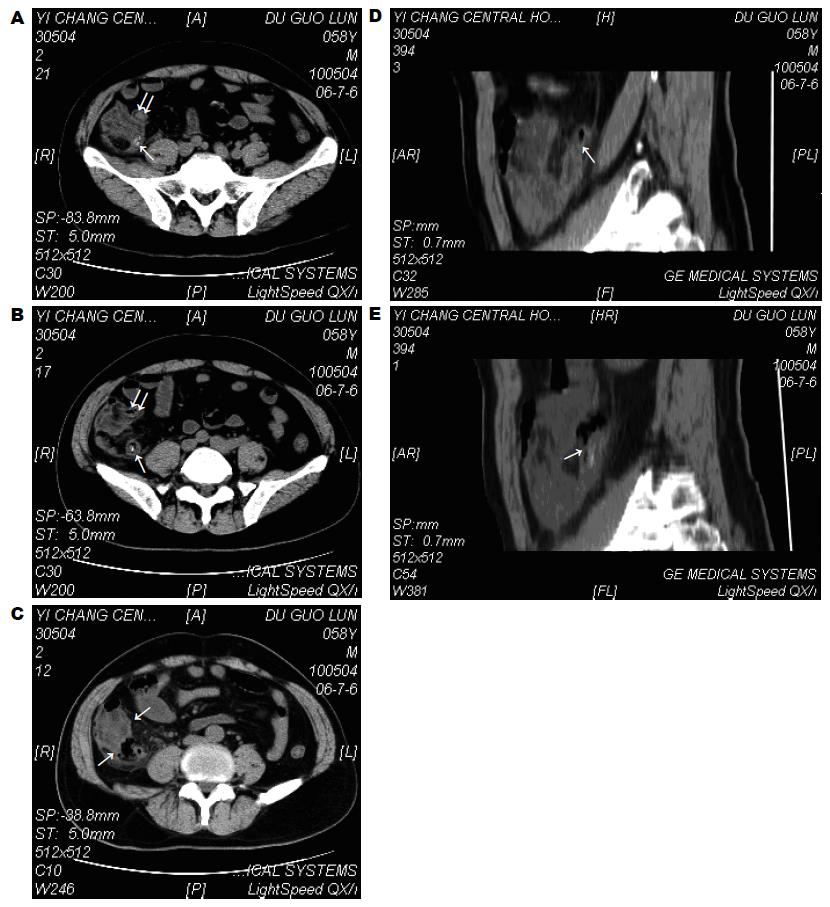
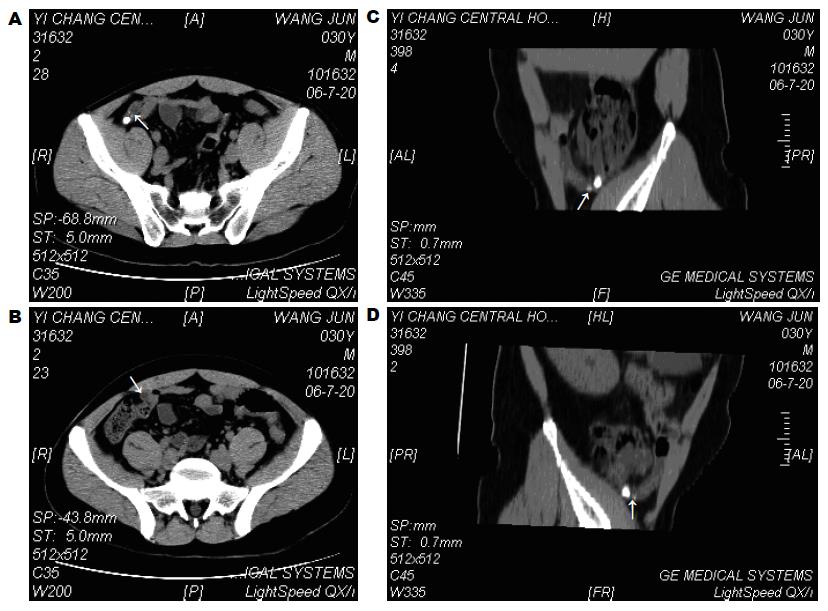
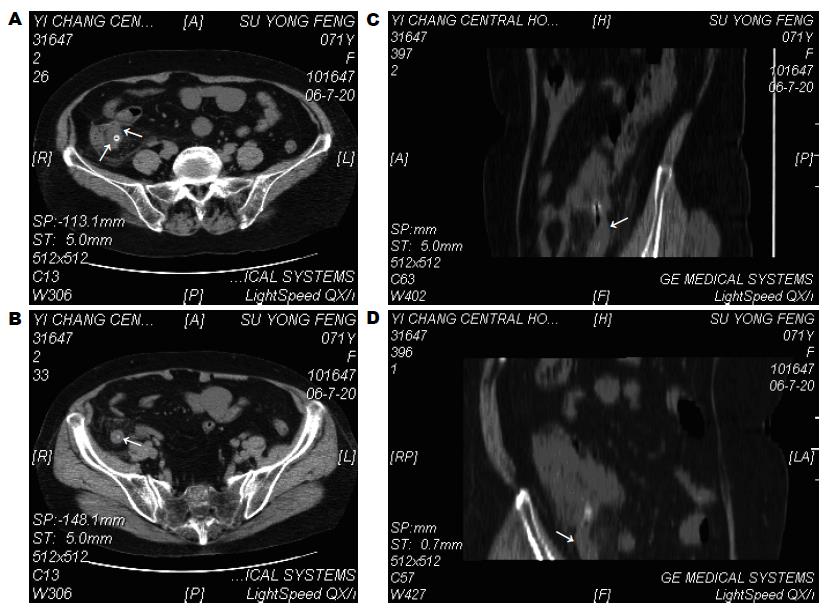
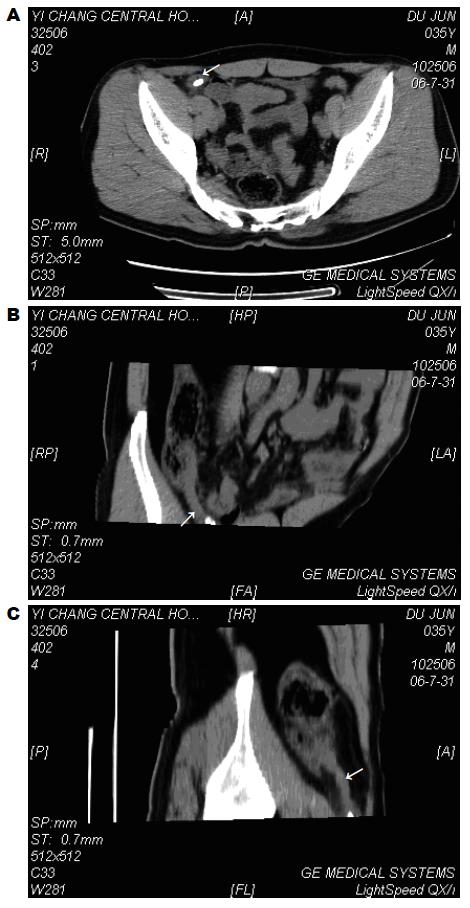
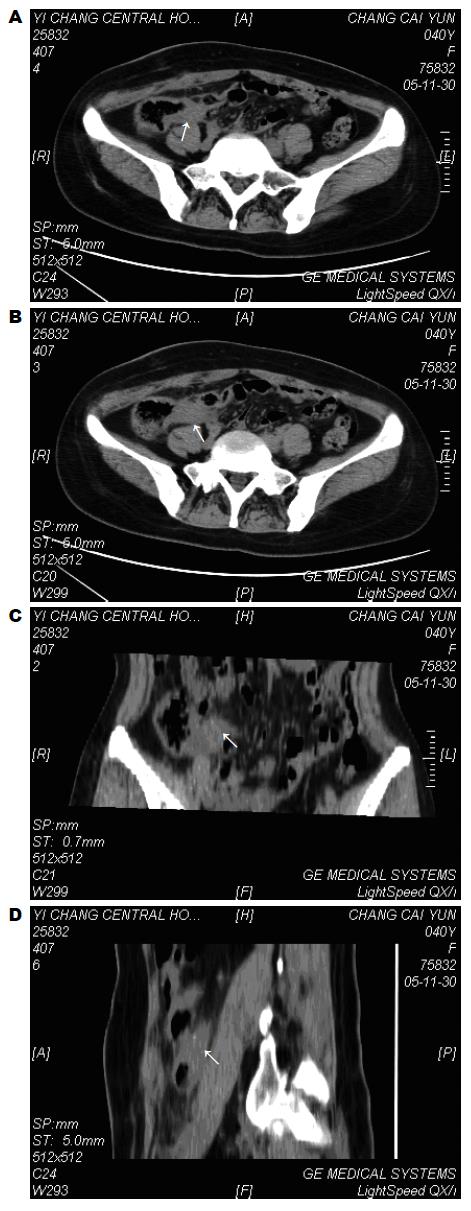
本组19例患者中, 单纯采用CT轴扫图像分析, 16例(84.2%)CT诊断为急性阑尾炎, 3例(15.8%)误诊. 有8例表现为阑尾增粗、壁增厚, 2例增强扫描后阑尾壁有明显强化, 其中4例阑尾内见结石. 盲肠炎和(或)阑尾周围炎10例. 右下腹局限性脓肿5例, 其中2例伴有粪石. 1例盲肠周围见小气泡, 提示为穿孔. 1例女性患者由于表现为盆腔脓肿, 与周围广泛炎性黏连, CT误诊为盆腔炎, 2例患者表现为盲肠及回盲部壁增厚, 与周围黏连, 误诊为回盲部及升结肠肿瘤. 回顾性采用MPR法进行图像分析, 18例(94.7%)CT诊断为阑尾炎, 1例(5.3%)误诊为肠道肿瘤. 手术及病理诊断急性单纯性阑尾炎3例, 急性化脓性阑尾炎伴周围炎8例, 坏疽性阑尾炎2例, 急性阑尾炎穿孔1例, 阑尾周围脓肿5例(图1, 图2, 图3, 图4, 图5, 图6).
急性阑尾炎是临床常见急腹症之一, 大多数患者的临床表现典型, 结合实验室资料即可以明确诊断. 不需要借助影像学检查. 但是据外科文献[3,4]报道, 平均约20%的急性阑尾炎临床症状不典型; 另有一些其他病变酷似阑尾炎的临床表现, 事实上, 40岁以下妇女由于很难与盆腔炎性疾病和急性妇科病区别, 阑尾切除的假阳性率高达35%-45%[3-4]. 因此需要借助影像学帮助鉴别. 对疑为急性阑尾炎的患者常规采用CT检查, 其特异度为95%, 敏感度为100%[1-5], 从而减少不必要的剖腹探查. 阑尾显示与CT检查扫描参数及质量有相当大的关系. 有文献报道使用5 mm层厚扫描, 对于临床怀疑阑尾炎患者诊断敏感性可达到100%. Weltman et al[1]的研究中采用5 mm层厚扫描, 94%可确定异常阑尾, 采用10 mm层厚扫描则仅为69%.
根据条件及患者状态可选择以下几种CT检查方法: (1)非增强的螺旋CT检查法: 不需要对比剂, 在一次屏气下, 连续扫描多层; (2)口服造影法: 用800 mL稀释的硫酸钡或2%的泛影葡胺等在扫描前15, 60 min分两次饮入以充盈小肠, 有时也可使阑尾充盈; (3)经直肠注入对比剂法; (4)静脉注入对比剂法: 经静脉团注对比剂或以1.5 mL/s的速度注入100 mL后再以1 mL/s的速度注入余下的50 mL. 我们认为由于阑尾炎的CT扫描多为急诊检查, 静脉注射非离子型对比剂价格较高昂, 而且多有不便, 同时也存在着对比剂过敏反应的危险, 故不宜作为常规检查方法; 口服对比剂后需60-90 min甚至更长时间方可到达回盲部, 耗时太长, 因此可能延误治疗; 而且与患者的肠道准备情况有关, 也不能广泛使用. 螺旋CT的MPR价格较便宜, 耗时少, 简便易行, 有利于对病变及其周围情况的观察, 提高不典型阑尾炎的诊断符合率, 故可广泛采用[10-16].
阑尾炎的常见CT表现为: (1)直接征象-阑尾的异常: 阑尾增粗(阑尾横径大于6 mm)、阑尾壁增厚、阑尾腔扩大、阑尾结石(若有穿孔, 阑尾结石亦可位于阑尾脓肿或周围组织内)、增强扫描阑尾壁可见强化; (2)间接征象-阑尾周围的异常: 阑尾周围炎性改变、阑尾脓肿(表现为盲肠周围或盆腔内低密度积液区, 或表现为软组织密度灶, 腔内或周围混有小气泡影)、回盲部局部淋巴结肿大、盲肠末端的异常(盲肠末端局部肠壁增厚, 即箭头征)[1-2,12-16].
鉴别诊断[8-16]: 克隆病、盲肠炎、肠结核、肠道肿瘤和盆腔炎等病变位于右下腹时, 可有与阑尾炎相似的CT表现, 应与之鉴别. 本组病例误诊为肿瘤2例, 盆腔炎1例. 误诊为肿瘤的原因是患者年龄大且无典型临床表现, 临床体检扪及右下腹包块, CT示盲肠壁明显增厚. 一般来说, 肠肿瘤往往表现为肠壁不对称性增厚, 不均匀性强化, 强化不如炎性肠壁明显, 如果发现邻近组织直接受侵、腹膜种植或远处转移则可以肯定诊断. 本组诊断为盆腔炎的病例CT仅表现为右下腹脓肿及周围炎性反应, 易与源于附件的炎症或脓肿相混淆, 但后者可见与子宫角相连, 常伴有盆腔积液, 脓肿内及周围很少有气体, 而阑尾脓肿常局限在盲肠周围或结肠后. 含气体的盆腔脓肿则提示胃肠道来源, 如阑尾炎、憩室炎和克隆病. 憩室炎在我国很少见, 如果见到憩室及局限性肠壁增厚和肠管周围炎则要考虑为憩室炎. 阑尾比较细长, 位置和形态变异大, 当病灶与周围广泛黏连时就更不易观察. 螺旋CT的MPR可以从不同的角度观察病变及其周围组织的情况, 有利于判断病灶的中心和起源, 尤其是可以细致地观察有无粪石或小气泡, 观察子宫和邻近脂肪间隙、肠道的情况, 为不典型阑尾炎的诊断和鉴别诊断提供参考. 本组病例采用MPR的方法较单纯采用轴扫的方法诊断符合率明显提高, 证明这一方法较为优越.
我们认为由于小儿患者腹腔内脂肪成分相对较少, 缺乏天然对比, 同时, 小儿肠袢较细小, 肠内容物多, 且迂曲, 相互重叠, 难以详细观察阑尾及回盲部的情况, 对诊断带来一定的困难, 对于采用MPR法仍然无法鉴别的病例, 应结合临床表现、CT增强检查及检查前口服或结肠内给予对比剂等方法. 对确定病变性质可能有帮助. 尤其是对右下腹有混杂密度包块的病例作用更大.
因本组为回顾性研究, 病例数较少, 对于这两种方法的比较还有待于大样本的进一步研究.
CT轴位扫描诊断阑尾炎的已有较多报道, 但应用螺旋CT MPR重建诊断阑尾炎尚未见文献报道, 本文着重分析两种方法对临床表现不典型的阑尾炎的诊断效果, 以期找到一种能广泛使用的检查方法, 从而提高诊断符合率.
症状和体征不典型的阑尾炎临床诊断困难, 易误诊, 螺旋CT MPR方法简单, 可从不同角度观察病变部位及其周围情况, 有利于鉴别诊断, 提高诊断符合率, 具有较高的临床价值.
螺旋CT多平面重建(MPR)对无典型临床表现的急性阑尾炎的诊断价值较高, 在国内首见报道.
MPR方法简单, 可从不同角度观察病变部位及其周围情况, 有利于鉴别诊断, 提高诊断符合率, 具有较高的临床价值. 本文对无典型临床表现的急性阑尾炎的诊断价值在国内首见报道, 有临床价值.
编辑: 张焕兰 电编:张敏
| 1. | Weltman DI, Yu J, Krumenacker J, Huang S, Moh P. Diagnosis of acute appendicitis: comparison of 5- and 10-mm CT sections in the same patient. Radiology. 2000;216:172-177. [PubMed] [DOI] |
| 2. | Sheafor DH, Hertzberg BS, Freed KS, Carroll BA, Keogan MT, Paulson EK, DeLong DM, Nelson RC. Nonenhanced helical CT and US in the emergency evaluation of patients with renal colic: prospective comparison. Radiology. 2000;217:792-797. [PubMed] [DOI] |
| 3. | Harisinghani MG, Gervais DA, Maher MM, Cho CH, Hahn PF, Varghese J, Mueller PR. Transgluteal approach for percutaneous drainage of deep pelvic abscesses: 154 cases. Radiology. 2003;228:701-705. [PubMed] [DOI] |
| 4. | Siewert B, Raptopoulos V, Liu SI, Hodin RA, Davis RB, Rosen MP. CT predictors of failed laparoscopic appendectomy. Radiology. 2003;229:415-420. [PubMed] [DOI] |
| 5. | MacKersie AB, Lane MJ, Gerhardt RT, Claypool HA, Keenan S, Katz DS, Tucker JE. Nontraumatic acute abdominal pain: unenhanced helical CT compared with three-view acute abdominal series. Radiology. 2005;237:114-122. [PubMed] [DOI] |
| 6. | Benjaminov O, Atri M, Hamilton P, Rappaport D. Frequency of visualization and thickness of normal appendix at nonenhanced helical CT. Radiology. 2002;225:400-406. [PubMed] [DOI] |
| 7. | Foley TA, Earnest F, Nathan MA, Hough DM, Schiller HJ, Hoskin TL. Differentiation of nonperforated from perforated appendicitis: accuracy of CT diagnosis and relationship of CT findings to length of hospital stay. Radiology. 2005;235:89-96. [PubMed] [DOI] |
| 8. | Taylor GA. Suspected appendicitis in children: in search of the single best diagnostic test. Radiology. 2004;231:293-295. [PubMed] [DOI] |
| 9. | Puig S, Hörmann M, Rebhandl W, Felder-Puig R, Prokop M, Paya K. US as a primary diagnostic tool in relation to negative appendectomy: six years experience. Radiology. 2003;226:101-104. [PubMed] [DOI] |
| 10. | Lardenoye SW, Puylaert JB, Smit MJ, Holscher HC. Appendix in children with cystic fibrosis: US features. Radiology. 2004;232:187-189. [PubMed] [DOI] |
| 11. | Wiersma F, Srámek A, Holscher HC. US features of the normal appendix and surrounding area in children. Radiology. 2005;235:1018-1022. [PubMed] [DOI] |
| 12. | Keyzer C, Zalcman M, De Maertelaer V, Coppens E, Bali MA, Gevenois PA, Van Gansbeke D. Comparison of US and unenhanced multi-detector row CT in patients suspected of having acute appendicitis. Radiology. 2005;236:527-534. [PubMed] [DOI] |
| 13. | Raptopoulos V, Katsou G, Rosen MP, Siewert B, Goldberg SN, Kruskal JB. Acute appendicitis: effect of increased use of CT on selecting patients earlier. Radiology. 2003;226:521-526. [PubMed] [DOI] |
| 14. | Paulson EK, Harris JP, Jaffe TA, Haugan PA, Nelson RC. Acute appendicitis: added diagnostic value of coronal reformations from isotropic voxels at multi-detector row CT. Radiology. 2005;235:879-885. [PubMed] [DOI] |