修回日期: 2003-08-10
接受日期: 2003-08-25
在线出版日期: 2004-02-15
目的: 通过对影响胃癌淋巴结转移因素的分析, 探讨较准确预测胃癌有无淋巴结转移及其程度的标志.
方法: 采用RT-PCR技术检测62例胃癌患者原发癌组织中Heparanase, MMP-7, VEGF-C, S100A4, hRad17, hTERT, CDH1, KAI1和nm23H1基因的mRNA表达, 结合系统的临床病理检查指标, 运用Binary Logistic regression进行多因素分析, 寻找影响胃癌淋巴结转移的客观标志.
结果: 上述基因在胃癌组织中均有不同程度表达, 其中S100A4和hTERT阳性率最高(96.8%), CDH1表达阳性率最低(64.5%). 多因素分析表明淋巴管癌栓(P = 0.009)和Heparanase表达(P = 0.014)是判断有无淋巴结转移的独立因素, 相对危险度分别为21.137和9.768. 在预测胃癌淋巴结转移程度上(小于或等于6个为轻度转移, 大于或等于7个为重度转移), Lauren分型和MMP-7, hTERT, CDH1基因表达是独立因素(P = 0.012, 0.037, 0.009, 0.021), 其相对危险度分别为10.068, 8.046, 9.159, 0.087, 浆膜受侵面积亦是重要的影响因素.
结论: 胃癌组织中Heparanase高表达、淋巴管癌栓阳性者, 有淋巴结转移的可能性较大; 而组织学为弥漫型、浆膜受侵面积大于20 cm2、原发癌灶中MMP-7、hTERT高表达、CDH1低表达者, 淋巴结转移程度相对较重. 术前检测上述基因mRNA表达并确定Lauren分型, 术中结合胃浆膜受侵面积, 对制定治疗方案有指导意义.
引文著录: 黄宝俊, 徐惠绵, 赵雨杰, 王天骄, 田大彤, 陈峻青. 胃癌淋巴结转移预测的多因素分析. 世界华人消化杂志 2004; 12(2): 266-270
Revised: August 10, 2003
Accepted: August 25, 2003
Published online: February 15, 2004
AIM: To analyze the factors influencing lymph node metastasis in gastric cancer and to screen the indicators that could predict more exactly the extent of lymph node metastasis before surgery.
METHODS: The mRNA expression of heparanase, MMP-7, VEGF-C, S100A4, hRad17, hTERT, CDH1, KAI1 and nm23H1 genes were examined in 62 gastric cancer tissues by reverse transcription polymerase chain reaction (RT-PCR). In combination with clinicopathological features, univariate and multivariate analyses were carried out in order to screen the factors affecting lymph node metastasis of gastric carcinoma.
RESULTS: All the genes above were expressed more or less in gastric cancer tissues. With regard to the positive rate, S100A4 and hTERT were the highest (both 96.8%) and CDH1 was the lowest (64.5%). Multivariate analysis with binary logistic regression showed that lymphatic invasion and heparanase mRNA expression were independent factors that judged whether there was lymph node metastasis, and the odds ratios [Exp (B)] were 21.137 (95%CI 2.115-211.211) and 9.768 (95%CI 1.582-60.300) respectively. When predicting the extent of the lymph node metastasis (the number of lymph node metastasis of no more than 6 was regarded as the fewer and lighter; no less than 7 as the more and heavier), MMP-7, hTERT and CDH1 genes mRNA expression and Lauren type of carcinoma were the independent factors (P = 0.037, 0.009, 0.021 and 0.012 respectively), Exp (B) was 8.046, 9.159, 0.087 and 10.068 respectively. The area of serosa involvement was also an important factor.
CONCLUSION: Heparanase mRNA expression and lymphatic invasion of gastric cancer tissue correlate with lymph node metastasis positively. The degree of lymph node metastasis is more serious in patients with diffusive histological type, area of serosa involvement more than 20 cm2 and MMP-7, hTERT mRNA overexpression, and CDH1 loss of expression in gastric cancer. Above examinations before surgery are indicated to arrive at an optimum treatment scheme.
- Citation: Huang BJ, Xu HM, Zhao YJ, Wang TJ, Tian DT, Chen JQ. Multivariate analysis of predicting lymph node metastasis in gastric cancer. Shijie Huaren Xiaohua Zazhi 2004; 12(2): 266-270
- URL: https://www.wjgnet.com/1009-3079/full/v12/i2/266.htm
- DOI: https://dx.doi.org/10.11569/wcjd.v12.i2.266
胃癌是我国人群中发病率和死亡率均占第一位的恶性肿瘤, 转移扩散是影响预后的首要原因[1-6]. 近年来对胃癌侵袭、转移分子机制的研究日趋深入[7-11], 以期寻求新的有效治疗措施, 然而外科手术仍为其主要的治疗手段, 合理的淋巴结清除是手术治疗成功的关键之一[12]. 但目前尚缺乏客观、有效的判定淋巴结转移及其程度的术前指标. 因此, 从分子水平深入研究胃癌淋巴结转移规律, 寻找预测胃癌淋巴结转移的客观标志, 具有重要临床价值. 文献[13-15]报道Heparanase, MMP-7[3,16], VEGF-C[17-19],S100A4[20], hRad17[21-22], hTERT[10-11,23], CDH1[4-5,24], KAI1[25]和nm23H1[7,26]基因的表达变化分别与不同肿瘤转移关系密切, 尤与淋巴结转移关系密切, 但多为单个或几个基因的研究分析, 尚有一定局限性. 我们运用RT-PCR技术, 同时、并行检测多个相关基因在胃癌组织中的表达, 结合临床病理特征, 进行多因素分析, 寻找影响胃癌淋巴结转移更加客观的指标, 以期术前做出较为准确的预测.
2001-09/2002-09中国医科大学附属第一医院肿瘤外科胃癌患者62例, 其中男41例, 女21例, 年龄28-77(58±1.7)岁, 术前均未经化、放疗. 取新鲜癌组织置液氮中速冻30 min后, -80 ℃深低温冰箱冻存, 其余标本行系统病理检查.
按说明书用TRIzol试剂(Invitrogen公司)提取癌组织总RNA, 并用紫外分光光度计定量、测纯度. 取A260/A280≥1.80的标本, 采用AMV酶反转录试剂盒(Promega公司)合成第一链cDNA, 以1 μg总RNA为模板, Oligo(dT)18为引物, 42 ℃反应1 h. 利用Primer Premier5软件设计Heparanase, MMP-7, VEGF-C, S100A4, hRad17, hTERT, CDH1, KAI1, nm23H1及GAPDH和beta actin基因RT-PCR引物, 分别将上、下游引物设计在不同外显子上, 并将引物Tm值设在55 ℃, 以保证扩增条件的一致性. 具体序列、产物长度及定位见表1. 分别取cDNA溶液4 μL进行PCR扩增, 94 ℃变性4 min, 经30个循环(94 ℃ 35 s、58 ℃ 45 s、72 ℃ 60 s), 72 ℃延伸7 min. 反应体系为: MgCl2 1.5 mmol/L, dNTP 200 μmol/L, 引物各0.5 μmol/L, Taq DNA聚合酶(华美公司)1.2 MU/20 L. 取各基因扩增产物4 μL进行梯度聚丙烯酰胺凝胶电泳(30 g/L浓缩胶和80 g/L分离胶), 银染色检测结果, 干燥后扫描图片存图, 详细步骤参见文献[22]. 应用Chemi Imager 5500自动电泳凝胶成像分析仪测定各基因扩增条带的灰度值(A), 计算各基因mRNA表达指数(I), I = A基因/Aactin B, 因beta actin在不同组织中表达量相对恒定, 银染后扩增条带为黑色, 而该系统检测灰度值时, 条带越暗(即产量越高)值越低, 故表达指数与各基因mRNA在不同组织中的含量呈负相关关系.
| 基因 | 引物 | 产物长度 | 产物定位 | |
| 正义 | 反义 | |||
| hTERT | 5'-ggcgacatggagaacaagc-3' | 5'-aggtgagactggctctgatgg-3' | 340 bp | 9-12exon |
| VEGF-C | 5'-gaggctggcaacataacaga-3' | 5'-ccttgagagagaggcactgt-3' | 321 bp | 2-4exon |
| hRad17 | 5'-aaaatcaagaggtccaag-3' | 5'-cctgagtaaagagcgtgt-3' | 335 bp | 11-14exon |
| S100A4 | 5'-cctggatgtgatggtgtc-3' | 5'-tcttcctgggctgcttat-3' | 278 bp | 1-2exon |
| heparanase | 5'-agaaagacggctaagatg-3' | 5'-atagggtaaccgcaagta-3' | 588 bp | 8-11exon |
| MMP-7 | 5'-agatgtggagtgccagatgt-3' | 5'-tagactgctaccatccgtcc-3' | 358 bp | 1-3exon |
| KAI1 | 5'-agcctgtatcaaagtcaccaa-3' | 5'-gcagaagcccttcctcaca-3' | 571 bp | 2-7exon |
| CDH1 | 5'-ccccataccagaacctcg-3' | 5'-accgcttccttcatagtcaa-3' | 742 bp | 12-16exon |
| nm23H1 | 5'-cgccttgtgggtctgaaa-3' | 5'-tgtggtctgccctcctgt-3' | 377 bp | 2-5exon |
| Actin B | 5'-gatgacccagatcatgtttg-3' | 5'-tggagttgaaggtagtttcg-3' | 491 bp | 2-4exon |
| GAPDH | 5'-cgaccactttgtcaagctca-3' | 5'-aggggtctacatggcaactg-3' | 227 bp | 7-9exon |
统计学处理 胃癌淋巴结转移单因素分析采用χ2检验(fisher's exact test), 多因素分析采用Binary Logistic regression model, 以P<0.05为差异具有显著性, 以上分析均用SPSS10.0软件完成.
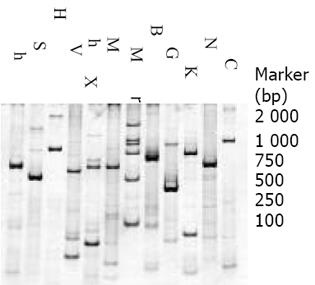
S100A4和hTERT表达阳性率最高(96.8%), 其次为hRad17(91.9%), KAI1(91.9%), Heparanase (88.7%), MMP-7(86.0%), nm23H1(80.6%)和VEGF-C(70.0%), 而CDH1表达阳性率最低(64.5%). 图1为不同基因在同一患者胃癌组织中表达的RT-PCR电泳图片, 其中hTERT, S100A4, Heparanase, MMP-7, KAI1, nm23H1表达相对较强, 而VEGF-C、hRad17、CDH1表达相对较弱.
1997年国际抗癌联盟(UICC)制定了胃癌新的TNM分期系统, 将胃癌转移淋巴结分级(pN)标准以转移淋巴结个数的量化指标为依据分成pN0(0个), pN1(1-6个), pN2(7-15个), pN3(15个以上), 王振宁et al[27]研究发现新TNM分期系统既显示了与预后的一致性, 又较好地反映了胃癌的生物学行为, 因此我们进一步将pN分级划为轻重两组: 小于或等于6个为轻度转移, 大于或等于7个为重度转移. 根据各基因的平均表达指数, 将表达水平分为高、低两组. 将基因表达高低及病理因素分别与淋巴结转移情况进行单因素分析. 结果表明原发癌组织低分化、小结节孤立型淋巴结、淋巴管癌栓阳性及Heparanase、hTERT高表达者, 淋巴结转移阳性率增加, VEGF-C高表达亦与淋巴结转移呈正相关, 但无统计学意义; 癌组织低分化、Lauren分型为弥漫型、浆膜受侵面积大于20 cm2、小结节孤立型淋巴结者, MMP-7, VEGF-C, hRad17, hTERT高表达和CDH1, KAI1低表达者, 淋巴结转移程度相对较重, 转移数量多在7个以上(表2).
| 相关因素 | 淋巴结转移 | 淋巴结转移程度 | |||||||
| 阴性 | 阳性 | χ2 | P | 轻 | 重 | χ2 | P | ||
| 正常+反应 | 1 | 2 | 3 | 0 | |||||
| 浆膜分型 | 结节 | 5 | 15 | 1.869 | 0.393 | 13 | 7 | 4.492 | 0.106 |
| 腱状+多彩弥漫 | 5 | 34 | 18 | 21 | |||||
| 浆膜受侵 | ≤10 | 8 | 29 | 24 | 13 | ||||
| 面积(cm2) | 11-19 | 2 | 12 | 1.06 | 0.589 | 8 | 6 | 7.5 | 0.024 |
| ≥20 | 1 | 10 | 2 | 9 | |||||
| 大体型 | 限局 | 3 | 12 | 0.069 | 0.793 | 11 | 4 | 2.733 | 0.098 |
| 浸润 | 8 | 39 | 23 | 24 | |||||
| 生长方式 | 团块+巢状 | 8 | 35 | 0.072 | 0.789 | 26 | 17 | 1.794 | 0.18 |
| 弥漫 | 3 | 16 | 8 | 11 | |||||
| 分化程度 | 高/中 | 6 | 12 | 4.225 | 0.04 | 15 | 3 | 8.315 | 0.004 |
| 低 | 5 | 39 | 19 | 25 | |||||
| Lauren分型 | 肠型 | 8 | 22 | 3.172 | 0.075 | 23 | 7 | 11.182 | 0.001 |
| 弥漫型 | 3 | 29 | 11 | 21 | |||||
| 侵透浆膜 | - | 8 | 34 | 0.152 | 0.697 | 26 | 16 | 2.625 | 0.105 |
| + | 3 | 17 | 8 | 12 | |||||
| 转移淋巴结 | 大结节融合 | 5 | 18 | 14 | 9 | ||||
| 分型 | 小结节孤立 | 0 | 27 | 14.631 | 0.001 | 9 | 18 | 11.952 | 0.003 |
| 一般型 | 6 | 6 | 11 | 1 | |||||
| 淋巴管 | - | 10 | 25 | 6.495 | 0.011 | 22 | 13 | 2.087 | 0.149 |
| 癌栓 | + | 1 | 26 | 12 | 15 | ||||
| MMP-7 | 低 | 6 | 24 | 0.203 | 0.652 | 22 | 8 | 8.028 | 0.005 |
| 高 | 5 | 27 | 12 | 20 | |||||
| Heparanase | 低 | 9 | 21 | 5.984 | 0.014 | 19 | 11 | 1.694 | 0.193 |
| 高 | 2 | 30 | 15 | 17 | |||||
| S100A4 | 低 | 8 | 31 | 0.553 | 0.457 | 24 | 15 | 1.95 | 0.167 |
| 高 | 3 | 20 | 10 | 13 | |||||
| VEGF-C | 低 | 10 | 31 | 3.666 | 0.056 | 27 | 14 | 5.93 | 0.015 |
| 高 | 1 | 20 | 7 | 14 | |||||
| hTERT | 低 | 9 | 25 | 3.93 | 0.047 | 27 | 7 | 18.356 | 0.00 0018 |
| 高 | 2 | 26 | 7 | 21 | |||||
| hRad17 | 低 | 7 | 31 | 0.031 | 0.86 | 25 | 13 | 4.753 | 0.029 |
| 高 | 4 | 20 | 9 | 15 | |||||
| nm23H1 | 低 | 7 | 27 | 0.418 | 0.518 | 17 | 17 | 0.712 | 0.399 |
| 高 | 4 | 24 | 17 | 11 | |||||
| KAI1 | 低 | 6 | 35 | 0.801 | 0.371 | 18 | 23 | 5.846 | 0.016 |
| 高 | 5 | 16 | 16 | 5 | |||||
| CDH1 | 低 | 8 | 37 | 0.0 001 | 0.99 | 20 | 25 | 7.16 | 0.007 |
| 高 | 3 | 14 | 14 | 3 | |||||
考虑存在混杂因素的影响, 进一步将有统计学意义的单因素结果进行二维Logistic回归分析. 结果显示淋巴管癌栓(P = 0.009)和Heparanase表达(P = 0.014)是判断有无淋巴结转移的独立因素, 若淋巴管癌栓阳性或Heparanase高表达, 则有淋巴结转移的危险分别增加21.137和9.768倍. 而淋巴结转移程度的分析结果表明: Lauren分型, MMP-7, hTERT 和CDH1表达是独立预测因素(P = 0.012, 0.037, 0.009, 0.021), 若原发癌组织为弥漫型, MMP-7, hTERT, CDH1高表达者, 其转移淋巴结数大于或等于7个的危险分别增加10.068, 8.046, 9.159和0.087倍. 其中浆膜受侵面积和VEGF-C表达虽无统计学意义(P = 0.052, 0.118), 但也是较重要的预测因素, 其相对危险度分别为3.157和4.649 (表3).
| 淋巴结转移 | 相关系数(x) | 回归系数(b) | 标准误(Sx) | 统计量Wald值 | 显著性P | 相对危险度Exp(B) | 95.0% CI for EXP(B) | |
| Lower | Upper | |||||||
| 淋巴管癌栓 | 3.051 | 1.174 | 6.794 | 0.009 | 21.137 | 2.115 | 211.211 | |
| 有 | Heparanase | 2.279 | 0.929 | 6.022 | 0.014 | 9.768 | 1.582 | 60.300 |
| 无 | hTERT | 1.563 | 0.946 | 2.731 | 0.098 | 4.775 | 0.748 | 30.500 |
| 常数项 | -4.511 | 1.846 | 5.968 | 0.015 | 0.011 | |||
| 浆膜受侵面积 | 1.15 | 0.592 | 3.77 | 0.052 | 3.157 | 0.989 | 10.074 | |
| 程度 | Lauren分型 | 2.309 | 0.915 | 6.37 | 0.012 | 10.068 | 1.675 | 60.504 |
| MMP-7 | 2.085 | 1 | 4.348 | 0.037 | 8.046 | 1.133 | 57.123 | |
| VEGF-C | 1.537 | 0.982 | 2.448 | 0.118 | 4.649 | 0.678 | 31.872 | |
| hTERT | 2.215 | 0.852 | 6.756 | 0.009 | 9.159 | 1.724 | 48.652 | |
| CDH1 | -2.444 | 1.063 | 5.291 | 0.021 | 0.087 | 0.011 | 0.697 | |
| 常数项 | -4.113 | 2.579 | 2.545 | 0.111 | 0.016 | |||
淋巴结转移、复发是影响胃癌预后的主要因素, 而无转移的淋巴结尚具有重要的免疫监视作用. 因此, 术前、术中准确判断淋巴结转移范围和程度, 施行合理的淋巴结清除术, 对提高疗效具有十分重要意义. 目前影响胃癌淋巴结转移因素的报道多停留在病理形态学水平, 或仅涉及一个(或几个)分子指标, 且多应用免疫组化、原位杂交等检测技术, 术前应用受到一定的限制[1,3-4,6,10,13,16,18,22,24,28-29]. 为了使胃癌淋巴结清除范围更趋于合理, 我们将病理因素和基因表达相结合, 从临床应用角度出发, 在方法和实验设计上做了改进. 采用RT-PCR技术, 操作相对简单, 而且术前胃镜检查时即可获得标本; 所选指标均是文献报道与肿瘤淋巴转移关系密切的基因, 代表性强; 病理因素与基因表达相结合, 单因素与多因素序贯分析, 结果更加全面、可靠; 引物设计时分别将上、下游引物设计在不同外显子上, 并将引物Tm值均设在55 ℃, 可保证扩增的真实性和条件的一致性, 免去多个基因检测需要多次PCR的烦琐, 便于临床推广应用.
有无淋巴结转移的单因素分析发现, 原发癌组织低分化、淋巴管癌栓阳性、小结节孤立型转移淋巴结及Heparanase, hTERT高表达者, 淋巴结转移阳性率增加, 这与文献[13-14,23,28]报道一致. 但经多因素分析发现, 只有淋巴管癌栓和Heparanase与淋巴结转移呈正相关关系, 淋巴管癌栓阳性者有淋巴结转移的风险增加21.1倍, 肝素酶高表达者淋巴结转移阳性的风险增加9.7倍. 癌细胞首先要侵入淋巴管形成癌栓, 而后才能引流到区域淋巴结形成转移灶, 因此淋巴管癌栓阳性者有淋巴结转移的可能性显著增加. 肝素酶是一种内切糖苷酶, 能够降解细胞外基质和脉管基底膜的主要成分硫酸肝素和硫酸肝素多糖, 是癌细胞侵袭和转移过程中的首要步骤. 肝素酶在正常组织中的表达严格限于胎盘和淋巴源性器官, 这是否影响其表达与胃癌淋巴结转移特异性相关尚需进一步研究探讨. Takaoka et al[13]研究发现在胃癌组织中肝素酶mRNA和蛋白质表达具有一致性, 因此检测肝素酶mRNA水平可以反应其蛋白质的高低.
淋巴结转移程度的单因素分析发现, 癌组织低分化、Lauren分型为弥漫型、浆膜受侵面积大于20 cm2、小结节孤立型淋巴结者, MMP-7, VEGF-C, hRad17, hTERT高表达和CDH1, KAI1低表达者, 淋巴结转移程度相对较重. 而多因素分析发现, 组织学类型、MMP-7, hTERT和CDH1表达是独立影响因素, 相对危险度分别为10.068, 8.046, 9.159和0.087; 浆膜受侵面积亦是较重要的影响因素(P = 0.052), 可能与例数较少有关. 浆膜受侵面积大于20 cm2者, 往往病期较晚; 而组织学为弥漫型者, 癌细胞的生物学行为恶性度往往较高, 均体现出高转移潜能, 我们认为浆膜受侵面积和组织学类型是影响胃癌淋巴结转移程度较为确切的大体指标. MMP-7能够降解Ⅳ型胶原、蛋白多糖、laminin、elastin等, 其与胃癌、结直肠癌、食管癌、胰腺癌、肺癌转移关系密切[3,16,30]. 端粒酶活性增高与多种肿瘤的临床病理因素及淋巴转移相关, 人端粒酶催化亚基(hTERT)在端粒酶表达中起决定性作用, hTERT基因表达水平与端粒酶活性一致[10-11,23]. E-钙黏附素(CDH1)与连环素结合形成复合体介导同种细胞间黏附反应, 研究发现许多人类肿瘤中CDH1表达下调与淋巴结转移和肿瘤侵袭性密切相关[4,24]. 我们运用多因素分析筛选发现MMP-7, hTERT和CDH1是影响胃癌淋巴结转移程度的标志基因, 我们还将进一步研究其相应蛋白质表达与胃癌淋巴结转移程度的相关性, 以期寻求新的有效治疗靶点.
总之, 淋巴管癌栓和肝素酶是预测胃癌有无淋巴结转移的特异性指标; MMP-7, hTERT, CDH1和Lauren分型、浆膜受侵面积是预测胃癌淋巴结转移严重程度的敏感性指标. 由此推测肝素酶可能是在胃癌淋巴结转移的始动阶段起重要作用, 而MMP-7, hTERT和CDH1是在胃癌淋巴结转移的加速阶段起重要作用. 术前RT-PCR检测胃原发癌组织中上述基因mRNA表达并确定Lauren分型, 术中结合胃浆膜受侵面积, 对制定治疗方案有一定指导意义.
编辑: N/A
| 1. | Zhang S, Li L, Lin JY, Lin H. Imbalance between expression of matrix metalloproteinase-9 and tissue inhibitor of metalloproteinase-1 in invasiveness and metastasis of human gastric carcinoma. World J Gastroenterol. 2003;9:899-904. [PubMed] [DOI] |
| 4. | Zhou YN, Xu CP, Han B, Li M, Qiao L, Fang DC, Yang JM. Expression of E-cadherin and beta-catenin in gastric carcinoma and its correlation with the clinicopathological features and patient survival. World J Gastroenterol. 2002;8:987-993. [PubMed] [DOI] |
| 5. | 周 永宁, 徐 采朴, 韩 彪, 王 金穗, 房 殿春, 彭 贵勇, 杨 建民, 刘 海. 胃癌E-钙粘蛋白表达与临床病理学的关系. 世界华人消化杂志. 2002;10:1121-1124. [DOI] |
| 6. | 王 耕, 杨 道华, 孙 勤, 代 全武, 惠 震, 陈 立新, 易 建华, 朱 礼国. 胃癌组织若干癌相关基因的表达与淋巴转移的关系. 世界华人消化杂志. 1999;7:803-804. [DOI] |
| 8. | Shao JC, Wu JF, Wang DB, Qin R, Zhang H. Relationship between the expression of human telomerase reverse transcriptase gene and cell cycle regulators in gastric cancer and its significance. World J Gastroenterol. 2003;9:427-431. [PubMed] [DOI] |
| 9. | Zhang H, Wu J, Meng L, Shou CC. Expression of vascular endothelial growth factor and its receptors KDR and Flt-1 in gastric cancer cells. World J Gastroenterol. 2002;8:994-998. [PubMed] [DOI] |
| 11. | Yao XX, Yin L, Sun ZC. The expression of hTERT mRNA and cellular immunity in gastric cancer and precancerosis. World J Gastroenterol. 2002;8:586-590. [PubMed] [DOI] |
| 13. | Takaoka M, Naomoto Y, Ohkawa T, Uetsuka H, Shirakawa Y, Uno F, Fujiwara T, Gunduz M, Nagatsuka H, Nakajima M. Heparanase expression correlates with invasion and poor prognosis in gastric cancers. Lab Invest. 2003;83:613-622. [PubMed] [DOI] |
| 14. | Tang W, Nakamura Y, Tsujimoto M, Sato M, Wang X, Kurozumi K, Nakahara M, Nakao K, Nakamura M, Mori I. Heparanase: a key enzyme in invasion and metastasis of gastric carcinoma. Mod Pathol. 2002;15:593-598. [PubMed] [DOI] |
| 15. | Endo K, Maejara U, Baba H, Tokunaga E, Koga T, Ikeda Y, Toh Y, Kohnoe S, Okamura T, Nakajima M. Heparanase gene expression and metastatic potential in human gastric cancer. Anticancer Res. 2001;21:3365-3369. [PubMed] |
| 16. | Liu XP, Kawauchi S, Oga A, Tsushimi K, Tsushimi M, Furuya T, Sasaki K. Prognostic significance of matrix metalloproteinase-7 (MMP-7) expression at the invasive front in gastric carcinoma. Jpn J Cancer Res. 2002;93:291-295. [PubMed] [DOI] |
| 17. | Duff SE, Li C, Jeziorska M, Kumar S, Saunders MP, Sherlock D, O'Dwyer ST, Jayson GC. Vascular endothelial growth factors C and D and lymphangiogenesis in gastrointestinal tract malignancy. Br J Cancer. 2003;89:426-430. [PubMed] [DOI] |
| 18. | Amioka T, Kitadai Y, Tanaka S, Haruma K, Yoshihara M, Yasui W, Chayama K. Vascular endothelial growth factor-C expression predicts lymph node metastasis of human gastric carcinomas invading the submucosa. Eur J Cancer. 2002;38:1413-1419. [PubMed] [DOI] |
| 19. | Mattila MM, Ruohola JK, Karpanen T, Jackson DG, Alitalo K, Härkönen PL. VEGF-C induced lymphangiogenesis is associated with lymph node metastasis in orthotopic MCF-7 tumors. Int J Cancer. 2002;98:946-951. [PubMed] [DOI] |
| 20. | Rosty C, Ueki T, Argani P, Jansen M, Yeo CJ, Cameron JL, Hruban RH, Goggins M. Overexpression of S100A4 in pancreatic ductal adenocarcinomas is associated with poor differentiation and DNA hypomethylation. Am J Pathol. 2002;160:45-50. [PubMed] [DOI] |
| 21. | Sasaki H, Chen LB, Auclair D, Moriyama S, Kaji M, Fukai I, Kiriyama M, Yamakawa Y, Fujii Y. Overexpression of Hrad17 gene in non-small cell lung cancers correlated with lymph node metastasis. Lung Cancer. 2001;34:47-52. [PubMed] [DOI] |
| 23. | Hara H, Yamashita K, Shinada J, Yoshimura H, Kameya T. Clinicopathologic significance of telomerase activity and hTERT mRNA expression in non-small cell lung cancer. Lung Cancer. 2001;34:219-226. [PubMed] [DOI] |
| 25. | Muneyuki T, Watanabe M, Yamanaka M, Shiraishi T, Isaji S. KAI1/CD82 expression as a prognosic factor in sporadic colorectal cancer. Anticancer Res. 2001;21:3581-3587. [PubMed] |
| 26. | Chow NH, Liu HS, Chan SH. The role of nm23-H1 in the progression of transitional cell bladder cancer. Clin Cancer Res. 2000;6:3595-3599. [PubMed] |
| 30. | Sasaki H, Yukiue H, Moiriyama S, Kobayashi Y, Nakashima Y, Kaji M, Kiriyama M, Fukai I, Yamakawa Y, Fujii Y. Clinical significance of matrix metalloproteinase-7 and Ets-1 gene expression in patients with lung cancer. J Surg Res. 2001;101:242-247. [PubMed] [DOI] |