修回日期: 2002-09-02
接受日期: 2002-10-03
在线出版日期: 2003-02-15
目的: 肠外高营养对重症溃疡性结肠炎患者血清胃动素, 肽YY, IgG和糖蛋白含量的影响并讨论其变化的临床意义.
方法: 重症溃疡性结肠炎患者89例, 男51例, 女38例, 年龄23-57(平均38±13)岁, 均经电子结肠镜检查和X线钡灌肠检查, 以及组织学检查确诊, 并连续粪培养2次排除细菌感染, 同时排除阿米巴肠病, 血吸虫病, 肠道肿瘤和内分泌疾病. 病变部位包括乙状结肠45例, 降结肠21例, 结肠脾曲15例和横结肠8例; 临床类型包括复发型44例, 持续型30例和初发型15例. 采取肠外静脉补充足够的营养, 完全胃肠道休息. 并于确诊后3 d内和治疗缓解后的上午07: 00空腹采血, 用放射免疫法(RIA)测定血清胃动素(MTL), 肽YY(PYY)和IgG, 用血清电泳法测定α1, α2和γ糖蛋白.
结果: 经过4 wk治疗后痊愈27例(30%), 好转48例(54%), 无效14例(16%), 总有效率84%. 与对照比较, 重症溃疡性结肠炎患者血清MTL(ng/L, 311.6±99.8 vs 207.3±98.4, P<0.01), PYY(pmoL/L, 1.6±0.8 vs 1.1±0.6, P<0.05), IgG (g/L, 23.6±10.2 vs 13.1±6.9, P<0.01)和α1球蛋白 (g/L, 2.7±1.2 vs 1.5±0.9, P<0.01) 明显升高, 而α2球蛋白(g/L, 4.2±2.6 vs 6.8±2.3, P<0.05) 则降低, 但经过治疗后可恢复, 治疗有效和无效患者间上述变化无明显差异(P>0.05). 全部患者血清AST, ALT在正常范围, 血清白蛋白治疗后明显好转(g/L, 34.2±9.6 vs 21.4±8.7, P<0.05), 组织学也明显改善.
结论: 重症溃疡性结肠炎肠外静脉高营养疗法是一种有效可行的方法, 且可以改善血清MTL, PYY, IgG和α1, α2糖蛋白水平.
引文著录: 郭学刚, 孙安华, 李彩宁, 张宏博, 周新民, 许昌泰, 潘伯荣. 肠外高营养对重症溃疡性结肠炎患者血清胃动素, 肽YY, IgG和糖蛋白含量的影响. 世界华人消化杂志 2003; 11(2): 224-228
Revised: September 2, 2002
Accepted: October 3, 2002
Published online: February 15, 2003
AIM: To study the effects and clinical significance of parenteral hyperalimentation on levels of serum motilin, peptide YY, IgG and glycoproteins in patients with severe ulcerative colitis.
METHODS: Eighty-nine patients (males 51, females 38, age 23-57 years) with severe ulcerative colitis were examinated with colonoscope, barium enema, the diagnosis was confirmed histologically. Bacterial infection was excluded through twice consecutive stool cultures. And ameba, schistosomiasis, gastroentertinal cancer and endocrine diseases were also excluded. Ulcerative colitis was found in sigmoid (n = 45), descending colon (n = 21), colon splenic flexure (n = 15) and transverse colon (n = 8). Its clinical categories included relapse (n = 44), persistent (n = 30) and initial (n = 15). Parenteral hyperalimentation was applied to patients once diagnosis was made; three days later, fasting venous blood was drawed to test serum motilin (MTL), peptide YY (PYY) and IgG by radioimmunoassy, and serum α1, α2 and g glycoproteins by electrophoresis.
RESULTS: After 4-week period therapy with parental hypernutrition, 27 cases (30%) recovered completely, 48 (54%) improved, and 14(16%) failed to therapy, the total effective rate was 84%. Level of serum MTL, PYY, IgG, and α1-glycoprotein in colitis patients were significant higher than those in control, α 2-glycoprotein was lower than that in control (P < 0.05). All these abnormal data became normal after treatment. However, no difference of these parameters was observed between patients who were effective to therapy and those who failed to therapy (P < 0.05). No obvious change in serum aspartate aminotransferase (AST), alanine aminotransferase (ALT) and -glycoprotein was existed in all patients (P > 0.05). Level of serum albumin was increased(P < 0.05), and the histological change in ulcerative colitis was significantly improved after treatment.
CONCLUSION: The parenteral hyperalimentation therapy improved effectively serum levels of motilin, PYY, IgG and glycoproteins in patients with severe ulcerative colitis.
- Citation: Guo XG, Sun AH, Li CN, Zhang HB, Zhou XM, Xu CT, Pan BR. Effects of parenteral hyperalimentation on serum motilin, peptide YY, IgG and glycoproteins in severe ulcerative colitis. Shijie Huaren Xiaohua Zazhi 2003; 11(2): 224-228
- URL: https://www.wjgnet.com/1009-3079/full/v11/i2/224.htm
- DOI: https://dx.doi.org/10.11569/wcjd.v11.i2.224
溃疡性结肠炎(ulcerative colitis)是炎症性肠病(inflammatory bowel disease, IBD)的一种, 其病因不明, 是以浅表性, 非特异性炎症病变为主的肠道疾病, 主要累及乙状结肠, 也可累及其他部分或全部结肠[1-5]; 少数病变严重者可出现10 cm以内的反流性回肠炎. 临床症状以黏液脓血便, 腹痛, 腹泻或里急后重为主; 急性危重病例, 有全身症状, 并常伴有肠道外疾病和肝损害, 关节炎, 皮肤损害, 心肌病变, 口腔溃疡, 虹膜睫状体炎及内分泌病症[3-8]. 对溃疡性结肠炎的治疗方法包括激素, 磺胺类, 免疫抑制等, 但效果均欠佳[4,9-17]. 我们研究肠外高营养对重症溃疡性结肠炎的治疗效果及其对血清胃动素, 肽YY, IgG, α1(α1-Gly), α2(α2-Gly)和γ糖蛋白(γ-Gly)的影响.
1998-01/2001-12住院溃疡性结肠炎患者207例, 其中属重症的89例, 男51例, 女38例, 年龄23-57(平均38±13)岁. 全部患者均经电子结肠镜检查和X线钡灌肠检查, 以及组织学检查确诊, 并连续粪培养2次排除细菌感染, 同时排除阿米巴肠病, 血吸虫病, 肠道肿瘤和内分泌疾病. 病变部位包括乙状结肠45例, 降结肠21例, 结肠脾曲15例和横结肠8例; 临床类型包括复发型44例, 持续型30例和初发型15例. 另选健康对照23例, 男16名, 女7名, 年龄22-58 (平均37±12)岁, 排除胃肠道和内分泌疾病.
治疗原则是在发作期间, 主要采取对症治疗, 纠正营养缺乏, 恢复血容量, 纠正贫血, 控制合并症等处理. 我们主要采取肠外高营养, 其治疗方案是: 静脉补充足够的营养, 完全胃肠道休息, 待病情缓解后逐步恢复饮食, 以保持长久的缓解状态. 所用药物为: 肠外高营养配方: 200 g/L脂肪乳250 mL; 氨基酸500 mL; 支链氨基酸250 mL; 250 g/L葡萄糖250 mL(必要时); 100 g/L葡萄糖500-1 000 mL; 生理盐水500 mL; 100 g/L氯化钾30-50 mL; 维他得匹特10 mL; 水乐维他10 mL; 胰岛素20-30 U; 安达美10 mL. 上述混入3 000 mL袋中深静脉滴注, 1次/d, 4 wk. 治疗1 wk后无效患者则加用少量激素, 有发热者(≥38.5℃)给予抗生素. 全部患者都经 治疗4 wk后进行结果分析: 痊愈好转-临床症状减轻, 肠镜等检查, 肠黏膜检查恢复正常; 好转-临床症状减轻, 肠镜检查, 肠黏膜病变较前明显改善, 大便常规检查有少量红, 白细胞; 无效-治疗后, 临床症状和肠镜等检查, 无改善或无明显改善. 研究对象还于确诊后3 d内和静脉高营养治疗缓解后的上午07: 00空腹采血, 用放射免疫法(RIA)测定血清胃动素(MTL), 肽YY(PYY)和IgG, 用血清电泳法测定α1, α2和γ糖蛋白.
统计学处理 测定结果用表示, 与对照组比较用非配对学生t检验.
经过4 wk治疗后痊愈27例(30%), 好转48例(54%), 无效14例(16%), 总有效率84%. 重症溃疡性结肠炎患者血清MTL, PYY, IgG和α1糖蛋白明显高于对照组, 但经过治疗后可恢复(表1), 治疗有效和无效患者间上述变化无明显差异(P>0.05). 全部患者血清AST, ALT在正常范围, γ糖蛋白变化不明显(g/L, 9.7±4.6), 血清白蛋白明显好转(g/L, 34.2±9.6 vs 21.4±8.7, P<0.05). 治疗无效的14例上述各指标治疗前后无明显改变(P >0.05).
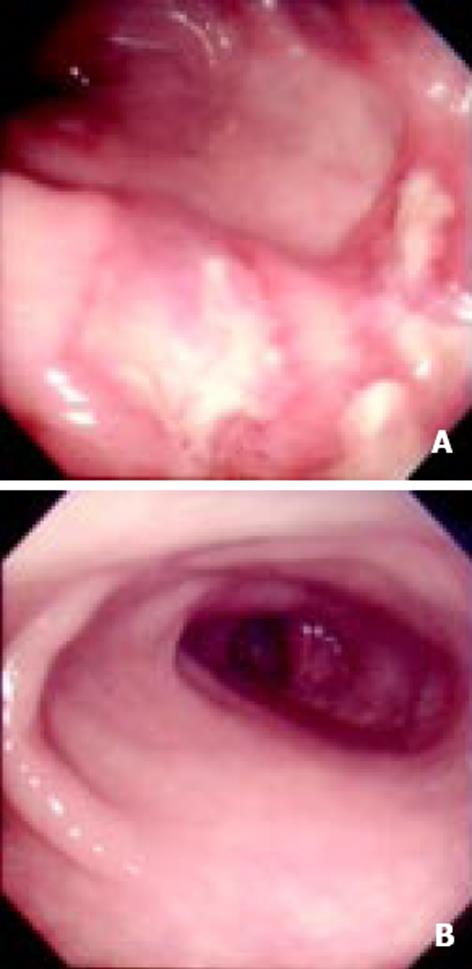
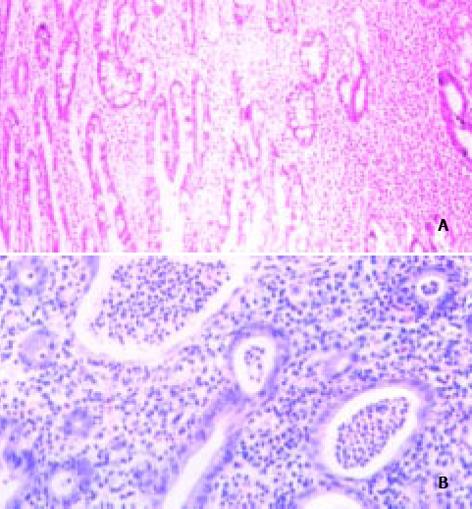
所有患者均为急性期重症, 其黏膜充血, 水肿更显著, 镜下病变部位基本无正常黏膜(图1A), 与治愈后形成明显对比(图1B). 黏膜呈粗细不等的颗粒状.或溃疡明显增多并融合成片, 有黏膜桥形成. 极易接触出血或黏膜糜烂结肠自发出血, 有假膜或黏液脓血性渗出物覆盖, 有时见岛状或类假息肉样黏膜再生. 重症溃疡性结肠炎治疗前病理组织可见中性细胞浸润, 淋巴细胞, 浆细胞也较多及假性息肉(图2A); 腺上皮间中性炎细胞浸润, 杯状细胞减少; 隐窝炎症或脓肿形成和他固有膜血管的炎症(图2B). 经治疗病情缓解后病变明显改善, 取代上述的是肠腺细胞排列不规则, 隐窝数减少, 既有瘢痕组织又有基底膜增厚; 杯状细胞增多, 黏膜下层纤维化加重, 可见淋巴管扩张; 固有膜层圆细胞浸润明显或大淋巴滤泡出现.
溃疡性结肠炎为-病程经历甚为悬殊而又无特异治疗的疾病. 在发作期间, 主要采取对症治疗, 纠正营养缺乏, 恢复血容量, 纠正贫血, 控制合并症等处理, 并应鼓励患者增强治病信心, 坚持合理必要的治疗, 多数患者可达到完全缓解[5-7,10-15,18-25]. 缓解期治疗则基于力争和保持缓解状态. 减少发作次数, 减轻发作程度和缩短发作期限. 我们主要采取肠外静脉补充足够的营养, 完全休息胃肠道, 待病情缓解后逐步恢复饮食, 以保持长久的缓解状态, 结果收到满意的效果, 且患者血清胃动素, 肽YY, IgG, α1和α2糖蛋白含量基本恢复[22-28]. 溃疡性结肠炎初起病情较轻或疾病较平稳恢复期, 可采用中医辨证治疗, 可口服或直肠给药. 当暴发型, 危重病证以及较为严重的并发症, 宜采用西药治疗以及激素治疗, 待病情平稳时, 可结合中医药治疗[29-35].
血清蛋白电泳α1糖蛋白升高是溃疡性结肠炎活动期的可靠指标, 我们研究结果也说明这-点. α2糖蛋白升高则反应病情缓解γ球蛋白下降为预后不良的征兆, 低蛋白血症说明病变范围广, 通常已越过乙状结肠[17-21].
溃疡性结肠患者发病的解剖和生理基础可能是肠黏膜屏障或他的通透性存在某些缺陷, 细胞因子是炎症反应的必需中介物(如白介素, 肿瘤坏死因子和干扰素等), 这些细胞因子具有类似激素对全身的作用, 同时伴有严重的和潜在的危险作用[21-25,36-42]. 我们的研究中患者血清MTL, PYY, IgG和α1糖蛋白均有改变, 且临床治愈或好转后血清IgG和α1糖蛋白下降, 提示溃疡性结肠炎的发生可能与细胞因子的作用有关, 这-结果与以往研究类似[23,29-34]. 我们采用肠外高营养疗法, 使患者的胃肠道得以完全休息, 这样可能通过减少对肠道刺激从而改善体内炎症反应, 以达到治疗目的. 胃动素是22个氨基酸残基组成的多肽, 正常情况影响血中胃动素水平与进餐和进餐的种类, 胃肠道的消化过程和消化期间, 胃容量的扩大, 小肠活动状态和十二指肠内酸度, 其他消化道激素的作用等因素有关[24-28,43-46]. 溃疡性结肠炎患者血清MTL升高可能由于结肠黏膜炎症作用使下消化道蠕动增快, 机体为调节内外平衡, 胃小肠以适应结肠运动, 故血清MTL分泌和释放增加. PYY的主要作用为收缩血管, 抑制胰腺外分泌, 抑制胃肠蠕动及胃酸分泌. 我们研究中血清PYY升高可能系结肠炎症刺激所致. IgG主要作用是参与免疫, 溃疡性结肠炎作为一种与免疫相关的疾病, 必然有体内IgG的改变, 本文结果也证实这-点.
治疗重症溃疡性结肠炎通常用柳氮磺胺吡啶类药物, 如5-氨水扬酸(5-aminosalicylic acid)[28], 利多格雷(ridogrel)[29]等, 但有时效果不理想. 严重患者在内科多次治疗无效时可考虑外科治疗[11]. 溃疡结肠炎原因不明, 尚无具体的预防措施, 对于反复发作或持续的患者, 保持心情舒畅恬静, 注意饮食有节, 起居有常, 避免劳累, 预防肠道感染, 对阻止复发或病情进一步发展有-定作用[40-47]. 此外还应注意心理调节和注意控制饮食, 对腹痛腹泻者, 宜食少渣, 易消化, 低脂肪, 高蛋白饮食, 对有或可疑不耐受的食物, 如虾, 蝎, 鳖, 牛奶, 花生等应尽量避免食用, 应忌食辣椒, 冰冻, 生冷食品, 戒除烟酒.
编辑: N/A
| 1. | Welters CF, Heineman E, Thunnissen FB, van den Bogaard AE, Soeters PB, Baeten CG. Effect of dietary inulin supplementation on inflammation of pouch mucosa in patients with an ileal pouch-anal anastomosis. Dis Colon Rectum. 2002;45:621-627. [PubMed] [DOI] |
| 2. | Kurbegow AC, Ferry GD. Guided self-management and patient-directed follow-up of ulcerative colitis: a randomised trial. J Pediatr Gastroenterol Nutr. 2002;34:428-429. [PubMed] [DOI] |
| 3. | Bariol C, Meagher AP, Vickers CR, Byrnes DJ, Edwards PD, Hing M, Wettstein AR, Field A. Early studies on the safety and efficacy of thalidomide for symptomatic inflammatory bowel disease. J Gastroenterol Hepatol. 2002;17:135-139. [PubMed] [DOI] |
| 4. | van Bergeijk JD, Wilson JH, Nielsen OH, von Tirpitz C, Karvonen AL, Lygren I, Rädler A, Waldum HL, Mulder CJ, Friis S. Octreotide in patients with active ulcerative colitis treated with high dose corticosteroids (OPUS 1). Eur J Gastroenterol Hepatol. 2002;14:243-248. [PubMed] [DOI] |
| 5. | Ben-Josef E, Han S, Tobi M, Vargas BJ, Stamos B, Kelly L, Biggar S, Kaplan I. Intrarectal application of amifostine for the prevention of radiation-induced rectal injury. Semin Radiat Oncol. 2002;12:81-85. [PubMed] [DOI] |
| 6. | Malchow H, Gertz B; CLAFOAM Study group. A new mesalazine foam enema (Claversal Foam) compared with a standard liquid enema in patients with active distal ulcerative colitis. Aliment Pharmacol Ther. 2002;16:415-423. [PubMed] [DOI] |
| 7. | Tremaine WJ, Brzezinski A, Katz JA, Wolf DC, Fleming TJ, Mordenti J, Strenkoski-Nix LC, Kurth MC; AXYS Ulcerative Colitis Study Group. Treatment of mildly to moderately active ulcerative colitis with a tryptase inhibitor (APC 2059): an open-label pilot study. Aliment Pharmacol Ther. 2002;16:407-413. [PubMed] [DOI] |
| 8. | Sood A, Midha V, Sood N, Kaushal V, Awasthi G. Methylprednisolone acetate versus oral prednisolone in moderately active ulcerative colitis. Indian J Gastroenterol. 2002;21:11-13. [PubMed] |
| 9. | Kayazawa M, Saitoh O, Kojima K, Nakagawa K, Tanaka S, Tabata K, Matsuse R, Uchida K, Hoshimoto M, Hirata I. Lactoferrin in whole gut lavage fluid as a marker for disease activity in inflammatory bowel disease: comparison with other neutrophil-derived proteins. Am J Gastroenterol. 2002;97:360-369. [PubMed] [DOI] |
| 10. | Xu CT, Pan BR. Current medical therapy for ulcerative colitis. World J Gastroenterol. 1999;5:64-72. [PubMed] [DOI] |
| 11. | Zhang Y, Wang ZH, Huang MT. Relationship between electrogastric dysrhythmia and leucin-encephalin in rats. Huaren Xiaohua Zazhi. 1998;6:969-971. [DOI] |
| 12. | Mansfield JC, Giaffer MH, Cann PA, McKenna D, Thornton PC, Holdsworth CD. A double-blind comparison of balsalazide, 6.75 g, and sulfasalazine, 3 g, as sole therapy in the management of ulcerative colitis. Aliment Pharmacol Ther. 2002;16:69-77. [PubMed] [DOI] |
| 13. | Green JR, Mansfield JC, Gibson JA, Kerr GD, Thornton PC. A double-blind comparison of balsalazide, 6.75 g daily, and sulfasalazine, 3 g daily, in patients with newly diagnosed or relapsed active ulcerative colitis. Aliment Pharmacol Ther. 2002;16:61-68. [PubMed] [DOI] |
| 14. | Skelly MM, Logan RF, Jenkins D, Mahida YR, Hawkey CJ. Toxicity of mycophenolate mofetil in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2002;8:93-97. [PubMed] [DOI] |
| 15. | Rizzello F, Gionchetti P, Galeazzi R, Novelli G, Valpiani D, D'Arienzo A, Manguso F, Castiglione G, Varoli G, Campieri M. Oral beclomethasone dipropionate in patients with mild to moderate ulcerative colitis: a dose-finding study. Adv Ther. 2001;18:261-271. [PubMed] [DOI] |
| 16. | Bauditz J, Wedel S, Lochs H. Thalidomide reduces tumour necrosis factor alpha and interleukin 12 production in patients with chronic active Crohn's disease. Gut. 2002;50:196-200. [PubMed] [DOI] |
| 17. | Vrij AA, Jansen JM, Schoon EJ, de Bruïne A, Hemker HC, Stockbrügger RW. Low molecular weight heparin treatment in steroid refractory ulcerative colitis: clinical outcome and influence on mucosal capillary thrombi. Scand J Gastroenterol Suppl. 2001;41-47. [PubMed] [DOI] |
| 18. | Shen B, Achkar JP, Lashner BA, Ormsby AH, Remzi FH, Brzezinski A, Bevins CL, Bambrick ML, Seidner DL, Fazio VW. A randomized clinical trial of ciprofloxacin and metronidazole to treat acute pouchitis. Inflamm Bowel Dis. 2001;7:301-305. [PubMed] [DOI] |
| 19. | Kruis W, Schreiber S, Theuer D, Brandes JW, Schütz E, Howaldt S, Krakamp B, Hämling J, Mönnikes H, Koop I. Low dose balsalazide (1.5 g twice daily) and mesalazine (0.5 g three times daily) maintained remission of ulcerative colitis but high dose balsalazide (3.0 g twice daily) was superior in preventing relapses. Gut. 2001;49:783-789. [PubMed] [DOI] |
| 20. | Joelsson M, Andersson M, Bark T, Gullberg K, Hallgren T, Jiborn H, Magnusson I, Raab Y, Sjödahl R, Ojerskog B. Allopurinol as prophylaxis against pouchitis following ileal pouch-anal anastomosis for ulcerative colitis. A randomized placebo-controlled double-blind study. Scand J Gastroenterol. 2001;36:1179-1184. [PubMed] [DOI] |
| 21. | Robinson A, Thompson DG, Wilkin D, Roberts C; Northwest Gastrointestinal Research Group. Guided self-management and patient-directed follow-up of ulcerative colitis: a randomised trial. Lancet. 2001;358:976-981. [PubMed] [DOI] |
| 22. | Maunder RG, Esplen MJ. Supportive-expressive group psychotherapy for persons with inflammatory bowel disease. Can J Psychiatry. 2001;46:622-626. [PubMed] [DOI] |
| 23. | Xu CT, Wang RL, Ma LS. Alterations of serum motilin, peptide YY, IgG and ferritin in patients with ulcerative colitis. Xin Xiaohuabingxue Zazhi. 1997;5:247-248. |
| 24. | Mantzaris GJ, Petraki K, Archavlis E, Amberiadis P, Kourtessas D, Christidou A, Triantafyllou G. A prospective randomized controlled trial of intravenous ciprofloxacin as an adjunct to corticosteroids in acute, severe ulcerative colitis. Scand J Gastroenterol. 2001;36:971-974. [PubMed] [DOI] |
| 25. | Farup PG, Hinterleitner TA, Lukás M, Hébuterne X, Rachmilewitz D, Campieri M, Meier R, Keller R, Rathbone B, Oddsson E. Mesalazine 4 g daily given as prolonged-release granules twice daily and four times daily is at least as effective as prolonged-release tablets four times daily in patients with ulcerative colitis. Inflamm Bowel Dis. 2001;7:237-242. [PubMed] [DOI] |
| 26. | Shen B, Achkar JP, Lashner BA, Ormsby AH, Remzi FH, Bevins CL, Brzezinski A, Petras RE, Fazio VW. Endoscopic and histologic evaluation together with symptom assessment are required to diagnose pouchitis. Gastroenterology. 2001;121:261-267. [PubMed] [DOI] |
| 27. | Bouma G, Kaushiva A, Strober W. Experimental murine colitis is regulated by two genetic loci, including one on chromosome 11 that regulates IL-12 responses. Gastroenterology. 2002;123:554-565. [PubMed] [DOI] |
| 28. | Mahmud N, O'Toole D, O'Hare N, Freyne PJ, Weir DG, Kelleher D. Evaluation of renal function following treatment with 5-aminosalicylic acid derivatives in patients with ulcerative colitis. Aliment Pharmacol Ther. 2002;16:207-215. [PubMed] [DOI] |
| 29. | Tytgat GN, Van Nueten L, Van De Velde I, Joslyn A, Hanauer SB. Efficacy and safety of oral ridogrel in the treatment of ulcerative colitis: two multicentre, randomized, double-blind studies. Aliment Pharmacol Ther. 2002;16:87-99. [PubMed] [DOI] |
| 30. | Jugde F, Alizadeh M, Boissier C, Chantry D, Siproudhis L, Corbinais S, Quelvennec E, Dyard F, Campion JP, Gosselin M. Quantitation of chemokines (MDC, TARC) expression in mucosa from Crohn's disease and ulcerative colitis. Eur Cytokine Netw. 2001;12:468-477. [PubMed] |
| 31. | Zhang ZY, Hou ZJ, Guo JY. Gastrointestinal hormones and their clinic application. Huaren Xiaohua Zazhi. 1998;6:447-448. [DOI] |
| 32. | Yi SX, Lin YP, Yan J, Chang XR, Yang Y. Effect of electro-acupuncture on gastric motility, substance P (SP) and motilin (MTL) in rats. Shijie Huaren Xiaohua Zazhi. 2001;9:284-287. [DOI] |
| 33. | Kirsner JB. Historical origins of current IBD concepts. World J Gastroenterol. 2001;7:175-184. [PubMed] [DOI] |
| 34. | Wu HG, Zhou LB, Pan YY, Huang C, Chen HP, Shi Z, Hua XG. Study of the mechanisms of acupuncture and moxibustion treatment for ulcerative colitis rats in view of the gene expression of cytokines. World J Gastroenterol. 1999;5:515-517. [PubMed] [DOI] |
| 35. | Gao W, Huang YX, Chen H, Zhao NX, Sun DY, Zhang HX, Wang QL. Regulatory mechanis m of electroacupuncture on the stomach channel brain gut peptide immune network. Shijie Huaren Xiaohua Zazhi. 2001;9:279-283. [DOI] |
| 36. | Zhang K, Deng CS, Zhu YQ, Yang YP, Zhang YM. Significance of nuclear factor-kB, cyclooxygenase 2 and inducible nitric oxide synthase expression in human ulcerative colitis tissues. Shijie Huaren Xiaohua Zazhi. 2002;10:575-578. [DOI] |
| 37. | Xia B. Etiology and pathogenesis of inflammatory bowel disease. Shijie Huaren Xiaohua Zazhi. 2001;9:245-250. [DOI] |
| 38. | Xu MQ, Xue L, Gong JP. Significance of Kupffer cell NF-kB activation during hepatic ischemia/reperfusion in rats. Shijie Huaren Xiaohua Zazhi. 2001;9:1250-1253. [DOI] |
| 39. | Mei Q, Yu JP, Xu JM, Xiang L. The effect of melatonin on the immunological function of colitis in rats. Shijie Huaren Xiaohua Zazhi. 2002;10:193-196. [DOI] |
| 40. | Weaver SA, Russo MP, Wright KL, Kolios G, Jobin C, Robertson DA, Ward SG. Regulatory role of phosphatidylinositol 3-kinase on TNF-alpha-induced cyclooxygenase 2 expression in colonic epithelial cells. Gastroenterology. 2001;120:1117-1127. [PubMed] [DOI] |
| 41. | Qi JM, Zhang YD. Expression of eNOS and iNOS in rats of acute liver failure. Shijie Huaren Xiaohua Zazhi. 2001;9:1003-1007. [DOI] |
| 42. | Wu HP, Wu KC, Li L, Yao LP, Lan M, Wang X, Fan DM. Cloning of human cyclooxygenase 2(COX-2) encoding gene and study of gastric cancer cell transfected with its antisense vector. Shijie Huaren Xiaohua Zazhi. 2000;8:1211-1217. [DOI] |
| 43. | Sun DY, Huang YX, Cu ZH, Gao W, Wang QL. Effect of electro-puncture on gastric antral pressure and relationship with brain gut peptides level of gastric mucus in dogs. Shijie Huaren Xiaohua Zazhi. 1999;7:997-998. [DOI] |
| 44. | Sun DY, Huang YX, Cu ZH, Gao W, Wang QL, Liu GS. Effects of electroacupuncture on gastric mucosal blood flow and plasma gut hormone level in dogs. Huaren Xiaohua Zazhi. 1998;6:936-938. [DOI] |
| 45. | Peng ZS, Hu PJ, Lin HL, Cui Y, Chen W. Evaluation of biopsy pathology i n diagnosis of ulcerative colitis. Shijie Huaren Xiaohua Zazhi. 2001;9:1269-1273. [DOI] |
| 46. | Chen ZY, Yan MX, Xiang BK, Zhan HW. Alterations of gut hormones of blood and colonic mucosa in rats with chronic stress. Shijie Huaren Xiaohua Zazhi. 2001;9:59-61. [DOI] |
| 47. | Xu CT, Pan BR. Gene therapy in gastrointestinal diseases. Ross Gastroenterol Zh. 2001;2:5-25. [PubMed] |