Published online Dec 15, 2003. doi: 10.3748/wjg.v9.i12.2751
Revised: September 9, 2003
Accepted: September 15, 2003
Published online: December 15, 2003
AIM: Activated pancreatic stellate cells (PSCs) have been implicated in the pathogenesis of pancreatic fibrosis and inflammation. Primary PSCs can be subcultured only several times because of their limited growth potential. A continuous cell line may therefore be valuable in studying molecular mechanisms of these pancreatic disorders. The aim of this study was to establish a cell line of rat PSCs by spontaneous immortalization.
METHODS: PSCs were isolated from the pancreas of male Wistar rats, and conventional subcultivation was performed repeatedly. Telomerase activity was measured using the telomere repeat amplification protocol. Activation of transcription factors was assessed by electrophoretic mobility shift assay. Activation of mitogen-activated protein (MAP) kinases was examined by Western blotting using anti-phosphospecific antibodies. Expression of cytokine-induced neutrophil chemoattractant-1 was determined by enzyme immunoassay.
RESULTS: Conventional subcultivation yielded actively growing cells. One clone was obtained after limiting dilution, and designated as SIPS. This cell line has been passaged repeatedly more than 2 years, and is thus likely immortalized. SIPS cells retained morphological characteristics of primary, culture-activated PSCs. SIPS expressed α-smooth muscle actin, glial acidic fibrillary protein, vimentin, desmin, type I collagen, fibronectin, and prolyl hydroxylases. Telomerase activity and p53 expression were negative. Proliferation of SIPS cells was serum-dependent, and stimulated with platelet-derived growth factor-BB through the activation of extracellular signal-regulated kinase. Interleukin-1β activated nuclear factor-κB, activator protein-1, and MAP kinases. Interleukin-1β induced cytokine-induced neutrophil chemoattractant-1 expression through the activation of nuclear factor-κB and MAP kinases.
CONCLUSION: SIPS cells can be useful for in vitro studies of cell biology and signal transduction of PSCs.
- Citation: Masamune A, Satoh M, Kikuta K, Suzuki N, Shimosegawa T. Establishment and characterization of a rat pancreatic stellate cell line by spontaneous immortalization. World J Gastroenterol 2003; 9(12): 2751-2758
- URL: https://www.wjgnet.com/1007-9327/full/v9/i12/2751.htm
- DOI: https://dx.doi.org/10.3748/wjg.v9.i12.2751
Chronic pancreatitis as well as pancreatic cancer are accompanied by progressive fibrosis that is characterized by loss of functional tissue and its replacement by extracellular matrix rich connective tissues[1,2]. In contrast to liver fibrosis, the molecular mechanisms of pancreatic fibrogenesis remain to be elucidated. In 1998, star-shaped cells in the pancreas, namely pancreatic stellate cells (PSCs), were identified and characterized[3,4]. They are morphologically very similar to the hepatic stellate cells that play a central role in fibrosis of the liver[5]. In normal pancreas, stellate cells are quiescent and can be identified by the presence of vitamin A-containing lipid droplets in the cytoplasm. In response to pancreatic injury or inflammation, they are transformed (“activated”) from quiescent phenotype into highly proliferative myofibroblast-like cells which express the cytoskeletal protein α-smooth muscle actin (α-SMA), and produce type I collagen and other extracellular matrix components. Many of the morphological and metabolic changes associated with the activation of PSCs in animal models of fibrosis also occur when these cells are grown in culture on plastics in serum-containing medium. Therefore, culture of primary PSCs on plastics has been accepted as an established model that mimics the phenotypic changes that occur during the process of PSC activation following pancreatic injury. There is accumulating evidence that PSCs, like hepatic stellate cells, are responsible for the development of pancreatic fibrosis[3,4,6]. Furthermore, PSCs might participate in the pathogenesis of acute pancreatitis through the expression of monocyte chemoattractant protein-1 and intercellular adhesion molecule-1[7,8]. The activation of signaling pathways such as p38 mitogen-activated protein (MAP) kinase[9] is likely to play a key role in PSC activation. However, the precise intracellular signaling pathways in PSCs are largely unknown.
Although primary stellate cell culture is a useful tool for studying molecular mechanisms of pancreatic fibrosis and inflammation in vitro, their isolation is time-consuming, yields are relatively low, and there is considerable heterogeneity between preparations. Several weeks in culture are required to obtain sufficient cells to perform experiments. In addition, primary cells can be subcultured only several times because of their limited life span in vitro. Because rat cells are known to be immortalized by spontaneous transformation, this study aimed to establish a rat PSC line by spontaneous immortalization.
[γ-32P]ATP was obtained from Amersham Biosciences UK, Ltd. (Buckinghamshire, England). Rat recombinant platelet-derived growth factor (PDGF)-BB was from R&D Systems (Minneapolis, MN). Recombinant human interleukin (IL)-1β was from Roche Applied Science (Mannheim, Germany). Rabbit antibodies against phosphorylated MAP kinases, total MAP kinases, and inhibitor of nuclear factor κB (NF-κB)-α (IκB-α) were purchased from Cell Technologies, Inc. (Beverly, MA). Rabbit polyclonal antibody against p53 was from Santa Cruz Biotechnology (Santa Cruz, CA). Rabbit antibodies against rat type I collagen and prolyl hydroxylases (α, β) were from LSL Cosmo Bio (Tokyo, Japan). Rabbit anti-rat fibronectin antibody was from Chemicon International (Temecula, CA). Rabbit antibody against glyceraldehyde-3-phosphate dehydrogenase (G3PDH) was from Trevigen (Gaithersburg, MD). SP600125, U0126 and SB202190 were from Calbiochem (La Jolla, CA). All other reagents were products of Sigma-Aldrich (St. Louis, MO) unless specifically described.
All animal procedures were performed in accordance with the National Institutes of Health Animal Care and Use Guidelines. Rat PSCs were prepared from the pancreas tissues of male Wistar rats (Japan SLC Inc., Hamamatsu, Japan) weighing 200-250 g as previously described[3]. Isolated stellate cells were cultured in Ham’s F-12 containing 10% heat-inactivated fetal bovine serum (FBS; ICN Biomedicals, Aurora, OH), penicillin sodium, and streptomycin sulfate. When reaching confluent, the cells were trypsinized with 0.05% trypsin/0.01% EDTA. Initially, cells were passaged at a ratio of 1:3. After the 10th passage, cells were split at 1:5. A homogeneous population of cells, designated as SIPS, was cloned by limiting dilution, and expanded. SAM-K is another rat PSC line established by retrovirus-mediated introduction of simian virus 40 large T antigen[10]. SAM-K cells and primary PSCs were maintained in Ham’s F-12 containing 10% FBS, penicillin sodium, and streptomycin sulfate.
SIPS cells were grown directly on slides, serum-starved for 24 hours, and immunostaining for α-SMA was performed using a streptavidin-biotin-peroxidase complex detection kit (Histofine Kit; Nichirei, Tokyo, Japan) as previously described[11]. Briefly, cells were fixed in 100% methanol at -20 °C, and then endogenous peroxidase activity was blocked by incubation with hydrogen peroxide in methanol for 5 minutes. After immersion in normal rabbit serum, the slides were incubated with mouse anti-α-SMA antibody (at 1:200 dilution) at 4 °C overnight. The slides were incubated with biotinylated anti-mouse immunoglobulin antibody, and peroxidase-conjugated streptavidin. Finally, color was developed by incubating the slides with diaminobenzidine (Dojindo, Kumamoto, Japan). Expression of glial acidic fibrillary protein, vimentin, desmin, type I collagen, fibronectin, and prolyl hydroxylases (α, β) was examined in a similar manner.
The levels of activated, phosphorylated MAP kinases were determined by Western blotting as previously described[12]. Briefly, cells were lysed in sodium dodecyl sulfate buffer (62.5 mM Tris-HCl at pH 6.8, 2% sodium dodecyl sulfate, 10% glycerol, 50 mM dithiothreitol, 0.1% bromphenol blue) for 15 minutes on ice. The samples were then sonicated for 2 seconds, heated for 5 minutes, and centrifuged at 12000×g for 5 minutes to remove insoluble cell debris. Cellular proteins (approximately 100 μg) were fractionated on a 10% sodium dodecyl sulfate-polyacrylamide gel. They were transferred to a nitrocellulose membrane (Bio-Rad, Hercules, CA), and the membrane was incubated overnight at 4 °C with rabbit anti-phosphospecific MAP kinase antibodies (at 1:1000 dilution). After incubation with peroxidase-conjugated goat anti-rabbit secondary antibody for 1 hour, proteins were visualized using an ECL kit (Amersham Biosciences UK, Ltd.). Levels of total MAP kinases, p53, G3PDH, and IκB-α were determined in a similar manner.
Telomerase activity was measured using the telomere repeat amplification protocol (TRAP) with the Telo TAGGG Telomerase PCR ELISAkit (Roche Applied Science). Briefly, SIPS, SAM-K, and primary PSCs (passage 3) were harvested separately, and the cell number was counted. The cell extracts were prepared from an equal number of cells, and used in telomerase-mediated elongation, adding the telomeric repeats to the 3’ end of the biotin-labeled synthetic P1-TS-primer. These elongation products were amplified by PCR using the primers P1-TS and P2, generating PCR products with the telomerase-specific 6-nucleotide increments. An aliquot of the resulting PCR product was denatured, hybridized to a digoxigenin-labeled, telomeric repeat-specific detection probe, and immobilized to a streptavidin-coated microtiter plate. Then, peroxidase-conjugated anti-digoxigenin antibody was added to detect the immobilized PCR product, and the telomerase activity was determined, after the addition of 3,3’, 5,5’-tetramethylbenzidine (substrate), as O.D.450-O.D.690. Ribonuclease A-treated cell extracts were used as negative controls. The mean of the absorbance readings of the negative control was subtracted from those of the samples, and the samples were regarded as telomerase positive if the O.D. difference was higher than 0.2.
Senescence of SIPS, SAM-K, and primary PSCs (passage 20) was examined by SA-β-Gal staining[13]. Cells were grown directly on slides, fixed, and stained with β-Gal staining solution (β-galactosidase staining kit; Mirus, Madison, WI), pH adjusted to 6.0, for 16 hours at 37 °C. After washed with phosphate-buffered saline, the slides were viewed under light microscope.
Serum-starved SIPS cells (approximately 80% density) were treated with FBS at various concentrations or PDGF-BB (at 25 ng/ml). Cell proliferation was assessed using a commercial kit (Cell proliferation ELISA, BrdU; Roche Applied Science) according to the manufacturer’s instructions. This is a colorimetric immunoassay based on the measurement of 5-bromo-2’-deoxyuridine (BrdU) incorporation during DNA synthesis[14]. After 24-hour incubation with experimental reagents, cells were labeled with BrdU for 3 hours at 37 °C. Cells were then fixed, and incubated with peroxidase-conjugated anti-BrdU antibody. The peroxidase substrate 3,3’,5,5’-tetramethylbenzidine was added, and BrdU incorporation was quantitated by O.D.370-O.D.492.
Following 1-hour-incubation, approximately 5 × 106 cells were harvested and nuclear extracts were prepared, and electrophoretic mobility shift assay was performed as previously described[15]. Double-stranded oligonucleotide probes for NF-κB (5’-AGTTGAGGGGACTTTCCCAGGC-3’), and activator protein-1 (AP-1) (5’-CGCTTGATGAGTCAGCCGGAA-3’) were end-labeled with [γ-32P]ATP. Nuclear extracts (approximately 5 μg) were incubated with the labeled oligonucleotide probe for 20 minutes at 22 °C, and electrophoresed through a 4% polyacrylamide gel. Gels were dried and autoradiographed at -80 °C overnight. A 100-fold excess of unlabelled oligonucleotide was incubated with nuclear extracts for 10 minutes prior to the addition of the radiolabeled probe in the competition assays.
After a 24 hour-incubation, cell culture supernatants were harvested and stored at -80 °C. CINC-1 levels in the culture supernatants were measured by enzyme immunoassay (Panapharm Laboratories, Udo, Japan) according to the manufacturer's instructions.
The results were expressed as mean ± standard deviation (mean ± SD). Luminograms and autoradiograms are representative of at least three experiments. Differences between experimental groups were evaluated by two-tailed unpaired Student’s t test. A P value of less than 0.05 was considered statistically significant.
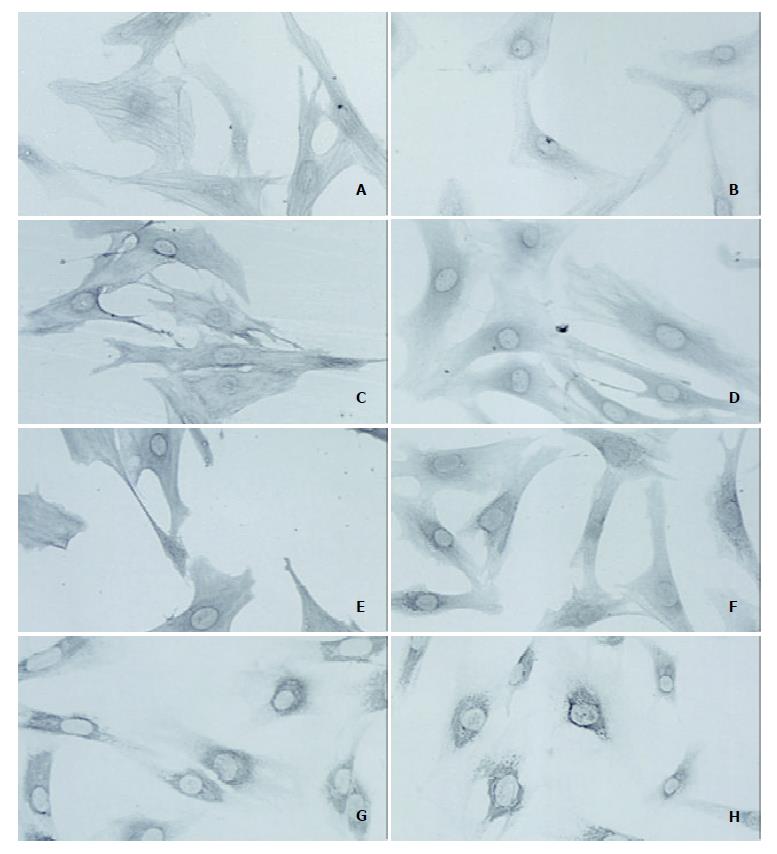
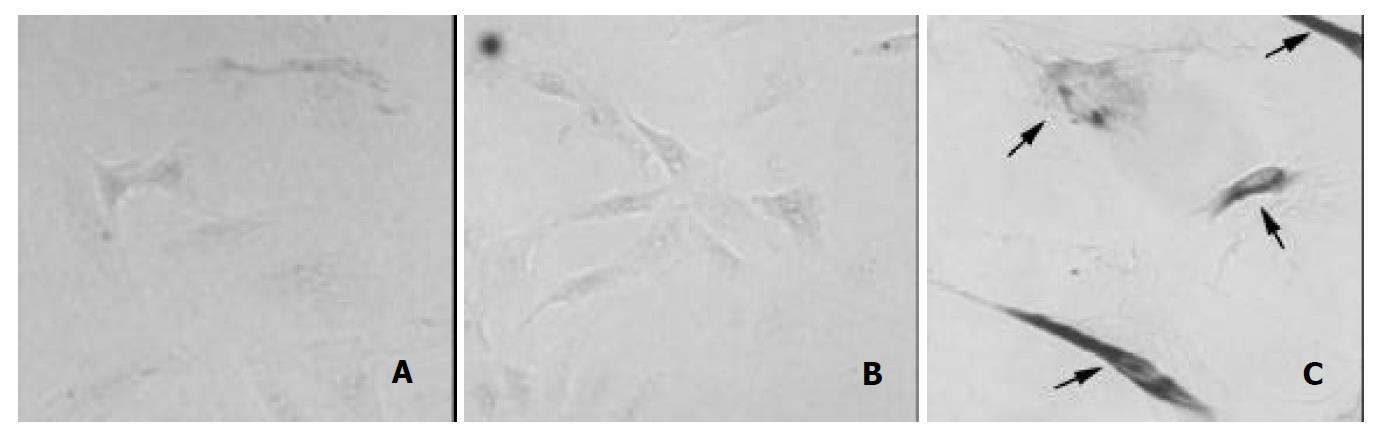
PSCs were isolated from the pancreas of male Wistar rats, and conventional subcultivation was performed repeatedly. This procedure yielded actively growing cells. After limited dilution, one clone was obtained and designated as SIPS. SIPS cells were myofibroblast-like shaped, and morphologically very similar to primary, culture-activated PSCs. The characteristic fiber-like pattern of positive α-SMA staining was observed throughout the cytoplasm in SIPS cells (Figure 1A). In addition, SIPS cells showed positive staining for cytoskeletal proteins glial acidic fibrillary protein (Figure 1B), vimentin (Figure 1C), and desmin (Figure 1D). SIPS cells also expressed extracellular matrix proteins type I collagen (Figure 1E) and fibronectin (Figure 1F). SIPS cells expressed prolyl hydroxylases (α, β) (Figure 1G, H), that are key enzymes in the hydroxylation of the proline residues in procollagen and are useful markers of collagen synthesis[7]. These results suggest that SIPS cells shared many phenotypical and functional characteristics with primary, culture-activated PSCs. During the two years of culture, SIPS cells have been passaged repeatedly over 100 population doublings without showing any evidence of senescence. Indeed, SA-β-Gal, a biomarker of senescent cells[13], was not detected in SIPS and in SAM-K cells (Figure 2A, B). In contrast, SA-β-Gal was detected in late-passage (passage 20) primary PSCs (Figure 2C). The phenotypic characteristics of SIPS remained unaltered, suggesting that they have acquired an immortalized phenotype. SIPS cells have conserved the characteristics of non-transformed cells since they did not form foci, and did not grow on soft agar (data not shown). the samples were regarded as telomerase positive (“a”) if the difference in absorbance was higher than 0.2. Data are shown as mean ± SD (n = 6).
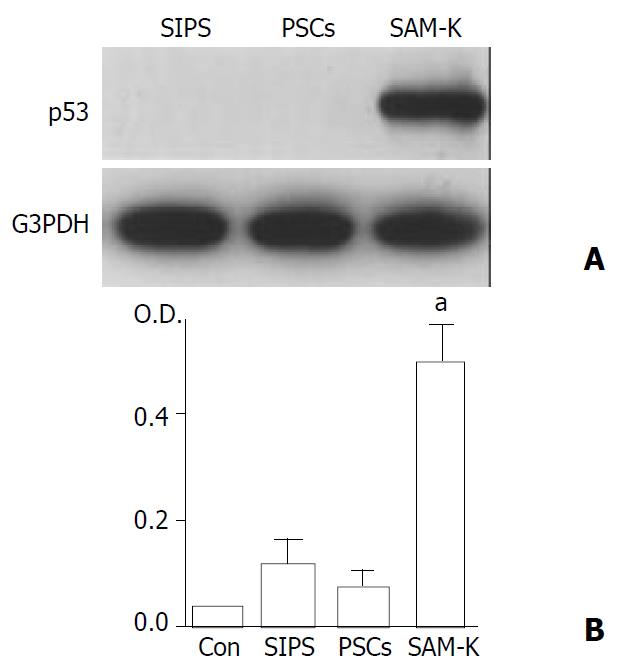
We next examined telomerase activity and p53 expression, potentially important factors in cellular immortalization[16,17]. p53 expression was not detected in SIPS cells and primary PSCs (passage 3), whereas the p53 level was very high in SAM-K cells (Figure 3A). As measured by the TRAP assay, SIPS cells and primary PSCs were negative for telomerase activity, whereas SAM-K cells were positive (Figure 3B).
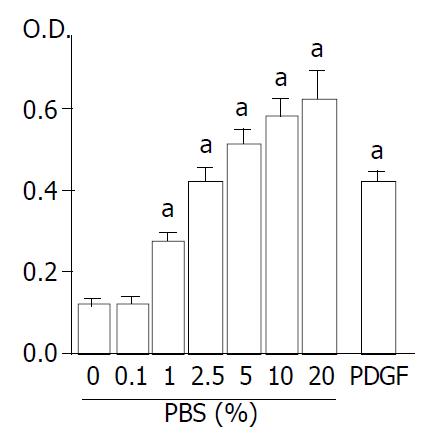
Previous studies have shown that proliferation of primary PSCs was stimulated by growth factors such as serum and PDGF-BB[18-20]. Especially, PDGF-BB has been shown to be the most potent mitogen for PSCs, and is likely to be an important mediator of the increased proliferation of the cells both in vivo and in vitro[18,19]. We examined whether proliferation of SIPS cells were also stimulated by serum and PDGF-BB. Treatment of the cells with FBS stimulated proliferation in a dose-dependent manner; serum-induced proliferation was significant at as low as 1% (P < 0.05) (Figure 4). In addition, PDGF-BB stimulated proliferation of SIPS cells; PDGF-BB (at 25 ng/ml) induced proliferation by approximately three fold in serum-free medium (Figure 4).
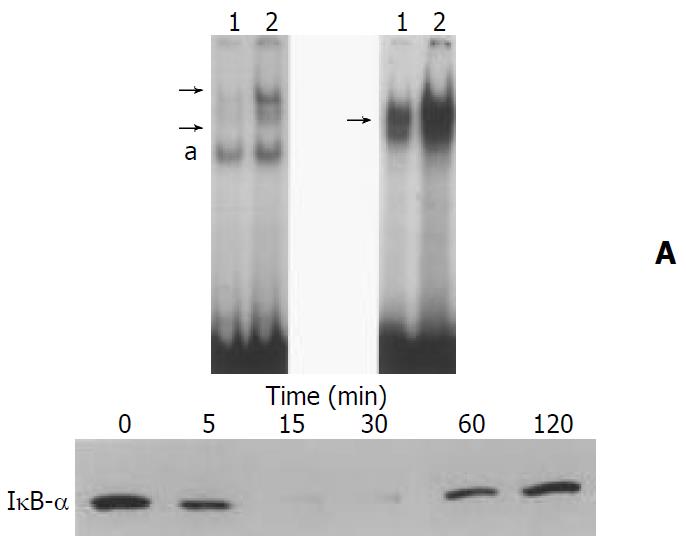
We have previously shown that proinflammatory cytokines IL-1β and tumor necrosis factor-α activated transcription factors NF-κB and AP-1 in primary PSCs[7,8]. We examined whether IL-1β activated these transcription factors in SIPS cells. Nuclear extracts were prepared from SIPS cells treated with IL-1β for 1 hour, and specific binding activities of NF-κB and AP-1 were assessed by electrophoretic mobility shift assay. IL-1β increased NF-κB and AP-1 binding activities (Figure 5A, B). The specificity of these binding activities was confirmed by competition assays using 100-fold excess of unlabeled oligonucleotides (data not shown). Phosphorylation and degradation of IκB-α is necessary for the activation of NF-κB[21]. We examined the effects of IL-1β on the cellular IκB-α levels by Western blotting. IL-1β induced transient degradation of IκB-α, further supporting that IL-1β activated NF-κB (Figure 5C).
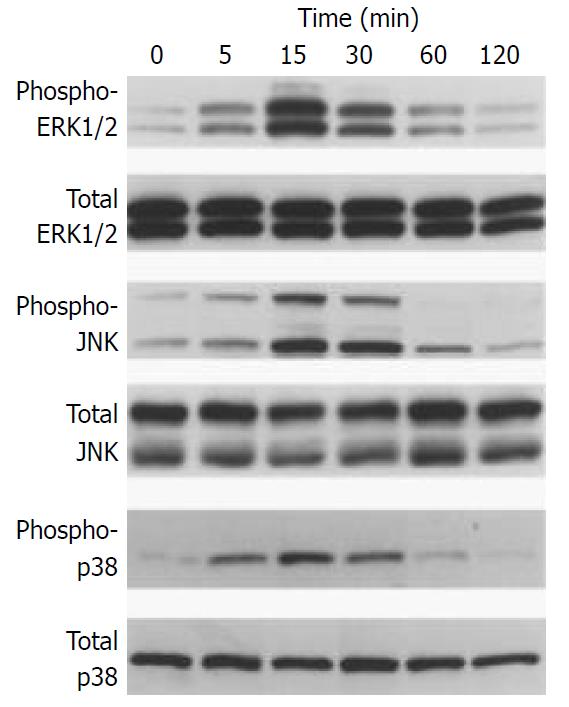
Induction of the expression of AP-1 components c-Fos and c-Jun by a variety of stimuli such as growth factors and cytokines was mediated by the activation of three distinct MAP kinases: extracellular signal-regulated kinase (ERK) 1/2, c-Jun N-terminal kinase (JNK), p38 MAP kinase[22]. Because the activation of these kinases occurred through phosphorylation, we examined whether IL-1β activated these MAP kinases in SIPS cells by Western blotting using anti-phosphospecific MAP kinase antibodies. These antibodies recognized only phosphorylated form of MAP kinases, thus allowing the assessment of activation of these kinases. IL-1β activated these three classes of MAP kinases in a time-dependent manner, peaking from 5 to 15 minutes (Figure 6). The levels of total MAP kinases were unaffected by the treatment, indicating that the lanes had been equally loaded.
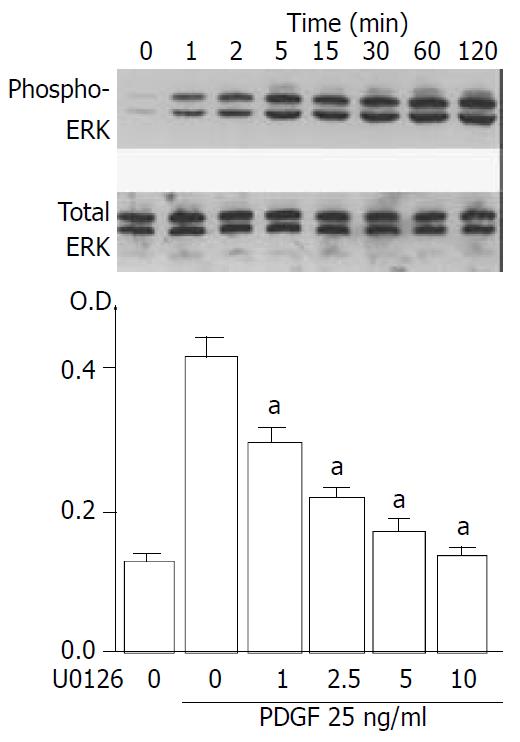
We and others have shown that activation of ERK plays key roles in the PDGF-induced proliferation of PSCs[20,23]. We examined whether PDGF-BB activated ERK in PSCs. PDGF- BB activated ERK1/2 in a time-dependent manner (Figure 7A). U0126, a specific MAP kinase kinase inhibitor[24], inhibited PDGF-induced proliferation in a dose-dependent manner (Figure 7B). Thus, activation of ERK plays a central role in the proliferation of SIPS, as is the case for primary PSCs.
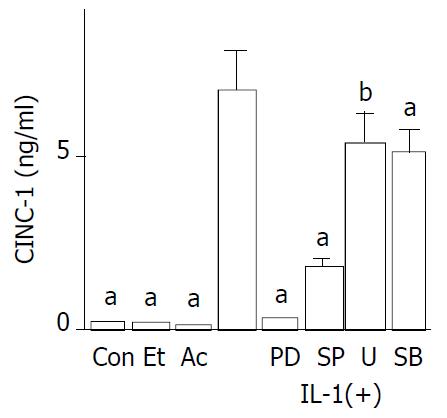
Activated PSCs acquire the proinflammatory phenotype; they may modulate the recruitment and activation of inflammatory cells through the expression of monocyte chemoattractant protein-1[7] and intercellular adhesion molecule-1[8]. Monocyte chemoattractant protein-1 is a C-C chemokine and potent mononuclear cell chemoattractant. CINC-1, a C-X-C chemokine, is a rat homologue of IL-8, and a potent neutrophil attractant[25]. It remained unknown whether primary PSCs expressed CINC-1. We examined whether SIPS cells express CINC-1 in response to IL-1β by enzyme immunoassay. SIPS cells constitutively produced CINC-1 at very low levels. IL-1β significantly induced the production of CINC-1 (Figure 8). Ethanol and acetaldehyde at clinically relevant concentrations failed to induce CINC-1 production. To elucidate the roles of NF-κB and MAP kinases for the expression of CINC-1 in SIPS cells, we used specific inhibitors to block these pathways. First, we treated SIPS cells with IL-1β in the presence of pyrrolidine dithiocarbamate (PDTC), a specific inhibitor of NF-κB activation[26]. As shown in Figure 8, PDTC decreased the IL-1β-induced CINC-1 production to near the basal levels. SP600125 is a reversible ATP-competitive inhibitor of JNK that inhibits c-jun phosphorylation and the expression of proinflammatory genes such as IL-2, and tumor necrosis factor-α[27]. SP600125 at 10 μM decreased the IL-1β-induced CINC-1 production approximately by 75%. We next examined the effects of U0126[24], a specific inhibitor of MAP kinase kinase activation, which prevents the activation of ERK1/2. U0126 at 10 μM partially inhibited inducible CINC-1 expression. A selective p38 MAP kinase inhibitor, SB202190[28], at 25 μM also partially inhibited inducible CINC-1 production. Similar results were obtained with tumor necrosis factor-α-induced CINC-1 expression (data not shown). In these experiments, the inhibitors at the indicated concentrations did not affect the cell viability during the incubation as assessed by trypan blue exclusion test (data not shown). However, at higher concentrations, some cytotoxic effects were observed during the incubation. These results suggested that activation of NF-κB and JNK plays a key role in inducible CINC-1 expression in SIPS cells. Activation of ERK and p38 MAP kinase pathways is partially required for optimal CINC-1 expression.
In response to pancreatic injury or inflammation, PSCs undergo a transformation from quiescent cells to activated, proliferating myofibroblast-like cells, which produce cytokines and extracellular matrix proteins. It has been established that activated PSCs play an important role in the pathogenesis of pancreatic fibrosis and inflammation[3,4,8]. Although primary stellate cell culture is a useful tool for studying molecular mechanisms of pancreatic fibrosis and inflammation in vitro, their isolation is time-consuming, yields are relatively low, and there is considerable heterogeneity between preparations. In addition, primary cells can be subcultured only several times because of their limited growth potential. To circumvent these problems, we have established and validated a new rat PSC line, named SIPS. This SIPS cell line has been developed through spontaneous immortalization, and can be passaged indefinitely compared with the limited number of passages for primary PSCs. SIPS cells have been passaged repeatedly without showing any evidence of senescence. Indeed, SA-β-Gal, a biomarker of senescent cells[13], was not detected in SIPS cells. SIPS cells retained the morphologic characteristics of primary PSCs as well as the expression of the cytoskeletal proteins α-SMA and glial acidic fibrillary protein. SIPS cells maintained the functional characteristics of primary PSCs; SIPS cells showed positive staining for type I collagen, fibronectin, and prolyl hydroxylases. Proliferation of PSCs was stimulated by FBS and PDGF-BB. SIPS cells responded to IL-1β, resulting in the activation of NF-κB, AP-1, and MAP kinases. In addition, SIPS cells exhibited proinflammatory response; SIPS cells expressed CINC-1 in response to IL-1β. Thus, SIPS cells retain several aspects of the primary and culture-activated PSCs.
We have previously established an immortalized cell line of rat PSCs, named SAM-K, by the introduction of the simian virus 40 T antigen[10]. Although SAM-K cells were found to be useful for establishment of stable transfectants, it was also shown that large T antigen led to the alternation of genome such as p53 expression[10]. The resulting genetic manipulations might limit the use of SAM-K cells for studies like defining genetic changes that occur during cell differentiation and transformation. In this study, we examined the expression of p53 and telomerase activity, both of which are shown to be associated with immortalization of mammalian cells[16,17]. We found that p53 expression and telomerase activity was negative in SIPS cells as is the case for primary PSCs. This is in striking contrast to SAM-K cells, where p53 expression and telomerase activity were high. These results suggest that different mechanisms involved for immortalization of SIPS and SAM-K cells, and that SIPS cells have more similar phenotype to primary PSCs than SAM-K cells do. Obviously, further studies are necessary to clarify the molecular mechanisms responsible for immortalization of SIPS cells.
To our knowledge, this is the first report describing the establishment of stellate cell line of the pancreas by spontaneous immortalization. In culture, PSCs are morphologically very similar to the hepatic stellate cells. To date, several hepatic stellate cell lines have been established by spontaneous immortalization. Greenwel et al[29] reported the characterization of two rat hepatic stellate cell lines, one from normal and the other from cirrhotic liver. Although both cell lines resembled primary cultures of hepatic stellate cells, significant differences in cell proliferation and IL-6 production between the two cell lines were found. Sauvant et al[30] reported that immortalized rat hepatic stellate cells were able to convert retinol into retinoic acid. Rodent cells are known to undergo spontaneous immortalization with a frequency of 10-5–10-6 that makes isolation of immortal cell lines from rodent populations experimentally practical even without transfer of an oncogene, whereas the spontaneous immortalization of human cells is a very rare event; the frequency is thought to be less than 10-12[31]. Schnabl et al[32] reported immortal activated human hepatic stellate cells generated by ectopic telomerase expression. They showed that activated human hepatic stellate cells had little, if any, detectable telomerase activity. Telomerase-induced hepatic stellate cells did not undergo oncogenic transformation and showed morphologic characteristics of activated stellate cells. In addition, mRNA expression in telomerase-positive cells and -negative cells were very similar. It would be of particular interest to see if human PSC line could be established by the introduction of ectopic telomerase expression.
Proliferation of PSCs is a fundamental feature of pancreatic fibrosis. PDGF has been shown to be the most potent mitogen for PSCs in vitro[18,19]. PDGF-BB stimulated proliferation of SIPS, and the stimulation was abolished in the presence of U126, a MAP kinase kinase inhibitor[24]. This is in agreement with the previous studies showing that ERK is a key mediator of mitogenic signals in rat PSCs[20,23].
Activated PSCs acquire the proinflammatory phenotype; they may modulate the recruitment and activation of inflammatory cells. We have shown that proinflammatory cytokines such as IL-1β and tumor necrosis factor-α induced expression of monocyte chemoattractant protein-1 and intercellular adhesion molecule-1 in primary PSCs[7,8]. In addition, we here showed for the first time that IL-1β induced CINC-1 expression in SIPS cells. CINC-1 production in response to IL-1β was also observed in primary PSCs (Satoh et al manuscript in preparation). Although it has been shown that hepatic stellate cells express CINC-1 both in vivo and in vitro[33], whether PSCs expressed CINC-1 and its regulatory mechanisms remained unknown. In this study, inducible CINC-1 production was abolished by PDTC, a specific inhibitor of NF-κB activation, and strongly decreased by SP600125, an inhibitor of JNK. Inhibition of ERK pathway by U0126 and of p38 MAP kinase by SB202190 partially inhibited IL-1β-induced CINC-1 production. Collectively, activation of NF-κB and JNK plays a key role, and that of ERK and p38 MAP kinase plays a partial role for optimal CINC-1 expression in SIPS cells. This is in agreement with the regulatory mechanisms of IL-8, a human homologue of CINC-1[34]. Maximal IL-8 amounts are generated by a combination of three different mechanisms: first, de-repression of the gene promoter; second, transcriptional activation of the gene by NF-κB and JNK pathways; and third, stabilization of the mRNA by the p38 MAP kinase pathway. In addition, activation of ERK pathway contributes to IL-8 expression[34]. Similar to PSCs[35], ethanol and acetaldehyde at clinically relevant concentrations activated ERK, JNK and p38 MAP kinase (data not shown), but failed to induce CINC-1 expression in SIPS cells. Thus, activation of MAP kinases is required, but not sufficient for optimal CINC-1 expression in SIPS cells. We have previously shown that ethanol and acetaldehyde induced type I collagen gene expression through p38 MAP kinase in primary PSCs[35]. Further studies are necessary to clarify whether ethanol and acetaldehyde induce the collagen gene expression in a similar manner.
In summary, SIPS cells are a newly established PSC line morphologically, phenotypically and functionally similar to primary, activated PSCs. Unlike SAM-K cells, immortalization was not associated with elevated p53 expression or telomerase activity. SIPS cells can be used for both transient and stable transections (Masamune et al unpublished observation), facilitating the overexpression of ectopic genes. Its phenotypic characteristics as well as its responsiveness to proinflammatory cytokines and growth factors make it a useful tool for investigation of the pathogenesis of pancreatic inflammation and fibrosis and thereby for future therapeutic development.
A.M. and M.S. equally contributed to this work
Edited by Ma JY
| 1. | Etemad B, Whitcomb DC. Chronic pancreatitis: diagnosis, classification, and new genetic developments. Gastroenterology. 2001;120:682-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 859] [Cited by in RCA: 758] [Article Influence: 31.6] [Reference Citation Analysis (1)] |
| 2. | Lankisch PG. Natural course of chronic pancreatitis. Pancreatology. 2001;1:3-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 110] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 3. | Apte MV, Haber PS, Applegate TL, Norton ID, McCaughan GW, Korsten MA, Pirola RC, Wilson JS. Periacinar stellate shaped cells in rat pancreas: identification, isolation, and culture. Gut. 1998;43:128-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 719] [Cited by in RCA: 716] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 4. | Bachem MG, Schneider E, Gross H, Weidenbach H, Schmid RM, Menke A, Siech M, Beger H, Grünert A, Adler G. Identification, culture, and characterization of pancreatic stellate cells in rats and humans. Gastroenterology. 1998;115:421-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 744] [Cited by in RCA: 798] [Article Influence: 29.6] [Reference Citation Analysis (0)] |
| 5. | Friedman SL. Molecular regulation of hepatic fibrosis, an integrated cellular response to tissue injury. J Biol Chem. 2000;275:2247-2250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1567] [Cited by in RCA: 1597] [Article Influence: 63.9] [Reference Citation Analysis (0)] |
| 6. | Haber PS, Keogh GW, Apte MV, Moran CS, Stewart NL, Crawford DH, Pirola RC, McCaughan GW, Ramm GA, Wilson JS. Activation of pancreatic stellate cells in human and experimental pancreatic fibrosis. Am J Pathol. 1999;155:1087-1095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 323] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 7. | Masamune A, Kikuta K, Satoh M, Sakai Y, Satoh A, Shimosegawa T. Ligands of peroxisome proliferator-activated receptor-gamma block activation of pancreatic stellate cells. J Biol Chem. 2002;277:141-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 109] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 8. | Masamune A, Sakai Y, Kikuta K, Satoh M, Satoh A, Shimosegawa T. Activated rat pancreatic stellate cells express intercellular adhesion molecule-1 (ICAM-1) in vitro. Pancreas. 2002;25:78-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 51] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Masamune A, Satoh M, Kikuta K, Sakai Y, Satoh A, Shimosegawa T. Inhibition of p38 mitogen-activated protein kinase blocks activation of rat pancreatic stellate cells. J Pharmacol Exp Ther. 2003;304:8-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 77] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 10. | Satoh M, Masamune A, Sakai Y, Kikuta K, Hamada H, Shimosegawa T. Establishment and characterization of a simian virus 40-immortalized rat pancreatic stellate cell line. Tohoku J Exp Med. 2002;198:55-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Masamune A, Shimosegawa T, Kimura K, Fujita M, Sato A, Koizumi M, Toyota T. Specific induction of adhesion molecules in human vascular endothelial cells by rat experimental pancreatitis-associated ascitic fluids. Pancreas. 1999;18:141-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Masamune A, Satoh K, Sakai Y, Yoshida M, Satoh A, Shimosegawa T. Ligands of peroxisome proliferator-activated receptor-gamma induce apoptosis in AR42J cells. Pancreas. 2002;24:130-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 42] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Dimri GP, Lee X, Basile G, Acosta M, Scott G, Roskelley C, Medrano EE, Linskens M, Rubelj I, Pereira-Smith O. A biomarker that identifies senescent human cells in culture and in aging skin in vivo. Proc Natl Acad Sci USA. 1995;92:9363-9367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5281] [Cited by in RCA: 5768] [Article Influence: 192.3] [Reference Citation Analysis (0)] |
| 14. | Porstmann T, Ternynck T, Avrameas S. Quantitation of 5-bromo-2-deoxyuridine incorporation into DNA: an enzyme immunoassay for the assessment of the lymphoid cell proliferative response. J Immunol Methods. 1985;82:169-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 146] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 15. | Masamune A, Igarashi Y, Hakomori S. Regulatory role of ceramide in interleukin (IL)-1 beta-induced E-selectin expression in human umbilical vein endothelial cells. Ceramide enhances IL-1 beta action, but is not sufficient for E-selectin expression. J Biol Chem. 1996;271:9368-9375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 60] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 16. | Banerjee A, Srivatsan E, Hashimoto T, Takahashi R, Xu HJ, Hu SX, Benedict WF. Immortalization of fibroblasts from two patients with hereditary retinoblastoma. Anticancer Res. 1992;12:1347-1354. [PubMed] |
| 17. | Liu JP. Studies of the molecular mechanisms in the regulation of telomerase activity. FASEB J. 1999;13:2091-2104. [PubMed] |
| 18. | Apte MV, Haber PS, Darby SJ, Rodgers SC, McCaughan GW, Korsten MA, Pirola RC, Wilson JS. Pancreatic stellate cells are activated by proinflammatory cytokines: implications for pancreatic fibrogenesis. Gut. 1999;44:534-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 474] [Cited by in RCA: 484] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 19. | Luttenberger T, Schmid-Kotsas A, Menke A, Siech M, Beger H, Adler G, Grünert A, Bachem MG. Platelet-derived growth factors stimulate proliferation and extracellular matrix synthesis of pancreatic stellate cells: implications in pathogenesis of pancreas fibrosis. Lab Invest. 2000;80:47-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 151] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 20. | Masamune A, Kikuta K, Satoh M, Kume K, Shimosegawa T. Differential roles of signaling pathways for proliferation and migration of rat pancreatic stellate cells. Tohoku J Exp Med. 2003;199:69-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 67] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 21. | Grilli M, Chiu JJ, Lenardo MJ. NF-kappa B and Rel: participants in a multiform transcriptional regulatory system. Int Rev Cytol. 1993;143:1-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 676] [Cited by in RCA: 741] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 22. | Karin M, Liu Zg, Zandi E. AP-1 function and regulation. Curr Opin Cell Biol. 1997;9:240-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2004] [Cited by in RCA: 2076] [Article Influence: 74.1] [Reference Citation Analysis (0)] |
| 23. | Jaster R, Sparmann G, Emmrich J, Liebe S. Extracellular signal regulated kinases are key mediators of mitogenic signals in rat pancreatic stellate cells. Gut. 2002;51:579-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 114] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 24. | Favata MF, Horiuchi KY, Manos EJ, Daulerio AJ, Stradley DA, Feeser WS, Van Dyk DE, Pitts WJ, Earl RA, Hobbs F. Identification of a novel inhibitor of mitogen-activated protein kinase kinase. J Biol Chem. 1998;273:18623-18632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2416] [Cited by in RCA: 2560] [Article Influence: 94.8] [Reference Citation Analysis (0)] |
| 25. | Watanabe K, Koizumi F, Kurashige Y, Tsurufuji S, Nakagawa H. Rat CINC, a member of the interleukin-8 family, is a neutrophil-specific chemoattractant in vivo. Exp Mol Pathol. 1991;55:30-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 102] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 26. | Schreck R, Meier B, Männel DN, Dröge W, Baeuerle PA. Dithiocarbamates as potent inhibitors of nuclear factor kappa B activation in intact cells. J Exp Med. 1992;175:1181-1194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1186] [Cited by in RCA: 1228] [Article Influence: 37.2] [Reference Citation Analysis (0)] |
| 27. | Bennett BL, Sasaki DT, Murray BW, O'Leary EC, Sakata ST, Xu W, Leisten JC, Motiwala A, Pierce S, Satoh Y. SP600125, an anthrapyrazolone inhibitor of Jun N-terminal kinase. Proc Natl Acad Sci USA. 2001;98:13681-13686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2085] [Cited by in RCA: 2168] [Article Influence: 90.3] [Reference Citation Analysis (0)] |
| 28. | Lee JC, Laydon JT, McDonnell PC, Gallagher TF, Kumar S, Green D, McNulty D, Blumenthal MJ, Heys JR, Landvatter SW. A protein kinase involved in the regulation of inflammatory cytokine biosynthesis. Nature. 1994;372:739-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2614] [Cited by in RCA: 2664] [Article Influence: 85.9] [Reference Citation Analysis (0)] |
| 29. | Greenwel P, Schwartz M, Rosas M, Peyrol S, Grimaud JA, Rojkind M. Characterization of fat-storing cell lines derived from normal and CCl4-cirrhotic livers. Differences in the production of interleukin-6. Lab Invest. 1991;65:644-653. [PubMed] |
| 30. | Sauvant P, Sapin V, Abergel A, Schmidt CK, Blanchon L, Alexandre-Gouabau MC, Rosenbaum J, Bommelaer G, Rock E, Dastugue B. PAV-1, a new rat hepatic stellate cell line converts retinol into retinoic acid, a process altered by ethanol. Int J Biochem Cell Biol. 2002;34:1017-1029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 31. | Hopfer U, Jacobberger JW, Gruenert DC, Eckert RL, Jat PS, Whitsett JA. Immortalization of epithelial cells. Am J Physiol. 1996;270:C1-11. [PubMed] |
| 32. | Schnabl B, Choi YH, Olsen JC, Hagedorn CH, Brenner DA. Immortal activated human hepatic stellate cells generated by ectopic telomerase expression. Lab Invest. 2002;82:323-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 92] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 33. | Maher JJ, Lozier JS, Scott MK. Rat hepatic stellate cells produce cytokine-induced neutrophil chemoattractant in culture and in vivo. Am J Physiol. 1998;275:G847-G853. [PubMed] |
| 34. | Hoffmann E, Dittrich-Breiholz O, Holtmann H, Kracht M. Multiple control of interleukin-8 gene expression. J Leukoc Biol. 2002;72:847-855. [PubMed] |
| 35. | Masamune A, Kikuta K, Satoh M, Satoh A, Shimosegawa T. Alcohol activates activator protein-1 and mitogen-activated protein kinases in rat pancreatic stellate cells. J Pharmacol Exp Ther. 2002;302:36-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 85] [Article Influence: 3.7] [Reference Citation Analysis (0)] |