Published online Oct 15, 2000. doi: 10.3748/wjg.v6.i5.664
Revised: August 11, 2000
Accepted: September 11, 2000
Published online: October 15, 2000
AIM: To observe the drug sensitizing effect and related mechanisms of fas gene transduction on human drug-resistant gastric cancer cell SGC7901/VCR (resistant to Vincristine).
METHODS: The cell cycle alteration was observed by FACS. The sensitivity of gastric cancer cells to apoptosis was determined by in vitro apoptosis assay. The drug sensitization of cells to several anti-tumor drugs was observed by MTT assay. Immunochemical method was used to show expression of P-gp and Topo II in gastric cancer cells.
RESULTS: Comparing to SGC7901 and pBK-SGC7901/VCR, fas-SGC7901/VCR showed decreasing G2 cells and increasing S cells, the G2 phase fraction of pBK-SGC7901/VCR was about 3.0 times that of fas-SGC7901/VCR, but S phase fraction of fas-SGC7901/VCR was about 1.9 times that of pBK-SGC7901/VCR, indicating S phase arrest of fas-SGC7901/VCR. FACS also suggested apoptosis of fas-SGC7901/VCR. fas-SGC7901/VCR was more sensitive to apoptosis inducing agent VM-26 than pBK-SGC7901/VCR. MTT assay showed increased sensitization of fas-SGC7901/VCR to DDP, MMC and 5-FU, but same sensitization to VCR according to pBK-SGC7901/VCR. SGC7901, pBK-SGC7901/VCR and fas-SGC7901/VCR had positively stained Topo II equally. P-gp staining in pBK-SGC7901/VCR was stronger than in SGC7901, but there was little staining of Pgp in fas-SGC7901/VCR.
CONCLUSION: fas gene transduction could reverse the MDR of human drug-resistant gastric cancer cell SGC7901/VCR to a degree, possibly because of higher sensitization to apoptosis and decreased expression of P-gp.
- Citation: Yin F, Shi YQ, Zhao WP, Xiao B, Miao JY, Fan DM. Suppression of P-gp induced multiple drug resistance in a drug resistant gastric cancer cell line by overexpression of Fas. World J Gastroenterol 2000; 6(5): 664-670
- URL: https://www.wjgnet.com/1007-9327/full/v6/i5/664.htm
- DOI: https://dx.doi.org/10.3748/wjg.v6.i5.664
Multidrug resistance (MDR), the principal mechanism by which many cancers develop resistance to chemotherapeutic drugs, is a major factor in the failure of many forms of chemotherapy[1]. It affects patients with a variety of blood cancers and solid tumors, including breast, ovarian, lung and lower gastrointestinal tract cancers.
Tumors usually consist of mixed populations of malignant cells, some of which are drug sensitive while others are drug resistant. Chemotherapy kills drug sensitive cells, but may leave behind a high proportion of drug resistant cells. As the tumor begins to grow again, chemotherapy may fail because the remaining tumor cells are now resistant to it.
Resistance to therapy has been correlated to the presence of at least two molecular ‘pumps’ that actively expel chemotherapeutic drugs from the tumor cells. This action thus spares tumor cells from the effects of the drug, which has to actinside the cell at the nucleus or the cytoplasm. The two pumps commonly found to confer chemoresistance in cancer are P-glycor protein (P-gp) and the so-called multidrug resistance-associated protein (MRP). But they are not the complete story, and can not explicate the phenomenon of MDR fully.
Recent studies indicate that some cancer cells are resistant to signals of apoptosis and so making cell life longer might be an important part of MDR mechanisms.
In this study, we assumed that inducing apoptosis in drug resistant tumors might reverse MDR. So we transfected fas gene, which is a key molecule in the signal transduction pathway of apoptosis, into drug resistant gastric cancer cells, and observed the expression of target genes in transfectants and the sensitivity of transfectants to chemotherapeutic agents in order to find the pathway of signal transduction for reversing gastric cancer MDR.
Gastric cancer cell line SGC7901, pBK-SGC7901/VCR (SGC7901/VCR is transfected by pBK-CMV expression vectors persistently), pBK-fas cDNA (1.83 kb full length fas cDNA, was inserted into pBK-CMV expression vectors), and fas-SGC7901/VCR cell transfectants (SGC7901/VCR is transfected by pBK-fas-expression vectors persistently) were kept in our department. Chemical reagents were obtained from Sigma, except as noted. Chemical reagents including PMSF, SDS, and avidin-biotin peroxidase complex (ABC) kit were obtained from SABC and Promega. P-gp mouse IgG antibody and topoisomerase II (Topo II) mouse IgG antibody were kindly given by Dr. Liu. All the antibodies and rabbit anti-human Fas polyclonal antibody were products of Dako. RPMI1640 was obtained from GIBCO, fetal bovine serum from HYCLON E, mitomycin C (MMC) from Kyowa Hakko Kogyo Co. Ltd, vincristine (VCR) and doxorubin (Dox) from the Twelfth Shanghai Pharmaceutical Product Factory, 5-fluorouracil (5-FU) from Shanghai Xudong Pharmaceutical Company, and cisplatinum (DDP) from Shandong Qilu Pharmaceutical Product Factory.
Western blot analysis Cells in log phase were harvested and washed with PBS twice, then lyzed in lysis buffer (150 mmol/L Tris-Cl pH8.0; 50 mmol/L NaCl; 0.2 mmol/L EDTA; 0.1 mmol/L PMSF; 10 g/L NP-40). SDS-PAGE was performed using 100 μg or 150 μg total protein per lane, one electrophoresis gel was stained with commassie brilliant blue R-250, another was blotted to nitrocellular filter. After blocking with 50 g/L defatted milk, the filter was incubated with rabbit anti-human Fas polyclonal antibody overnight at 4 °C, then washed three times 5 min each time with TBS and incubated with HRP-conjugated goat anti-rabbit IgG at 37 °C for 30 min. Finally, the positive bands were visualized by incubation with peroxidase substrate solution D iaminobenzidine (DAB).
Cell culture MDR gastric cancer cell subline SGC7901/VCR was induced by pulse treatment of the parent cell line SGC7901 at a single dose of Vincristine. Having been exposed to 1.0 mg/L Vincristine for one hour, SGC7901 cells were replated in drug-free culture medium to allow exponential growth of cells to be recovered prior to another stimulation. Once stable resistant phenotype was developed, the SGC7901/VCR cells were grown in drug free growth medium.
Cytotoxity assay Dose-survival curves defining the sensitivity of gastric cancer cell line SGC7901, pBK-SGC7901/VCR and fas-SGC7901/VCR cell transfectants to VCR, DDP, MMC, Dox and 5-FU were obtained using MTT cytotoxic assay. Cells in log growth period (3-4) × 107/L diluted with 200 μL RPMI 1640 supplemented with 100 mL/L fetal bovine serum were seeded into 96-well plates in triplicate for each treatment, after culturing for 12 h, added Dox (0.1, 1, 10 and 100 μg), DDP (0.1, 1, 10 and 100 μg), 5-FU (0.7, 7, 70 and 700 μg), MMC (0.1, 1.0, 10 and 100 μg) and VCR (0.1, 1.0, 10 and 100 μg) according to the clinically established plasma peak concentration. Three days later, 20 μL MTT solution (5 g/L) was put into plates, and then the supernatant was discarded after 4 h, 150 μL DMSO was added to melt crystal. A value was read at 590 nm wavelength.
FACS analysis Cells (3-4) × 107/L were seeded in 25 cm2 tissue culture flasks for 36 h-40 h, after reaching log growth, cells were digested by 2.5 g/L trypsin and harvested by centrifugation. Then the cells were fixed with ethanol and stained with propidum iodide, and subjected to fluorescence-activated cell sorting (FACS) analysis for DNA content at the Fourth Military Medical University.
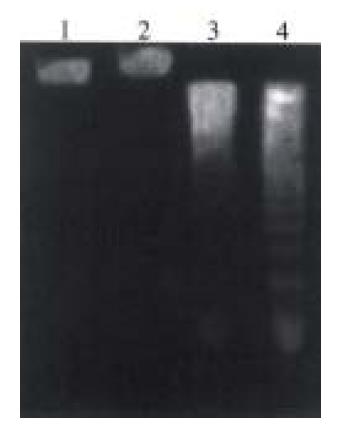
In vitro apoptosis assay Cells (3-4) × 107/L were seeded in 25 cm2 tissue culture flasks and allowed to reach log growth for 36 h-40 h. After exposure to apoptosis inductor VM-26 for 24 h at two different doses 1.25 μmol/L and 2.5 μmol/L, subsequently culture the cells in RPMI 1640 supplemented with 100 mL/L fetal bovine serum containing no VM-26 for 48 h, then harvest the cells for genomic DNA extraction, and electro phoresis in 10 g/L agarose gel at 50 V for 1 h[2].
Immunocytochemistry Tissue immunocytochemical staining was done with the ABC kit. Cells (3-4) × 107/L were seeded in a glass slide in 100 g/L RPMI 1640. After the cells attached tightly to the slides, and reached log growth for 36 h-48 h, slides were washed with PBS for 3-5 min, then immersed in 40 g/L paraformaldehyde phosphated buffer solution for 5-10 min. Slides were immersed for 45 min in 3 mL/L peroxide in methanol (to deplete endoge nous peroxidase) and normal goat serum diluted to 1:100 in PBS for 20 min. Primary antibodies against P-gp, Topo II and control normal mouse serum were used at dilution of 1:100, applied to cell attached slides and incubated in a humidified chamber at a room temperature for 30 min and 4 °C overnight. The slides were then washed with PBS for 10 min. Biotinylated goat anti-mouse IgG was applied on to the cell sections, and incubated at room temperature for 30 min. After washing with PBS for 10min, these tissues were incubated with avidin DH-Biotinylated peroxidase for 45 min. Finally, color was developed by immersion of the sections in a peroxidase substrate solution DAB.
For each slide, the extent and intensity of staining with P-gp and Topo II antibody was graded on a scale of 0-4+ by a blinded observer on two separate occasions using coded slides, and an average score was calculated. The observer assessed all tissues on the slides to assign the scores. A 4+ grade implied that all staining was maximally intense throughout the specimen, while 0 implied that staining was absent throughout the specimen.
SDS-PAGE (Figure 1A) showed no significant differences between fas-SGC7901/VCR protein and that of pBK-SGC7901/VCR control cells. Western blot (Figure 1B) indicated a weak band of Mr36000-40000 in lane 3 which is consistent with Mr of Fas protein, when 150 μg total protein of pBK-SGC7901/VCR was loaded, while lanes 4 and 5 of fas transfectants had strong positive band of Mr 36000-40000 respectively, the band of lane 4 was slightly weaker than that of lane 5 because of quantity of loading.
As shown in Figure 2, fas-SGC7901/VCR cell transfectants were more sensitive to MMC, DDP and 5-FU. The survival rates of transfectants treated with VCR and Dox were only lowered slightly, compared with non-transfectants, which showed that fas-SGC7901/VCR cell transfectants remained resistant to VCR and Dox.
By using FCM to analyze cell cycle, the apoptotic peak appeared only in fas-SGC7901/VCR cell transfectants and there were no significant differences between them in G1 phase. These data show that Fas takes part in induction of apoptosis and differentiation of gastric cancer cells. Analysis of cell cycle distribution demonstrated that the fraction number of fas-SGC7901/VCR cells in G1/0 phase, G2 and S phase was about 0.70, 0.06 and 0.24, that of pBK-SGC7901/VCR was about 0.67, 0.17 and 0.13 respectively, and the G2 phase fraction of pBK.SGC7901/VCR was about 3.0 times that of fas-SGC7901/VCR, but S phase fraction of fas-SGC7901/VCR was about 1.9 times that of pBK-SGC7901/VCR, indicating S phase arrest of fas-SGC7901/VCR (Table 1).
| Cell line | G1 | G2 | S | G1/G2 |
| SGC7901 | 0.73 | 0.11 | 0.16 | 0.188 |
| pBK-SGC7901/VCR | 0.67 | 0.17 | 0.13 | 0.186 |
| fas-SGC7901/VCR | 0.70 | 0.06 | 0.24 | 0.190 |
As shown in Figure 3, fas-SGC7901/VCR cell transfectants remained sensitive to VM-26, and characteristic DNA ladder bands of apoptosis appeared.
In order to assess whether the overexpression of Fas in drug resistant gastric cancer cell line SGC7901/ VCR involved inhibition of other MDR inducing factors except induction of apoptosis, we detected topoisomerase II (Topo II) and P-gp protein expression in these cell lines by immunocytochemistry. There was no difference in the expression of Topo II among SGC7901, pBK-SGC7901/VCR and fas-SGC7901/VCR. All these had positive staining of Topo II, and an average score of about 2+ grades was calculated. P-gp staining on pBK-SGC7901/VCR was stronger than that on SGC7901, and scored a grade of 4+. But there was weak staining of P-gp on fas-SGC7901/VCR (Figure 4). These data suggested that Fas proteins increased sensitivity of drug resistant gastric cancer cell line SGC7901/VCR to chemotherapeutic drugs may be through decreasing P-gp protein.
Apoptosis is an important and well-controlled form of cell death that occurs under a variety of physiological and pathological conditions. This process has been recognized to be of major importance for embryonic development, tissue homeostasis, neurodegeneration, autoimmune diseases, AIDS, carcinogenesis, cancer pro gression, specially for killing cancer cells induced by chemotherapeutic drugs[3-9]. Once the apoptosis program is activated, it starts with blebbing of the membrane, followed by degradation of the chromosomal DNA by nucleases, resulting in condensation and fragmentation, finally, phagocytes remove cell fragments without causing any inflammatory reaction. Some proto-oncogenes and tumor suppressor genes can regulate apoptosis[10-18] and there are also accumulated evidences which show that these apoptosis regulating genes are important for the development of digestive system[19-24].
Multidrug resistance represents a major obstacle in the successful therapy of neoplastic diseases. Studies have demonstrated that this form of drug resistance occurs both in cultured tumor cell lines as well as in human cancers. Recent studies indicate that genes that regulate apoptotic cell death might play an important role in determining the sensitivity of tumor cells to chemotherapy. Many chemotherapeutic agents are found to act through damaging DNA or regulating apoptosis related genes p53, c-myc, bcl-2, bax, p21, c-H-ras to trigger apoptosis[25-28].
Strobel et al[29] found that SW626 cells overexpressing BAX aresens itized to the cytotoxic effects of alkaloid derivatives such as paclitaxel and Vincristine, and demonstrate that these seemingly disparate effects are explained by an enhanced accumulation of paclitaxel in BAX-overexpressing cells, an effect due to diminished drug efflux. These data suggest that stable transfectants that overexpress BAX may be sensitized to apoptotic cell death through a novel mechanism involving the enhancement of intracellular levels of naturally occurring toxins. NicA mhlaoibh et al[30] used an in vitro model, the resistant variant, DLKP-SQ/10p derived from human lung carcinoma clonal cell line DLKP-SQ to 10 sequential pulses of pharmacologically attainable doses of doxorubicin, demonstrating that overexpression of the pro-apoptotic bcl-xS gene in the DLKP-SQ/10p line partially reversed resistance not only to P-gp-associated drugs, doxorubicin, but also to 5-fluorouracil, indicating that the ratio of bcl family members may be important in determining sensitivity to chemotherapeutic drug-induced apoptosis.
Recently mutated N-ras oncogene has been implicated in melanoma resistance to cisplatin, both in vitro and in vivo, and the role of two other oncogenes, bcl-2 and p53, which are already involved in the chemoresistance of hematological and solid malignancies. The finding that many chemotherapeutic agents can kill suscep tible cells through the apoptosis pathway provides new molecular insight into chemoresistance mechanisms and suggests that apoptosis and/or resistance to apoptosis of tumor cells should be investigated to clarify further the mechanism of tumor chemoresistance[31].
Anti-cancer drugs and cytotoxic cytokines such as members of the TNF/Fas-ligand family play a predominant role in apoptosis induction in tumor cells including gastric cancer[32,33]. And compared with normal tissues, malignant tumor cells, especially metastatic tumor cells present extremely lower expression of Fas, while most benign tumors are similar to their original tissues in the expression of Fas. It is hypothesized that malignant tumors might suppress Fas expression or lose Fas molecule in order to avoid the surveillance of Fas ligand. This explains the lack of Fas expression in drug resistant cells. Our laboratory found that Fas-antigen expression in human gastric cell line SGC79 01/VCR is lower than that of SGC7901, and it seems that the alteration of Fas expression following drug-resistance is not restricted to one cell type. Cai et al[34] also found that after being treated by anti-Fas in the presence of IFN-gamma, human breast carcinoma cell line MCF7/Adr (resistant to adriamycin) was resistant to Fas-mediated apoptosis, and this resistance was correlated with a loss of surface Fas-protein expression[35]. Furthermore, the down-regulation of Fas expression and subsequent resistance to anti-Fas were observed in other drug-resistant cancer cell lines including human ovarian-carcinoma IGR-OV1/VCR cells and leukemic lymphoblast CEM/VLB cells. But no evidence shows whether the down-regulation of Fas expression increases resistance to not only anti-Fas, but also to other chemotherapy drugs, and whether there is crosstalking between MDR signaling and Fas expression.
We investigated whether the CD95/CD95L system plays a role in this process. We used the human gastric cell line SGC7901, and its derivative SGC7901/VCR (induced by sequential pulses of high dose of VCR and resistant to VCR) to determine the impact of acquired chemotherapeutic drug and cytokine resistance on susceptibility to Fas-induced cytotoxicity.
CD95 (Fas/APO-1) is a death-promoting receptor that belongs to the tumor necrosis factor (TNF) receptor I family[36,37]. Triggering of the CD95 molecule by either agonistic antibodies or the natural ligand CD95L (FasL) induces apoptosis[38]. Ligand binding induces trimerization of CD95, and the trimerized cytoplasmic region then transduces the signal by recruiting a molecule called FADD (Fas-associating protein with death domain) or MORT1 (mediator of receptor-induced toxicity), which binds to CD95 via interaction of the death domain at its COOH terminus[39-43]. The NH2-terminal region of FADD is responsible for downstream signal transduction by recruitment of a prote in called FLICE (FADD-like interleukin-1β-converting enzyme [ICE]) or MACH (MORT1-associated CED-3 homologue), recently designated as caspase-8[44-46]. The NH2 terminus of caspase-8 binds to FADD/MORT1, while its COOH-terminal region is related to the caspase-3 (CPP32) subfamily. Therefore, FLICE/ MACH preferentially cleaves caspase-3 substrates such as poly (ADP) ribose polymerase (PARP)[45], and ICE proteases including CPP32[47].
In this study, there is evidence that Fas can increase sensitivity to the cytotoxic effects of therapeutic drugs through increasing cell arrests of S phase. MTT assays show that overexpression of Fas could increase sensitivity of gastric cancer cells, to the cytotoxic effects of topoisomerase II-directed chemotherapeutic agents such as VM-26, but not doxorubin. It is suggested that transduction of pro-apoptosis Fas gene into drug resistant cells is obviously helpful in increasing the drug sensitivity.
Considerable evidence has indicated that the multidrug transporter or P-glycoprotein plays a role in the development of simultaneous resistance to multiple cytotoxic drugs in cancer cells[48-50]. P-glycoprotein appears to act as an energy-dependent efflux pump to remove various natural product drugs from the cells before they have a chance to exert their cytotoxic effects. But expression of the MDR1 gene product has been associated with a poor prognosis in clinical studies. To obtain insight into the mechanism of drug resistance, the expression of P-170 glycoprotein as potentially able to contribute to drug resistance was investigated in these three kinds of cell lines by immunochemical technology. We found that P-glycoprotein (P-gp) is overexpressed in multidrug resistant human gastric cancer cell line SGC7901/VCR than SGC7901, but there was little expression of P-gp on fas-SGC7901/VCR.
These data suggest that stable transfectants that overexpress Fas may be sensitized to apoptotic cell death through a novel mechanism involving the enhancement of intracellular levels of naturally occurring toxins such as alkaloid der ivatives.
These results revealed that fas-gene transduction could reverse the MDR of h uman drug-resistant gastric cancer cell SGC7901/VCR to a degree, partly because of Fas induced decreased expression of P-gp.
Other observations suggest that P-gp may play a specific role in regulating some caspase-dependent apoptotic pathways, and there is a complicated cross talking between Fas and P-gp. Researchers found that classical multidrug resistant human CEM and K562 tumor cell lines expressing high levels of P-gp were less sensitive to multiple forms of caspase-dependent cell death, including that mediated by cytotoxic drugs and ligation of Fas, and inhibition of P-gp function also enhanced drug or Fas-mediated activation of caspase-3 in drug-resistant CEM cells[51].
In this study we have demonstrated that inducing apoptosis by fas transducti on correlates with the development of sensitivity to MMC, DDP, 5-FU to a degree, and Fas can repress P-gp through a series of cross-linked signal transduction. Therefore, apoptosis inducing gene products may not only increase sensitivity to the cytotoxic effects of chemotherapeutic agents by means of apoptosis, but also through other signal transduction. So gene therapy of introducing pro-apoptosis inducing gene may be a good method to overcome MDR in tumors. However, the mechanism of MDR is much complicated, and in tumors the drug resistance is multifactorial. Research to overcome this resistance should therefore be directed towards a combined treatment that eliminates all of these.
Edited by You DY Verified by Ma JY
| 1. | Arceci RJ. Tumor cell survival and resistance to therapy. Curr Opin Hematol. 1996;3:279-287. [PubMed] |
| 2. | Desjardins LM, MacManus JP. An adherent cell model to study different stages of apoptosis. Exp Cell Res. 1995;216:380-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 60] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Ashkenazi A, Dixit VM. Apoptosis control by death and decoy receptors. Curr Opin Cell Biol. 1999;11:255-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 975] [Cited by in RCA: 943] [Article Influence: 36.3] [Reference Citation Analysis (0)] |
| 4. | Steller H. Mechanisms and genes of cellular suicide. Science. 1995;267:1445-1449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1812] [Cited by in RCA: 1753] [Article Influence: 58.4] [Reference Citation Analysis (0)] |
| 5. | Jacobson MD, Weil M, Raff MC. Programmed cell death in animal development. Cell. 1997;88:347-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2027] [Cited by in RCA: 1949] [Article Influence: 69.6] [Reference Citation Analysis (0)] |
| 6. | Yet WC, Pompa JL, McCurrach ME, Shu HB, Elia AJ, Shahinian A, Ng M, Wakeham A, Khoo W, Mitchell K. FADD: Essential for embryo development and signaling from some, but not all, inducers of apop tosis. Science. 1998;279:1954-1958. |
| 7. | Nagata S. Apoptosis by death factor. Cell. 1997;88:355-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3739] [Cited by in RCA: 3644] [Article Influence: 130.1] [Reference Citation Analysis (0)] |
| 8. | Lowe SW, Ruley HE, Jacks T, Housman DE. p53-dependent apoptosis modulates the cytotoxicity of anticancer agents. Cell. 1993;74:957-967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2022] [Cited by in RCA: 2066] [Article Influence: 64.6] [Reference Citation Analysis (0)] |
| 9. | Thulasi R, Harbour DV, Thompson EB. Suppression of c-myc is a critical step in glucocorticoid-induced human leukemic cell lysis. J Biol Chem. 1993;268:18306-18312. [PubMed] |
| 10. | Harrington EA, Fanidi A, Evan GI. Oncogenes and cell death. Curr Opin Genet Dev. 1994;4:120-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 193] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 11. | Chen RF, Zou SQ, Qian JQ. Apoptosis and expression of bcl-2 gene in gallbladder neoplasms. Huaren Xiaohua Zazhi. 1998;6:680-682. |
| 12. | Qiao Q, Wu JS, Zhang J, Ma QJ, Lai DN. Expression and significance of apoptosis related gene bcl-2, bax in human large intestine adenocarc inoma. Shijie Huaren Xiaohua Zazhi. 1999;7:936-938. |
| 13. | Yuan RW, Ding Q, Jiang HY, Qin XF, Zou SQ, Xia SS. Bcl-2, P53 protein expression and apoptosis in pancreatic cancer. Shijie Huaren Xiaohua Zazhi. 1999;7:851-854. |
| 14. | Hinds PW, Weinberg RA. Tumor suppressor genes. Curr Opin Genet Dev. 1994;4:135-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 152] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 15. | Wyllie AH. The genetic regulation of apoptosis. Curr Opin Genet Dev. 1995;5:97-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 166] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 16. | Hermeking H, Eick D. Mediation of c-Myc-induced apoptosis by p53. Science. 1994;265:2091-2093. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 525] [Cited by in RCA: 542] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 17. | Reed JC. Bcl-2 and the regulation of programmed cell death. J Cell Biol. 1994;124:1-6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1619] [Cited by in RCA: 1686] [Article Influence: 54.4] [Reference Citation Analysis (0)] |
| 18. | Arends MJ, McGregor AH, Toft NJ, Brown EJ, Wyllie AH. Susceptibility to apoptosis is differentially regulated by c-myc and mutated Ha-ras oncogenes and is associated with endonuclease availability. Br J Cancer. 1993;68:1127-1133. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 80] [Cited by in RCA: 89] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Sun YX, Chen CJ, Zhou HG, Shi YQ, Pan BR, Feng WY. Expression of c-myc and p53 in colorectal adenoma and adenocarcinoma. Huaren Xiaohua Zazhi. 1998;6:1054-1056. |
| 20. | Chen CJ, Sun YX, Zhou HG, Pan BR, Zheng SG, Hong XZ, Liu JH, Feng WY. bcl 2 and p53 expressions in colorectal adenoma and carcinoma. Huaren Xiaohua Zazhi. 1998;6:683-685. |
| 21. | Wang LD, Zhou Q, Wei JP, Yang WC, Zhao X, Wang LX, Zou JX, Gao SS, Li YX, Yang C. Apoptosis and its relationship with cell proliferation, p53, Waf1p21, bcl-2 and c-myc in esophageal carcinogenesis studied with a high-risk population in northern China. World J Gastroenterol. 1998;4:287-293. [PubMed] |
| 22. | Liu HF, Liu WW, Fang DC, Men RP. Expression of bcl-2 protein in gastric carcinoma and its significance. World J Gastroenterol. 1998;4:228-230. [PubMed] |
| 23. | Cao GD, Wang SW, Wu SS, Li HF, Zhang WG. Retrovirus mediated antisense RNA to bcl 2 alter the biological behavior of stomach carcinoma MGC 803 cell lines. World J Gastroentero. 1998;4:45-48. |
| 24. | Liu HF, Liu WW, Fang DC, Men RP. Expression and significance of proapoptotic gene Bax in gastric carcinoma. World J Gastroenterol. 1999;5:15-17. [PubMed] |
| 25. | Ketley NJ, Allen PD, Kelsey SM, Newland AC. Modulation of idarubicin-induced apoptosis in human acute myeloid leukemia blasts by all-trans retinoic acid, 1,25(OH)2 vitamin D3, and granulocyte-macrophage colony-stimulating factor. Blood. 1997;90:4578-4587. [PubMed] |
| 26. | Nooter K, Boersma AW, Oostrum RG, Burger H, Jochemsen AG, Stoter G. Constitutive expression of the c-H-ras oncogene inhibits doxorubicin-induced apoptosis and promotes cell survival in a rhabdomyosarcoma cell line. Br J Cancer. 1995;71:556-561. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 27. | Xiao B, Shi YQ, Zhao YQ, You H, Wang ZY, Liu XL, Yin F, Qiao TD, Fan DM. Transduction of Fas gene or Bcl-2 antisense RNA sensitizes cultured drug resistant gastric cancer cells to chemotherapeutic drugs. World J Gastroenterol. 1998;4:421-425. [PubMed] |
| 28. | Shi YQ, Xiao B, Miao JY, Zhao YQ, You H, Fan DM. Construction of eukaryotic expression vector pBK fas and MDR reversal test of drug resistant gastric cancer cells. Shijie Huaren Xiaohua Zazhi. 1999;7:309-312. |
| 29. | Strobel T, Kraeft SK, Chen LB, Cannistra SA. BAX expression is associated with enhanced intracellular accumulation of paclitaxel: a novel role for BAX during chemotherapy-induced cell death. Cancer Res. 1998;58:4776-4781. [PubMed] |
| 30. | NicAmhlaoibh R, Heenan M, Cleary I, Touhey S, O'Loughlin C, Daly C, Nuñez G, Scanlon KJ, Clynes M. Altered expression of mRNAs for apoptosis-modulating proteins in a low level multidrug resistant variant of a human lung carcinoma cell line that also expresses mdr1 mRNA. Int J Cancer. 1999;82:368-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 31. | Serrone L, Hersey P. The chemoresistance of human malignant melanoma: an update. Melanoma Res. 1999;9:51-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 93] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 32. | Liu HF, Liu WW, Fang DC. Induction of apoptosis in human gastric carcinoma cell line SGC 7901 by anti Fas monoclonal antibody. Shijie Huaren Xiaohua Zazhi. 1999;7:476-478. |
| 33. | Liu HF, Liu WW, Fang DC, Liu FX, He GY. Clinical significance of Fas antigen expression in gastric carcinoma. World J Gastroenterol. 1999;5:90-91. [PubMed] |
| 34. | Cai Z, Stancou R, Körner M, Chouaib S. Impairment of Fas-antigen expression in adriamycin-resistant but not TNF-resistant MCF7 tumor cells. Int J Cancer. 1996;68:535-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 35. | Friesen C, Fulda S, Debatin KM. Deficient activation of the CD95 (APO-1/Fas) system in drug-resistant cells. Leukemia. 1997;11:1833-1841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 137] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 36. | Trauth BC, Klas C, Peters AM, Matzku S, Möller P, Falk W, Debatin KM, Krammer PH. Monoclonal antibody-mediated tumor regression by induction of apoptosis. Science. 1989;245:301-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1286] [Cited by in RCA: 1275] [Article Influence: 35.4] [Reference Citation Analysis (0)] |
| 37. | Itoh N, Yonehara S, Ishii A, Yonehara M, Mizushima S, Sameshima M, Hase A, Seto Y, Nagata S. The polypeptide encoded by the cDNA for human cell surface antigen Fas can mediate apoptosis. Cell. 1991;66:233-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1952] [Cited by in RCA: 2034] [Article Influence: 59.8] [Reference Citation Analysis (0)] |
| 38. | Suda T, Takahashi T, Golstein P, Nagata S. Molecular cloning and expression of the Fas ligand, a novel member of the tumor necrosis factor family. Cell. 1993;75:1169-1178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1816] [Cited by in RCA: 1824] [Article Influence: 57.0] [Reference Citation Analysis (0)] |
| 39. | Boldin MP, Varfolomeev EE, Pancer Z, Mett IL, Camonis JH, Wallach D. A novel protein that interacts with the death domain of Fas/APO1 contains a sequence motif related to the death domain. J Biol Chem. 1995;270:7795-7798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 746] [Cited by in RCA: 764] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 40. | Chinnaiyan AM, O'Rourke K, Tewari M, Dixit VM. FADD, a novel death domain-containing protein, interacts with the death domain of Fas and initiates apoptosis. Cell. 1995;81:505-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1780] [Cited by in RCA: 1800] [Article Influence: 60.0] [Reference Citation Analysis (0)] |
| 41. | Peter ME, Krammer PH. Mechanisms of CD95 (APO-1/Fas)-mediated apoptosis. Curr Opin Immunol. 1998;10:545-551. [PubMed] |
| 42. | Aragane Y, Kulms D, Metze D, Wilkes G, Pöppelmann B, Luger TA, Schwarz T. Ultraviolet light induces apoptosis via direct activation of CD95 (Fas/APO-1) independently of its ligand CD95L. J Cell Biol. 1998;140:171-182. [PubMed] |
| 43. | Medema JP, Scaffidi C, Kischkel FC, Shevchenko A, Mann M, Krammer PH, Peter ME. FLICE is activated by association with the CD95 death-inducing signaling complex (DISC). EMBO J. 1997;16:2794-2804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 918] [Cited by in RCA: 931] [Article Influence: 33.3] [Reference Citation Analysis (0)] |
| 44. | Alnemri ES, Livingston DJ, Nicholson DW, Salvesen G, Thornberry NA, Wong WW, Yuan J. Human ICE/CED-3 protease nomenclature. Cell. 1996;87:171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1686] [Cited by in RCA: 1653] [Article Influence: 57.0] [Reference Citation Analysis (0)] |
| 45. | Boldin MP, Goncharov TM, Goltsev YV, Wallach D. Involvement of MACH, a novel MORT1/FADD-interacting protease, in Fas/APO-1- and TNF receptor-induced cell death. Cell. 1996;85:803-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1726] [Cited by in RCA: 1748] [Article Influence: 60.3] [Reference Citation Analysis (0)] |
| 46. | Muzio M, Chinnaiyan AM, Kischkel FC, O'Rourke K, Shevchenko A, Ni J, Scaffidi C, Bretz JD, Zhang M, Gentz R. FLICE, a novel FADD-homologous ICE/CED-3-like protease, is recruited to the CD95 (Fas/APO-1) death--inducing signaling complex. Cell. 1996;85:817-827. [PubMed] |
| 47. | Muzio M, Salvesen GS, Dixit VM. FLICE induced apoptosis in a cell-free system. Cleavage of caspase zymogens. J Biol Chem. 1997;272:2952-2956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 260] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 48. | Liu ZM, Shou NH. Expression significance of mdr1 gene in gastric carcinoma tissue. Shijie Huaren Xiaohua Zazhi. 1999;7:145-146. |
| 49. | Xu BH, Zhang RJ, Lu DD, Chen XD, Wang NJ. Expression of mdrl gene coded Pglycoprotein in hepatocellular carcinoma and its clinical significance. Huaren Xiaohua Zazhi. 1998;6:783-785. |
| 50. | Kong XB, Yang ZK, Liang LJ, Huang JF, Lin HL. Overexpression of P-glycoprotein in hepatocellular carcinoma and its clinical implication. World J Gastroenterol. 2000;6:134-135. [PubMed] |
| 51. | Smyth MJ, Krasovskis E, Sutton VR, Johnstone RW. The drug efflux protein, P glycoprotein, additionally protects drug resistant tumor cells from mul tiple forms of caspase-dependent apoptosis. Proc Natl Acad Sci USA. 1998;95:7024-7029. [RCA] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 263] [Article Influence: 9.7] [Reference Citation Analysis (0)] |