Published online Apr 15, 1999. doi: 10.3748/wjg.v5.i2.156
Revised: January 19, 1999
Accepted: January 3, 1999
Published online: April 15, 1999
AIM To evaluate the curative effect of pylorus and pyloric vagus-preserving gastrectomy (PPVPG) on peptic ulcer.
METHODS Treating 132 cases of GU and DU with PPVPG, and com parative studies made with 24 cases treated with Billroth I (B I) and 20 cases with Billroth II (B II); advantages and shortcomings evaluated.
RESULTS Not a single death after PPVPG. No recurrence of the disorder in the subsequent follow-up for an average of 6.5 years. Curative effect (visik I-&-II) 97.7%. Acidity reduction similar to that found in B I and B II, but 97.7% of the B I and all B II cases having more than second degree intestinal fluid reflux, in contrast to 7.1% in PPVPG cases. Dumping syndrome occurred in the B I and B II cases, none in PPVPG cases. With regard to gastric emptying, food digestion, absorption, body weight and life quality, PPVPG proved to be superior to Billroth procedure.
CONCLUSION PPVPG has the advantages of conventional Billroth gastrectomy in reducing acid, removing ulcer focus, and at the same time preserves the pylorus and pyloric vagus for maintaining the normal gastric physiological function. Dumping syndrome, intestinal fluid reflux and other complications of conventional gastrectomy may be avoided.
- Citation: Lu YF, Zhang XX, Zhao G, Zhu QH. Gastroduodenal ulcer treated by pylorus and pyloric vagus-preservinggastrectomy. World J Gastroenterol 1999; 5(2): 156-159
- URL: https://www.wjgnet.com/1007-9327/full/v5/i2/156.htm
- DOI: https://dx.doi.org/10.3748/wjg.v5.i2.156
Subtotal resection of stomach (Billroth, 1881), usually referred to as the conve ntional procedure, has been used for over 100 years in the surgical treatment of peptic ulcer. However, such operation, owing to the loss of pyloric function, often causes postoperative problems, such as rapid gastric emptying, dumping syndrome, intestinal content reflux, indigestion, poor absorption, etc. In order to avoid such complications to the fullest extent, we designed the PPVPG and did repeated animal experiments before its clinical application in January 1988. Since that time we treated 132 cases of gastric and duodenal ulcers with gratifying results, with 44 cases treated with Billroth operation for comparison.
The patients under treatment were 121 males and 11 females, 17-67 years old, medium age 46. They had ulcer histories from 1 year to 31 years, averaging 8.3 years. Most (97%) of them had symptoms, such as pains in the upper abdomens, nau sea and vomiting, poor appetite, acidic cructation and heartburn. They took medi cines regularly as part of the treatment. Film takings of the digestive tracts with barium meal and gastroscopy indicated the presence of ulcers, in diameters area of 10 mm-30 mm(51 gastric and 81 duodenal including four cases of compound ulcers). Pylorus stenosis occurred in 4 cases, and duodenal stenosis in 3 cases.
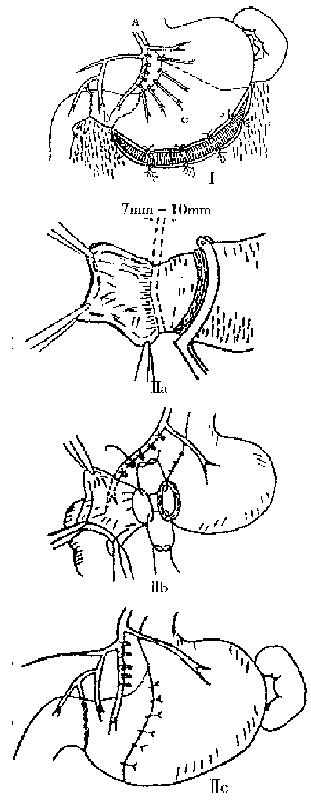
The operation started with dissecting the greater currature from a point 2 cm above the pylorus to the last two branches of the left gastroepiploric artery. The lesser close to the gastric wall, was set free by dissection. The arterior and posterior vagal trunks, hepatic branches and the last 2-3 branches of Lataget vagus innervating the pyloric region, together with attached blood vessels, were carefully preserved; only the vagus branches innervating the body of th e stomach and blood vessels were selectively excised. With the upper part of the gastric body cut off, we sutured the out-edge-of the lesser curve side conven tionally in one layer, reserving 3.5 cm of the greater curve side for anastomosis. The antral cut-edge was trimmed to a concave shape. The antral seromus cular layer from the lesser curvature to the greater curvature where Latarget nerve senter were preserved. The antral mucosa 7 mm-10 mm-proximal to the pyloric ring was excised, and then the mucosal edge 6 cm proximal to the pyloric ring was sutured round all layers of cut edge near the greater curvature (stoma for anastomosis). The antral seromuscular flap with attaching vagus branches was sutured to the region of anastomosis (Figure 1).
Treatment of the ulcer focus. The ulcer was resected together with large part of the stomach in 47 cases; longitudinal section and transverse suture were done in 42 cases of duodenal ulcer and the ulcer of pyloric canal; in 4 cases of bulbar posterior duodenal penetrating ulcer, we freed the back wall of duodenum and the ulcer was transversely sutured, the 4 cases of gastric and duodenal compound ulcers were treated respectively according to the afore-mentioned principle; in those cases with concurrent duodenal or pylorus stenosis, 3 cases were treated with duodenoplasty and 4 cases with pylorus dilatation; and no particular treatm ent was given in 28 cases, and the ulcers were allowed to heal by themselves.
PPVPG has been done in 132 patients with peptic ulcers. Comparative studies were made between PPVPG and Billroth procedures (B I 24 cases and B II 20 cases).
Postoperative examinations (10-15 days) of gastric juice and serum gastrin were carried out in 64 patients. By comparing with the preoperative basic level, the mean basic acid output (BAO) reduction rate was 70.5%, and the mean maximal acid output (MAO) reduction rate 76.3%. The above two indices and postprandial se rum gastrin reduction rate were more or less similar to those in cases undergoing B I and B II operations in the same period (Tables 1, 2 and 3).
A test meal consisting of noodles soup 150 g + 100 g barium sulfate was given to patients of different groups 4 weeks after operation. A normal gastric complete emptying time was seen in 81.8% of the PPVPG group, 50% of the B I gro up and all cases of the B II group in which complete emptying occurred in 30 minutes. The results demonstrate that the conventional subtotal gastrectomy with Billroth anastomosis has the disadvantage of greatly quickened gastric emptying time. Furthermore, 9.1% gastric retention occurred in Billroth operation, whereas only 2.3% (3/132) of the PPVPG patients had such complication.
Three months postoperatively, patients with one of the following three complaints were suggestive of having dumbing syndrome: a. postprandial dizziness, b. cold sweating and c. palpitation[2]. Thus, the dumping syndrome was noted in 16.7% of the B I group and 15.0% of the B II group, but in none of the PPVPG group.
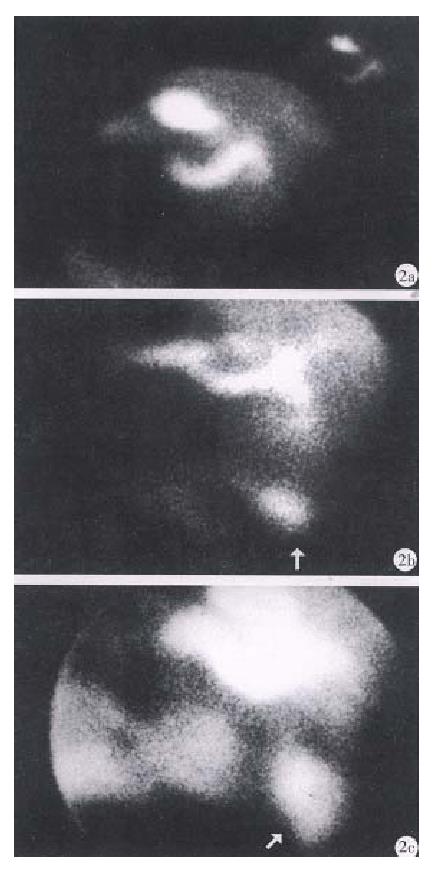
Four weeks after the operation, duodeno-gastric reflux was measured by dynamic scanning by means of intravenous injection of 99 mTc-EHIDA 185MBq (5mci). The degree of reflux was divided into six grades, and only those higher than grade II had an apparent clinical value[3]. In 96 patients after PPVPG, only 7 (7.3%) had reflux to a small extent, with no clinical symptoms; whereas those undergoing B I and B II, reflux occurred in 97.9% of the patients (Figure 2, Table 4), either with or without subjective symptoms. Bacterial cultures of the gastric juice were positive in all cases with reflux.
| Operation mode n | Reflux indexes grades (%) | ||||||||
| I < 5% | II -10% | III -20% | IV -30% | V -40% | VI > 40% | Total | % | ||
| PPVPG | 84 | 6 | 0 | 0 | 0 | 0 | 0 | 6 | 7.1 |
| B I | 24 | 0 | 6 | 7 | 5 | 5 | 0 | 23 | 95.8 |
| B II | 20 | 0 | 0 | 5 | 6 | 4 | 5 | 20 | 100.0 |
Beginning on the 7th postoperative day, the patients were given a specially prepared diet for 4 consecutive days. It was discovered that (1) diarrhea occurred in 11.4% of the cases with the Billroth operations, but in none of the cases with PPVPG; (2) the amount of fat globules in the stool of PPVPG cases was much less than that in B I and B II cases; (3) the postoperative urinary nitrogen excretion was 13.1gm per day in the PPVPG cases, 17 gm in B I cases and 20.1 gm in B II cases. These results suggested that patients undergoing Billroth operations had relatively poorer function of digestion and absorption, and their catabolism increased; and (4) body weight was measured three months before and after operations, 92.8% of the patients with PPVPG showed no body weight loss, a result much better than 79% with BI and 65% with BII.
Through phone calls or by mails and re-examinations at the outpatient department, our follow-ups have lasted over a period of 1-10 years, averaging 6.5 years as a whole. To our satisfaction, no ulcer relapses or complications have been found in the surveys of 132 patients, Visik grades I, II 97.7%. Gastroscopic examinations done in 72 (54.5%) of 132 patients showed a complete disappearance of the original ulcer foci together with normal remanent gastric mucosa and pylorus.
Despite different explanations for the causation and evolution of peptic ulcer, acknowledged explanation for gastric acid is involved. Therefore, a reduction of gastric acid secretion is regarded as the principle of surgical treatment of ulcer. In the conventional Billroth operation, this point has been fully asserted, but also considered as an important standard for judging ulcer recurrence rate. In this regard, PPVPG and Billroth are equally effective. PPVPG effectively reduces gastric acid by stripping off the antral mucosa containing many G cells, resulting in decreased hormonal stimulation, and by subtotal resection of stomach corpus which leads to greatly reduced parietal cells. As the vagus branch innervating the remanent stomach body is separated by excision and its direct effect on the parietal cells thus stopped, so the operation effectively reduces gastric acid. The mean BAO decreased by 70.5% and the mean MAO by 76.3%, they bore no marked difference with those of homochronous Billroth operations (P > 0.05). The small part of antral mucosa was preserved for the purpose of anastomosing it with the cut edge near the greater curve so as to avoid the stenosis of anastomotic more likely to occur in stoma directly anastomosing the cut edge with the mucosa of the pyloric tube and also to avoid the possibility that excessive excision would affect the function and integrity of pyloric sphincter. The small part of antrum mucosa retained, in fact, would be just good enough for being scarred. The scar width of the anastomotic stoma in experimental dogs was 6 mm-8 mm 6 months after operation and would lose its function of promoti ng secretion. Care must be taken, however, to make the antral mucosa 7 mm-10 mm wide. The width less than 7 mm may lead to the stenosis of anastomotic stoma, but more than 10 mm will affect the reduction of gastric acid. AN NN et al[4] considered the optimal free HCl concentration after the resection of stomach as 20 clinical units, and the mean free HCl of PPVPG was 15.68 clinical units (equal to 15.68 mmol/L). What is more important is that in the postoperative follow-ups, not a single case of relapse was found and the curative effect was proved to be highly gratifying. All these demonstra te that PPVPG designed is scientific enough to meet all clinical requirements. With the vagus resected, the action potential of gastric smooth muscle is 8-20 times less than normal[1], leading to a delay of gastric emptying and retention. The preservation of vagus in the operation is to avoid this condition and also to retain the physiological function of pyloric sphincter. The small part of seromuscular flap retained in PPVPG protects the branches of latarjer vagus passing through it to the pylorus along with the attaching blood vessels and also reinforce the anastomotic stoma to prevent from leaking. PPVPG has the advantages of conventional Billroth gastrectomy in reducing acid, removed ulcer focus, at the same time preserves pylorus and pyloric vagus, which enables the pylorus and the remanent stomach to function normally. PPVPG has greatly avoided postoperative complications of the subtotal gastric resection, such as dumping syndrome, intestinal fluid reflux and so on. Safe and adaptable to wide variety of indications, PPVPG carves not only a new course for the surgical treatment of peptic ulcer, including perforated ulcer, profuse bleeding due to gastroduodenal ulcer, and slight duodenal or pylorus stenosis, but also can be applied to other benign gastric lesion such as polyposis, leiomyoma and ectopic pancreas.
Edited by Han-Ming Lu
| 1. | Lu Y, Hoa Y, Jia S, Gao C. Experimental study of pylorus and pyloric vagus preserving gastrectomy. World J Surg. 1993;17:525-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Sekine T, Sato T, Maki T, Shiratori T. Pylorus-preserving gastrectomy for gastric ulcer--one- to nine-year follow-up study. Surgery. 1975;77:92-99. [PubMed] |
| 3. | Gu SQ. Determination of duodenal gastric reflex. Beijing Yixue. 1988;4:78-81. |
| 4. | An NN, Ky R, Wang MS. Clinical experience of 18 cases of gas-trectomy preserving pylorus. Shiyong Waike Zazhi. 1986;6:245-247. |