Published online Feb 15, 1998. doi: 10.3748/wjg.v4.i1.24
Revised: September 20, 1997
Accepted: October 10, 1997
Published online: February 15, 1998
AIMS: To observe the therapeutic effect of Wei-xibaonizhuan pills on gastric precancerous lesions.
METHODS: Thirty patients with gastric precancerous lesions were treated with Weixibaonizhuan pills for 3 months. Of the 36 cases, 13 (36.1%) were mild atrophic gastritis, 14 (38.9%) moderate atrophic gastritis and 9 (25.0%) severe atrophic gastritis; among them 22 (61.1%) and 27 cases (75.0%) were accompanied with intestinal metaplasia (IM) and dysplasia (DYS) respectively. Of the 36 patients, 20 were men and 16 women, aged from 30-60 years and those aged 30-59 years accounted for 61.1%. The course of disease ranged from 3 months to 21 years, and 20 (55.6%) of them had a course of 5-10 years. The clinical manifestations were fullness of the abdomen (31 cases),abdominalgia (27 cases), anorexia (30 cases), gas eructation (26 cases), acid regurgitation (6 cases) and loose stool (9 cases). When treatment ended, the improvement of patients’ clinical symptoms, atrophy of gastric mucosa, IM and DYS were analysed.
RESULTS: After 3 months’ treatment with Wei-xibaonizhuan pills,7 cases recovered, 11 cases were much improved, 13 cases showed some improvement, and 5 cases were ineffective; the total rate of symptomatic improvement was 86.1%. Of the 13 cases with mild atrophic gastritis, 11 cases changed into superficial gastritis, and 2 cases had no changes. Of the 14 cases of moderate atrophic gastritis, 4 cases changed into superficial gastritis, 7 cases changed into mild atrophic gastritis, and 3 cases had no changes. Five of 9 cases of severe atrophic gastritis were reduced to moderate atrophic gastritis, and 4 cases had no changes. The total effective rate was 77.8% in chronic atrophic gastritis. Of the 9 cases with mild IM, IM disappeared in 6 cases and 3 showed no change. Of the 10 cases with moderate IM, it disappeared in 2 cases, 5 cases changed to mild IM, and 3 cases had no change. One of the 4 cases of severe IM changed to moderate IM and 3 had no change. The total effective rate was 63.6% in IM. Of the 16 cases of mild DYS, 11 cases showed disappearance of DYS and 5 had no change. In 9 cases of moderate DYS, 2 showed disappearance, 5 changed to mild DYS and 2 had no change. Two cases of severe DYS, both showed no change. The total effective rate was 66.7% in DYS. Before treatment, the I, II, III and IV degree positive expressions of CEA were present in 13, 12, 9 and 2 cases, respectively, whereas after treatment, the positive expressions were present in 25, 7, 3 and 1, respectively. Before treatment, the I, II, III and IV degree positive expressions of PCNA were present in 16, 11, 10 and 4 respectively, but after treatment, they were present in 21, 9, 5 and 1 respectively. In short, the positive expressions of CEA and PCNA of gastric mucosa were significantly decreased after treatment (P < 0.01).
CONCLUSION: Weixibaonizhuan pill has a therapeutic effect in gastric precancerous lesions.
- Citation: Zhang XC, Gao RF, Li BQ, Ma LS, Mei LX, Wu YZ, Liu FQ, Lian ZL. Clinical and experimental study of therapeutic effect of Weixibaonizhuan pills on gastric precancerous lesions. World J Gastroenterol 1998; 4(1): 24-27
- URL: https://www.wjgnet.com/1007-9327/full/v4/i1/24.htm
- DOI: https://dx.doi.org/10.3748/wjg.v4.i1.24
Gastric carcinogenesis often arises from some precancerous lesion for cancer development. Effective treatment of such lesions would be helpful in decreasing the risk of gastric cancer. We have used Weixibaonizhuan pills (WXBNZ pills ) to treat them and have obtained a good result.
Thirty-six patients with gastric precancerous lesions were diagnosed through gastroscopy and mucosal biopsy[1]. Among them, 13 (36.1%) cases were mild chronic atrophic gastritis (CAG), 14 (25.0%) cases moderate CAG, and 9 severe CAG. Twenty-two ( 61.1%) and 27 (75.0%) cases were accompanied intestinal metaplasia ( IM ) and dysplasia (DYS), respectively. Of the 36 patients 20 were men and 16 women; their age ranged from 30-60 years, and those between 40-59 years of age accounted for 61.1%. The course of disease ranged from 3 months to 21 years, and 20 of them (55.6%) had a course of 5-10 years. The clinical manifestations were as follows: (1) abdominal fullness or feeling of obstruction in the stomach (31 cases), worse in afternoon or after eating and abated after eructation or passing wind from bowels; (2) abdominalgia (27 cases) in middle abdomen and epigastrium, more often vague, or distending, burning, stabbing, with tenderness; (3) anorexia (30 cases); (4) eructation after eating or of frequent occurrence (26 cases); (5) acid regurgitation (6 cases) became severe when fasting; and (6) loose stool (9 cases), watery or unformed.
All patients took WXBNZ pill ( composed of 15 kinds of herbs including Radix Codonopsis pilosulae, Radix Salviae Miltiorhizae, Herba Solani Nigri, Radix et Rhizoma Rhei, Rhizoma coptidis , etc, prepared by the Research and Treatment Center of Gastroenterology of Taiyuan) 6 grams three times a day for a course of 3 months. Gastroscopic and pathologic studies of biopsy specimens were performed before and within 2 weeks after treatment. During gastroscopy, 1 biopsy specimen was taken each from the antral lesser curvature, greater curvature, anterior wall and antrum-body transitional zone, respectively, and additional 1-2 biopsy spe-cimens were taken from the grossly identifiable lesions. The examinations were made by fixed doctors. In addition to routine HE staining, we also used immunohistochemical technique to detect the expression of CEA and PCNA of gastric mucosa. CEA antibody (rabbit against human) and PCNA antibody (mouse against human) were provided by Zymed Co. and universe type biotinylated secondary antibody was made in our lab. The staining procedure was performed according to the literature[2].
Of the 36 cases, 7 recovered with a disappearance of clinical symptoms, 11 had significant improvement of symptoms, 13 showed some improvement, and 5 had no change. The total effective rate was 86.1%.
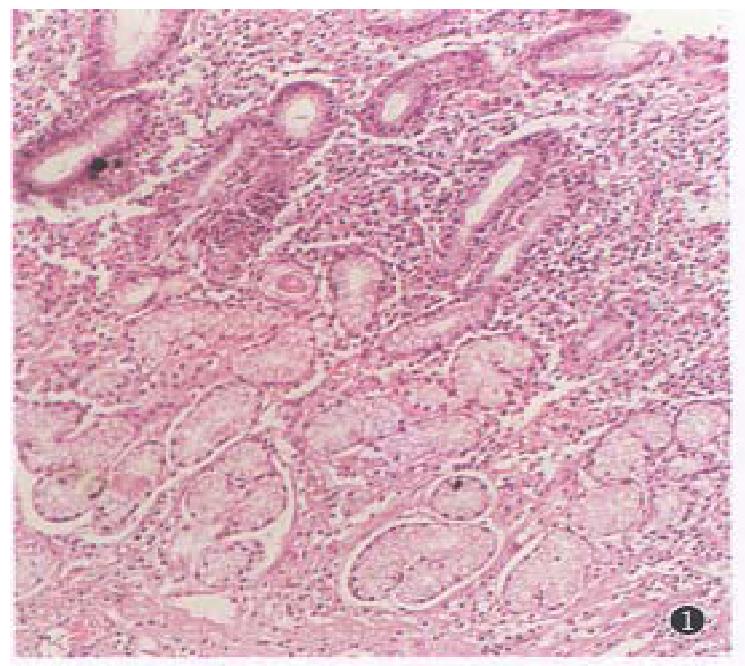
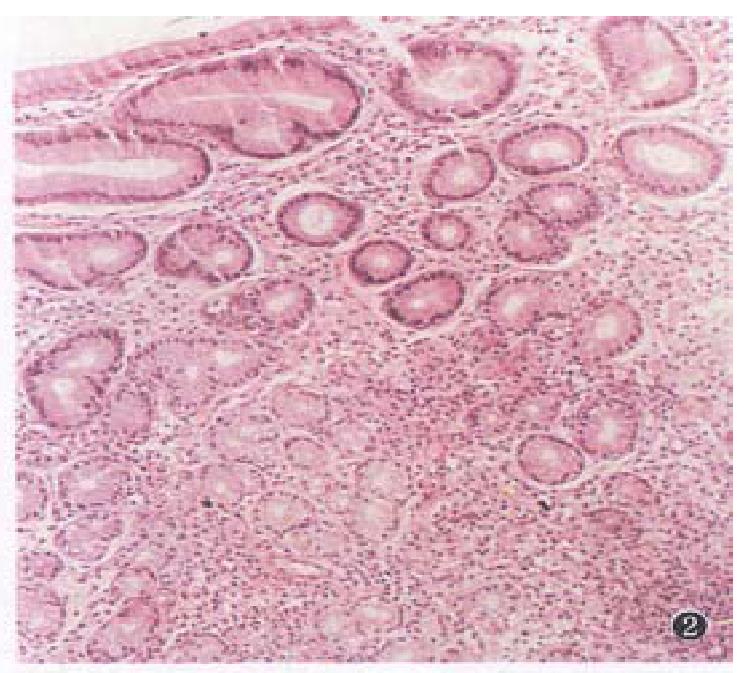
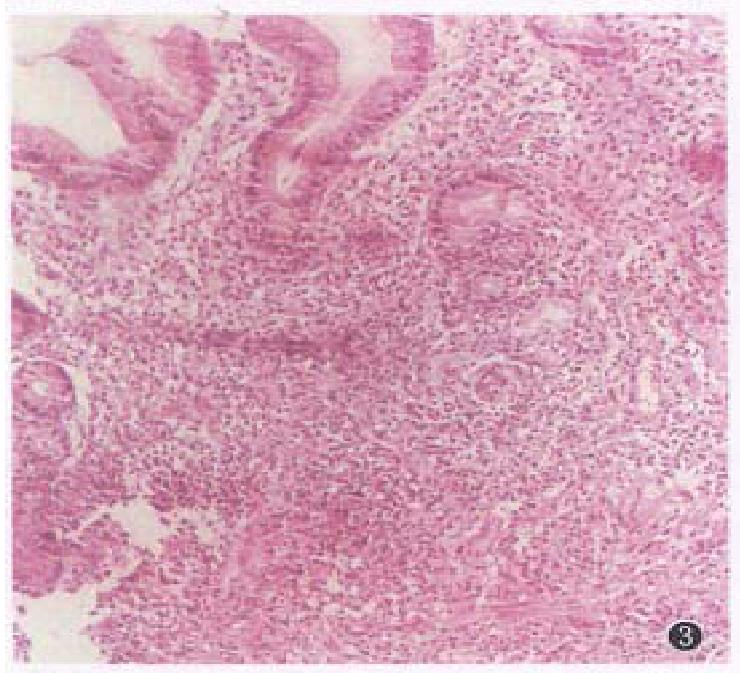
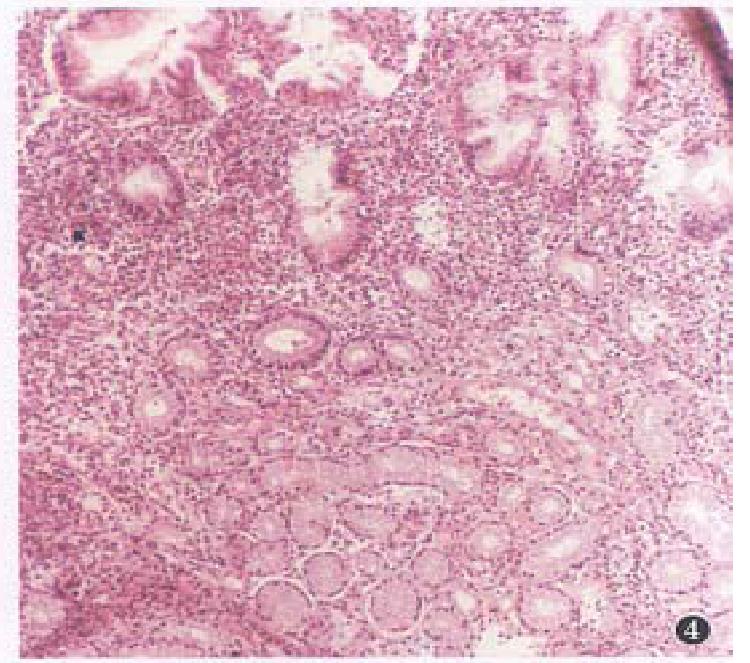
In 13 cases of mild CAG, 11 cases changed to superficial gastritis, and 2 had no change, the effective rate being 84.6%. Among 14 cases of moderate CAG, 4 changed to superficial gastritis, 7 changed to mild CAG (Figure 1, Figure 2), 3 cases had no change, the effective rate being 78.6%. Five of the 9 cases of severe CAG changed to moderate CAG (Figure 3, Figure 4), and 4 cases had no change, the effective rate being 55.6%. The total effective rate for CAG was 77.8%, and the therapeutic effectiveness seemed to be better in mild and moderate CAG.
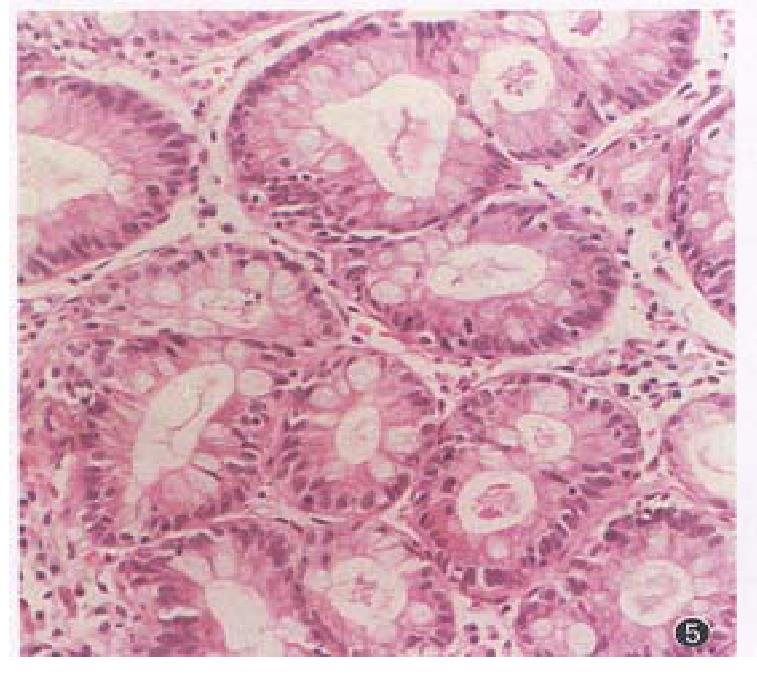
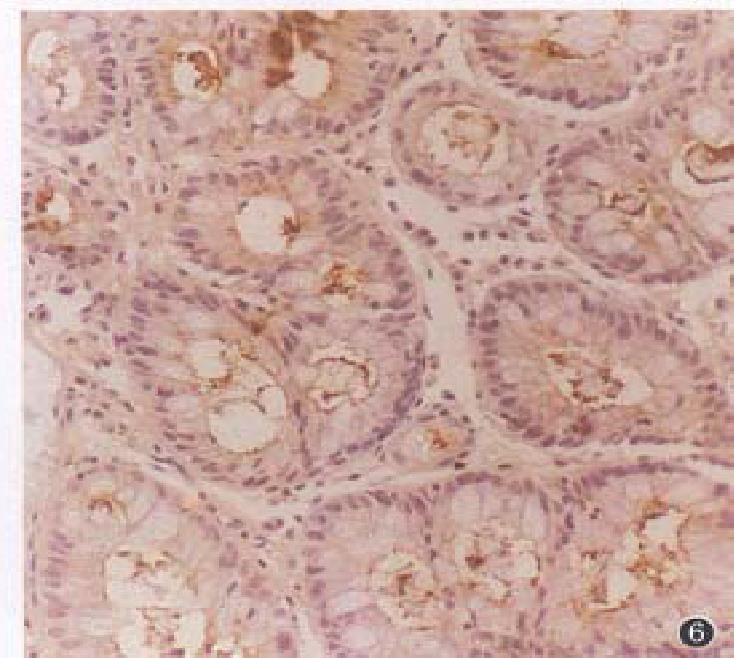
In the 9 cases of mild IM, it disappeared in 6 cases, and 3 cases had no change, the effective rate being 66.7%. In the 10 cases of moderate IM, 2 cases showed a disappearance of IM, 5 cases changed to mild IM and 3 cases had no change (Figure 5, Figure 6), the effective rate being 70.0%. Only one of the 4 cases of severe IM changed to moderate IM and 3 had no change, the effective rate being 25.0%. The total effective rate for IM was 63.6% and the therapeutic effectiveness was better in mild and moderate IM.
In the 16 cases of mild DYS, 11 cases showed its disappearance and 5 had no change, the effective rate being 68.8%. In the 9 cases of moderate DYS, 2 had a disappearance of DYS, 5 changed to mild DYS and 2 had no change, the efficacy rate was 77.8%. Both of the 2 cases of severe DYS showed no change after treatment, the efficacy rate was 0.0%. The total effective rate was 66.7% in DYS, and the therapeutic effectiveness was better in mild and moderate DYS.
A semiquantitative method was used to judge the brown-stained positive cells[3]. The positive degree was scored according to the number of positive cells. Grade I: 0%-25%, grade II: 26%-50%, grade III: 51%-75%, and grade IV: 76%-100%. The expression of CEA decreased significantly after treatment (P < 0.01), (Table 1).
| Treatment | Grades | |||
| I | II | III | IV | |
| Before | 13 | 12 | 9 | 2 |
| After | 25 | 7 | 3 | 1 |
The positive criteria of PCNA was similar to CEA. The PCNA expression decreased significantly after treatment (P < 0.01) (Table 2).
| Treatment | Grades | |||
| I | II | III | IV | |
| Before | 26 | 11 | 10 | 4 |
| After | 21 | 9 | 5 | 1 |
The rate of cancer transformation in patients with CAG was reported to be 0.2%[4]; those with mild DYS was 2.5%-11%[5]; moderate DYS, 4%-35%[5,6]; severe DYS, 10%-83%[7]; and IM, 1.9%[4]. It can be suggested that treatment of procancerous lesions may decrease the incidence of gastric cancer effectively. The long-standing chronic gastritis may result in gastric mucosal atrophy, dysplasia and IM of glandular epithelium. As a consequence of such pathologic changes, the patient may have hyposecretion of gastric acid and pepsin, along with symptoms of dyspepsia, such as anorexia and abdominal distention after eating, loose stool, malnutrition, etc. According to the theory of traditional Chinese medicine (TCM), such manifestations belong to an “ insufficiency of the Spleen and Stomach qi”. Another group of patients presenting symptoms of epigastric pain, eructation, acid regurgitation, nausea, etc belong to “disharmony between the Liver and the Stomach” with stagnation and reversed flow of qi, together with the production of Heat. So chronic gastritis with precancerous lesions is a complicated ailment in TCM with regard to its cause ad pathogenesis. The rationale of its management is to strengthen the Spleen and Stomach, to enhance the body resistance, to consolidate the constitution, to promote flow of qi and blood, and to disperse Heat. Only by this way can the symptoms and pathology be improved effectively. We used WXBNZ pills, which was composed of 15 kinds of herbs and had the above-montioned effects of strengthening the Spleen and Stomach, strengthening the body resistance, to consolidate the constitution, promoting flow of qi and blood and dispersing Heat, in treating the patients with gastric precancerous lesions. The total effective rates for clinical symptoms, CAG, DYS, IM were 86.1%, 77.8%, 66.7%, 63.6%, respectively. These results indicated that WXBNZ pills had a good therapeutic effect in gastric precancerous lesions.
From the results in this study we can infer that WXBNZ pills has a better therapeutic effects in mild and moderate CAG, DYS and IM, but gives poor results in severe CAG, DYS and IM. Therefore, early diagnosis and early treatment of such lesions are recommended. In normal gastric mucosa, CEA staining is negative or restricted to the secretory margin of cells. In precancerous lesions, the CEA staining showed a positive expression not only at the secretory margin of cells but also in the apical cytoplasm or further dispersed in the whole cell membrane and cytoplasm. We found in our previous study that positive expression of CEA increased progressively as the precancerous lesions progressed[2]. The positive expression of CEA may reflect the beginning of a deviation or transition of normal state of cell differentiation toward malignancy. In this study, the positive expression of CEA decreased and disappeared gradually after WXBNZ pills treatment, indicating that WXBNZ pill might have some effect of inhibiting the CEA expression and accele-rating the recovery of gastric mucosal function. Recent studies have shown that PCNA is related intimately to the DNA synthetic phase (S phase), and is a good marker reflecting the activity of cell proliferation[3]. In this study, the high positive expression of PCNA in the gastric mucosa with precancerous lesions decreased distinctly after WXBNZ pills treatment. These results suggested that WXBNZ pills could inhibit the cell proliferative activities and abnormal hyperplasia of gastric mucosa in patients with precancerous lesions.
Project supported by grants from the Shanxi Commission of Science and Technology, No.930001.
| 1. | Bureau of Medical Administration of People's Republic of China. Diagnostic and therapeutic standardization of common tumors in China, First ed. Beijing: Press of Beijing Medical University and Peking Union Medical College 1991; 37-41. |
| 2. | Li BQ, Zhang XC, Mei LX, Liu FQ. Immunohistological study of CEA and PCNA in gastric epithelial dysplasia. Chin J New Gastroenterol. 1996;4:29-30. |
| 3. | Garcia RL, Coltrera MD, Gown AM. Analysis of proliferative grade using anti-PCNA/cyclin monoclonal antibodies in fixed, embedded tissues. Comparison with flow cytometric analysis. Am J Pathol. 1989;134:733-739. [PubMed] |
| 4. | Xu CP, Liu WW. Follow-up study of chronic gastritis, intestinal metaplasia and atypical hyperplasia. Chin J Digestion. 1984;4:10-11. |
| 5. | Rugge M, Farinati F, Di Mario F, Baffa R, Valiante F, Cardin F. Gastric epithelial dysplasia: a prospective multicenter follow-up study from the Interdisciplinary Group on Gastric Epithelial Dysplasia. Hum Pathol. 1991;22:1002-1008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 52] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Coma del Corral MJ, Pardo-Mindan FJ, Razquin S, Ojeda C. Risk of cancer in patients with gastric dysplasia. Follow-up study of 67 patients. Cancer. 1990;65:2078-2085. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Farinati F, Cardin F, Di Mario F, Valiante F, Naccarato R, Arslan-Pagnini C, Rugge M, Baffa R. Follow-up in gastric dysplasia patients. Am J Surg Pathol. 1989;13:173-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |