Published online Mar 7, 2024. doi: 10.3748/wjg.v30.i9.1096
Peer-review started: December 17, 2023
First decision: January 16, 2024
Revised: January 26, 2024
Accepted: February 18, 2024
Article in press: February 18, 2024
Published online: March 7, 2024
Processing time: 79 Days and 9.6 Hours
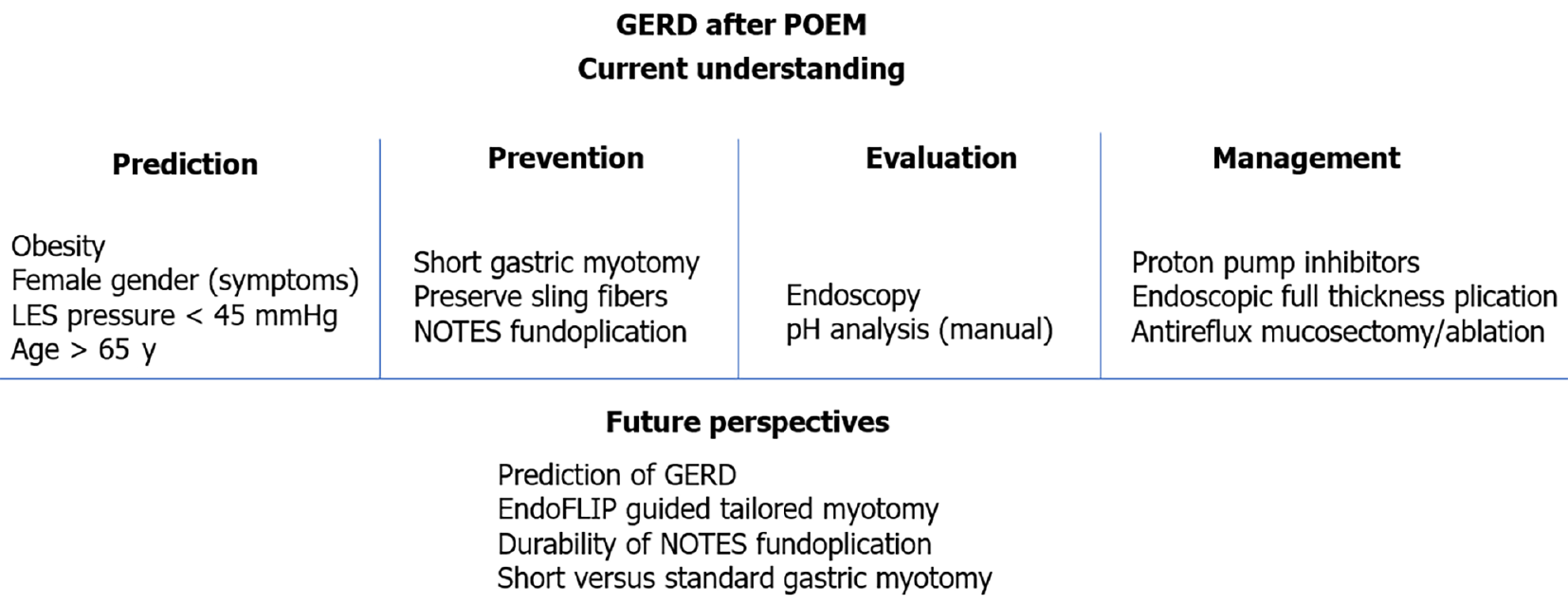
Achalasia cardia, the most prevalent primary esophageal motility disorder, is predominantly characterized by symptoms of dysphagia and regurgitation. The principal therapeutic approaches for achalasia encompass pneumatic dilatation (PD), Heller's myotomy, and the more recent per-oral endoscopic myotomy (POEM). POEM has been substantiated as a safe and efficacious modality for the management of achalasia. Although POEM demonstrates superior efficacy compared to PD and an efficacy parallel to Heller's myotomy, the incidence of gastroesophageal reflux disease (GERD) following POEM is notably higher than with the aforementioned techniques. While symptomatic reflux post-POEM is relatively infrequent, the significant occurrence of erosive esophagitis and heightened esophageal acid exposure necessitates vigilant monitoring to preclude long-term GERD-related complications. Contemporary advancements in the field have enhanced our comprehension of the risk factors, diagnostic methodologies, preventative strategies, and therapeutic management of GERD subsequent to POEM. This review focuses on the limitations inherent in the 24-h pH study for evaluating post-POEM reflux, potential modifications in the POEM technique to mitigate GERD risk, and the strategies for managing reflux following POEM.
Core Tip: Per-oral endoscopic myotomy (POEM) has gained recognition as a primary therapeutic intervention for achalasia cardia. POEM is distinguished by its effectiveness and a commendable safety profile. However, gastroesophageal reflux disease (GERD) has emerged as an important long term adverse event after POEM. Notably, the incidence of GERD is higher after POEM when compared to the other leading treatment modalities including pneumatic dilatation and Heller’s myotomy with fundoplication. Since the introduction of POEM in 2010, there has been considerable advancement in our understanding of GERD after POEM. This article aims to elucidate the recent developments in predicting, preventing, assessing, and managing GERD subsequent to POEM intervention.
- Citation: Nabi Z, Inavolu P, Duvvuru NR. Prediction, prevention and management of gastroesophageal reflux after per-oral endoscopic myotomy: An update. World J Gastroenterol 2024; 30(9): 1096-1107
- URL: https://www.wjgnet.com/1007-9327/full/v30/i9/1096.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i9.1096
Per-oral endoscopic myotomy (POEM) is an established endoscopic treatment modality for achalasia and allied non-achalasia spastic esophageal motility disorders. Contemporary guidelines from leading gastrointestinal societies endorse POEM as a primary treatment option for achalasia[1-4]. While the safety and efficacy of POEM are well-established, the emergence of postoperative gastroesophageal reflux disease (GERD) has become a prominent concern in recent literature[5]. Studies employing endoscopic and pH monitoring studies have revealed a notably high incidence of GERD following POEM[5-7]. Comparative analyses in randomized studies have demonstrated a significantly higher incidence of GERD in comparison to pneumatic dilatation (PD) and laparoscopic Heller’s myotomy (LHM)[8,9]. Consequently, recent research has increasingly concentrated on the prevention, diagnosis and management of GERD after POEM.
This review aims to provide an overview of the latest developments in predicting, preventing, evaluating, and managing GERD subsequent to POEM.
POEM represents the most recent advancement among the available treatment options for achalasia cardia[10]. Initial studies primarily concentrated on assessing the safety and the efficacy of POEM in providing symptomatic relief. Consequently, early investigations lacked comprehensive data on post-POEM reflux, resulting in a wide variation in reported GERD prevalence following the procedure[5]. Recent research efforts have undertaken more rigorous evaluations of GERD post-POEM (Table 1). In a multicenter study involving 282 patients, post POEM reflux esophagitis and GERD on pH analysis was reported in 23.2% and 57.8% of patients, respectively[6]. Nabi et al[11] evaluated GERD in 209 consecutive patients who underwent POEM[11]. A high DeMeester score (> 14.72), reflux esophagitis, and symptomatic GERD were identified in 47.9%, 41.9%, and 29.3% of patients, respectively[11]. Additionally, two rando
| Ref. | Country | n | GERD on pH analysis | Symptoms | Erosive esophagitis | PPI use |
| Kumbhari et al[6], 2017 | Multicenter | 282 | 57.8% | 39.9% | Overall: 23.2% | 38.6% |
| Modayil et al[12], 2021 | United States | 610 | 57.1% | 20.5% (> 1/week) | Overall: 49.8% | 74.7% |
| Nabi et al[11], 2020 | India | 209 | 47.9% | 29.3% | Overall: 41.9% | NR |
| Shiwaku et al[7], 2022 | Japan, Multicenter | 2905 | NR | 15.9% (GERD Q > 7) | Overall: 64.9%. Severe (LA C and D): 7.5% | 33.2% |
| Abu-Nuwar et al[17], 2022 | United States | 183 | Objective GERD (pH/endoscopy): 50.5% | 38.8% | - | NR |
| Simkova et al[67], 2023 | Czech Republic | 522 | 47.1% | 32.6% | 41.4%. Severe (LA C and D): 4.6% | 52.1% |
In contrast to the notable incidence of erosive esophagitis and increased esophageal acid exposure observed on pH analysis, the majority (60% to 80%) of patients remain asymptomatic for reflux[5,6,11]. Karyampudi et al[13] compared post POEM reflux with reflux in individuals without esophageal motility disorders[13]. They concluded that despite more severe esophagitis, the symptoms in post-POEM reflux cases tend to be milder and the correlation between reflux and symptoms is weaker compared to controls.
In summary, while the occurrence of reflux esophagitis and increased esophageal acid exposure is high after POEM, symptomatic GERD is infrequent, and severe reflux esophagitis is not commonly observed in these cases.
Understanding the risk factors for GERD following POEM is crucial not only for preventive strategies but also for necessitating close monitoring. Various studies have identified several risk factors associated with post-POEM reflux. These include a higher body mass index (BMI > 35 kg/m2), the presence of hiatal hernia, a low integrated relaxation pressure post-POEM, pre-POEM lower esophageal sphincter (LES) pressures below 45 mmHg, low post-POEM LES pressure, and female gender[6,14-21].
Additionally, certain technical aspects of the POEM procedure have been implicated in predisposing patients to GERD. These factors encompass long esophageal myotomy, posterior myotomy, full thickness myotomy and excess myotomy (> 4 cm) on the gastric side[22,23]. A comprehensive study from Japan involving 2905 patients identified additional risk factors including age ≥ 65 years [relative risk (RR) 1.72], previous treatments (RR 2.21), Eckardt score ≥ 7 (RR 0.68), sigmoid-type achalasia (RR 1.40), and esophageal myotomy exceeding 10 cm (RR 1.59) as being associated with severe reflux esophagitis[7]. Contrarily, other studies have not confirmed a correlation between post-POEM reflux and patient or procedural factors, including obesity, gender, full thickness myotomy, long esophageal myotomy and orientation of myotomy[6,11,24,25]. The divergent findings across different studies underscore that the prediction of GERD following POEM necessitates further exploration through high quality research (Table 2).
| Factors | Conclusions reported in published studies | Ref. |
| Patient related factors | ||
| Female gender | Symptoms of GERD more likely in females | [6,11,17] |
| No effect of gender on post POEM reflux | [11] | |
| Age | Age > 65 yr is a risk factor for GERD (RR: 1.72) | [7] |
| Hiatus hernia | Presence of hiatal hernia predisposes to post POEM reflux | [14] |
| Obesity | BMI > 35 is a risk factor for GERD | [14,20] |
| BMI > 30 is an independent risk factor | [17] | |
| Increase in BMI after POEM is a risk factor for new onset GERD symptoms | [15] | |
| Obesity is not a risk factor for GERD | [21] | |
| Manometry parameters and GERD | ||
| LES pressure | Pre-operative resting LES pressure ≤ 45 mmHg (OR: 1.86) | [17] |
| IRP | Low IRP after POEM is a risk factor | [19,23] |
| POEM technique related factors | ||
| Length of myotomy | Long esophageal myotomy predisposes to increased esophageal acid exposure | [7,32] |
| Myotomy length < 7 cm associated with less PPI use | [70] | |
| No impact of esophageal myotomy length on GERD | [17,33,34] | |
| Long gastric myotomy predisposes to severe esophagitis | [22] | |
| Short (1 cm) gastric myotomy associated with less symptoms and reflux esophagitis | [41] | |
| Myotomy along gastric side not associated with ≥ LA grade B esophagitis | [57] | |
| Posterior POEM | Posterior myotomy leads to higher rates of increased esophageal acid exposure | [5] |
| Reflux rates similar between anterior and posterior POEM | [54,55] | |
| Full thickness myotomy | Clinically relevant GERD higher after full thickness myotomy | [23] |
| Incidence of GERD similar between selective circular and full thickness myotomies | [38,56] | |
| Sling fibers | Preservation of sling fibers reduces ≥ LA grade B esophagitis | [42,43] |
| No significant effect of sling fiber preservation on the rate of GERD | [44] | |
| NOTES fundoplication | POEM-F reduces the incidence of GERD at 1-yr | [47] |
| Fundoplication wrap remains intact in 83% cases at 1-yr | [47] | |
| Loosening of wrap in substantial proportion (41.2%) at 3-months | [50] | |
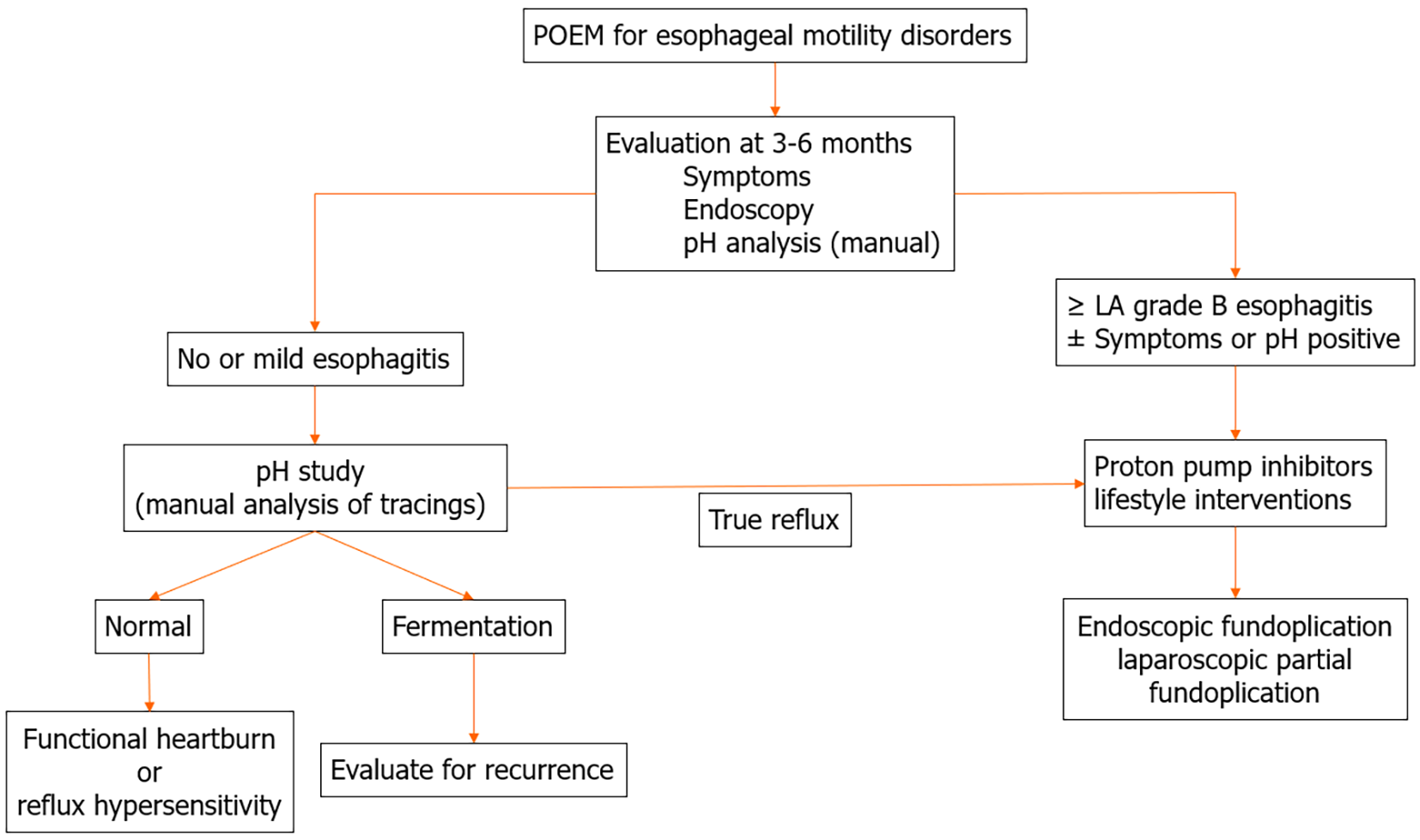
The assessment of GERD after POEM encompasses a multifaceted approach involving endoscopy, pH analysis, and symptom assessment through standardized questionnaires (Figure 1).
Published studies report symptomatic GERD in 16% to 40% of cases after POEM. Intriguingly, symptoms can be absent even in cases exhibiting severe reflux esophagitis and increased esophageal acid exposure on pH studies. The weak correlation between symptoms and both reflux esophagitis and increased esophageal acid exposure suggests that symptomatic presentation alone may not be a reliable indicator of GERD after POEM. Therefore, proactive monitoring is advised regardless of the presence or absence of reflux symptoms after POEM.
Reflux esophagitis (LA grade ≥ B) on endoscopy has been identified as an objective and reliable marker of GERD[26]. However, the presence of ulcers with distinct endoscopic appearance is not uncommon after POEM and should be distinguished from reflux esophagitis. A comprehensive study from the United States involving 610 patients found solitary esophagogastric junction ulcers in 29% of the cases[12]. The study posits that these ulcers might indicate ischemic, poorly healing mucosa rather than being a direct consequence of reflux esophagitis.
The quantification of esophageal acid exposure is generally regarded as the definitive method for confirming GERD. However, several noteworthy considerations arise, particularly in the context of achalasia. Unlike typical GERD cases, achalasia patients have impaired peristalsis leading to significant stasis, which can lead to fermentation and subsequent esophageal acidification. As a result, there is a potential for misclassification of fermentation-induced esophageal acidification as GERD in this population[27,28].
A detailed study focusing on reflux in treated achalasia patients revealed that most occurrences of esophageal acidification were not related to reflux[29]. Automated pH analysis systems are unable to distinguish between true esophageal acid exposure and false GERD due to fermentation induced acidification. Therefore, manual interpretation of pH tracings becomes essential to differentiate between these two scenarios[30]. Characteristic patterns of esophageal acid exposure in cases with achalasia include: (1) A rapid decline in pH to less than 3 with slow clearance, indicative of true GERD; and (2) a gradual decrease in pH, seldom falling below 3.7, characteristic of fermentation secondary to food stasis[30]. In a recent prospective study including 54 patients undergoing POEM, "true acid reflux" was identified in 29.6% of cases, in contrast to 64.8% as indicated on automated analysis[31]. This finding underscores the importance of manual review of pH tracings to accurately identify "true acid reflux" in patients with achalasia after POEM.
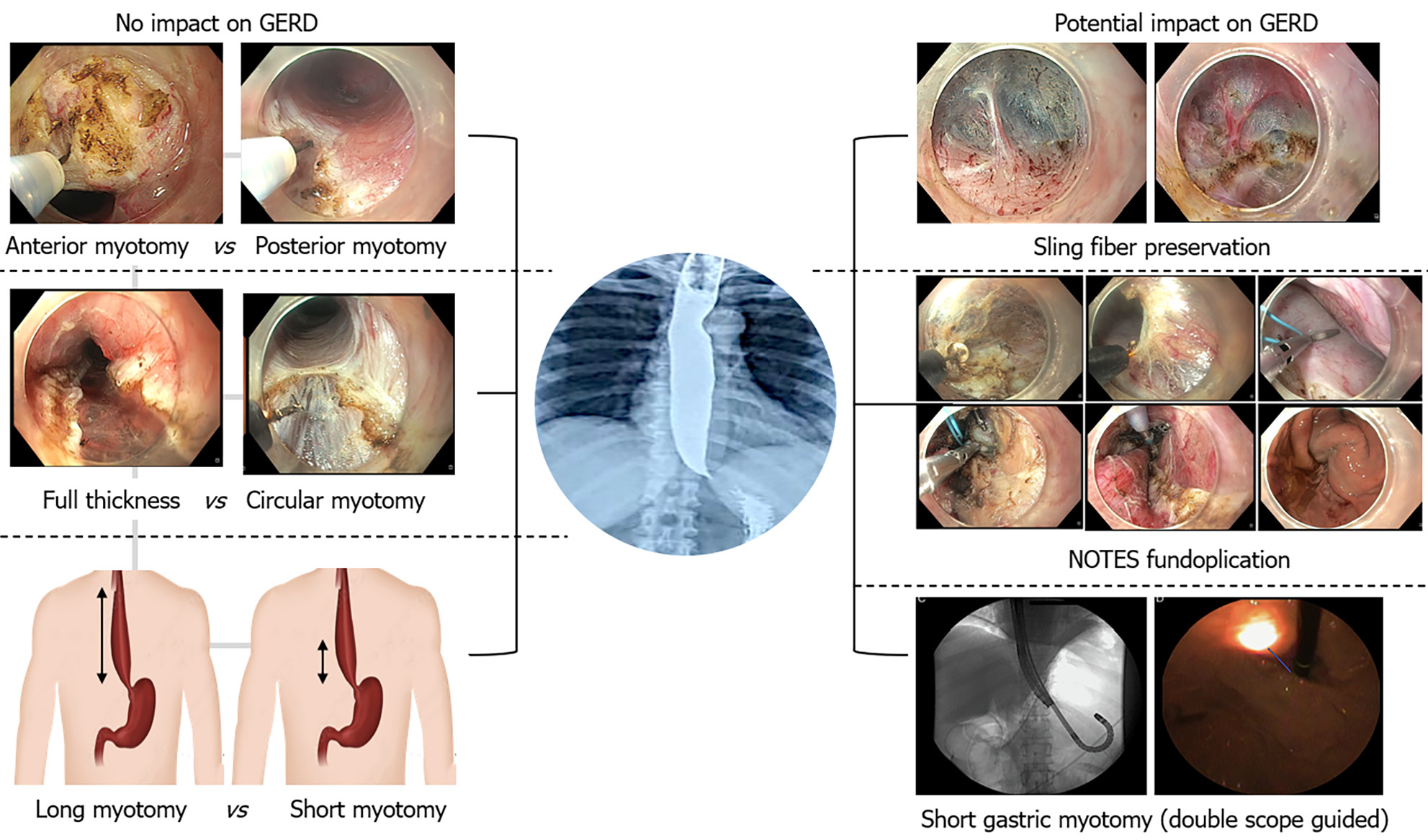
Given the high incidence of GERD after POEM, the development of preventative measures is of paramount importance. However, the current body of research concerning preventive approaches for GERD after POEM is limited. The preponderance of existing studies have focused on assessing the clinical effectiveness of modified POEM techniques with only a few dedicated to evaluating their impact on the incidence of post-operative GERD.
While the clinical effectiveness of short esophageal myotomy (≤ 5 cm) and selective circular myotomy has been established as comparable to standard esophageal myotomy and full-thickness myotomy, their effect on post-operative GERD remains unclear[23,32-34]. Theoretically, short esophageal myotomy might facilitate partial recovery of peristalsis, potentially leading to reduced esophageal acid exposure. However, robust data are required to substantiate this theory. A retrospective study involving 237 patients noted partial peristaltic recovery in 22% of patients after POEM[35]. Another study indicated a lower frequency of GERD symptoms and reflux esophagitis in patients exhibiting partial peristaltic recovery post-POEM, with preprocedural LES resting pressure and the Eckardt score predictive of this recovery[36]. However, these findings require confirmation through high-quality clinical trials.
The role of longitudinal esophageal muscles in both health and disease remains an area of ongoing research. Longitudinal muscles are thought to contribute to esophageal shortening and may be implicated in the genesis of chest pain in achalasia patients[37]. Interestingly, one study found a higher incidence of post-POEM reflux in cases who underwent full thickness myotomy[23]. However, this finding is contrasted by another study that reported differing results[38].
Overall, the prevention of GERD following POEM is a complex issue that requires further exploration and validation through well-designed research studies.
An extended gastric myotomy (3 cm vs 1.5 cm) has been shown to improve the results of LHM for achalasia[39]. However, LHM typically includes a concurrent fundoplication procedure. In contrast, fundoplication is not performed in conjunction with POEM, and consequently, longer gastric myotomies in the context of POEM may increase the risk of developing GERD. Grimes et al[22] assessed the impact of the gastric myotomy length on post POEM reflux[22]. They found that gastric myotomy extending beyond 2.5 cm was associated with increased rates of moderate esophagitis (LA grade B). The authors also advocated the utilization of a double scope method to precisely control the gastric myotomy length. This technique not only assists in determining the myotomy length, but also aids in assessing the myotomy orientation[40]. In a case control study, the incidence of reflux esophagitis was compared between patients with a short gastric myotomy (1 cm) and those with a standard gastric myotomy (2-3 cm)[41]. The study observed a significantly lower incidence of LA grade B or higher esophagitis in the short myotomy group (0% vs 30%, P = 0.01), along with lower mean GerdQ scores (6.5 vs 8.2, P = 0.001)[41].
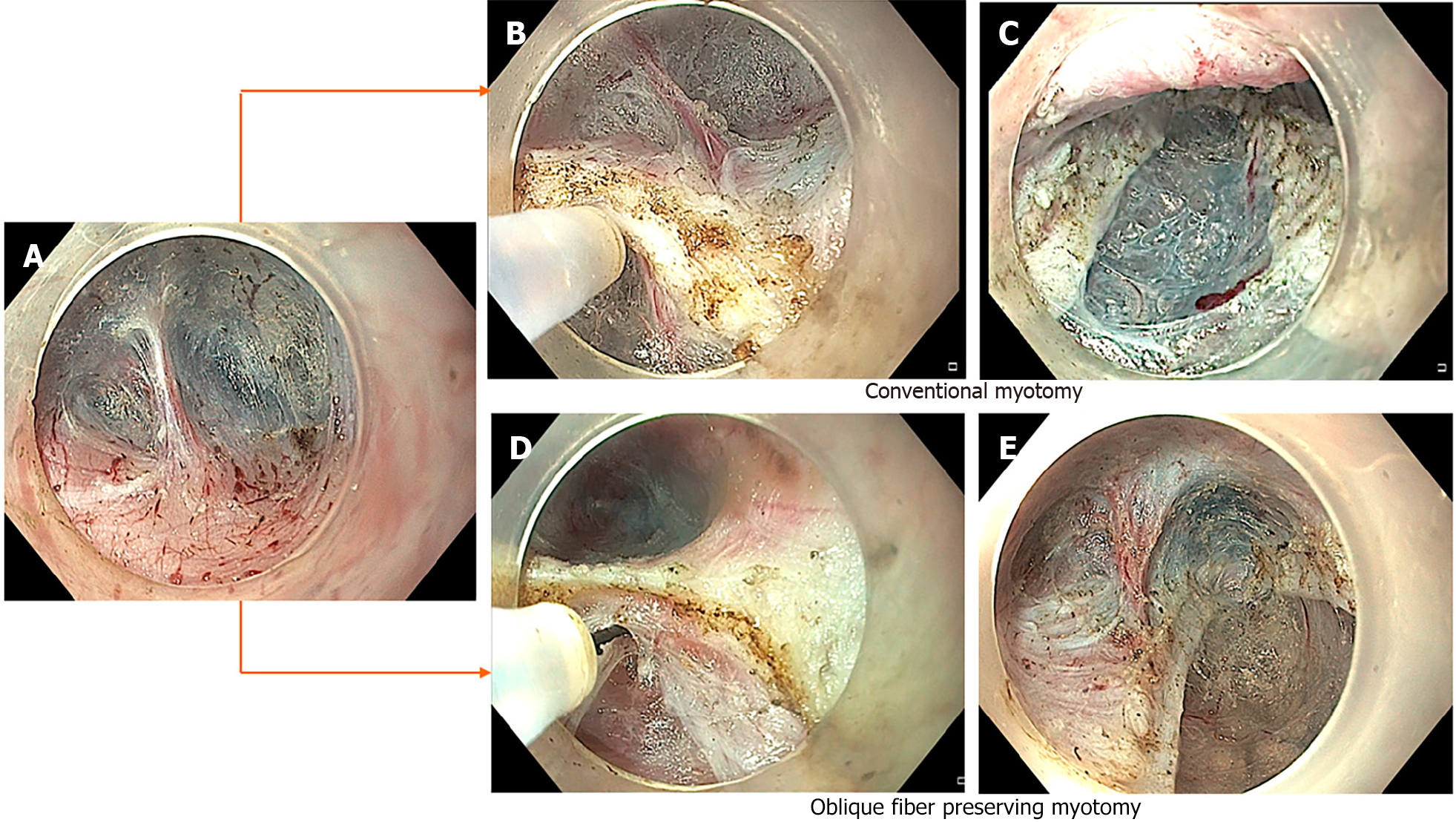
Other techniques for mitigating reflux involves preservation of sling fibers during posterior POEM and incorporating natural orifice transluminal endoscopic surgery fundoplication (NOTES-F) in anterior POEM. Sling fibers, crucial to the natural anti-reflux barrier, are visible towards the gastric side during posterior myotomy (Figure 2). Re-orienting the direction of myotomy during POEM can facilitate the preservation of these fibers. Tanaka et al[42] reported a significant reduction in the frequency of grade B or higher reflux esophagitis in cases where sling fibers were preserved during posterior POEM (31.3% vs 58.1%)[42]. Shiwaku et al[43] found that while overall rates of reflux esophagitis were similar between conventional and sling fiber preserving groups, severe esophagitis (LA grade C/D) was significantly less frequent in the latter (44.1% vs 18.5%)[43]. The gastroesophageal flap valve grade was better preserved in cases without severed sling fibers (4.4% vs 19.8%)[43]. In contrast, a randomized trial concluded that preserving sling fibers does not significantly impact post POEM reflux esophagitis[44]. This trial observed similar incidences of grade B or higher esophagitis (25.9% vs 31.6%), mean number of reflux episodes (48.2 ± 36.6 vs 48.9 ± 40.3), increased esophageal acid exposure (45.5% vs 31.7%) and high DeMeester scores (38.6% vs 41.5%) in both the groups.
Given that sling fibers cross the dissection field from left to right, performing a short gastric myotomy might be essential to preserve them[40]. Stavropoulos et al[45] highlighted this technique (anti-reflux POEM), where sling fibers are preserved by orienting the myotomy at 2 o’ clock and limiting the length of gastric myotomy[45]. The anti-reflux POEM group demonstrated significantly lower acid exposure (4.5% vs 10.3%, P < 0.001), fewer reflux episodes (31 vs 53, P = 0.02) and reduced GERD symptoms (5.2% vs 18.1%) compared to controls.
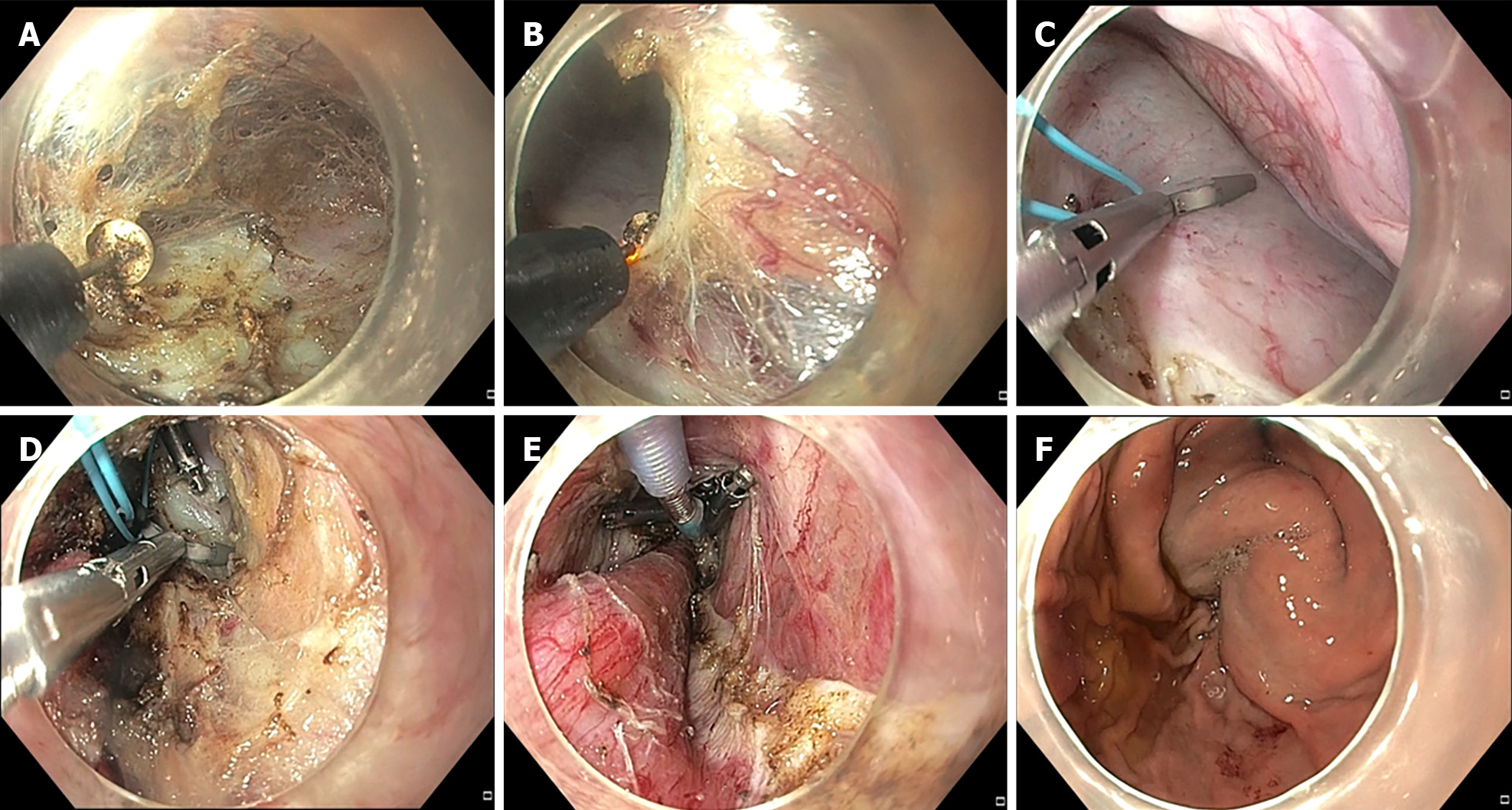
NOTES-F has gained attention as a preventive measure for GERD following POEM. This procedure involves performing an anterior myotomy followed by dissection along the serosal side to access the peritoneum. A peritoneal opening is created and the anterior surface of the stomach is accessed. The left lobe of liver serves as a landmark in the peritoneal cavity. The anterior stomach wall is then pulled towards the myotomy site using a forceps or an endoclip. A second slim endoscope within the gastric lumen confirms the wrap formation. The wrap is secured using several endoclips over an endoloop along the serosal aspect of stomach and distal end of the myotomy. Subsequently, the endoloop is tightened and the excess portion is trimmed using a loop cutter (Figure 3).
Inoue et al[46] demonstrated the safety and feasibility of creating a fundoplication wrap with anterior POEM using an endoloop and endoclips in a proof-of-concept study[46]. Bapaye et al[47] later reported sustained wrap integrity in 82.6% patients at a median follow-up of 12 months, with increased esophageal acid exposure and mild esophagitis in 11.1%, and 18.2% of patients, respectively[47]. Despite the safety and feasibility in case reports and small case series, concerns have arisen regarding the durability of wrap[48,49]. A retrospective study including 17 cases who underwent NOTES-F showed loosening of the fundal wrap in 29.4% and 41.2% patients at 1-month and 3 months, respectively[50]. This aligns with observations of progressive increase in the incidence of GERD after LHM with fundoplication due to loosening of the wrap[51,52]. Refinement in NOTES-F procedure remains an active research[53]. Given the low incidence of severe GERD (< 10%) post-POEM, selecting the appropriate candidates for this procedure and conducting quality studies with long-term follow-up are essential before routine clinical implementation.
Other modifications in POEM technique, such as anterior vs posterior myotomy, and variations in myotomy length or thickness, have not shown substantial impact on the incidence of GERD[32-34,38,54-56] (Figure 4).
Proton pump inhibitors (PPIs) are the primary treatment for GERD post-POEM. Studies show that post POEM reflux esophagitis responds well to PPIs and refractory GERD is distinctly uncommon after POEM[11,12,57]. In two large studies, the response to PPIs in cases with erosive esophagitis after POEM was 81.4% and 87%, respectively[11,12]. Importantly, non-compliance to PPIs was the major reason in cases with residual esophagitis, emphasizing the importance of compliance in managing post-POEM GERD.
Device assisted endoscopic fundoplication has been increasingly recognized as a viable approach for managing GERD following POEM[58-61]. A multicenter retrospective study explored the efficacy of transoral incisionless fundoplication in a cohort of 12 patients who developed GERD after POEM[61]. This study observed a marked reduction in the need for twice daily PPIs, alongside notable improvements in the frequency of daily symptoms and GERD Health-related Quality of Life scores, mean DeMeester scores, and mean percentage acid exposure time. In a separate randomized trial including 60 patients, Maydeo et al[62] evaluated the effectiveness of endoscopic full thickness plication (EFTP) using the GERDx device (G-SURG GmbH, Seeon-Seebruck, Germany) in cases with PPI dependent GERD after POEM[62]. At the 3-month follow-up, the study reported significant improvements in the EFTP group, with a notably higher proportion of patients exhibiting acid exposure time below 6% (69% vs 10.3%). Additionally, the median GERDQ scores were significantly better in the EFTP group. However, it's important to note that while these results are promising, the study did not find a significant improvement in esophagitis, and a substantial portion of the EFTP group (28%) continued to require PPIs for symptom management.
Electrical stimulation therapy (EST) has been effectively utilized for the treatment of GERD[63,64]. Emerging data suggest that EST of the LES may offer a potential therapeutic option for post POEM reflux[65,66]. In a porcine study, two electrical leads were implanted at the LES level and electrical stimulation applied with the Endostim system[65]. After myotomy, the LES pressure significantly dropped to 10.60 ± 3.24 mmHg (P = 0.03). Subsequent to electrical stimulation, there was a substantial increase in LES pressure to 21.74 ± 4.65 mmHg (P = 0.01). These findings suggest that EST could play a significant role in the management of GERD after POEM, highlighting its potential to augment LES function and mitigate reflux symptoms[65].
There is a significant body of research documenting the prevalence of GERD during brief follow-up, but long-term data on GERD progression and its consequences are relatively scarce. A large single-center study involving 610 patients reported the development of short segment Barrett’s esophagus and peptic strictures in a small number of cases (five patients each) within 2 to 6 years after POEM[12]. Similarly, others have also reported the development of Barrett’s esophagus as a sequelae to post POEM reflux. Notably, these long-term sequelae of GERD were predominantly observed in patients who were noncompliant with PPIs.
Emerging evidence indicates that both the incidence and severity of reflux may reduce over time after POEM[12,67]. In a study by Modayil et al[12], paired pH studies were conducted on 21 patients at a median of 5 months and 57 months after POEM[12]. They reported a significant reduction in the total number of refluxes (22 vs 66, P = 0.001), and DeMeester scores (21 vs 38, P = 0.03). Interestingly, 35% of patients with initially positive pH studies exhibited normalized results on long-term follow-up[12]. The authors proposed that this improvement might be attributed to remodeling of gastroesophageal junction over time, a hypothesis supported by paired endoluminal functional lumen imaging probe (EndoFLIP) studies showing increased LES pressure and reduced cross sectional area, distensibility, and compliance of gastroesophageal junction several months after POEM[12]. Further, a large multicenter Japanese study reported a significant decrease in the prevalence of symptomatic GERD at 5-year follow-up compared to 1-year after POEM[7]. This suggests a generally favorable natural course of post POEM reflux implying that conservative management may often be adequate. In two long-term follow-up studies by Simkova et al[67] and Nabi et al[68], the rates of symptomatic GERD and reflux esophagitis decreased over time, with a notable reduction in severe esophagitis (LA grades C/D). A recent systematic review and meta-analysis echoed these findings, showing a decrease in erosive esophagitis rates over time (28% at ≤ 6 months and 13% patients at ≥ 2years)[69]. The landmark randomized trial comparing POEM to LHM, reported a reduction in the incidence of reflux esophagitis from 57% at one year to 44% at 2-years after POEM. In contrast, an increase was observed in the LHM group over the same period. This pattern aligns with previous studies which report a progressive increase in acid reflux after LHM at long-term follow-up[52].
In summary, while the incidence of endoscopic reflux appears to diminish over time after POEM, vigilant follow-up remains crucial. Ensuring adherence to PPI therapy is essential, given the potential development of Barrett’s esophagus and peptic strictures as long-term complications of post-POEM reflux.
In the era of precision medicine, the traditional approach of arbitrarily choosing a myotomy length (especially gastric) during POEM is being re-evaluated. The advent of technologies like EndoFLIP is paving the way for more objective criteria in determining the length of myotomy. EndoFLIP facilitates intraoperative assessment of LES distensibility during POEM, enabling the tailoring of myotomies to achieve optimal distensibility while mitigating the risk of postoperative reflux[70]. The potential of intraoperative impedance planimetry in predicting GERD after POEM has been explored in recent studies. Attar and colleagues reported that patients with a distensibility index ≥ 2.7 and a final cross-sectional area ≥ 83 were more likely to develop esophagitis after POEM[71]. Similarly, post LHM distensibility index was higher in those who developed erosive esophagitis compared to those without esophagitis (9.3 vs 4.8 mm(2)/mmHg, P < 0.05)[72]. These studies suggest an association between EndoFLIP measurements and the risk of post-operative GERD. However, not all studies have confirmed the utility of EndoFLIP in predicting reflux after POEM, indicating a need for further high-quality research before its routine clinical application can be recommended. The future of POEM lies in integrating such advanced technologies with clinical practice, enhancing the precision and efficacy of treatments in esophageal motility disorders.
GERD is a frequent occurrence following POEM, with a higher incidence compared to PD and LHM. The effective identification of risk factors, the implementation of preventive measures, and timely intervention are essential to mitigate complications associated with prolonged esophageal acid exposure post-POEM. There has been considerable advancement in understanding the factors predisposing to GERD, as well as in the diagnostic and therapeutic approaches following POEM. While modifications to the POEM technique have been shown to maintain efficacy, their impact on reducing the incidence of GERD post-procedure has not been as promising. Conclusive evidence from high-quality research is needed before definitive conclusions can be drawn regarding the efficacy of these modified techniques in preventing GERD after POEM (Figure 5).
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lei JJ, China S-Editor: Fan JR L-Editor: A P-Editor: Yu HG
| 1. | Jung HK, Hong SJ, Lee OY, Pandolfino J, Park H, Miwa H, Ghoshal UC, Mahadeva S, Oshima T, Chen M, Chua ASB, Cho YK, Lee TH, Min YW, Park CH, Kwon JG, Park MI, Jung K, Park JK, Jung KW, Lim HC, Jung DH, Kim DH, Lim CH, Moon HS, Park JH, Choi SC, Suzuki H, Patcharatrakul T, Wu JCY, Lee KJ, Tanaka S, Siah KTH, Park KS, Kim SE; Korean Society of Neurogastroenterology and Motility. 2019 Seoul Consensus on Esophageal Achalasia Guidelines. J Neurogastroenterol Motil. 2020;26:180-203. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 66] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 2. | Khashab MA, Vela MF, Thosani N, Agrawal D, Buxbaum JL, Abbas Fehmi SM, Fishman DS, Gurudu SR, Jamil LH, Jue TL, Kannadath BS, Law JK, Lee JK, Naveed M, Qumseya BJ, Sawhney MS, Yang J, Wani S. ASGE guideline on the management of achalasia. Gastrointest Endosc. 2020;91:213-227.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 133] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 3. | Oude Nijhuis RAB, Zaninotto G, Roman S, Boeckxstaens GE, Fockens P, Langendam MW, Plumb AA, Smout A, Targarona EM, Trukhmanov AS, Weusten B, Bredenoord AJ. European guidelines on achalasia: United European Gastroenterology and European Society of Neurogastroenterology and Motility recommendations. United European Gastroenterol J. 2020;8:13-33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 126] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 4. | Vaezi MF, Pandolfino JE, Yadlapati RH, Greer KB, Kavitt RT. ACG Clinical Guidelines: Diagnosis and Management of Achalasia. Am J Gastroenterol. 2020;115:1393-1411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 235] [Article Influence: 47.0] [Reference Citation Analysis (0)] |
| 5. | Nabi Z, Ramchandani M, Reddy DN. Per-oral endoscopic myotomy and gastroesophageal reflux: Where do we stand after a decade of "POETRY"? Indian J Gastroenterol. 2019;38:287-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 6. | Kumbhari V, Familiari P, Bjerregaard NC, Pioche M, Jones E, Ko WJ, Hayee B, Cali A, Ngamruengphong S, Mion F, Hernaez R, Roman S, Tieu AH, El Zein M, Ajayi T, Haji A, Cho JY, Hazey J, Perry KA, Ponchon T, Kunda R, Costamagna G, Khashab MA. Gastroesophageal reflux after peroral endoscopic myotomy: a multicenter case-control study. Endoscopy. 2017;49:634-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 124] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 7. | Shiwaku H, Sato H, Shimamura Y, Abe H, Shiota J, Sato C, Ominami M, Sakae H, Hata Y, Fukuda H, Ogawa R, Nakamura J, Tatsuta T, Ikebuchi Y, Yokomichi H, Hasegawa S, Inoue H. Risk factors and long-term course of gastroesophageal reflux disease after peroral endoscopic myotomy: A large-scale multicenter cohort study in Japan. Endoscopy. 2022;54:839-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 32] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 8. | Werner YB, Hakanson B, Martinek J, Repici A, von Rahden BHA, Bredenoord AJ, Bisschops R, Messmann H, Vollberg MC, Noder T, Kersten JF, Mann O, Izbicki J, Pazdro A, Fumagalli U, Rosati R, Germer CT, Schijven MP, Emmermann A, von Renteln D, Fockens P, Boeckxstaens G, Rösch T. Endoscopic or Surgical Myotomy in Patients with Idiopathic Achalasia. N Engl J Med. 2019;381:2219-2229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 398] [Cited by in RCA: 344] [Article Influence: 57.3] [Reference Citation Analysis (1)] |
| 9. | Ponds FA, Fockens P, Lei A, Neuhaus H, Beyna T, Kandler J, Frieling T, Chiu PWY, Wu JCY, Wong VWY, Costamagna G, Familiari P, Kahrilas PJ, Pandolfino JE, Smout AJPM, Bredenoord AJ. Effect of Peroral Endoscopic Myotomy vs Pneumatic Dilation on Symptom Severity and Treatment Outcomes Among Treatment-Naive Patients With Achalasia: A Randomized Clinical Trial. JAMA. 2019;322:134-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 259] [Article Influence: 43.2] [Reference Citation Analysis (0)] |
| 10. | Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1168] [Cited by in RCA: 1234] [Article Influence: 82.3] [Reference Citation Analysis (1)] |
| 11. | Nabi Z, Ramchandani M, Kotla R, Tandan M, Goud R, Darisetty S, Rao GV, Reddy DN. Gastroesophageal reflux disease after peroral endoscopic myotomy is unpredictable, but responsive to proton pump inhibitor therapy: a large, single-center study. Endoscopy. 2020;52:643-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 12. | Modayil RJ, Zhang X, Rothberg B, Kollarus M, Galibov I, Peller H, Taylor S, Brathwaite CE, Halwan B, Grendell JH, Stavropoulos SN. Peroral endoscopic myotomy: 10-year outcomes from a large, single-center U.S. series with high follow-up completion and comprehensive analysis of long-term efficacy, safety, objective GERD, and endoscopic functional luminal assessment. Gastrointest Endosc. 2021;94:930-942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 57] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 13. | Karyampudi A, Nabi Z, Ramchandani M, Darisetty S, Goud R, Chavan R, Kalapala R, Rao GV, Reddy DN. Gastroesophageal reflux after per-oral endoscopic myotomy is frequently asymptomatic, but leads to more severe esophagitis: A case-control study. United European Gastroenterol J. 2021;9:63-71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 14. | Hungness ES, Sternbach JM, Teitelbaum EN, Kahrilas PJ, Pandolfino JE, Soper NJ. Per-oral Endoscopic Myotomy (POEM) After the Learning Curve: Durable Long-term Results With a Low Complication Rate. Ann Surg. 2016;264:508-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 109] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 15. | Akhtar N, Yaghnam I, Mikhail D, Klombers S, Razjouyan H, Abraham M. Increase in body mass index is an important predictor of developing gastroesophageal reflux disease (GERD) after per-oral endoscopic myotomy (POEM). Gastrointest Endosc. 2023;97:AB982. [DOI] [Full Text] |
| 16. | Rassoul Abu-Nuwar M, Eriksson SE, Sarici IS, Zheng P, Hoppo T, Jobe BA, Ayazi S. GERD after Peroral Endoscopic Myotomy: Assessment of Incidence and Predisposing Factors. J Am Coll Surg. 2023;236:58-70. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 15] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 17. | Abu-Nuwar MR, Eriksson S, Zheng P, Jobe B, Ayazi S. Gastroesophageal Reflux after Peroral Endoscopic Myotomy: An Assessment of Incidence and Predisposing Factor. J Am Coll Surg. 2022;235:S22. [RCA] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 18. | Benedict JJ, Golas AA, Richter JE, Velanovich V. Health-Related Quality of Life and Physiological Outcomes of Peroral Endoscopic Myotomy for Achalasia. J Laparoendosc Adv Surg Tech A. 2017;27:778-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Familiari P, Greco S, Gigante G, Calì A, Boškoski I, Onder G, Perri V, Costamagna G. Gastroesophageal reflux disease after peroral endoscopic myotomy: Analysis of clinical, procedural and functional factors, associated with gastroesophageal reflux disease and esophagitis. Dig Endosc. 2016;28:33-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 83] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 20. | Ward MA, Whitfield EP, Hasan SS, Ogola GO, Leeds SG. Objectively Confirmed Gastroesophageal Reflux Disease Following Per Oral Endoscopic Myotomy Higher in Obese Patients (BMI>30). Surg Laparosc Endosc Percutan Tech. 2020;31:146-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | Sanaka MR, Parikh MP, Subramanium S, Thota PN, Gupta NM, Lopez R, Gabbard S, Murthy S, Raja S. Obesity Does Not Impact Outcomes or Rates of Gastroesophageal Reflux After Peroral Endoscopic Myotomy in Achalasia. J Clin Gastroenterol. 2020;54:338-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Grimes KL, Bechara R, Shimamura Y, Ikeda H, Inoue H. Gastric myotomy length affects severity but not rate of post-procedure reflux: 3-year follow-up of a prospective randomized controlled trial of double-scope per-oral endoscopic myotomy (POEM) for esophageal achalasia. Surg Endosc. 2020;34:2963-2968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 23. | Wang XH, Tan YY, Zhu HY, Li CJ, Liu DL. Full-thickness myotomy is associated with higher rate of postoperative gastroesophageal reflux disease. World J Gastroenterol. 2016;22:9419-9426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 64] [Cited by in RCA: 55] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 24. | Lyons J, Boutros C, Khan SZ, Benson J, Hashimoto DA, Marks J. Preoperative patient factors and anatomy do not predict who will develop reflux after per oral endoscopic myotomy. Surg Endosc. 2023;37:7178-7182. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 25. | Srinivasan S, Radadiya D, Patel H, Perisetti A, Chandrasekar VT, Desai M, Repici A, Hassan C, Duvvur N, Sharma P. Post-per-oral endoscopic myotomy (POEM) GERD: A systematic evaluation and meta-analysis. Gastrointest Endosc. 2023;97:AB971. [DOI] [Full Text] |
| 26. | Visaggi P, Del Corso G, Gyawali CP, Ghisa M, Baiano Svizzero F, Stefani Donati D, Venturini A, Savarino V, Penagini R, Zeki S, Bellini M, Savarino EV, de Bortoli N. Ambulatory pH-Impedance Findings Confirm That Grade B Esophagitis Provides Objective Diagnosis of Gastroesophageal Reflux Disease. Am J Gastroenterol. 2023;118:794-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 29] [Reference Citation Analysis (0)] |
| 27. | Crookes PF, Corkill S, DeMeester TR. Gastroesophageal reflux in achalasia. When is reflux really reflux? Dig Dis Sci. 1997;42:1354-1361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 80] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 28. | Smart HL, Foster PN, Evans DF, Slevin B, Atkinson M. Twenty four hour oesophageal acidity in achalasia before and after pneumatic dilatation. Gut. 1987;28:883-887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 57] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Ponds FA, Oors JM, Smout AJPM, Bredenoord AJ. Reflux symptoms and oesophageal acidification in treated achalasia patients are often not reflux related. Gut. 2021;70:30-39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 42] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 30. | Bechara R, Inoue H, Shimamura Y, Reed D. Gastroesophageal reflux disease after peroral endoscopic myotomy: lest we forget what we already know. Dis Esophagus. 2019;32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 31. | Singh AP, Singla N, Budhwani E, Januszewicz W, Memon SF, Inavolu P, Nabi Z, Jagtap N, Kalapala R, Lakhtakia S, Darisetty S, Reddy DN, Ramchandani M. Defining "true acid reflux" after peroral endoscopic myotomy for achalasia: a prospective cohort study. Gastrointest Endosc. 2024;99:166-173.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 3] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 32. | Gu L, Ouyang Z, Lv L, Liang C, Zhu H, Liu D. Safety and efficacy of peroral endoscopic myotomy with standard myotomy versus short myotomy for treatment-naïve patients with type II achalasia: a prospective randomized trial. Gastrointest Endosc. 2021;93:1304-1312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 44] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 33. | Nabi Z, Ramchandani M, Sayyed M, Chavan R, Darisetty S, Goud R, Murthy HVV, Reddy DN. Comparison of Short Versus Long Esophageal Myotomy in Cases With Idiopathic Achalasia: A Randomized Controlled Trial. J Neurogastroenterol Motil. 2021;27:63-70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 60] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 34. | Familiari P, Borrelli de Andreis F, Landi R, Mangiola F, Boskoski I, Tringali A, Perri V, Costamagna G. Long versus short peroral endoscopic myotomy for the treatment of achalasia: results of a non-inferiority randomised controlled trial. Gut. 2023;72:1442-1450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 29] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 35. | Vackova Z, Mares J, Krajciova J, Rabekova Z, Zdrhova L, Loudova P, Spicak J, Stirand P, Hucl T, Martinek J. Esophageal Motility Patterns After Peroral Endoscopic Myotomy in Patients With Achalasia. J Neurogastroenterol Motil. 2021;27:205-214. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 36. | Shi LL, Yang T, Jiang N, Lyu Y, Guo HM, Yang H, Yin Q, Zou XP, Zhang NN. A comprehensive analysis of partial peristalsis recovery after peroral endoscopic myotomy in patients with achalasia. J Dig Dis. 2023;24:224-230. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 37. | Mittal RK, Hong SJ, Bhargava V. Longitudinal muscle dysfunction in achalasia esophagus and its relevance. J Neurogastroenterol Motil. 2013;19:126-136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 38. | Li C, Gong A, Zhang J, Duan Z, Ge L, Xia N, Leng J, Li M, Liu Y. Clinical Outcomes and Safety of Partial Full-Thickness Myotomy versus Circular Muscle Myotomy in Peroral Endoscopic Myotomy for Achalasia Patients. Gastroenterol Res Pract. 2017;2017:2676513. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 39. | Oelschlager BK, Chang L, Pellegrini CA. Improved outcome after extended gastric myotomy for achalasia. Arch Surg. 2003;138:490-5; discussion 495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 191] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 40. | Inoue H, Shiwaku H, Kobayashi Y, Chiu PWY, Hawes RH, Neuhaus H, Costamagna G, Stavropoulos SN, Fukami N, Seewald S, Onimaru M, Minami H, Tanaka S, Shimamura Y, Santi EG, Grimes K, Tajiri H. Statement for gastroesophageal reflux disease after peroral endoscopic myotomy from an international multicenter experience. Esophagus. 2020;17:3-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 41. | Farina D, Olson DA, Carlson D, Kahrilas PJ, Pandolfino JE, Aadam AA. Impact of a short gastric myotomy on gastroesophageal reflux following per-oral endoscopic myotomy (POEM). Gastrointest Endosc. 2022;95:AB403-AB404. [DOI] [Full Text] |
| 42. | Tanaka S, Toyonaga T, Kawara F, Watanabe D, Hoshi N, Abe H, Ariyoshi R, Ohara Y, Takao T, Morita Y, Umegaki E, Kodama Y. Novel per-oral endoscopic myotomy method preserving oblique muscle using two penetrating vessels as anatomic landmarks reduces postoperative gastroesophageal reflux. J Gastroenterol Hepatol. 2019;34:2158-2163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 43. | Shiwaku H, Inoue H, Shiwaku A, Okada H, Hasegawa S. Safety and effectiveness of sling fiber preservation POEM to reduce severe post-procedural erosive esophagitis. Surg Endosc. 2022;36:4255-4264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 24] [Article Influence: 8.0] [Reference Citation Analysis (1)] |
| 44. | Nabi Z, Chandran V, Basha J, Ramchandani M, Inavolu P, Kalpala R, Goud R, Jagtap N, Darisetty S, Gupta R, Tandan M, Lakhtakia S, Kotla R, Devarasetty R, Rao GV, Reddy DN. Conventional versus oblique fiber-sparing endoscopic myotomy for achalasia cardia: a randomized controlled trial (with videos). Gastrointest Endosc. 2024;99:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 45. | Stavropoulos SN, Modayil RJ, Zhang X, Omrani LR, Islam S, Kollarus M, Taylor S, Widmer JL, Grendell JH. The "Anti-reflux" poem: A technique modification that drastically reduces objectively measured reflux after per-oral endoscopic myotomy (POEM). Gastrointest Endosc. 2022;95:AB400. [DOI] [Full Text] |
| 46. | Inoue H, Ueno A, Shimamura Y, Manolakis A, Sharma A, Kono S, Nishimoto M, Sumi K, Ikeda H, Goda K, Onimaru M, Yamaguchi N, Itoh H. Peroral endoscopic myotomy and fundoplication: a novel NOTES procedure. Endoscopy. 2019;51:161-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 94] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 47. | Bapaye A, Dashatwar P, Dharamsi S, Pujari R, Gadhikar H. Single-session endoscopic fundoplication after peroral endoscopic myotomy (POEM+F) for prevention of post gastroesophageal reflux - 1-year follow-up study. Endoscopy. 2021;53:1114-1121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 48. | Shrigiriwar A, Zhang LY, Ghandour B, Bejjani M, Mony S, Bapaye A, Khashab MA. Technical details and outcomes of peroral endoscopic myotomy with fundoplication: the first U.S. experience (with video). Gastrointest Endosc. 2023;97:585-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 49. | Mandavdhare HS, Samanta J, Varma P, Praveen Kumar-M, Gupta P, Singh H, Dutta U, Kochhar R. Per oral endoscopic myotomy with fundoplication is a technically feasible NOTES for achalasia cardia. Minim Invasive Ther Allied Technol. 2022;31:319-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 50. | Patil G, Dalal A, Maydeo A. Early outcomes of peroral endoscopic myotomy with fundoplication for achalasia cardia - Is it here to stay? Dig Endosc. 2021;33:561-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 51. | Ortiz A, de Haro LF, Parrilla P, Lage A, Perez D, Munitiz V, Ruiz D, Molina J. Very long-term objective evaluation of heller myotomy plus posterior partial fundoplication in patients with achalasia of the cardia. Ann Surg. 2008;247:258-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 52. | Csendes A, Braghetto I, Burdiles P, Korn O, Csendes P, Henríquez A. Very late results of esophagomyotomy for patients with achalasia: clinical, endoscopic, histologic, manometric, and acid reflux studies in 67 patients for a mean follow-up of 190 months. Ann Surg. 2006;243:196-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 138] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 53. | Toshimori A, Inoue H, Shimamura Y, Abad MRA, Onimaru M. Peroral endoscopic fundoplication: a brand-new intervention for GERD. VideoGIE. 2020;5:244-246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 54. | Tan Y, Lv L, Wang X, Zhu H, Chu Y, Luo M, Li C, Zhou H, Huo J, Liu D. Efficacy of anterior versus posterior per-oral endoscopic myotomy for treating achalasia: a randomized, prospective study. Gastrointest Endosc. 2018;88:46-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (1)] |
| 55. | Khashab MA, Sanaei O, Rivory J, Eleftheriadis N, Chiu PWY, Shiwaku H, Ogihara K, Ismail A, Abusamaan MS, El Zein MH, Wong VW, Billioux VG, Kumbhari V, Kalloo AN, Ponchon T, Pioche M. Peroral endoscopic myotomy: anterior versus posterior approach: a randomized single-blinded clinical trial. Gastrointest Endosc. 2020;91:288-297.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 56. | Li QL, Chen WF, Zhou PH, Yao LQ, Xu MD, Hu JW, Cai MY, Zhang YQ, Qin WZ, Ren Z. Peroral endoscopic myotomy for the treatment of achalasia: a clinical comparative study of endoscopic full-thickness and circular muscle myotomy. J Am Coll Surg. 2013;217:442-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 124] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 57. | Shiwaku H, Inoue H, Sasaki T, Yamashita K, Ohmiya T, Takeno S, Nimura S, Yamashita Y. A prospective analysis of GERD after POEM on anterior myotomy. Surg Endosc. 2016;30:2496-2504. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 58. | Tyberg A, Choi A, Gaidhane M, Kahaleh M. Transoral incisional fundoplication for reflux after peroral endoscopic myotomy: a crucial addition to our arsenal. Endosc Int Open. 2018;6:E549-E552. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 53] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 59. | Keihanian T, Zabad N, Mercado MO, Abidi W, Patel K, Othman M, Jawaid S. Feasibility and efficacy of transoral incisionless fundoplication in management of post per oral endoscopic myotomy gastroesophageal reflux disease: A prospective single center study. Gastrointest Endosc. 2023;97:AB1113-AB1114. [DOI] [Full Text] |
| 60. | Dewitt J, Al-Haddad M, Stainko S, Perkins A, Fatima H, Birdas T. Transoral incisionless fundoplication with or without laparoscopic hiatal hernia repair for treatment OF gastroesophageal reflux disease after peroral endoscopic myotomy. Gastrointest Endosc. 2023;97:AB996. [DOI] [Full Text] |
| 61. | Brewer Gutierrez OI, Chang KJ, Benias PC, Sedarat A, Dbouk MH, Godoy Brewer G, Lee DP, Okolo Iii PI, Canto MI, Khashab MA. Is transoral incisionless fundoplication (TIF) an answer to post-peroral endoscopic myotomy gastroesophageal reflux? A multicenter retrospective study. Endoscopy. 2022;54:305-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 17] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 62. | Maydeo A, Patil G, Kamat N, Dalal A, Vadgaonkar A, Parekh S, Daftary R, Vora S. Endoscopic full-thickness plication for the treatment of gastroesophageal reflux after peroral endoscopic myotomy: a randomized sham-controlled study. Endoscopy. 2023;55:689-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 63. | Rodríguez L, Rodriguez P, Gómez B, Ayala JC, Saba J, Perez-Castilla A, Galvao Neto M, Crowell MD. Electrical stimulation therapy of the lower esophageal sphincter is successful in treating GERD: final results of open-label prospective trial. Surg Endosc. 2013;27:1083-1092. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 64. | Rodríguez L, Rodriguez PA, Gómez B, Netto MG, Crowell MD, Soffer E. Electrical stimulation therapy of the lower esophageal sphincter is successful in treating GERD: long-term 3-year results. Surg Endosc. 2016;30:2666-2672. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 65. | Ciotola F, Ditaranto A, Bilder C, Badaloni A, Lowenstein D, Riganti JM, Hoppo T, Jobe B, Nachman F, Nieponice A. Electrical stimulation to increase lower esophageal sphincter pressure after POEM. Surg Endosc. 2015;29:230-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 66. | Rieder E, Paireder M, Kristo I, Schwameis K, Schoppmann SF. Electrical Stimulation of the Lower Esophageal Sphincter to Treat Gastroesophageal Reflux After POEM. Surg Innov. 2018;25:346-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 67. | Simkova D, Vackova Z, Mares J, Hugova K, Hucl T, Stirand P, Hustak R, Spicak J, Martinek J. Gastroesophageal reflux and its sequelae after per-oral endoscopic myotomy (POEM). Gastrointest Endosc. 2023;97:AB1085. [DOI] [Full Text] |
| 68. | Nabi Z, Karyampudi A, Ramchandani M, Chavan R, Basha J, Inavolu P, Darisetty S, Goud R, Reddy DN. Predictors of Long-Term Outcomes, Recurrent Dysphagia, and Gastroesophageal Reflux After Per-oral Endoscopic Myotomy in Esophageal Motility Disorders. J Gastrointest Surg. 2022;26:1352-1361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 69. | Nabi Z, Mandavdhare H, Akbar W, Talukdar R, Reddy DN. Long-term Outcome of Peroral Endoscopic Myotomy in Esophageal Motility Disorders: A Systematic Review and Meta-analysis. J Clin Gastroenterol. 2023;57:227-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 70. | Knight W, Kandiah K, Vrakopoulou Z, White A, Barbieri L, Tewari N, Couch J, DiMaggio F, Barley M, Ragunath K, Catton J, Botha A. Early outcomes following EndoFLIP-tailored peroral endoscopic myotomy (POEM): the establishment of POEM services in two UK centers. Dis Esophagus. 2023;36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 71. | Attaar M, Su B, Wong HJ, Kuchta K, Denham W, Haggerty SP, Linn J, Ujiki MB. Intraoperative impedance planimetry (EndoFLIP™) results and development of esophagitis in patients undergoing peroral endoscopic myotomy (POEM). Surg Endosc. 2021;35:4555-4562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 72. | Holmstrom AL, Campagna RJ, Carlson DA, Pandolfino JE, Soper NJ, Hungness ES, Teitelbaum EN. Comparison of preoperative, intraoperative, and follow-up functional luminal imaging probe measurements in patients undergoing myotomy for achalasia. Gastrointest Endosc. 2021;94:509-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |