INTRODUCTION
In Pérez-Holanda’s editorial[1], the author discussed the research of Agatsuma et al[2]. The work by Agatsuma et al[2] showed that despite evidence that early colorectal cancer (CRC) detection is beneficial, up to 50% of candidates reject this option through screening of asymptomatic subjects, and many affected patients are diagnosed at an advanced stage. Early diagnosis is essential for successful treatment of cancer. Numerous clinical studies have shown that early detection, diagnosis and treatment can result in the cure of certain cancers[3,4]. To date, there is no effective cure for advanced cancer. Therefore, cancer treatment should prioritize preventive measures to ensure early detection and diagnosis. This approach provides a reliable foundation for effective treatment and is a crucial factor in reducing mortality rates.
CRC is one of the most common malignant tumors worldwide[5]. The latest GLOBOCAN data showed that CRC incidence and mortality in 2022 ranked third and second, respectively, among global malignancies[6]. The early diagnosis of CRC should be prioritized. The effectiveness and compliance of diagnostic methods have a certain impact on whether people would choose screening. In this editorial, we explore strategies for the early diagnosis of CRC.
EARLY DIAGNOSTIC STRATEGIES FOR CRC
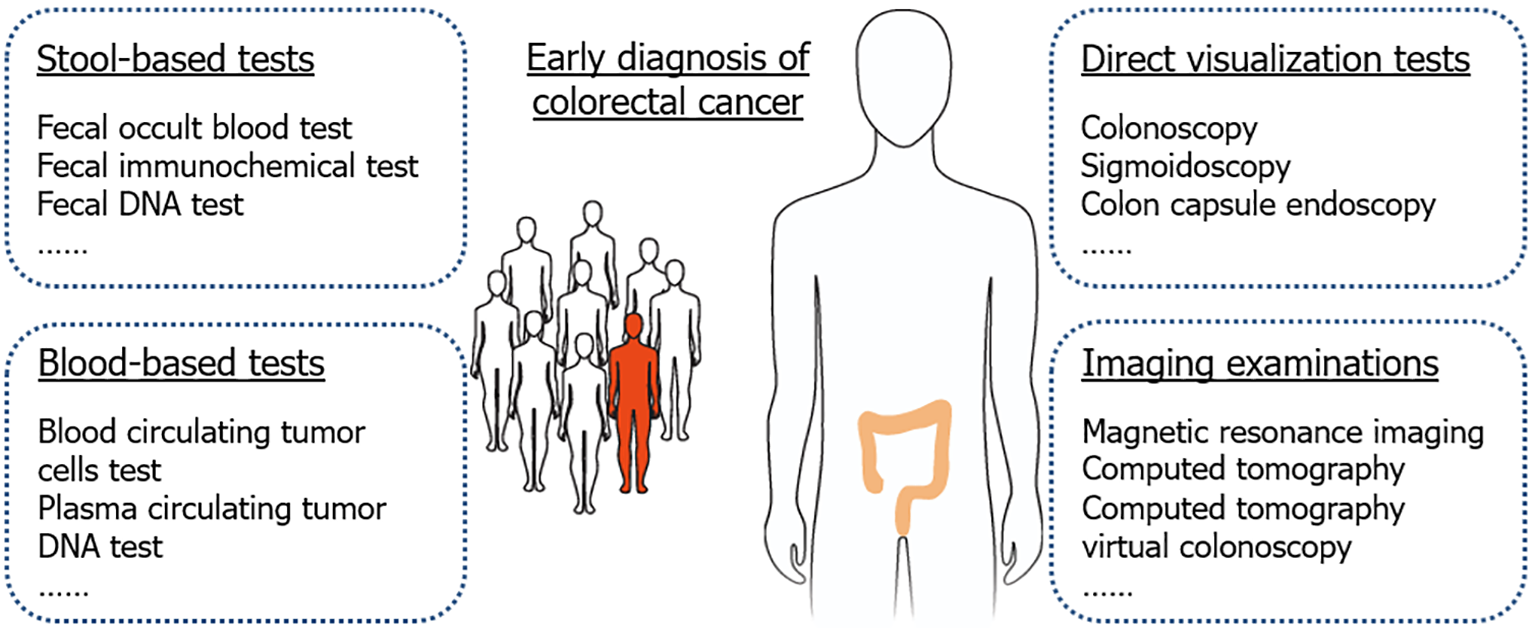
At present, the main methods for early diagnosis of CRC include stool-based tests, blood-based tests, direct visualization tests, and imaging examinations (Figure 1).
Figure 1 The main methods for early diagnosis of colorectal cancer.
Stool-based tests
The fecal occult blood test (FOBT) is a common method for the early diagnosis of CRC. The FOBT can lower mortality in CRC patients. However, due to its low detection sensitivity, it does not decrease the incidence of CRC[7]. In addition, the results of the FOBT are highly susceptible to dietary interference, leading to an increase in the false positive rate. Therefore, the FOBT has been gradually replaced by the fecal immunochemical test (FIT).
By using the principle of the human hemoglobin antigen antibody reaction, the FIT can overcome the deficiencies of the FOBT, avoid the influence of food and other factors, and significantly improve the sensitivity, specificity and positive predictive value of diagnostic results. This has resulted in the FIT being recommended by several guidelines worldwide for the early diagnosis of CRC. Studies have shown that the sensitivity of the FIT in the diagnosis of CRC is 73.8%, but its sensitivity in the detection of advanced precancerous lesions is low, generally only 23.8%[8].
The fecal DNA test mainly targets gene mutations and/or methylation in shed colorectal cells, and can also be combined with the FIT. Currently, the multi-target stool FIT-DNA test (Cologuard) is approved by the United States food and drug administration (FDA) for CRC screening and has a higher sensitivity than the FIT (92.3% vs 73.8%)[8]. Cologuard technology analyzes the hemoglobin content of stool samples, multiple DNA methylation and mutation markers, and the total amount of human DNA contained in cells shed by CRC or precancerous lesions. In 2019, exact sciences launched the BLUE-C study with the Mayo Clinic to improve Cologuard laboratory processes to achieve the goal of improving Cologuard’s performance. At present, the CRC detection sensitivity of Cologuard 2.0 has been improved to 94%, and exact sciences is applying for FDA approval for marketing[9]. However, the main drawback of fecal DNA testing for early CRC screening in the population at this stage is that the price is relatively high, and it is unrealistic for application in large-scale population screening.
Blood-based tests
Liquid biopsies overcome many of the limitations of tissue biopsies, and blood-based tests to detect circulating tumor cells (CTC) and circulating tumor DNA (ctDNA) are the most widely studied. Compared with tissue biopsy, CTC and ctDNA detection has the advantages of being non-invasive or minimally invasive, repeatable detection, high sensitivity and specificity, which can provide real-time information on the disease status of CRC patients, and contribute to the early diagnosis, prognosis assessment and treatment response monitoring of CRC[10,11]. One of the targets of the plasma ctDNA test is gene mutation. However, due to the fact that the mutation rate of a single gene associated with CRC is usually less than 60%, it is difficult to achieve the purpose of screening and diagnosis through the detection of a single gene mutation. Next-generation sequencing can detect multiple gene mutations simultaneously. However, due to the high cost, there are still many obstacles to further expansion of application. Another ideal target for the plasma ctDNA test is gene methylation, for example, the methylate SEPT9 gene in plasma ctDNA samples has been approved by the FDA for early diagnosis of CRC[12]. Bao et al[13] studied cell-free DNA fragmentomics of various types of cancer, including CRC, and developed a cancer early detection model using different algorithms. In addition to the above targets, a research team has integrated multi-modal information of ctDNA (including genomics, epigenomics, fragmentomics and proteomics) for early diagnosis of CRC, with detection sensitivity and specificity of 93% and 90%, respectively[14]. Recently, the ECLIPSE study validated Shield as an easy-to-perform, highly sensitive CRC screening blood test with 83% sensitivity and 90% specificity[15]. In late July this year, Guardant Health announced that Shield was approved by the FDA. Shield is first blood test approved by FDA as a screening option for CRC (https://investors.guardanthealth.com/press-releases/press-releases/2024/Guardant-Healths-Shield-Blood-Test-Approved-by-FDA-as-a-Primary-Screening-Option-Clearing-Path-for-Medicare-Reimbursement-and-a-New-Era-of-Colorectal-Cancer-Screening/default.aspx). Compared to Cologuard, Shield has an advantage in compliance, but not in performance. In the field of CRC early screening, compliance is an unavoidable topic. The reason is that the “gold standard” proctoscopy procedure is painful for most patients.
Compared to the FIT, the fecal multi-target DNA test and blood-based test have greater advantages in the early diagnosis of CRC, but their high cost limits their widespread application in large-scale population screening. Compared with the examination of fecal samples, plasma ctDNA can not only be used as a means of screening and diagnosis, but can also be applied in the dynamic monitoring of postoperative recurrence of CRC, which has the advantage of whole-process management.
Direct visualization tests
Colonoscopy has a unique and irreplaceable position in the diagnosis of CRC, and is the core link in the entire CRC early diagnostic process. A few developed countries use colonoscopy for one-step screening, but due to its poor compliance and high cost, most countries, including China, use colonoscopy as a follow-up confirmatory test for all those who test positive at first screening[16].
Sigmoidoscopy screening can significantly decrease the incidence and mortality of CRC in the population; however, due to its inherent limitations, sigmoidoscopy cannot visualize the proximal colon, potentially leading to missed diagnoses of proximal CRC. In addition, the lack of sedation and fear of pain are barriers to participation with flexible sigmoidoscopy[17].
Colon capsule endoscopy (CCE) has the advantages of less pain and convenience for patients. At present, some studies have attempted to use CCE for early diagnosis of CRC[18]. A barrier to CCE is the requirement of colon preparation, especially if the colonoscopy cannot be performed on the same day. Artificial intelligence and machine learning are particularly promising in CCE, with the potential for autonomous testing and can be combined with genomic or proteomic screening[19].
Imaging examinations
Magnetic resonance imaging (MRI), as the preferred staging tool for early CRC, has high accuracy in tumor localization, determining the scope of resection, and determining the relationship between tumor and peritoneal recursion[20]. MRI has the characteristics of high resolution, no ionizing radiation, high safety and high accuracy, and can clearly show the infiltration of cancer cells and the relationship with the surrounding tissue structure, and is an important imaging method for the diagnosis of CRC. The technology is promising, but more large-scale studies are needed.
Computed tomography (CT) offers high-density resolution. When combined with a contrast agent, CT can clearly display the cross-section of the colorectal wall, accurately assess its thickness and pathological morphology, and effectively show the surrounding areas outside the colorectal wall. Therefore, CT examination can provide valuable information regarding invasion of the intestinal wall, the extent of the spread outside the wall, whether the local lymph nodes are enlarged, and whether distant metastasis is present, etc., which can help determine the preoperative stage of CRC and provide a basis for selecting the appropriate treatment approach[21]. CT images can show the lymph nodes around the primary focus and the drainage area, but cannot show the internal structure of the lymph nodes, and the size is only used as the criterion to judge metastasis, which has certain limitations.
CT virtual colonoscopy refers to the method of diagnosing intestinal tumors by obtaining three-dimensional images of the colorectal region through simulated imaging of abdominal high-precision CT examination after intestinal cleaning[22]. This method requires intestinal preparation, relatively complicated operation, expensive examination, and has many problems such as false positives, radiation hazards and low population acceptance. It is mainly suitable for cases that cannot complete total colonoscopy.
Positron emission tomography combined with CT (PET-CT) does not significantly outperform CT or MRI in determining local or distant metastasis, and it incurs higher examination costs. Consequently, routine screening for early CRC is not recommended[23,24]. However, PET-CT can be an effective supplementary examination for patients with complex conditions where routine methods do not provide a clear diagnosis. It is particularly recommended preoperatively for patients with stage III or higher tumors to assess the presence of distant metastasis.