Published online Jan 28, 2023. doi: 10.3748/wjg.v29.i4.744
Peer-review started: September 13, 2022
First decision: October 19, 2022
Revised: November 5, 2022
Accepted: November 28, 2022
Article in press: November 28, 2022
Published online: January 28, 2023
Processing time: 129 Days and 9.2 Hours
The impact of the coronavirus on hospitalizations for gastrointestinal (GI) disease, particularly at a population level is understudied.
To investigate trends in hospitalizations, inpatient endoscopy resource utilization, and outcomes during the first year of the coronavirus pandemic and subsequent lockdowns.
Using the California State Inpatient Database for 2018-2020, we explored year-to-year and 2020 month-to-month trends in hospitalizations, length of stay, and inpatient mortality (all-cause & viral pneumonia-specific) for common inpatient GI diagnoses including acute pancreatitis, diverticulitis, cholelithiasis, non-infectious gastroenteritis, upper and lower GI bleeding (LGIB), Clostridium difficile, viral gastroenteritis, inflammatory bowel disease, and acute cholangitis.
Disease-specific hospitalizations decreased for all included conditions except nonvariceal upper GI bleeding (NVUGIB), LGIB, and ulcerative colitis (UC) (ptrend < 0.0001). All-cause inpatient mortality was higher in 2020 vs 2019, for acute pancreatitis (P = 0.029), diverticulitis (P = 0.04), NVUGIB (P = 0.003), and Crohn’s disease (P = 0.004). In 2020, hospitalization rates were lowest in April, November, and December. There was no significant corresponding increase in inpatient mortality except in UC (ptrend = 0.048). Viral pneumonia and viral pneumonia complicated by respiratory failure increased (P < 0.001) among GI hospitalizations. Endoscopy utilization within 24 h of admission was unchanged for GI emergencies except NVUGIB (P < 0.001).
Our findings suggest that hospitalization rates for common GI conditions significantly declined in California during the COVID pandemic, particularly in April, November and December 2020. All-cause mortality was significantly higher among acute pancreatitis, diverticulitis, NVUGIB, and Crohn’s disease hospitalizations. Emergency endoscopy rates were mostly comparable between 2020 and 2019.
Core Tip: In the current study, we found that, in the first year of the pandemic (2020), the lowest hospitalization rates for common gastrointestinal (GI) conditions in California coincided with peaks of the pandemic in April, November, and December. Overall, there was a 15% hospitalization rate reduction for acute GI conditions in 2020 (the first year of the pandemic) compared to 2019. No significant increase in all-cause mortality for GI admissions was observed for any of the conditions studied except acute pancreatitis, diverticulitis, nonvariceal upper GI bleeding (NVUGIB) and Crohn’s disease. Emergency endoscopies within the first 24 h for acute GI conditions in 2020 were comparable with previous years except for NVUGIB. Unfortunately, there was a corresponding increase in all-cause mortality for NVUGIB. We also outline and create plots of the number of admissions and associated in patient all-cause mortality by month of the year for the conditions studied.
- Citation: Adekunle AD, Rubens M, Sedarous M, Tariq T, Okafor PN. Trends in gastrointestinal disease hospitalizations and outcomes during the first year of the coronavirus pandemic. World J Gastroenterol 2023; 29(4): 744-757
- URL: https://www.wjgnet.com/1007-9327/full/v29/i4/744.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i4.744
The COVID-19 pandemic had an immense impact on public health globally[1,2]. The first official case in the United States was confirmed on January 20, 2020[3]. Subsequently, containment measures were implemented with the goal of curtailing the spread of the coronavirus. On March 19th, 2020, the state of California became the first in the United States to issue a mandatory stay-at-home order[4]. This was eventually followed by other states which issued similar mandates[5]. In the wake of the spreading pandemic and implementation of control measures, there was a drastic decline in healthcare resource utilization for preventive, elective, and emergency purposes[2,6-8]. Widespread delays and outright refrainment from health care seeking were observed[9], as well as the dynamic restructuring of health systems to focus on expanding capacity for COVID response and limiting COVID exposure[7,8,10,11].
Multiple studies have revealed that at the peak of the pandemic, hospitalization rates among patients with acute gastrointestinal (GI) diseases dropped precipitously[12,13]. Additionally, widespread procedural delays and an overall decrease in the performance of endoscopic procedures were observed[14-16]. Many elective and ambulatory endoscopic procedures were canceled while health systems and national societies formulated guidelines. For instance, patients hospitalized with GI bleeding were found to have more severe laboratory parameters on presentation, lower odds of inpatient endoscopy, increased length of stay, and a higher likelihood of receiving a blood transfusion than those admitted during the pre-COVID period[17].
Diagnoses such as acute pancreatitis, diverticulitis, and GI hemorrhage have historically accounted for the majority of GI admissions in the United States[18]. While it is known that there was an overall decline in admissions for non-COVID-related diagnoses, it remains unclear how outcomes of acute GI diseases evolved through the various waves of the pandemic and phases of lockdowns[7,19]. Existing data have emerged mostly from single-institution studies[7,9,15-17,20]. These studies have suggested an increase in emergency procedures during the pandemic but have yielded mixed results regarding outcomes such as in-hospital mortality rates[17,20-22].
In this study, we describe the trends in hospitalizations, endoscopy utilization, and inpatient mortality from 2018 to 2020 for twelve of the most common inpatient GI diagnoses, using a statewide database. Findings offer insight into how outcomes evolved through the various phases of the pandemic and provide population-level data beneficial to healthcare systems and policymakers.
Data for this study was obtained from the California Healthcare Cost and Utilization Project State Inpatient Databases (HCUP-SIDs) for the years 2018 through 2020. The SID are a set of state-specific, all-payer, administrative databases maintained by the Agency for Healthcare Research and Quality as part of the HCUP. These data are collected annually and include discharge information from over 90% of discharges from eligible hospitals. The data elements captured include demographic information such as patient age, sex, race, marital status, zip code, payer, and income quartile (based on the median income for residential zip code) as well as elements pertaining to hospitalization such as length of stay, discharge disposition, primary and secondary discharge diagnoses, procedures, total hospital charges and outcomes[23,24]. An extensive description of the SID is available elsewhere[23,24]. Based on the determination that this study did not meet the Department of Health and Human Services definition of human subject research, this study was considered exempt by the Stanford University Institutional Review Board.
The analysis cohort comprised adult (≥ 18 years old) hospitalizations for 12 acute GI conditions in California, between January 1, 2018, and December 31, 2020. We used International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes, similar to previous studies (see appendix) for disease identification[25]. Hospitalizations for acute pancreatitis, cholelithiasis, diverticulitis, non-infectious gastroenteritis/colitis, non-variceal upper GI bleeding, variceal upper GI bleeding, lower GI bleeding/diverticular bleeding, Clostridium difficile, viral gastroenteritis, Crohn’s disease, ulcerative colitis (UC) were included for analysis (see appendix for the ICD code algorithms used). These diagnosis categories were chosen based on previously published population-level studies that showed them as the most prevalent inpatient GI diseases per rank ordering[26]. Observations of 10 or fewer in count were excluded from reporting per the HCUP data use agreement. All authors had access to the study data and reviewed and approved the final manuscript.
The outcomes of interest included year-to-year trends from 2018 to 2019, and 2020 month-to-month variations in acute GI hospitalizations, hospital length of stay, and all-cause inpatient mortality. We also explored viral pneumonia-associated mortality outcomes from 2018 to 2020 among patients hospitalized with GI conditions to assess the burden on these patients. In addition, we analyzed patterns in endoscopy intervention for emergency GI conditions such as food impaction, foreign body ingestion, acute variceal/non-variceal hemorrhage, and acute cholangitis during the pandemic. These procedures were defined using the International Classification of Diseases, Tenth Revision, procedural coding system (ICD-10 PCS) codes similar to those used in previous studies[26,27] (please see appendix for ICD codes used). Hospitalization costs were not estimated because at the time of analysis 2020 cost-to-charge data were not available. We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines to improve the quality of reporting[28].
Descriptive statistics were used to describe demographic and clinical characteristics of GI-related hospitalizations. Frequencies and percentages were used to describe categorical variables. To compare categorical variables, we used Chi-square test. We compared demographic and clinical characteristics of GI admissions by year of hospitalizations. For selected GI conditions, we compared the total number of discharges, hospital length of stay, and in-hospital mortality by year. For selected GI procedures, we compared the total number of discharges, hospital length of stay, in-hospital mortality, number of procedures within the first 24 h of admission, and number of procedures after the first 24 h of admission. For estimating trends, we used logistic regression. Statistical significance was set at P < 0.05 and all tests were two-tailed. All analyses were performed using SAS version 9.4 (Cary NC, United States).
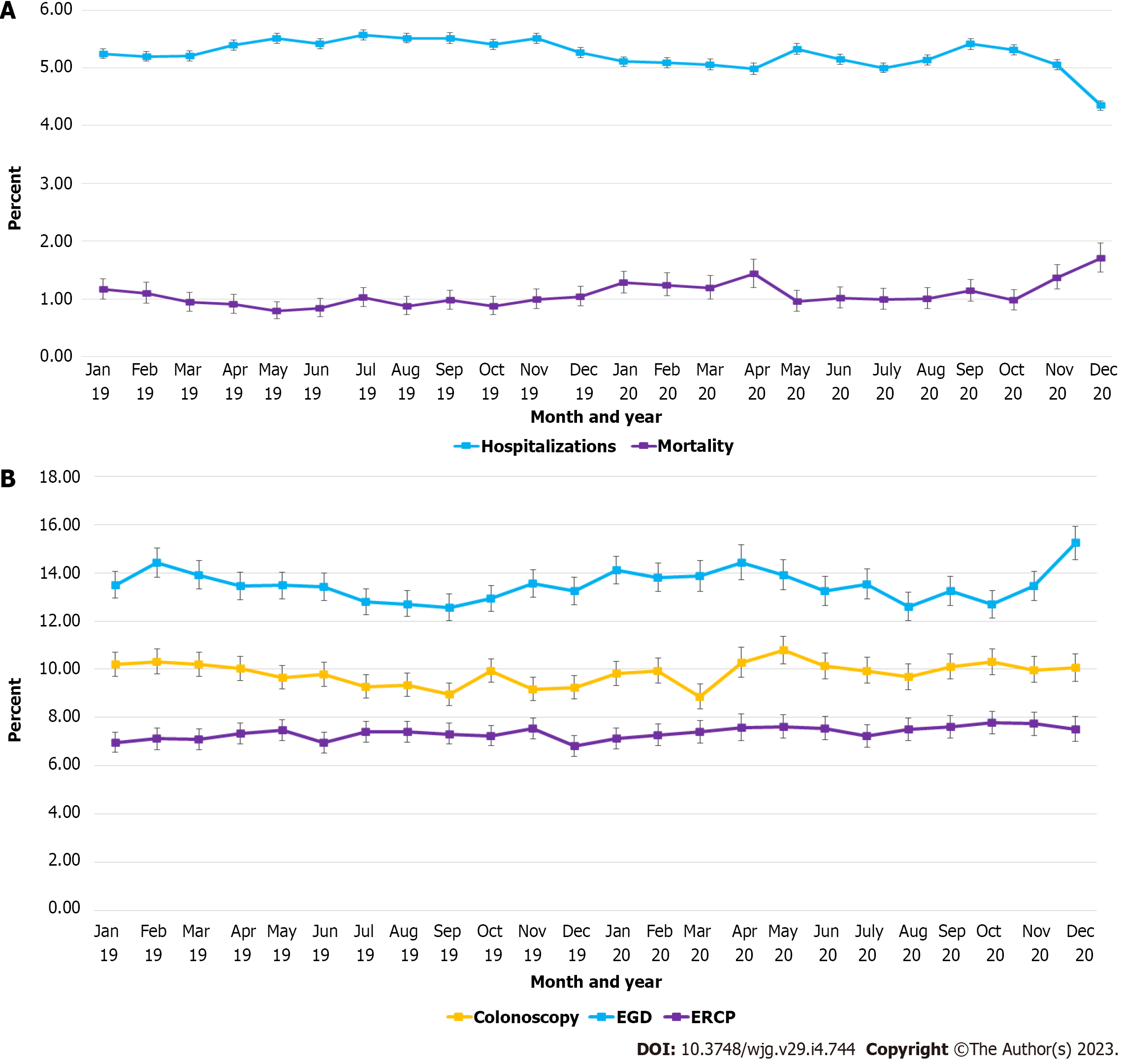
Between January 1, 2018 and December 31, 2020, there were a total of 486543 hospitalizations for the 12 included acute GI conditions in California State. While annual hospitalizations were comparable between 2018 and 2019, there was a 15% hospitalization rate reduction in 2020 (173535 in 2018, 174827 in 2019, and 145545 in 2020). For all the years included in the analysis, acute cholelithiasis was the most common GI discharge diagnosis followed by acute upper GI bleeding, and then acute pancreatitis (Table 1). Disease-specific hospitalizations also significantly decreased for all conditions studied except non-variceal upper GI bleeding (NVUGIB) (P for trend = 0.853), lower GI bleeding (P for trend = 0.329), and UC (P for trend = 0.132) (Table 2). The 2020 month-to-month trend analysis revealed the lowest hospitalization rates in April, November, and December 2020, corresponding with the peaks of the pandemic (Figure 1A).
| GI conditions | 2018 | 2019 | 2020 | Relative change | P for trend |
| Acute pancreatitis | |||||
| Total number of discharges, n (%) | 26771 (0.8) | 26675 (0.8) | 23828 (0.8) | -11.0 | 0.028 |
| Total hospital stays (in thousands) days | 109.6 | 107.6 | 99.4 | -9.3 | 0.118 |
| Mortality, n (%) | 124 (0.5) | 134 (0.5) | 144 (0.6) | 16.1 | 0.029 |
| Cholelithiasis | |||||
| Total number of discharges | 39473 (1.2) | 39710 (1.3) | 33215 (1.2) | -15.9 | < 0.001 |
| Total hospital stays (in thousands) days | 129.1 | 130.5 | 107.4 | -16.8 | 0.152 |
| Mortality, n (%) | 96 (0.2) | 94 (0.2) | 81 (0.2) | -15.6 | 0.994 |
| Diverticulitis | |||||
| Total number of discharges | 16899 (0.5) | 16992 (0.5) | 13855 (0.5) | -18.0 | < 0.001 |
| Total hospital stays (in thousands) days | 75.7 | 76.0 | 61.5 | -18.8 | 0.495 |
| Mortality, n (%) | 77 (0.5) | 67 (0.4) | 87 (0.6) | 13.0 | 0.042 |
| Noninfectious gastroenteritis/colitis | |||||
| Total number of discharges | 9376 (0.3) | 9236 (0.3) | 6734 (0.2) | -28.2 | < 0.001 |
| Total hospital stays (in thousands) days | 27.3 | 27.8 | 21.3 | -22.0 | < 0.001 |
| Mortality, n (%) | 31 (0.3) | 35 (0.4) | 26 (0.4) | -16.1 | 0.543 |
| Nonvariceal upper GI bleeding | |||||
| Total number of discharges | 32207 (1.0) | 33361 (1.1) | 29155 (1.0) | -9.5 | 0.853 |
| Total hospital stays (in thousands) days | 125.6 | 132.6 | 116.9 | -6.9 | 0.002 |
| Mortality, n (%) | 581 (1.8) | 604 (1.8) | 623 (2.1) | 7.2 | 0.003 |
| Variceal upper GI bleeding | |||||
| Total number of discharges | 1007 (0.0) | 880 (0.0) | 808 (0.0) | -19.8 | 0.006 |
| Total hospital stays (in thousands) days | 4.0 | 3.7 | 3.2 | -20.0 | 0.635 |
| Mortality, n (%) | 35 (3.5) | 38 (4.3) | 39 (4.8) | 11.4 | 0.149 |
| Lower GI bleeding and diverticular bleeding | |||||
| Total number of discharges | 11549 (0.4) | 11914 (0.4) | 10613 (0.4) | -8.1 | 0.329 |
| Total hospital stays (in thousands) days | 43.4 | 44.2 | 40.0 | -7.8 | 0.783 |
| Mortality, n (%) | 132 (1.1) | 127 (1.1) | 100 (0.9) | -24.2 | 0.145 |
| Clostridium difficile | |||||
| Total number of discharges | 1552 (0.0) | 1457 (0.0) | 963 (0.0) | -38.0 | < 0.001 |
| Total hospital stays (in thousands) days | 9.8 | 9.3 | 6.3 | -35.7 | 0.532 |
| Mortality, n (%) | 17 (1.1) | 20 (1.4) | 15 (1.6) | -11.8 | 0.308 |
| Viral gastroenteritis | |||||
| Total number of discharges | 6005 (0.2) | 5652 (0.2) | 3794 (0.1) | -36.8 | < 0.001 |
| Total hospital stays (in thousands) days | 17.0 | 16.0 | 11.6 | -31.8 | < 0.001 |
| Mortality, n (%) | 15 (0.2) | 19 (0.3) | 18 (0.5) | 20.0 | 0.066 |
| Crohn’s disease | |||||
| Total number of discharges | 14273 (0.5) | 14510 (0.5) | 12583 (0.4) | -11.8 | 0.021 |
| Total hospital stays (in thousands) days | 76.6 | 77.5 | 70.1 | -8.5 | 0.060 |
| Mortality, n (%) | 245 (1.7) | 242 (1.7) | 276 (2.2) | 12.7 | 0.004 |
| Ulcerative colitis | |||||
| Total number of discharges | 12805 (0.4) | 12919 (0.4) | 11848 (0.4) | -7.5 | 0.132 |
| Total hospital stays (in thousands) days | 74.7 | 75.5 | 70.5 | -5.6 | 0.361 |
| January, 2020 | February, 2020 | March, 2020 | April, 2020 | May, 2020 | June, 2020 | July, 2020 | August, 2020 | September, 2020 | October, 2020 | November, 2020 | December, 2020 | Relative change | P for trend | ||
| Acute pancreatitis | |||||||||||||||
| Total number of discharges | 2163 (0.8) | 1935 (0.8) | 1956 (0.9) | 1642 (0.9) | 2002 (0.9) | 2092 (0.9) | 2063 (0.8) | 2077 (0.9) | 2106 (0.9) | 2096 (0.8) | 1913 (0.8) | 1783 (0.7) | -17.6% | < 0.0001 | |
| Mortality | 21 (1.0) | 12 (0.6) | 16 (0.8) | 8 (0.5) | 6 (0.3) | 12 (0.6) | 11 (0.5) | 14 (0.7) | 12 (0.6) | 8 (0.4) | 10 (0.5) | 14 (0.8) | -33.3% | 0.211 | |
| Cholelithiasis | |||||||||||||||
| Total number of discharges | 3170 (1.1) | 2926 (1.1) | 2437 (1.1) | 2050 (1.1) | 2743 (1.2) | 2831 (1.2) | 2759 (1.1) | 2858 (1.2) | 3112 (1.3) | 3137 (1.3) | 2864 (1.2) | 2328 (1.0) | -26.6% | < 0.0001 | |
| Mortality | 6 (0.2) | 9 (0.3) | 2 (0.1) | 4 (0.2) | 7 (0.3) | 4 (0.1) | 3 (0.1) | 7 (0.2) | 14 (0.4) | 7 (0.2) | 8 (0.3) | 10 (0.4) | 66.7% | 0.060 | |
| Diverticulitis | |||||||||||||||
| Total number of discharges | 1349 (0.5) | 1315 (0.5) | 1067 (0.5) | 746 (0.4) | 1050 (0.5) | 1141 (0.5) | 1183 (0.5) | 1302 (0.5) | 1247 (0.5) | 1351 (0.5) | 1161 (0.5) | 943 (0.4) | -30.1% | 0.0004 | |
| Mortality | 9 (0.7) | 11 (0.8) | 11 (1.0) | 6 (0.8) | 3 (0.3) | 3 (0.3) | 4 (0.3) | 9 (0.7) | 10 (0.8) | 7 (0.5) | 7(0.6) | 7 (0.7) | -22.2% | 0.501 | |
| Noninfectious gastroenteritis/colitis | |||||||||||||||
| Total number of discharges | 720 (0.3) | 643 (0.3) | 538 (0.2) | 426 (0.2) | 539 (0.2) | 535 (0.2) | 554 (0.2) | 560 (0.2) | 641 (0.3) | 670 (0.3) | 510 (0.2) | 398 (0.2) | -44.7% | < 0.0001 | |
| Mortality | 2 (0.3) | 2 (0.3) | 3 (0.6) | 2 (0.5) | 2 (0.4) | 2 (0.4) | 3 (0.5) | 2 (0.4) | 2 (0.3) | 2 (0.3) | 1 (0.2) | 3 (0.8) | 50.0% | 0.859 | |
| Nonvariceal upper GI bleeding | |||||||||||||||
| Total number of discharges | 2971 (1.1) | 2692 (1.1) | 2458 (1.1) | 1960 (1.0) | 2361 (1.1) | 2440 (1.0) | 2451 (1.0) | 2325 (1.0) | 2428 (1.0) | 2396 (1.0) | 2450 (1.0) | 2223 (0.9) | -25.2% | <.0001 | |
| Mortality | 68 (2.3) | 61 (2.3) | 52 (2.1) | 55 (2.8) | 48 (2.0) | 40 (1.6) | 49 (2.0) | 35 (1.5) | 46 (1.9) | 47 (2.0) | 72 (2.9) | 50 (2.2) | -26.5% | 0.882 | |
| Variceal upper GI bleeding | |||||||||||||||
| Total number of discharges | 80 (0.0) | 59 (0.0) | 71 (0.0) | 53 (0.0) | 55 (0.0) | 74 (0.0) | 65 (0.0) | 64 (0.0) | 73 (0.0) | 57 (0.0) | 74 (0.0) | 83 (0.0) | 3.8% | 0.042 | |
| Mortality | 2 (2.5) | 2 (3.4) | 1 (1.4) | 1 (1.9) | 1 (1.8) | 6 (8.1) | 5 (7.7) | 4 (6.3) | 6 (8.2) | 2 (3.5) | 2 (2.7) | 7 (8.4) | 250.0% | 0.050 | |
| Lower GI bleeding and diverticular bleeding | |||||||||||||||
| Total number of discharges | 1039 (0.4) | 943 (0.4) | 884 (0.4) | 743 (0.4) | 843 (0.4) | 834 (0.4) | 835 (0.3) | 906 (0.4) | 936 (0.4) | 916 (0.4) | 921 (0.4) | 813 (0.3) | -21.8 | 0.231 | |
| Mortality | 13 (1.3) | 6 (0.6) | 12 (1.4) | 5 (0.7) | 9 (1.1) | 6 (0.7) | 7 (0.8) | 9 (1.0) | 7 (0.7) | 7 (0.8) | 8 (0.9) | 11 (1.4) | -15.4 | 0.822 | |
| Clostridium difficile | |||||||||||||||
| Total number of discharges | 96 (0.0) | 98 (0.0) | 85 (0.0) | 63 (0.0) | 67 (0.0) | 81 (0.0) | 82 (0.0) | 80 (0.0) | 89 (0.0) | 95 (0.0) | 70 (0.0) | 57 (0.0) | -40.6 | 0.131 | |
| Mortality | 2 (2.1) | 2 (2.0) | 4 (4.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (2.4) | 4 (5.0) | 0 (0.0) | 0 (0.0) | 1 (1.4) | 0 (0.0) | -100.0 | 0.157 | |
| Viral gastroenteritis | |||||||||||||||
| Total number of discharges | 468 (0.2) | 395 (0.2) | 366 (0.2) | 248 (0.1) | 263 (0.1) | 296 (0.1) | 288 (0.1) | 325 (0.1) | 325 (0.1) | 327 (0.1) | 296 (0.1) | 197 (0.1) | -57.9% | 0.536 | |
| Mortality | 4 (0.9) | 0 (0.0) | 2 (0.5) | 2 (0.8) | 2 (0.8) | 3 (1.0) | 0 (0.0) | 0 (0.0) | 2 (0.6) | 1 (0.3) | 2 (0.7) | 0 (0.0) | -100.0% | 0.402 | |
| Crohn’s disease | |||||||||||||||
| Total number of discharges | 1262 (0.5) | 1137 (0.4) | 977 (0.4) | 817 (0.4) | 998 (0.5) | 997 (0.4) | 1076 (0.4) | 1102 (0.5) | 1120 (0.5) | 1078 (0.4) | 1040 (0.4) | 979 (0.4) | -22.4% | 0.035 | |
| Mortality | 29 (2.3) | 26 (2.3) | 18 (1.8) | 25 (3.1) | 16 (1.6) | 25 (2.5) | 16 (1.5) | 20 (1.8) | 25 (2.2) | 22 (2.0) | 23 (2.2) | 31 (3.2) | 6.9% | 0.627 | |
| Ulcerative colitis | |||||||||||||||
| Total number of discharges | 1109 (0.4) | 1038 (0.4) | 917 (0.4) | 787 (0.4) | 953 (0.4) | 984 (0.4) | 1039 (0.4) | 973 (0.4) | 1068 (0.4) | 1081 (0.4) | 970 (0.4) | 929 (0.4) | -16.2% | 0.0005 | |
| Mortality | 31 (2.8) | 32 (3.1) | 19 (2.1) | 28 (3.6) | 19 (2.0) | 23 (2.3) | 22 (2.1) | 23 (2.4) | 26 (2.4) | 27 (2.5) | 35 (3.6) | 46 (5.0) | 48.4% | 0.048 | |
| Acute cholangitis | |||||||||||||||
| Total number of discharges | 121 (0.0) | 107 (0.0) | 111 (0.0) | 74 (0.0) | 108 (0.0) | 103 (0.0) | 101 (0.0) | 126 (0.1) | 128 (0.1) | 161 (0.1) | 118 (0.0) | 108 (0.0) | -10.7% | 0.032 | |
| Mortality | 1 (0.8) | 0 (0.0) | 0 (0.0) | 2 (2.7) | 0 (0.0) | 1 (1.0) | 1 (1.0) | 0 (0.0) | 1 (0.8) | 1 (0.6) | 0 (0.0) | 2 (1.9) | 100.0% | 0.671 | |
Baseline patient characteristics were similar across study years. Patients aged 45-64 years accounted for the greatest proportion of hospitalizations (33.2% in 2018, 32.7% in 2019, and 32% in 2020) while those aged ≥ 85 accounted for the smallest proportion (8.7% in 2018, 8.6% in 2019, and 8.3% in 2020) (Table 3). The majority of hospitalizations were among females (54% in 2018, 53.9% in 2019, and 52.7% in 2020) and Non-Hispanic Whites (48.3% in 2018, 46.8% in 2019, and 46.2% in 2020). Hispanics accounted for the second-highest proportion of hospitalizations (32% in 2018, 32.5% in 2019, and 33% in 2020) while other racial groups accounted for a minority of hospitalizations across all 3 study years (Table 3).
| Variables | 2018 | 2019 | 2020 | P value |
| Age, yr | < 0.001 | |||
| 18-44 | 47019 (27.7) | 46521 (27.2) | 40924 (28.1) | |
| 45-64 | 56369 (33.2) | 5598 (32.7) | 46629 (32.0) | |
| 65-84 | 51757 (30.5) | 53860 (31.5) | 45944 (31.6) | |
| ≥ 85 | 14693 (8.7) | 14806 (8.6) | 12062 (8.3) | |
| Sex | < 0.001 | |||
| Male | 78081 (46.0) | 78928 (46.1) | 68873 (47.3) | |
| Female | 91745 (54.0) | 92239 (53.9) | 76677 (52.7) | |
| Race | < 0.001 | |||
| White | 81404 (48.3) | 79531 (46.8) | 66613 (46.2) | |
| African American | 13080 (7.8) | 13016 (7.7) | 11219 (7.8) | |
| Hispanic | 53962 (32.0) | 55153 (32.5) | 47629 (33.0) | |
| Asian Pacific Islander | 13422 (8.0) | 13894 (8.2) | 11375 (7.9) | |
| Native American | 555 (0.3) | 835 (0.5) | 485 (0.3) | |
| Other | 6286 (3.7) | 7336 (4.3) | 6947 (4.8) | |
| Payer | < 0.001 | |||
| Medicare | 68639 (40.4) | 70861 (41.4) | 59701 (41.0) | |
| Medicaid | 48581 (28.6) | 48048 (28.1) | 42046 (28.9) | |
| Private | 45612 (26.9) | 44389 (25.9) | 37733 (25.9) | |
| Self-pay | 3492 (2.1) | 3864 (2.3) | 2948 (2.0) | |
| No charge | 204 (0.1) | 272 (0.2) | 170 (0.1) | |
| Other | 3254 (1.9) | 3707 (2.2) | 2931 (2.0) | |
| Elixhauser comorbidity index | < 0.001 | |||
| 0 | 28927 (17.0) | 28648 (16.7) | 23244 (16.0) | |
| 1 | 31228 (18.4) | 31049 (18.1) | 26001 (17.9) | |
| 2 | 28036 (16.5) | 28078 (16.4) | 24118 (16.6) | |
| ≥ 3 | 81647 (48.1) | 83401 (48.7) | 72196 (49.6) | |
| Bacterial pneumonia | 4232 (2.5) | 4285 (2.5) | 3856 (2.6) | 0.008 |
| Bacterial pneumonia/respiratory failure specific mortality | 248 (0.1) | 271 (0.2) | 275 (0.2) | 0.009 |
| Viral pneumonia | 76 (0.0) | 82 (0.0) | 724 (0.5) | < 0.001 |
| Viral pneumonia/respiratory failure specific mortality | 6 (0.0) | 5 (0.0) | 80 (0.1) | < 0.001 |
| COVID-19 specific mortality | - | - | 123 (0.08) | < 0.001 |
| All-cause mortality | 1667 (1.0) | 1644 (1.0) | 1723 (1.2) | < 0.001 |
For the entire cohort of GI hospitalizations, all-cause inpatient mortality was higher in 2020 compared to 2019 (1.2% vs 1.0%, P < 0.001). However, when individual diagnoses were examined, for most of the diseases, all-cause inpatient mortality was no different in 2020 compared to 2019 except among patients hospitalized with acute pancreatitis (0.6% vs 0.5%, P = 0.029), diverticulitis (0.6% vs 0.4%, P = 0.04), NVUGIB (2.1% vs 1.8%, P = 0.003), and Crohn’s disease (2.2% vs 1.7%, P = 0.004) (Table 2).
To determine the trends in all-cause GI inpatient mortality, a 2020 month-to-month analysis was performed that did not reveal any significant variations except for UC hospitalizations where the highest inpatient mortality rate was observed in December 2020 (5%, P for trend = 0.048) (Table 2). We also examined month-to-month (Supplementary Figure 1), and year-to-year changes in viral pneumonia admissions among patients with the aforementioned GI diagnoses. We observed a significant increase in viral pneumonia hospitalizations among the entire cohort and also a significant increase in viral pneumonia-specific mortality from 2018 to 2020 (Table 3). In the absence of a dedicated ICD-10 code for COVID-19 in the years preceding the pandemic, we could not directly compare rates. We did however examine COVID-19-specific mortality rates for the year 2020 and found a mortality rate of 0.08%.
We examined patterns of endoscopy utilization including upper endoscopy, colonoscopy, flexible sigmoidoscopy, and endoscopic retrograde cholangiopancreatography (ERCP) in California between 2018 and 2020 for GI emergencies (Figure 1B). Except upper endoscopy for acute variceal hemorrhage which significantly reduced in 2020 (744 vs 690, P = 0.007), likely as a result of overall reduced hospitalization rates, there was no significant difference in inpatient endoscopic intervention rates in 2020 compared to 2019 (Table 4). Trend analysis showed that mortality for GI bleed emergencies was comparable for acute variceal and lower GI bleeding in the pre-pandemic and pandemic eras. However, in 2020, there was a significant rise in all-cause mortality among patients hospitalized with acute nonvariceal upper GI bleeding.
| 2018 | 2019 | 2020 | Relative change | P for trend | |
| ANVH (upper endoscopy) | |||||
| Total number of discharges | 15310 (0.5) | 15942 (0.5) | 13622 (0.5) | -11.0% | 0.121 |
| Total hospital stays (in thousands) days | 65.0 | 69.2 | 60.2 | -7.4% | 0.002 |
| Mortality | 321 (2.1) | 335 (2.1) | 346 (2.5) | 7.8% | 0.012 |
| Procedure within 24 h | 5005 (32.7) | 5185 (32.5) | 4132 (30.3) | -17.4% | < 0.001 |
| AVH (upper endoscopy) | |||||
| Total number of discharges | 867 (0.0) | 744 (0.0) | 690 (0.0) | -20.4% | 0.007 |
| Total hospital stays (in thousands) days | 3.6 | 3.2 | 2.8 | -22.2% | 0.697 |
| Mortality | 26 (3.0) | 22 (3.0) | 26 (3.8) | 0.0% | 0.414 |
| Procedure within 24 h | 348 (40.1) | 327 (44.0) | 283 (41.0) | -18.7% | 0.653 |
| LGIB (lower endoscopy) | |||||
| Total number of discharges | 5524 (0.2) | 5722 (0.2) | 4973 (0.2) | -10.0% | 0.724 |
| Total hospital stays (in thousands) days | 21.7 | 22.1 | 19.9 | -8.3% | 0.436 |
| Mortality | 29 (0.5) | 35 (0.6) | 17 (0.3) | -41.4% | 0.201 |
| Procedure within 24 h | 859 (15.6) | 975 (17.0) | 793 (15.9) | -7.7% | 0.534 |
| Acute cholangitis (ERCP) | |||||
| Total number of discharges | 1038 (0.0) | 962 (0.0) | 882 (0.0) | -15.0% | 0.137 |
| Total hospital stays (in thousands) days | 4.3 | 4.4 | 3.7 | -14.0% | 0.505 |
| Mortality | 6 (0.6) | 4 (0.4) | 5 (0.6) | -16.7% | 0.952 |
| Procedure within 24 h | 268 (25.8) | 260 (27.0) | 220 (24.9) | -17.9% | 0.695 |
| Food impaction (EGD/upper endoscopy) | |||||
| Total number of discharges | 127 (0.0) | 143 (0.0) | 118 (0.0) | -7.1% | 0.834 |
| Total hospital stays (in thousands) days | 0.6 | 0.6 | 0.6 | 0.0% | 0.849 |
| Mortality | 4 (3.1) | 3 (2.1) | 0 (0.0) | -100.0% | 0.086 |
| Procedure within 24 h | 73 (57.5) | 70 (49.0) | 60 (50.8) | -17.8% | 0.289 |
| Foreign body (EGD) | |||||
| Total number of discharges | 21 (0.0) | 17 (0.0) | 20 (0.0) | -4.8% | 0.891 |
| Mortality | 1 (4.8) | 2 (11.8) | 0 (0.0) | -100.0% | 0.512 |
| Procedure within 24 h | 7 (33.3) | 7 (41.2) | 12 (60.0) | 71.4% | 0.091 |
| SBP-paracentesis | |||||
| Total number of discharges | 3254 (0.1) | 3486 (0.1) | 3344 (0.1) | 2.8% | < 0.001 |
| Total hospital stays (in thousands) days | 32.4 | 35.3 | 33.8 | 4.3% | 0.594 |
| Mortality | 621 (19.1) | 631 (18.1) | 592 (17.7) | -4.7% | 0.147 |
| Procedure within 24 h | 928 (28.5) | 1044 (30.0) | 1022 (30.6) | 10.1% | 0.065 |
Sensitivity analyses demonstrated that for patients with acute nonvariceal bleeding, a significantly lower proportion received upper endoscopic intervention within the first 24 h of admission in 2020 compared to 2019 (30.3% vs 32.5%, P < 0.001), while the proportions were unchanged compared to previous years for patients hospitalized with acute variceal bleeding and lower GI bleeding (Table 4). ERCP utilization for acute cholangitis, intervention within the first 24 h (24.9% vs 27%, P = 0.700) and mortality from acute cholangitis (0.6% vs 0.4%. P = 0.950) did not significantly differ between all 3 years (Table 4). A graphical representation of monthly trends in endoscopy interventions and mortality in 2020 is shown in Supplementary Figure 2.
In this population-level study, we evaluated trends and outcomes of hospitalizations for acute GI conditions in 2020, the first year of the COVID pandemic in California, using a statewide database. Using the 2018 and 2019 data as a comparator group, we found significantly lower rates of hospitalization for most acute GI conditions in 2020 compared to previous years. We also found concomitant increases in all-cause inpatient mortality for four of the diagnoses studied including acute pancreatitis, diverticulitis, NVUGIB, and Crohn’s disease in 2020 compared to 2019. In addition, a 2020 month-to-month hospitalization trends analysis demonstrated the lowest hospitalization rates in April, November, and December of 2020.
The observed decline in hospitalizations for acute GI conditions is consistent with findings from previously published studies and likely reflects an interplay of factors during the COVID pandemic[12,13,29]. First, it has been suggested that people were willing to delay much-needed healthcare out of fear of potential exposure to COVID-19[9,11,29,30]. Additionally, the shelter-in-place measures in the spring of 2020 along with the restructuring of healthcare services necessitated by the pandemic are believed to have further reduced healthcare utilization for non-COVID indications[7,29].
The April nadir occurred after the implementation of multiple measures including the cancellation of all large events and the issuance of a stay-at-home order in March, by the California state government[13]. After the release of an initial reopening plan on April 28th, 2020 by the governor of California; and during the implementation of the early phases of the plan (in the summer months), we observed an uptick in hospitalization rates[31]. However, these never returned to pre-pandemic numbers. Coinciding with the reintroduction of restrictions later in the year, total hospitalization numbers for acute GI conditions plunged again. These lower hospitalization numbers continued through December as California and the rest of the United States battled another wave of the coronavirus pandemic[31].
Regarding GI outcomes with the fluctuations in hospitalization rates, fortunately, for most of the acute GI conditions studied, there was no significant increase in all-cause inpatient mortality, except for acute pancreatitis, diverticulitis, NVUGIB, and Crohn’s disease admissions. Although we could not determine the time of symptom onset before admission, it is possible that previously reported delays in presentation coupled with higher acuity on presentation could have contributed to the observed increases in mortality for these conditions. A previous study of acute myocardial infarctions revealed significant delays in presentation and higher mortality in the setting of the pandemic[9]. Additionally, a collaborative report from Harvard T.H. Chan School of Public Health, the Robert Wood Johnson Foundation, and National Public Radio revealed that 2 in 10 adults had reported having household members who had delayed care for a serious medical condition in the setting of the pandemic. Furthermore, over 50% of those reporting delayed care had also reported experiencing resultant adverse effects[29]. The delayed presentation has been correlated with worse health outcomes[32].
Multiple studies reported increases in alcohol intake during the pandemic which could potentially explain the worse outcomes seen in acute pancreatitis hospitalizations[33,34]. However, we could not reliably ascertain the etiology of acute pancreatitis given the claims-based nature of the databases. In addition, we observed increased mortality among patients with Crohn’s disease, but it remains unclear if the immunosuppression associated with the treatment of this inflammatory bowel disease increases the risk of COVID-related morbidity and mortality and/or if the excess mortality was attributable to COVID.
Although widespread procedural delays have been reported in the setting of the pandemic, our analysis of emergency procedural utilization revealed comparable rates of endoscopies for emergency GI conditions in 2020 with previous years, except when it came to NVUGIB where we observed a significant reduction in the proportion of patients receiving upper endoscopy within the first 24 h of presentation[14-16]. While this suggests that procedural delays could have played a role in the increase in NVUGIB-related inpatient mortality observed in 2020, it is difficult to attribute our findings solely to procedural delays as delays in presentation and higher acuity on presentation could have also played a role[9,29]. Nonetheless, current guidelines do recommend endoscopy within 24 h of presentation, and delays in endoscopy have been correlated with adverse outcomes in NVUGIB[35,36]. It is reassuring to note that outcomes of other GI emergencies such as acute variceal upper GI bleeding, lower GI bleeding, and acute cholangitis was not adversely impacted during the COVID pandemic. Although for these conditions, no reduction in emergency procedural utilization was noted.
The current study has multiple strengths. First, the use of a large, all-payer, statewide database allowed us to capture the impact of the pandemic at a large population level factoring in a diverse group of patients with different payer types. Additionally, our analyses of month-to-month trends for the year 2020, allowed us to evaluate trends in outcomes of interest in the light of the trajectory of the pandemic and our findings were reasonable as the lowest hospitalization numbers matched the phases of the documented lockdowns. We were also able to utilize ICD-10 codes and cohort identification algorithms that may reduce the risk of misclassification bias. Furthermore, we were able to compare 2020 data with the 2018 and 2019 SID data which provided baseline, pre-pandemic rates.
This study, however, has its limitations. First, given the widely varying approaches to the pandemic taken by individual states in the United States, generalizability might be limited. However, considering that our study corroborates findings from previous studies, it is unlikely that the observed patterns are only limited to California[12,13]. Another limitation is that we could not explore time to presentation and therefore cannot definitively conclude that delays in presentation contributed to the observed increases in mortality. Our study also did not explore out-of-hospital mortality, making it possible that the overall pandemic-related excess mortality is higher than observed in our study.
Also, the timeframe of the data did not include 2021. Consequently, we were unable to explore the evolution of outcomes after the initiation of widespread vaccination, beginning in late 2020, as well as in the light of the Delta and Omicron variant-related surges. It is also not possible to ascertain if the trends continued into 2021. Finally, we have to emphasize the possibility of misclassification bias given our use of an administrative dataset.
In conclusion, our findings suggest that during the first year of the COVID pandemic, there was a significant decline in hospitalization rates for common GI conditions in California, particularly in the months of April, November, and December 2020. Reassuringly, 2020 emergency endoscopy rates were mostly comparable with 2019 rates except when it came to emergency endoscopy for NVUGIB. These findings suggest that inpatient healthcare delivery for most patients with acute GI conditions remained largely unchanged during the COVID-19 pandemic. They do however reveal that patients hospitalized with acute pancreatitis, diverticulitis, nonvariceal upper GI bleeding and Crohn’s disease experienced higher all-cause inpatient mortality during the pandemic and highlight that further research is needed to elucidate the disease-specific and system-based risk factors for the increase in mortality observed in these conditions.
Healthcare resource utilization declined during the coronavirus pandemic. How this impacted gastrointestinal (GI) disease hospitalizations is not fully understood. We sought to investigate trends in hospitalizations, inpatient endoscopy utilization and outcomes during the first year of the pandemic and lockdowns.
The need for a population level understanding of the impact of the coronavirus pandemic on the outcomes of patients hospitalized with GI diseases.
To investigate trends in hospitalizations, inpatient endoscopy utilization and outcomes during the first year of the pandemic and lockdowns.
Using the California State Inpatient Database for 2018-2020, we explored year-to-year and 2020 month-to-month trends in hospitalizations, length of stay, and inpatient mortality (all-cause & viral pneumonia-specific) for common inpatient GI diagnoses including acute pancreatitis, diverticulitis, cholelithiasis, noninfectious gastroenteritis, upper and lower GI bleeding (LGIB), Clostridium difficile, viral gastroenteritis, inflammatory bowel disease, and acute cholangitis, using regression analyses. We also investigated endoscopy utilization for GI emergencies.
Disease-specific hospitalizations decreased for all included conditions except nonvariceal upper GI bleeding (NVUGIB), LGIB, and ulcerative colitis (UC) (ptrend < 0.0001). All-cause inpatient mortality was higher in 2020 compared to 2019, for acute pancreatitis (P = 0.029), diverticulitis (P = 0.04), NVUGIB (P = 0.003), and Crohn’s disease (P = 0.004). In 2020, hospitalization rates were lowest in April, November, and December. There was no significant corresponding increase in inpatient mortality except in UC (ptrend = 0.048). Endoscopy utilization within 24 h of admission was unchanged for GI emergencies except NVUGIB in which it was lower (P < 0.001).
Our findings suggest that hospitalization rates for common GI conditions significantly declined in California during the COVID pandemic, particularly in April, November and December 2020. All-cause mortality was significantly higher among acute pancreatitis, diverticulitis, NVUGIB, and Crohn’s disease hospitalizations. Emergency endoscopy rates were mostly comparable between 2020 and 2019.
We observed that patients hospitalized with acute pancreatitis, diverticulitis, nonvariceal upper GI bleeding and Crohn’s disease experienced higher all-cause inpatient mortality during the pandemic. Further research is needed to elucidate the disease-specific and system-based risk factors for the increase in mortality observed in these conditions.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Giacomelli L, Italy; Moussa BS, Egypt S-Editor: Chen YL L-Editor: A P-Editor: Chen YL
| 1. | Mafham MM, Spata E, Goldacre R, Gair D, Curnow P, Bray M, Hollings S, Roebuck C, Gale CP, Mamas MA, Deanfield JE, de Belder MA, Luescher TF, Denwood T, Landray MJ, Emberson JR, Collins R, Morris EJA, Casadei B, Baigent C. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396:381-389. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 436] [Cited by in RCA: 492] [Article Influence: 98.4] [Reference Citation Analysis (0)] |
| 2. | Eshraghian A, Taghavi A, Nikeghbalian S, Malek-Hosseini SA. Reduced rate of hospital admissions for liver-related morbidities during the initial COVID-19 outbreak. Lancet Gastroenterol Hepatol. 2020;5:803-804. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, Spitters C, Ericson K, Wilkerson S, Tural A, Diaz G, Cohn A, Fox L, Patel A, Gerber SI, Kim L, Tong S, Lu X, Lindstrom S, Pallansch MA, Weldon WC, Biggs HM, Uyeki TM, Pillai SK; Washington State 2019-nCoV Case Investigation Team. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med. 2020;382:929-936. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4155] [Cited by in RCA: 3820] [Article Influence: 764.0] [Reference Citation Analysis (1)] |
| 4. | Yeates EO, Juillard C, Grigorian A, Schellenberg M, Owattanapanich N, Barmparas G, Margulies D, Garber K, Cryer H, Tillou A, Burruss S, Penaloza-Villalobos L, Lin A, Figueras RA, Brenner M, Firek C, Costantini T, Santorelli J, Curry T, Wintz D, Biffl WL, Schaffer KB, Duncan TK, Barbaro C, Diaz G, Johnson A, Chinn J, Naaseh A, Leung A, Grabar C, Yeates TO, Nahmias J. The coronavirus disease 2019 (COVID-19) stay-at-home order's unequal effects on trauma volume by insurance status in Southern California. Surgery. 2021;170:962-968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Matrajt L, Leung T. Evaluating the Effectiveness of Social Distancing Interventions to Delay or Flatten the Epidemic Curve of Coronavirus Disease. Emerg Infect Dis. 2020;26:1740-1748. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 256] [Cited by in RCA: 215] [Article Influence: 43.0] [Reference Citation Analysis (0)] |
| 6. | Liguoro I, Pilotto C, Vergine M, Pusiol A, Vidal E, Cogo P. The impact of COVID-19 on a tertiary care pediatric emergency department. Eur J Pediatr. 2021;180:1497-1504. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 7. | Lee SH, Chang CH, Hu CC, Chang Y, Hsieh PH, Lin YC. The Risk Factor and Outcome of Metachronous Periprosthetic Joint Infections: A Retrospective Analysis With a Minimum Ten-Year Follow-Up. J Arthroplasty. 2021;36:3734-3740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, Gundlapalli AV; National Syndromic Surveillance Program Community of Practice. Impact of the COVID-19 Pandemic on Emergency Department Visits - United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:699-704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 577] [Cited by in RCA: 833] [Article Influence: 166.6] [Reference Citation Analysis (0)] |
| 9. | Aldujeli A, Hamadeh A, Briedis K, Tecson KM, Rutland J, Krivickas Z, Stiklioraitis S, Briede K, Aldujeili M, Unikas R, Zaliaduonyte D, Zaliunas R, Vallabhan RC, McCullough PA. Delays in Presentation in Patients With Acute Myocardial Infarction During the COVID-19 Pandemic. Cardiol Res. 2020;11:386-391. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 68] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 10. | Taquechel K, Diwadkar AR, Sayed S, Dudley JW, Grundmeier RW, Kenyon CC, Henrickson SE, Himes BE, Hill DA. Pediatric Asthma Health Care Utilization, Viral Testing, and Air Pollution Changes During the COVID-19 Pandemic. J Allergy Clin Immunol Pract. 2020;8:3378-3387.e11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 103] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 11. | Gale R, Eberlein S, Fuller G, Khalil C, Almario CV, Spiegel BMR. Public Perspectives on Decisions About Emergency Care Seeking for Care Unrelated to COVID-19 During the COVID-19 Pandemic. JAMA Netw Open. 2021;4:e2120940. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 12. | Oseran AS, Nash D, Kim C, Moisuk S, Lai PY, Pyhtila J, Sequist TD, Wasfy JH. Changes in hospital admissions for urgent conditions during COVID-19 pandemic. Am J Manag Care. 2020;26:327-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 13. | Birkmeyer JD, Barnato A, Birkmeyer N, Bessler R, Skinner J. The Impact Of The COVID-19 Pandemic On Hospital Admissions In The United States. Health Aff (Millwood). 2020;39:2010-2017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 355] [Cited by in RCA: 378] [Article Influence: 75.6] [Reference Citation Analysis (0)] |
| 14. | Issaka RB, Feld LD, Kao J, Hegarty E, Snailer B, Kalra G, Tomizawa Y, Strate L. Real-World Data on the Impact of COVID-19 on Endoscopic Procedural Delays. Clin Transl Gastroenterol. 2021;12:e00365. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 15. | Calderwood AH, Calderwood MS, Williams JL, Dominitz JA. Impact of the COVID-19 Pandemic on Utilization of EGD and Colonoscopy in the United States: An Analysis of the GIQuIC Registry. Tech Innov Gastrointest Endosc. 2021;23:313-321. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Mahadev S, Aroniadis OS, Barraza L, Agarunov E, Goodman AJ, Benias PC, Buscaglia JM, Gross SA, Kasmin FE, Cohen JJ, Carr-Locke DL, Greenwald DA, Mendelsohn RB, Sethi A, Gonda TA; NYSGE research committee. Impact of the COVID-19 pandemic on endoscopy practice: results of a cross-sectional survey from the New York metropolitan area. Gastrointest Endosc. 2020;92:788-789. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 17. | Kim J, Doyle JB, Blackett JW, May B, Hur C, Lebwohl B; HIRE study group. Effect of the Coronavirus 2019 Pandemic on Outcomes for Patients Admitted With Gastrointestinal Bleeding in New York City. Gastroenterology. 2020;159:1155-1157.e1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 77] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 18. | Milenkovic M, Russo CA, Elixhauser A. Hospital Stays for Gastrointestinal Diseases, 2004. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006 Feb-. [PubMed] |
| 19. | James N, Menzies M, Radchenko P. COVID-19 second wave mortality in Europe and the United States. Chaos. 2021;31:031105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 65] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 20. | Aulet T, Spencer S, Abelson J. Impact of the Early COVID-19 surge on the Outcomes of Diverticulitis. Dis Colon Rectum. 2021;64:15. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Reference Citation Analysis (0)] |
| 21. | Lau LHS, Wong SH, Yip TCF, Wong GLH, Wong VWS, Sung JJY. Collateral Effect of Coronavirus Disease 2019 Pandemic on Hospitalizations and Clinical Outcomes in Gastrointestinal and Liver Diseases: A Territory-wide Observational Study in Hong Kong. Gastroenterology. 2020;159:1979-1981.e3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 22. | Ciarleglio FA, Rigoni M, Mereu L, Tommaso C, Carrara A, Malossini G, Tateo S, Tirone G, Bjerklund Johansen TE, Benetollo PP, Ferro A, Guarrera GM, Grattarola M, Nollo G, Brolese A. The negative effects of COVID-19 and national lockdown on emergency surgery morbidity due to delayed access. World J Emerg Surg. 2021;16:37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 23. | Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project (HCUP). Introduction to the HCUP State Inpatient Databases (SID), Rockville, MD, 2021. [DOI] [Full Text] |
| 24. | Metcalfe D, Zogg CK, Haut ER, Pawlik TM, Haider AH, Perry DC. Data resource profile: State Inpatient Databases. Int J Epidemiol. 2019;48:1742-1742h. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 25. | Hirode G, Saab S, Wong RJ. Trends in the Burden of Chronic Liver Disease Among Hospitalized US Adults. JAMA Netw Open. 2020;3:e201997. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 107] [Cited by in RCA: 176] [Article Influence: 35.2] [Reference Citation Analysis (0)] |
| 26. | Peery AF, Crockett SD, Murphy CC, Lund JL, Dellon ES, Williams JL, Jensen ET, Shaheen NJ, Barritt AS, Lieber SR, Kochar B, Barnes EL, Fan YC, Pate V, Galanko J, Baron TH, Sandler RS. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2018. Gastroenterology. 2019;156:254-272.e11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 776] [Cited by in RCA: 1073] [Article Influence: 178.8] [Reference Citation Analysis (1)] |
| 27. | Sharma S, Weissman S, Mehta TI, Aziz M, Acharya A, Vohra I, Khan Z, Khan A, Nawras A, Sciarra M, Swaminath A. Role of Hospital Teaching Status on Outcomes of Patients with Inflammatory Bowel Disease: A Nationwide Analysis. Dig Dis Sci. 2021;66:2216-2226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 28. | von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147:573-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3559] [Cited by in RCA: 5773] [Article Influence: 320.7] [Reference Citation Analysis (0)] |
| 29. | Mahmud N, Hubbard RA, Kaplan DE, Serper M. Declining Cirrhosis Hospitalizations in the Wake of the COVID-19 Pandemic: A National Cohort Study. Gastroenterology. 2020;159:1134-1136.e3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 68] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 30. | Findling MG, Blendon RJ, Benson JM. Delayed Care with Harmful Health Consequences-Reported Experiences from National Surveys During Coronavirus Disease 2019. JAMA Health Forum. 2020;1:e201463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 55] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 31. | Shannon C. A timeline of California in the coronavirus pandemic, Sacramento, California, 2021. [DOI] [Full Text] |
| 32. | Mallick B, Dhaka N, Sharma V, Malik S, Sinha SK, Dutta U, Gupta P, Gulati A, Yadav TD, Gupta V, Kochhar R. Impact of timing of presentation of acute pancreatitis to a tertiary care centre on the outcome. Pancreatology. 2019;19:143-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 33. | Pollard MS, Tucker JS, Green HD Jr. Changes in Adult Alcohol Use and Consequences During the COVID-19 Pandemic in the US. JAMA Netw Open. 2020;3:e2022942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 431] [Cited by in RCA: 581] [Article Influence: 116.2] [Reference Citation Analysis (0)] |
| 34. | Barbosa C, Cowell AJ, Dowd WN. Alcohol Consumption in Response to the COVID-19 Pandemic in the United States. J Addict Med. 2021;15:341-344. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 144] [Cited by in RCA: 210] [Article Influence: 52.5] [Reference Citation Analysis (0)] |
| 35. | Laine L, Barkun AN, Saltzman JR, Martel M, Leontiadis GI. ACG Clinical Guideline: Upper Gastrointestinal and Ulcer Bleeding. Am J Gastroenterol. 2021;116:899-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 279] [Article Influence: 69.8] [Reference Citation Analysis (36)] |
| 36. | Guo CLT, Wong SH, Lau LHS, Lui RNS, Mak JWY, Tang RSY, Yip TCF, Wu WKK, Wong GLH, Chan FKL, Lau JYW, Sung JJY. Timing of endoscopy for acute upper gastrointestinal bleeding: a territory-wide cohort study. Gut. 2022;71:1544-1550. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |