Published online Aug 14, 2022. doi: 10.3748/wjg.v28.i30.4211
Peer-review started: February 10, 2022
First decision: April 5, 2022
Revised: April 17, 2022
Accepted: July 16, 2022
Article in press: July 16, 2022
Published online: August 14, 2022
Processing time: 180 Days and 23.4 Hours
Traumatic neuromas result from nerve injury after trauma or surgery but rarely occur in the bile duct. However, it is challenging to diagnose traumatic neuromas correctly preoperatively. Although some previous reports have described the imaging features of traumatic neuroma in the bile duct, no features of traumatic neuromas in the bile duct have been identified by using contrast-enhanced ultrasound (CEUS) imaging before.
A 55-year-old male patient presented to our hospital with a 3-mo history of abdominal distension and anorexia and history of cholecystectomy 4 years ago. Grayscale ultrasound demonstrated mild to moderate intrahepatic bile duct dilatation. Meanwhile, a hyperechoic nodule was found in the upper extrahepatic bile duct. The lesion approximately 0.8 cm × 0.6 cm with a regular shape and clear margins. The nodule of the bile duct showed slight hyperenhancement in the arterial phase and isoenhancement in the venous phase on CEUS. Laboratory tests showed that alanine aminotransferase and aspartate aminotransferase were increased significantly, while the tumor marker carbohydrate antigen 19-9 was increased slightly. Then, hilar bile duct resection and end-to-end bile ductal anastomosis were performed. The histological examination revealed traumatic neuroma of the extrahepatic bile duct. The patient had an uneventful recovery after surgery.
The current report will help enhance the current knowledge regarding identifying traumatic neuromas by CEUS imaging and review the related literature.
Core Tip: A traumatic neuroma results from nerve injury after trauma or surgery but rarely occurs in the bile duct. Herein, we present some of the sonographic features of ultrasound and contrast-enhanced ultrasound in a case of a traumatic neuroma. We report this unusual case and review the related literature to improve the diagnosis and differential diagnosis of a traumatic neuroma of the bile duct and related imaging findings.
- Citation: Yuan ZQ, Yan HL, Li JW, Luo Y. Contrast-enhanced ultrasound of a traumatic neuroma of the extrahepatic bile duct: A case report and review of literature. World J Gastroenterol 2022; 28(30): 4211-4220
- URL: https://www.wjgnet.com/1007-9327/full/v28/i30/4211.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i30.4211
A traumatic neuroma is a chronic reparative proliferative response of the nerve after trauma or surgery. It is composed of disorganized nerve fiber bundles with fibrous stroma, Schwann cells, perineural cells, axons, and endoneural fibroblasts[1]. The common sites of traumatic neuromas are the necks and extremities[2,3]. Although some studies have described traumatic neuromas in the bile duct, cases of sonographic features of contrast-enhanced ultrasound (CEUS) have not been published before. The clinical manifestation and imaging examination of a traumatic neuroma of the bile duct are not specific, which makes it challenging be accurately diagnosed preoperatively. Herein, we report a traumatic neuroma of the extrahepatic bile duct with detailed ultrasonographic imaging features. We also reviewed the literature on the imaging findings for traumatic neuromas.
A 55-year-old man was admitted to our hospital with unexplained abdominal distension and anorexia 3 mo ago.
The patient suffered from unexplained abdominal distension and anorexia for 3 mo. The patient developed darkened urine 2 mo ago. He experienced a weight loss of 5 kg over the course of the disease. He underwent contrast-enhanced computed tomography (CECT) examination at a local hospital, and a lesion was found in the extrahepatic bile duct, which was believed to be a tumor.
The patient underwent cholecystectomy for gallbladder stones with an uneventful postoperative recovery 4 years ago. He had a 10-year history of hypertension.
There was no other personal or family history of acute or chronic disease.
The patient showed no tenderness, rebound tenderness or muscle tension on abdominal palpation.
The liver function tests demonstrated increased levels of alanine aminotransferase (185 IU/L, normal range: < 50 IU/L), aspartate aminotransferase (148 IU/L, normal range: < 40 IU/L) and total bilirubin (37.0 μmol/L, normal range: 5 µmol/L to 28 µmol/L). Tumor markers included carbohydrate antigen 19-9 (98.6 U/mL, normal range: < 22 U/mL), carcinoembryonic antigen (0.97 ng/mL, normal range: < 5 ng/mL), and alpha-fetoprotein (4.67 ng/mL, normal range: < 7 ng/mL).
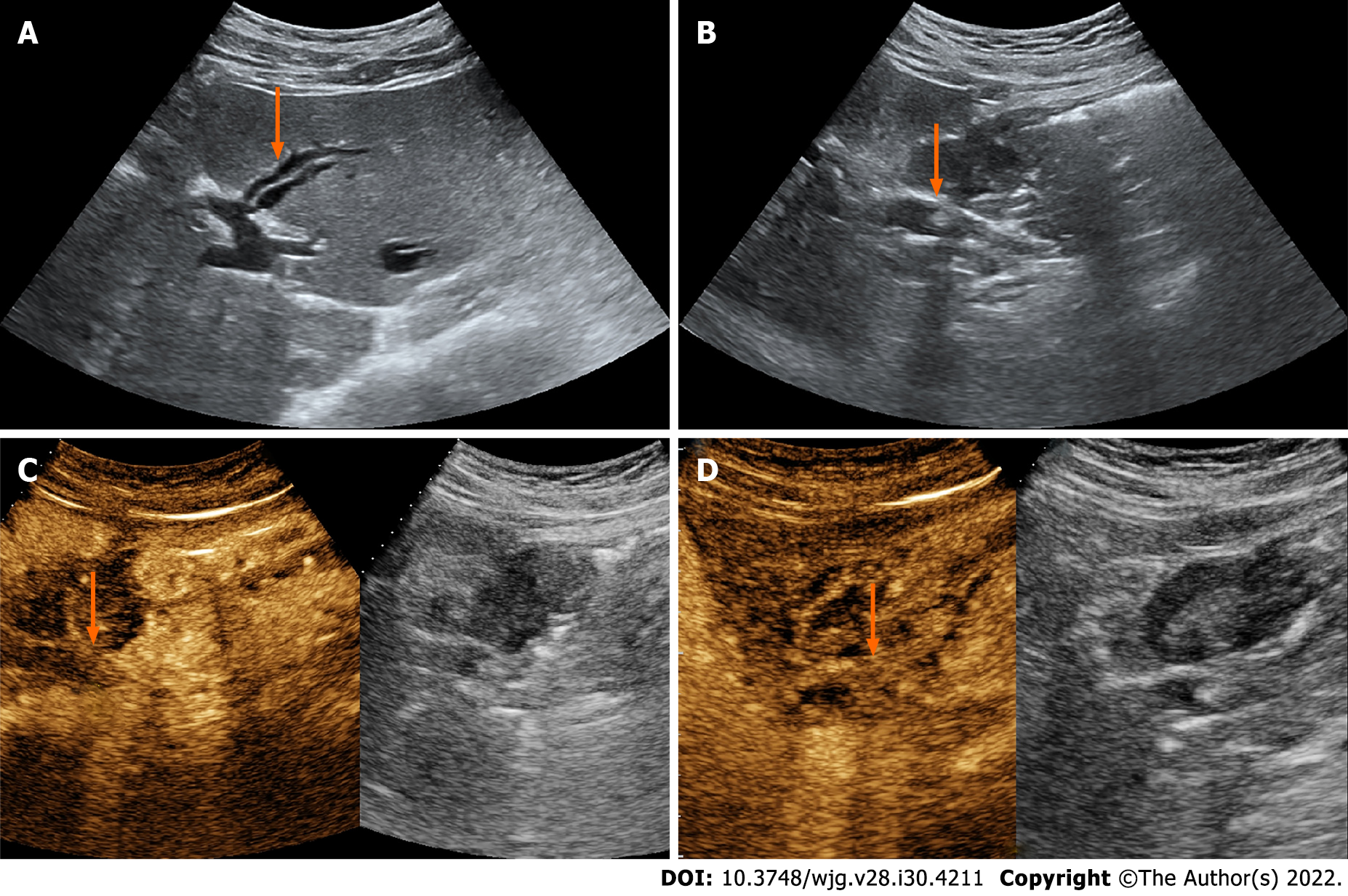
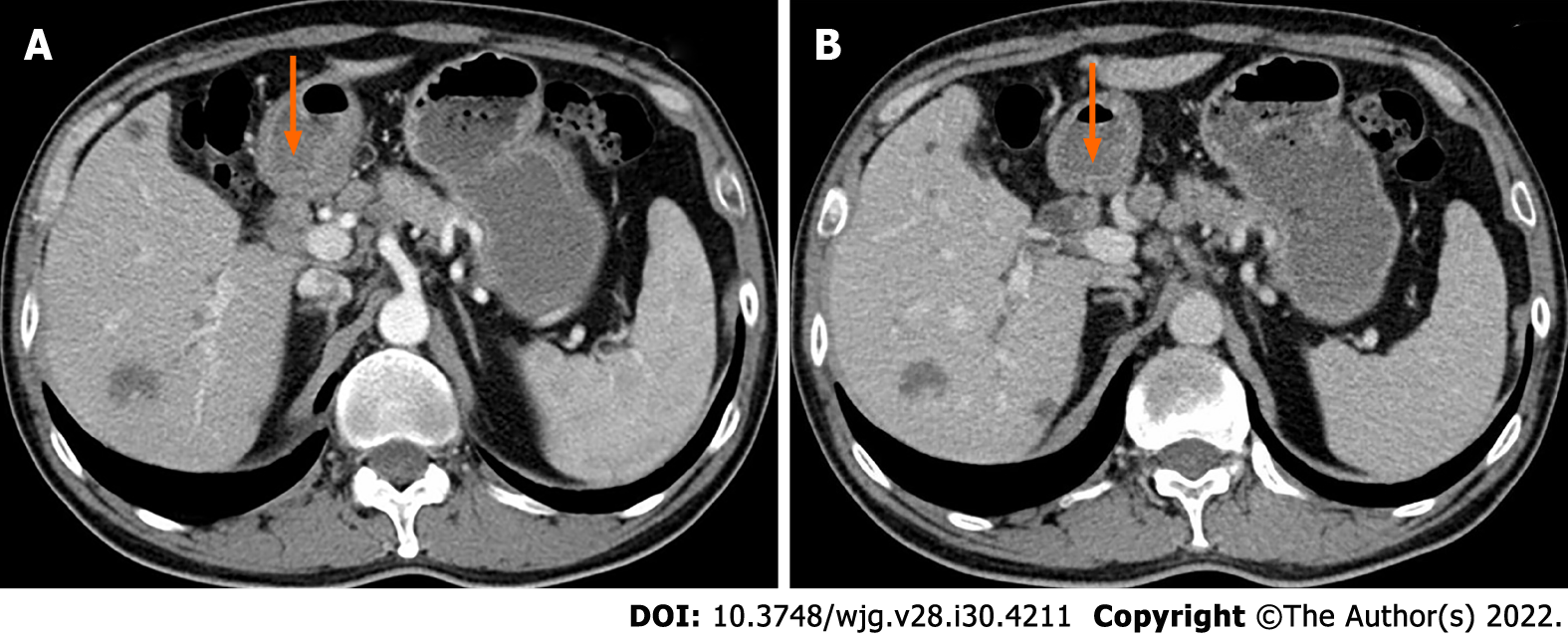
The patient underwent an abdominal ultrasound (US) examination by a Resona7 US system (Mindray Medical International, Shenzhen, Guangdong Province, China) equipped with an SC6-1U (1-6 MHz) transducer. The US revealed mild to moderate dilatation of the intrahepatic bile duct, and the diameter of the upper extrahepatic bile duct was 1.2 cm (Figure 1A). A hyperechoic nodule sized 0.8 cm × 0.6 cm was found in the upper extrahepatic bile duct with an almost regular shape and slightly clear margins (Figure 1B). The patient underwent CEUS with the patient’s consent for further diagnosis. A 2.4-mL US contrast agent SonoVue (Bracco, Milan, Italy) suspension was injected through the left cubital vein followed by a flush with 5 mL saline. In the arterial phase, the nodule showed slight heterogeneous hyperenhancement without rim-like enhancement (Figure 1C). The nodule appeared heterogeneous isoenhancement in the venous phase (Figure 1D). Additional CECT in our hospital showed a hypoenhancement nodule approximately 1.3 cm × 1.0 cm in size in the upper extrahepatic bile duct (Figure 2).
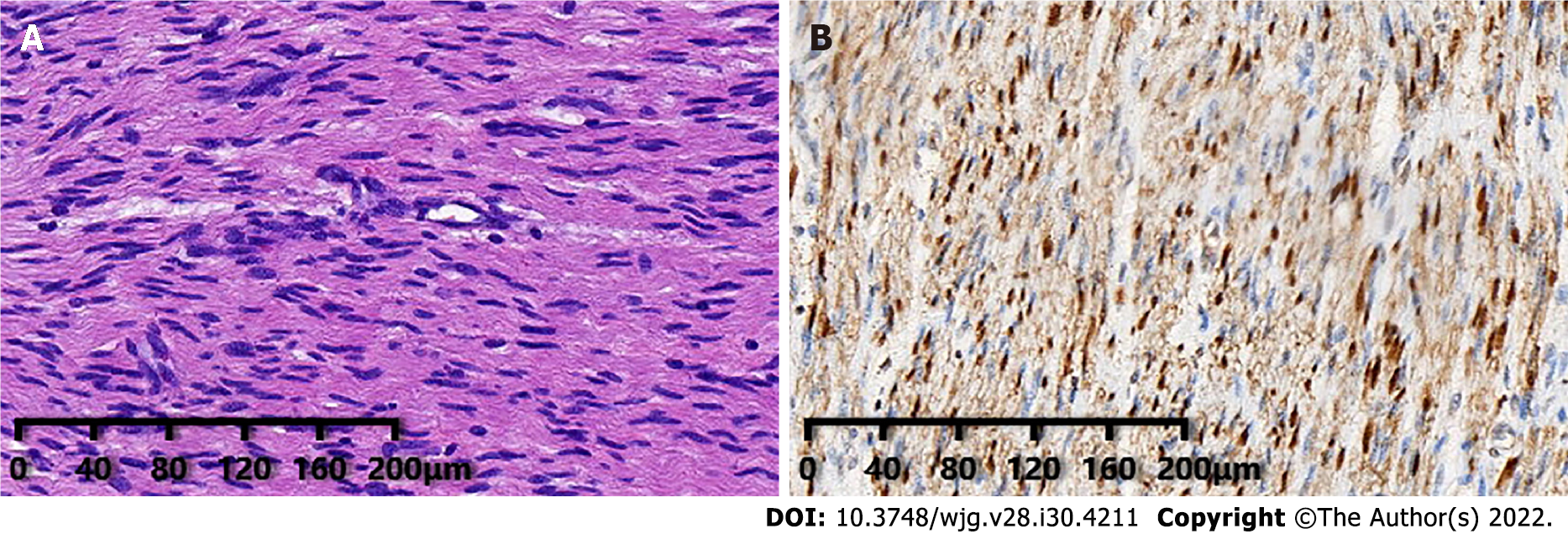
Based on the incidence of bile duct diseases, imaging findings and laboratory tests, the patient's clinical diagnosis was hilar cholangiocarcinoma. However, postoperative pathology of the common bile duct lesion showed a neoplastic proliferation of submucosal nerve tissue and fibrous tissue (Figure 3A), and an immunohistochemistry marker was positive for S-100 (Figure 3B). The above pathological findings indicated that the lesion in the bile duct was a traumatic neuroma.
During the surgery, intraoperative frozen pathology showed no tumor cells within the bile duct lesion. Therefore, hilar bile duct resection and end-to-end bile ductal anastomosis (EE) were performed. The patient recovered uneventfully after surgery.
There was no obvious abnormality on CECT for half a year after the operation.
Extrahepatic bile duct masses are commonly malignant tumors, while benign tumors account for only 6%[4-7]. Consequently, the possibility that extrahepatic bile duct lesions are traumatic neuromas is easily overlooked. It has been reported that most traumatic neuromas of the biliary tract arise in the cystic duct stump after cholecystectomy[8]. If a nerve is transected and its continuity cannot be reestablished, a traumatic neuroma may develop[9].
We reviewed the literature from 2000 to 2021 and found 18 publications regarding the imaging features of traumatic neuromas in the bile ducts[2,10-26]. The clinical findings and imaging features of these 18 reported cases are summarized in Table 1. Finally, 22 patients were included in the literature review for further analysis. The age of patients ranged from 17 to 81 years of age, and there was a significant male predominance, with 15 males (68.2%), 2 females, and 5 patients of unreported sex. Most cases were secondary to cholecystectomy, but a few were secondary to liver transplantation, hepatectomy and hilar cholangiocarcinoma. The major symptoms found in these patients were jaundice, abdominal pain, and weight loss, while some patients had no apparent symptoms.
| Ref. | Age | Sex | Symptoms | Location | Imaging findings | Preoperative diagnosis | Treatment |
| Shimura et al[10] | 70 | F | Abdominal discomfort | Extrahepatic bile duct | US: Hypoechoic tumor, bile duct slightly dilated | Did not indicate bile duct carcinoma | Bile duct excision and a Roux-en-Y hepaticojejunostomy |
| CT: Round, hyperdense, distinct margin tumor | |||||||
| Angiography: No encasement of the surrounding major vessels | |||||||
| Endoscopic retrograde cholangiography: A protuberant nodule | |||||||
| Intraductal ultrasonography: A smooth hypoechoic tumor | |||||||
| Watanabe et al[11] | 48 | M | Jaundice | Extrahepatic bile duct | Cholangiogram via the percutaneous transhepatic biliary drainage tube: The extrahepatic bile duct severely stenotic | ND | Bile duct excision and a Roux-en-Y hepaticojejunostomy |
| Iannelli et al[12] | 81 | M | Jaundice | Common bile duct | US: Dilatation of the intrahepatic bile ducts | ND | Bile duct excision and a Roux-en-Y hepaticojejunostomy |
| MRCP: A focal stricture | |||||||
| Ueno et al[2] | 60 | M | Jaundice | Mid-common bile duct | US: Dilatation of the bile ducts, a mildly echogenic mass | Could not confirm benign or malignant nature | Bile duct excision and a hepato-jejunal anastomosis |
| CT: Dilatation of the bile ducts, a markedly enhanced nodule | |||||||
| MRI: Dilatation of the bile ducts. Homogeneous enhanced nodule with an iso-intense to the aorta, both in the arterial and portal phase | |||||||
| Percutaneous transhepatic cholangiography: Dilatation of the bile ducts and a smooth stricture | |||||||
| Choi et al[13] | 46 | M | Increased liver enzymes | Right hepatic duct | CT: A mass approximately 2 cm | A bile duct cancer could not be excluded | Right hemihepatectomy |
| MRI: A mass approximately 2 cm | |||||||
| Kim et al[14] | 76 | M | ND | Mid-bile duct | CT: A small enhancing nodule | ND | Segmental resection with a Roux-en-Y hepaticojejunostomy |
| MRC: Eccentric wall thickening of the bile duct consistent with a neoplasm | |||||||
| Cheng et al[15] | 33 | F | Jaundice and weight loss | Remnant choledochal cyst | MRI: A mass | Cholangiocarcinoma | Excision of the remnant choledochal cyst and a new hepaticojejunostomy |
| Cheng et al[16] | 56 | M | Jaundice, abdominal pain and weight loss | Distal extrahepatic bile duct | US: Dilatation of bile duct | Ampullary or periampullary carcinoma | Pancreaticoduodenectomy |
| MRI: Dilatation of bile duct, a filling-defect in the distal bile duct and a thickened biliary wall around the ampulla of Vater | |||||||
| Cheng et al[17] | 68 | M | Progressive jaundice and abdominal pain | Bifurcation of the left and right hepatic duct | MRI: A mass with enhancement, a stricture of the hilar bile duct, dilatation of bile ducts | Cholangiocarcinoma | Excision of the mass and a new Roux-en-Y hepaticojejunostomy |
| Navez et al[18] | ND | ND | Jaundice (3 patients) or liver function test alteration (1 patient), a retro-obstructive choleperitoneum on the downstream biliary stenosis (1 patient) | Anastomotic biliary stricture | CT: Anastomotic biliary stricture (4 patients) | ND | Traumatic biliary neuromas resection combined with hepaticojejunostomy (1 patient); traumatic biliary neuromas resection and duct-to-duct biliary reconstruction protected by a T-tube (4 patients) |
| MRI: A markedly homogeneous high intensity nodule enhanced on portal-phase (1 patient), anastomotic biliary stricture (4 patients) | |||||||
| Terzi et al[19] | 17 | F | Persistent elevated transaminase and bilirubin levels | Anastomotic biliary | Percutaneous transhepatic cholangiography: A biliary stricture at the anastomosis | ND | Resection of the bile duct stricture and a Roux-en-Y hepaticojejunostomy |
| Toyonaga et al[20] | 76 | F | A bile duct nodule | Proximal common bile duct | CT: An 8 mm, smooth, and uniformly enhanced nodule | Submucosal tumor | Biopsy, observation for 1 year, no changes to the nodule |
| Contrast enhanced endoscopic ultrasonography: A clear boundary and a low echoic nodule, uniformly enhanced at early | |||||||
| Cholangioscopy: A smooth elevated lesion, covered with normal mucosa | |||||||
| Yang et al[21] | 65 | M | Jaundice | Right bile duct | MRI: A 1.0 cm × 1.5 cm mass | Cholangiocarcinoma | Resection of the mass and Roux-en-Y hepaticojejunostomy. |
| Hirohata et al[22] | 60 | F | No chief complaint | Junction of the cystic duct | US: A 6 mm round tumor, surrounding lymph nodes were not swollen | Cholangiocarcinoma | Surgery |
| MRI: A slightly high signal on T2 and the periphery remnant cystic duct of the tumor presented as a high-intensity lesion on T2 | |||||||
| EUS: A residual cystic duct tumor with enhancement | |||||||
| ERCP: Not invade the common bile duct | |||||||
| Yasuda et al[23] | 76 | M | ND | Stump of the dilatated cystic duct | EUS: A hypoechoic oval mass with a hyperechoic rim on the surface, 14 mm in diameter, hypervascularity | Amputation neuroma | Biopsy, observation |
| Cholangiogram: A hemispherical defect | |||||||
| Cholangioscopy: A hemispherical mass covered with thin normal cystic duct epithelium | |||||||
| Lalchandani et al[24] | 41 | M | Epigastric pain, weight loss, tea-colored urine | Common hepatic duct | US: Dilation of the bile ducts | Acute cholangitis | First: Biliary stent Finally: Bile duct resection and hepaticojejunostomy |
| ERCP: A 3-4 cm stricture | |||||||
| Kim et al[25] | 72 | M | A duodenal subepithelial tumor during a medical checkup | Near the duodenal wall and the cystic duct stump | CT: A 1.4 cm mass | Duodenal subepithelial tumor | Resection of the mass and duodenal wall, en-block resection of the mass and cystic duct origin |
| EUS: An 18 mm hypoechoic mass | |||||||
| Nechi et al[26] | 76 | M | Jaundice | The transition zone between the common hepatic duct and the main bile duct | US: Dilation of the bile ducts, a 5 mm hypoechoic nodule | Could not confirm benign or malignant nature | Resection of the main bile duct with a choledocho-duodenal anastomosis |
| MRI: Dilation of the common hepatic duct |
Unfortunately, no specific imaging features for traumatic neuromas of the bile duct have been found at present. Although some imaging modalities, such as US, computed tomography (CT), and nuclear magnetic resonance imaging (MRI), are valuable to some extent, it remains a challenge to diagnose traumatic bile duct neuromas preoperatively[17]. Imaging findings in these 22 patients varied from nodules or masses to localized bile duct stenosis with dilatation of the upper bile duct. It has been reported in the literature that the US imaging findings of extraabdominal nerve tumors and traumatic neuromas are generally hypoechoic masses, larger than the nerve trunk and continuous with the nerve[27]. However, the nerve injury related to cholecystectomy may be too small, so we could not find that the nerve is connected to traumatic neuroma of the bile duct. US was performed in 5 of the 22 patients, 2 of whom showed hypoechoic nodules, and the remaining 3 patients showed stenosis and dilatation of the bile ducts. However, our patient's US sonogram showed a hyperechoic nodule, indicating that the echogenicity of the nodule of traumatic neuroma was variable.
CECT was performed in 2 of the 18 cases, and an enhancing nodule was seen, which was consistent with the CECT findings of our patient. Traumatic neuromas also show enhancement on MRI when a contrast agent is used[28], which may be related to a damaged peripheral nerve blood barrier that occurred during a prior insult to the nerve[29-32]. One of these 18 cases described the enhancement pattern of traumatic neuroma on MRI in detail, which showed a marked homogeneously enhanced nodule that was iso-intense to the aorta in the atrial phase and a homogeneously enhanced nodule that was iso-intense to the aorta in the portal phase. There have been a few reports of other imaging techniques for diagnosing traumatic neuromas, such as magnetic resonance cholangiopancreatography, endoscopic US, contrast-enhanced harmonic endoscopic ultrasonography, intraductal ultrasonography and percutaneous transhepatic cholangiography. None of these imaging methods revealed specific features for traumatic neuromas.
It is challenging to distinguish bile duct traumatic neuroma from other lesions before surgery, so it is often misdiagnosed. The diagnosis of bile duct traumatic neuroma was correctly diagnosed in 1 of the 18 cases examined and confirmed by biopsy. The remaining cases were not correctly diagnosed, and it was difficult to distinguish between benign and malignant lesions in most cases. Therefore, surgery would be performed on a large proportion of patients. Once the patient underwent surgery, an intraoperative frozen section examination helped to confirm that the lesion was benign and extensive surgical resection of the traumatic neuroma was avoided[2,3]. The primary treatment reported in the literature consists of bile duct excision and hepaticojejunostomy (HJ). Although HJ is frequently recommended for reconstruction, the indications, surgical options and suture selection are also controversial. Some investigators also recommend EE because it is more physiological and can maintain physiological balance[33]. It is possible to achieve excellent long-term results and high quality of life using both HJ and EE when it is feasible for the proximal and distal ductal ends to permit EE[34]. Therefore, the choice of the optimum method is strictly correlated with the morphological nature of the lesion, which is different from one stage to the other, depending upon the moment of detection, and therefore have different surgical implications[35]. The surgeon found that the anastomosed edges blood supply was good and that there was no tension of the anastomosed edges in this patient. Therefore, according to the actual conditions of patients, as well as to maintain physiological balance, our hospital professor implemented EE for this patient.
In this patient, the symptoms of anorexia, weight loss and jaundice mimicked those often caused by malignant tumors of extrahepatic bile ducts. CEUS and CECT showed enhancement of the nodule. Based on the incidence of bile duct diseases and imaging findings, the surgeons misdiagnosed it as cholangiocarcinoma. Periductal infiltrative cholangiocarcinomas account for the majority of extrahepatic cholangiocarcinomas[36]. Extrahepatic cholangiocarcinomas may show hyperenhancement, isoenhancement, or hypoenhancement in the early phase of CEUS, and most of them show hypoenhancement in the late phase[37]. If we find a nodule in the bile duct, we should rule out the diagnosis of cholangiocarcinoma when the nodule does not show hypoenhancement in the late phase of CEUS. However, when traumatic neuroma presents as localized bile duct stenosis, it is relatively difficult to distinguish it from malignant lesions. When a patient has a history of biliary system surgery and the tumor markers are not significantly elevated, suspicion of traumatic neuroma increases. If conditions permit, patients can be protected from unnecessary surgeries by confirming the diagnosis with a biopsy. CEUS is beneficial for differentiating cholangiocarcinoma from traumatic neuromas, but more cases are needed to summarize the sonographic features of this disease. Recognizing of traumatic neuromas may aid in preoperative work up, planning, and patient counseling[24].
It is difficult to correctly diagnose traumatic neuroma of the bile duct before surgery. We should rule out malignant differential diagnoses, such as cholangiocarcinoma preoperatively, to avoid unnecessary surgery. The enhancement mode of CEUS may provide information to distinguish traumatic neuromas from malignant lesions. We need to combine the history of biliary tract surgery, clinical findings, imaging findings and laboratory tests to diagnose this disease.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Society of Ultrasound, Abdomen Ultrasound Subcommittee, Chinese Medical Doctor Association, No. 199174.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cochior D, Romania; Koganti S, United States S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Foltán R, Klíma K, Spacková J, Sedý J. Mechanism of traumatic neuroma development. Med Hypotheses. 2008;71:572-576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 80] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 2. | Ueno Y, Ikeda K, Maehara M, Sakaida N, Omura N, Kurokawa H, Sawada S. Traumatic neuroma of the bile duct. Abdom Imaging. 2008;33:560-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Herrera L, Martino E, Rodríguez-Sanjuán JC, Castillo J, Casafont F, González F, Figols J, Casanueva J, Cagigas M, Gómez-Fleitas M. Traumatic neuroma of extrahepatic bile ducts after orthotopic liver transplantation. Transplant Proc. 2009;41:1054-1056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Burhans R, Myers RT. Benign neoplasms of the extrahepatic biliary ducts. Am Surg. 1971;37:161-166. [PubMed] |
| 5. | Dowdy GS Jr, Olin WG Jr, Shelton EL Jr, Waldron GW. Benign tumors of the extrahepatic bile ducts. Report of three cases and review of the literature. Arch Surg. 1962;85:503-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 44] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Duncan JT Jr, Wilson H. Benign tumor of the common bile duct. Ann Surg. 1957;145:271-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Gertsch P, Thomas P, Baer H, Lerut J, Zimmermann A, Blumgart LH. Multiple tumors of the biliary tract. Am J Surg. 1990;159:386-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 41] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Larson DM, Storsteen KA. Traumatic neuroma of the bile ducts with intrahepatic extension causing obstructive jaundice. Hum Pathol. 1984;15:287-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Shumate CR, Curley SA, Cleary KR, Ames FC. Traumatic neuroma of the bile duct causing cholangitis and atrophy of the right hepatic lobe. South Med J. 1992;85:425-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Shimura K, Tamada K, Asada M, Watabiki N, Wada I, Tanaka N, Suzuki Y. Intraductal ultrasonography of traumatic neuroma of the bile duct. Abdom Imaging. 2001;26:632-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Watanabe O, Haga S, Okabe T, Kumazawa K, Shiozawa S, Tsuchiya A, Kajiwara T, Hirotani T, Aiba M. Amputation neuroma of common bile duct with obstructive jaundice. J Gastroenterol Hepatol. 2001;16:945-946. [PubMed] [DOI] [Full Text] |
| 12. | Iannelli A, Fabiani P, Karimdjee BS, Converset S, Saint-Paul MC, Gugenheim J. Traumatic neuroma of the cystic duct with biliary obstruction. Report of a case. Acta Gastroenterol Belg. 2003;66:28-29. [PubMed] |
| 13. | Choi SB, Park YN, Kim KS. Traumatic neuroma of the right hepatic duct undertaken right hemihepatectomy. ANZ J Surg. 2009;79:91-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Kim HH, Koh YS, Seoung JS, Hur YH, Cho CK. Education and imaging. Hepatobiliary and pancreatic: traumatic bile duct neuroma. J Gastroenterol Hepatol. 2011;26:1465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Cheng Y, Jia Q, Xiong X, Cheng N. Traumatic bile duct neuroma developing in a remnant choledochal cyst. Dig Liver Dis. 2014;46:e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Cheng Y, Jia Q, Xiong X, He D, Cheng NS. Hepatobiliary and pancreatic: traumatic neuroma of the ampulla of Vater. J Gastroenterol Hepatol. 2014;29:1342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Cheng Y, Jia Q, Xiong X, Cheng N. Traumatic bile duct neuroma after resection of hilar cholangiocarcinoma. Clin Res Hepatol Gastroenterol. 2014;38:127-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Navez J, Golse N, Bancel B, Rode A, Ducerf C, Mezoughi S, Mohkam K, Mabrut JY. Traumatic biliary neuroma after orthotopic liver transplantation: a possible cause of "unexplained" anastomotic biliary stricture. Clin Transplant. 2016;30:1366-1369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Terzi A, Kirnap M, Sercan C, Ozdemir G, Ozdemir BH, Haberal M. Traumatic Neuroma Causing Biliary Stricture After Orthotopic Liver Transplant, Treated With Hepaticojejunostomy: A Case Report. Exp Clin Transplant. 2017;15:175-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Toyonaga H, Taniguchi Y, Inokuma T, Imai Y. Traumatic bile duct neuroma diagnosed by boring biopsy with cholangioscopy. Gastrointest Endosc. 2018;87:1361-1362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Yang SS, Wu X, Lu J, Cheng NS. Jaundice 8years after left hemi-hepatectomy for hepatocellular carcinoma. Clin Res Hepatol Gastroenterol. 2020;44:622-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 22. | Hirohata R, Abe T, Amano H, Kobayashi T, Shimizu A, Hanada K, Yonehara S, Nakahara M, Ohdan H, Noriyuki T. Amputation neuroma derived from a remnant cystic duct 30 years after cholecystectomy: A case report. Int J Surg Case Rep. 2019;64:184-187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Yasuda I, Kobayashi S, Nagata K, Takahashi K, Entani T. Endoscopic images of amputation neuroma at the cystic duct stump. Gastrointest Endosc. 2019;90:986-987. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Lalchandani P, Korn A, Lu JG, French SW, Hou L, Chen KT. Traumatic bile duct neuroma presenting with acute cholangitis: A case report and review of literature. Ann Hepatobiliary Pancreat Surg. 2019;23:282-285. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Kim DH, Park JH, Cho JK, Yang JW, Kim TH, Jeong SH, Kim YH, Lee YJ, Hong SC, Jung EJ, Ju YT, Jeong CY, Kim JY. Traumatic neuroma of remnant cystic duct mimicking duodenal subepithelial tumor: A case report. World J Clin Cases. 2020;8:3821-3827. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | Nechi S, Nakhli A, Ben Hamida W, Bani A, Khsiba A, Ben Mohamed A, Chelbi E, Hamzaoui L, Touinsi H. Traumatic neuroma of the bile duct: A case report. Clin Case Rep. 2021;9:e04619. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 27. | Provost N, Bonaldi VM, Sarazin L, Cho KH, Chhem RK. Amputation stump neuroma: ultrasound features. J Clin Ultrasound. 1997;25:85-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 28. | Ahlawat S, Belzberg AJ, Montgomery EA, Fayad LM. MRI features of peripheral traumatic neuromas. Eur Radiol. 2016;26:1204-1212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 42] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 29. | Pindrik J, Chhabra A, Belzberg AJ. Update on peripheral nerve surgery. Neurosurgery. 2013;60 Suppl 1:70-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 30. | Seitz RJ, Reiners K, Himmelmann F, Heininger K, Hartung HP, Toyka KV. The blood-nerve barrier in Wallerian degeneration: a sequential long-term study. Muscle Nerve. 1989;12:627-635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 60] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 31. | Aagaard BD, Lazar DA, Lankerovich L, Andrus K, Hayes CE, Maravilla K, Kliot M. High-resolution magnetic resonance imaging is a noninvasive method of observing injury and recovery in the peripheral nervous system. Neurosurgery. 2003;53:199-203; discussion 203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 68] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 32. | Liao CD, Zhang F, Guo RM, Zhong XM, Zhu J, Wen XH, Shen J. Peripheral nerve repair: monitoring by using gadofluorine M-enhanced MR imaging with chitosan nerve conduits with cultured mesenchymal stem cells in rat model of neurotmesis. Radiology. 2012;262:161-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 33. | Górka Z, Ziaja K, Wojtyczka A, Kabat J, Nowak J. End-to-end anastomosis as a method of choice in surgical treatment of selected cases of biliary handicap. Pol J Surg. 1992;64:977-979. |
| 34. | Jabłońska B, Lampe P, Olakowski M, Górka Z, Lekstan A, Gruszka T. Hepaticojejunostomy vs. end-to-end biliary reconstructions in the treatment of iatrogenic bile duct injuries. J Gastrointest Surg. 2009;13:1084-1093. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 35. | Moldovan CA, Ungureanu DF, Beliș V. A proposed therapeutic algorithm based on multiple case analysis regarding the repair options of iatrogenic biliary lesions following open and laparoscopic surgery. J Mind Med Sci. 2016;3:162-171. |
| 36. | Oliveira IS, Kilcoyne A, Everett JM, Mino-Kenudson M, Harisinghani MG, Ganesan K. Cholangiocarcinoma: classification, diagnosis, staging, imaging features, and management. Abdom Radiol (NY). 2017;42:1637-1649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 84] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 37. | Xu HX. Contrast-enhanced ultrasound in the biliary system: Potential uses and indications. World J Radiol. 2009;1:37-44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 34] [Cited by in RCA: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |