Published online Aug 14, 2022. doi: 10.3748/wjg.v28.i30.4053
Peer-review started: January 18, 2022
First decision: March 8, 2022
Revised: March 16, 2022
Accepted: July 18, 2022
Article in press: July 18, 2022
Published online: August 14, 2022
Processing time: 203 Days and 12.9 Hours
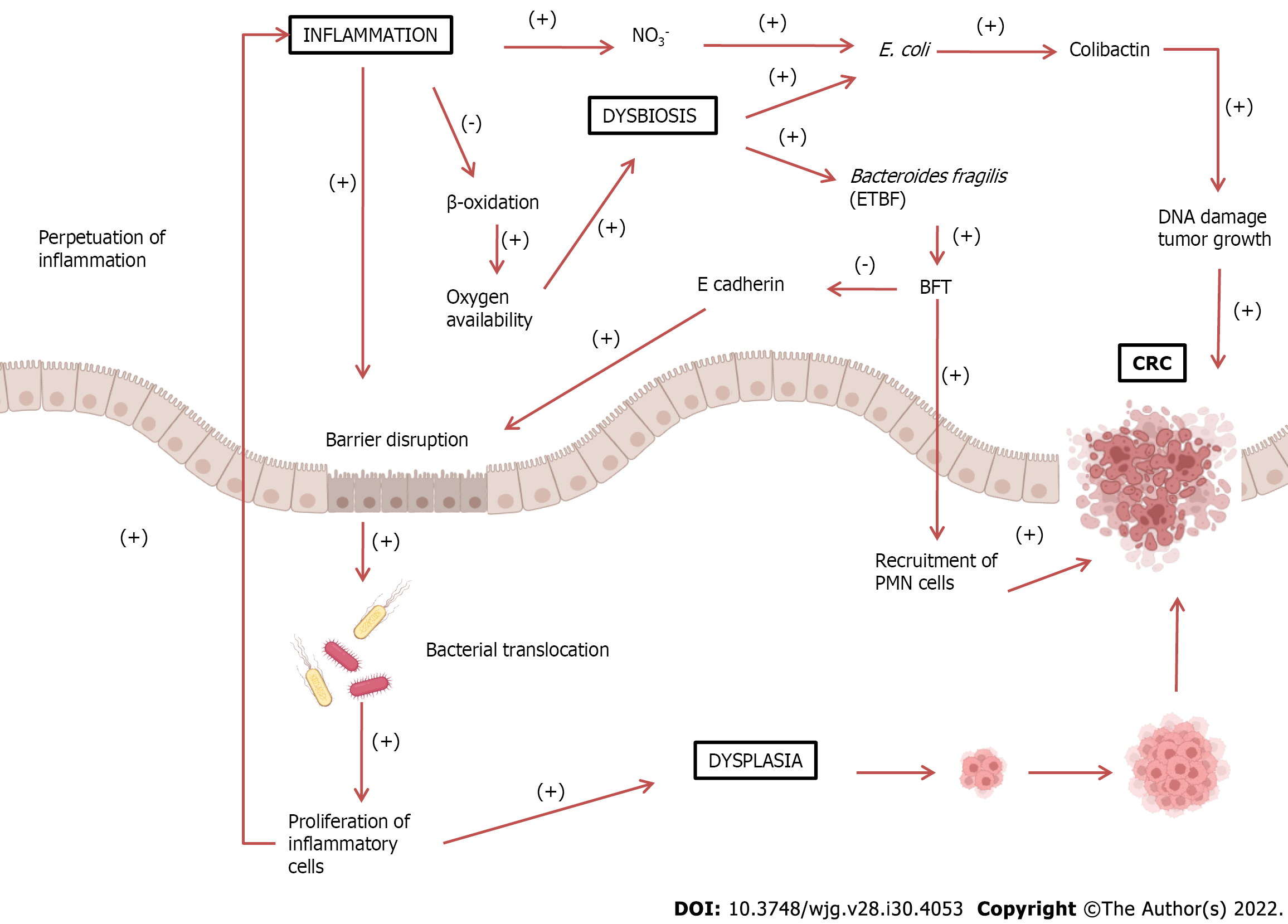
The gut microbiota is a complex community of microorganisms that inhabit the digestive tracts of humans, living in symbiosis with the host. Dysbiosis, characterized by an imbalance between the beneficial and opportunistic gut microbiota, is associated with several gastrointestinal disorders, such as irritable bowel syndrome (IBS); inflammatory bowel disease (IBD), represented by ulcerative colitis and Crohn’s disease; and colorectal cancer (CRC). Dysbiosis can disrupt the mucosal barrier, resulting in perpetuation of inflammation and carcinogenesis. The increase in some specific groups of harmful bacteria, such as Escherichia coli (E. coli) and enterotoxigenic Bacteroides fragilis (ETBF), has been associated with chronic tissue inflammation and the release of pro-inflammatory and carcinogenic mediators, increasing the chance of developing CRC, following the inflammation-dysplasia-cancer sequence in IBD patients. Therefore, the aim of the present review was to analyze the correlation between changes in the gut microbiota and the development and maintenance of IBD, CRC, and IBD-associated CRC. Patients with IBD and CRC have shown reduced bacterial diversity and abundance compared to healthy individuals, with enrichment of Firmicute sand Bacteroidetes. Specific bacteria are also associated with the onset and progression of CRC, such as Fusobacterium nucleatum, E. coli, Enterococcus faecalis, Streptococcus gallolyticus, and ETBF. Future research can evaluate the advantages of modulating the gut microbiota as preventive measures in CRC high-risk patients, directly affecting the prognosis of the disease and the quality of life of patients.
Core Tip: Dysbiosis is present in patients with inflammatory bowel disease (IBD) and colorectal cancer (CRC). Dysbiosis can lead to a disruption of the mucosal barrier of the digestive tract lining, resulting in the perpetuation of inflammation and carcinogenesis, thus increasing the risk of developing CRC in IBD patients. Therefore, the aim of this review was to analyze the correlation between changes in gut microbiota and the development of IBD, CRC, and IBD-associated CRC. Further studies should be carried out to identify bacterial species that cause imbalances in the gut microbiota, enabling the development of prevention strategies or treatment of IBD-associated CRC.
- Citation: Quaglio AEV, Grillo TG, De Oliveira ECS, Di Stasi LC, Sassaki LY. Gut microbiota, inflammatory bowel disease and colorectal cancer. World J Gastroenterol 2022; 28(30): 4053-4060
- URL: https://www.wjgnet.com/1007-9327/full/v28/i30/4053.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i30.4053
The human microbiome is composed of several types of microbes that colonize different niches of the human body, such as the skin, lungs, vagina, and gastrointestinal tract[1]. Of these, the gut microbiota is the most studied, due to the presence of greater diversity and number of microbial species compared to other parts of the body[1,2]. The gut microbiota is a complex community of approximately 100 trillion microorganisms, such as fungi, viruses, and protists, that inhabit the digestive tracts of humans, living in symbiosis with the host[3,4].
Alterations in the gut microbiota are associated with several diseases, including inflammatory bowel disease (IBD) and colorectal cancer (CRC)[2]. Thus, studies aimed at elucidating the role of the microbiota in each phase of each disease are necessary. Based on changes in the intestinal microbiota, new diagnostic tools and possible treatments can be developed. Further, studies aiming to correlate alterations in the microbiota or in specific bacterial populations with the diagnosis, prognosis, and/or treatment of diseases are necessary. Therefore, this mini-review was conducted to determine the correlation between changes in the gut microbiota and IBD, CRC, and IBD-associated CRC.
At birth, the intestinal tract is sterile[2], with bacterial colonization beginning as early as during the passage of the baby through the birth canal[5]. Colonization continues through feeding and other environmental contacts. Several factors are known to influence colonization, including gestational age, mode of delivery (vaginal birth vs cesarean delivery), diet (breast milk vs formula) and exposure to antibiotics, and sanitation[2].
During the first year of life, the microbial composition of the mammalian intestine is relatively simple and characterized by low diversity with relative dominance of species from the phyla Proteobacteria and Actinobacteria[2,5]. Over time, the microbiota becomes more diverse, with the Firmicutes and Bacteroidetes phyla later emerging as the predominant microbes characterizing the adult microbiota[2,6-8].
In an adult individual, over 90% of intestinal bacteria belong to Firmicutes, Bacteroidetes, Proteobacteria, or Actinobacteria phyla[4,7]. The gut microbiota can be differentiated into beneficial bacteria and opportunistic bacteria, the latter of which can cause infection[8]. Lactobacillus, Bifidobacterium, Enterococci, and Propionobacteria are some of the beneficial microbes, while the opportunistic groups include Bacteriodes, Bacilli, Clostridia, Enterobacteria, Actinobacteria, Peptococci, Staphylococci, and Streptococci[8].
The benefits of the gut microbiota to the host’s physiology are vast, including nutrition, immune development, and host defense[4,7]. In the field of nutrition, some bacterial species, such as Bifidobacterium, participate in the biosynthesis of several components as vitamin K and vitamin B[7]. In addition, some can provide short-chain fatty acids (SCFAs) by fermenting dietary fibers[7,9]. SCFAs are a group of small fatty acids (2 to 5 carbons) produced by anaerobic microorganisms that, after absorption, have systemic immunomodulatory and anti-inflammatory properties[9].
The most abundant SCFAs in the colon are acetate, propionate, and butyrate[7,9,10], which promote the proliferation of beneficial bacteria and stimulate regulatory T cells to reduce inflammatory mediators, associated with an increase in colonic oxygen consumption by epithelial cells, and enhancing immune regulation, and gut barrier function[9-11].
Imbalance between the beneficial and opportunistic groups causes dysbiosis, which is associated with gastrointestinal disorders such as IBS, IBD, and CRC[4,7,8].
IBD, a heterogeneous chronic and relapsing inflammatory illnesses of the digestive system, is traditionally classified into ulcerative colitis (UC) and Crohn’s disease (CD)[4,12,13]. Both UC and CD can cause several symptoms like diarrhea, rectal bleeding, and abdominal pain. However, inflammation in CD is transmural and can involve any part of the gastrointestinal tract. In contrast, inflammation in UC is more superficial and limited to the colon[14].
Although the cause of IBD is not fully known, genetic history is likely involved in the path
While IBD is a disease with the highest rates in industrialized countries, its incidence varies considerably worldwide, and newly industrialized areas such as India and South America presented a rapid increase in case numbers[7,13,14]. This enhancement can be related to dietary habits such as increased consumption of processed foods, sugars, and fats; overutilization of antibiotics; and an overall improvement in sanitary conditions and hygiene[13].
Nevertheless, the exact factors that trigger the first episode of inflammation and subsequent relapse remain unknown, it is now know that inflammatory episodes can result, in genetically predisposed people, from an immune response against intestinal microbial antigens under several environmental conditions[14]. Several IBD-associated susceptible genes are correlated with host responses to gut bacteria, suggesting that the gut microbiota also participate in the pathogenesis of IBD[7]. Dysbiosis is a reduction in microbial diversity, or a combination of the loss of beneficial bacteria and an increase in pathogenic bacteria[15], that may influence the pathogenesis of IBD.
The most prominent changes in the microbiota of IBD patients are the decreased diversity in bacteria species associated with decreased abundance of Bacteroidetes and Firmicutes[4,7] alongside an increase in the abundance of Proteobacteria[4].
In patients with IBD, the mucus layer is compromised, allowing luminal bacteria to penetrate and invade the submucosal layers, leading to the proliferative and inflammatory processes[4,13]. Then, mucosal destruction due to inflammatory injury further exposes the submucosa to more bacteria, leading to a vicious, positive feedback cycle of antigenic exposure and mucosal damage[13].
Faecalibacterium prausnitzii is one of the most abundant human gut bacteria and can be used as synonym of the gut health because of its anti-inflammatory and immunoregulatory properties[14]. One of the its products is butyrate, which is associated with an anti-inflammatory effect[7]. Several authors have correlated decreases in Faecalibacterium prausnitzii (F. prausnitzii) abundance with CD development[7,14,16] and in UC patients, a decrease was also observed during remission, being the recovery of the F. prausnitzii population associated with the maintenance of clinical remission[17].
Roseburia spp, including Roseburia faecis, Roseburia intestinalis (R. intestinalis), and Roseburia hominis (R. hominis), another genus of butyrate-producing bacteria, were significantly lower in healthy individuals with a high genetic risk for IBD compared to healthy individuals with low genetic risk[7]. R. hominis, specifically, was significantly reduced in UC patients, and an inverse correlation was observed between R hominis and disease severity[18]. In contrast, R. intestinalis supernatant suppressed the expression of interleukin (IL)-6 as well as the signal transducer and activator of transcription 3 (STAT3) via macrophage regulation in an in vitro experiment. Additionally, in dextran sodium sulfate- and 2,4,6-trinitrobenzene sulfonic acid-induced intestinal inflammation models, R. intestinalis supernatant reduced macrophages and Th17 cells in the colon, which was associated with the downregulation of IL-6 and STAT3[19].
In the field of pathogenic bacteria, several authors have described a relative increase in Proteobacteria, mainly Escherichia coli (E. coli), in IBD patients[7,20-22]. The exact mechanisms that lead to an increase in Proteobacteria during inflammation are not completely understood; however, Rizzatti et al[20] proposed two mechanisms: The oxygen hypothesis and the presence of nitrate. In a normal colon, epithelial cells deplete oxygen in the lumen through beta oxidation, creating an anaerobic environment[23]. In contrast, during an inflammatory episode, the beta oxidation capacity of colonic cells is decreased, thus increasing oxygen availability, which promotes dysbiosis and Proteobacteria growth[24]. Nitrate generated as a by-product during the inflammatory process conferred a growth advantage to the commensal bacteria E. coli in the large intestine, which then became predominant[25].
The increase in pathogenic bacteria in the digestive tract that can adhere to the colonic mucosa could alters the gut permeability, modifying the diversity and composition of intestinal microbiota, and ultimately leading to intestinal inflammation by regulating inflammatory genes expression[7].
Dysbiosis can further alter bacterial metabolites; decreased concentration of SCFAs has been reported as a result of a diminish in butyrate-producing bacteria like F. prausnitzii, in patients with IBD and in animal models of intestinal inflammation[7,9,10]. Decreased levels of SCFAs affects the differentiation and expansion of Treg cells and the growth of epithelial cells[26], leading to the loss of intestinal homeostasis.
CRC is the third most common cancer, and the second most frequent cause of cancer deaths worldwide being more common in developed than in developing countries[27,28]. Notwithstanding cases in all countries are on the rise, most CRC cases occur in Western countries, where there is an increase in incidence[28]. CRC rates in older adults in the United States have declined in recent years probably due to increased screening, but rates in younger adults have been rising, which may be correlated with higher incidence of obesity and other diet and lifestyle trends in the western hemisphere[29].
The exact mechanism for CRC onset and progression has not been fully elucidated, but it is generally believed to be the result of extensive and complex interactions between genetic and environmental factors[30]. According to Olovo et al[28], the progression of adenoma to carcinoma could be linked to the gut microbiota and conversely, a healthy microbiota is correlated with a minor risk of advanced adenoma[28].
Several factors that affect the gut microbiota are thought to be related to colon carcinogenesis, such as obesity, a high-fat diet, smoking, and frequent consumption of alcohol[30].
Patients with CRC have shown reduced bacterial diversity and abundance compared to healthy individuals, with enrichment of Firmicutes and Bacteroidetes[31]. Specific bacteria are also associated with the onset and progression of CRC, such as Fusobacterium nucleatum, E. coli, Enterococcus faecalis, Streptococcus gallolyticus, and enterotoxigenic Bacteroides fragilis (ETBF)[32].
The abundance of Fusobacterium nucleatum, an opportunistic pathogen found normally in the oral cavity, is correlated with age and tumor diameter in CRC patients[31,33,34]. Additionally, an overa
There is plenty of evidence of the tumor-promoting effects of Streptococcus gallolyticus in colon cells[35-37]. Colonic cells incubated with Streptococcus gallolyticus (S. gallolyticus) presented increased levels of β-catenin, c-Myc, and proliferating cell nuclear antigen (PCNA), all of which are transcription factors associated with cancer development[35]. In addition, in mice, administration of S. gallolyticus leads to more tumors, higher tumor burden, and dysplasia grade, and increased cell proliferation and β-catenin staining in colonic crypts compared to mice incubated with control bacteria[35]. Furthermore, CRC patients present high levels of this bacterium compared to healthy individuals[37]. However, CRC-specific conditions, such as the increased concentration of bile acids, could also promote S. gallolyticus colonization, creating a maintenance cycle for high levels of this bacterium in the gut[37].
ETBF is the most frequent anaerobe isolated from cases of diarrhea, peritonitis, intra-abdominal abscesses, and sepsis, and there is a positive correlation between the presence of ETBF and active IBD and CRC[38]. According to Appunni et al[39], co-colonization of toxigenic E. coli and ETBF in mice resulted in increased production of pro-inflammatory IL-17 and subsequent DNA damage, which could accelerate the development of CRC[39]. In addition, the toxin in ETBF could induce c-myc expression and IL-8 secretion causing oxidative DNA and epithelial barrier damage, and STAT3/Th17 immune responses activation, which are further correlated with an increased risk of CRC[38].
Intestinal inflammation is one of the most common risk factors for developing CRC. Besides being two to six times more likely to develop CRC than healthy people, IBD patients with cancer are affected younger than sporadic CRC patients[40]. Disease duration, extension of the lesions, inflammation, sclerosing cholangitis, age at onset and onset in childhood are factors linking IBD with an increased incidence of CRC[41,42].
Chronic inflammation initiates and drives tumorigenesis[42], leading to an “inflammation-dysplasia-carcinoma” sequence, not the “adenoma-sequence” classically described in sporadic CRC[40].
Popov et al[43]proposed the three main theories about bacterial involvement in the development of IBD-associated CRC: The alpha-bug hypothesis, driver-passenger hypothesis, and common ground hypothesis. In the alpha-bug hypothesis, a single bacterium (normally ETBF) is thought to cause all modifications and damage that lead to carcinogenesis. The driver-passenger hypothesis is similar, but after the attack by the first bacteria, other opportunistic bacteria start to grow and contribute to cancer development. Finally, in the common ground hypothesis, endogenous and exogenous factors form a “leaky gut,” allowing the passage of bacteria into the submucosal tissue, leading to chronic inflammation and the consequent emergence of cancer[43].
It is known that bacteria, through pathogen-associated molecular patterns (PAMPs), are capable of communicating with the tool-like receptors (TLRs), retinoic acid-inducible gene I-like receptors (RLRs), and nucleotide binding oligomerization domain-receptors (NLRs), and trigger an immune response[42]. Nuclear factor kB (NF-kB) can be activated by the TLR and tumor necrosis factor-α (TNF-α), inducing the transcription of several tumorigenesis genes such as COX-2, which then leads to the apoptosis of intestinal epithelial cells via tumor suppressor p53 pathways[40] and consequent breakdown of the intestinal barrier, allowing microbial translocation.
Increased quantities of Proteobacteria are associated with decreased levels of SCFAs and increased colonic inflammation[43]. In addition, intestinal Dysbiosis and barrier defects, associated with alterations in mucin secretion may happen even in the absence of active inflammation[43], perpetuating a favorable environment for the emergence of CRC.
Several studies have demonstrated the participation of bacteria such as E. coli, ETBF, and Fusobacterium nucleatum in chronic inflammation and cancer development in IBD patients[40,42-45].
A review by Yu et al[44] concluded that commensal bacteria, E. coli and E. faecalis, isolated from healthy subjects are capable of initiating intestinal inflammation in genetically deficient mice, suggesting that opportunistic commensal bacteria may become pathogenic only in genetically predisposed hosts[44]. Nevertheless, some types of E. coli can produce colibactin, a genotoxic compound capable of promoting tumor growth, alkylating DNA, and inducing tumorigenic double-stranded breaks[45]. According to Yang et al[45], inflammation may upregulate bacterial virulence genes, such as colibactin, and facilitate colonization of the mucosa, leading to increased colibactin-induced DNA damage in colonic epithelial cells, allowing this bacterial strain to exert its carcinogenic activity[42].
The enterotoxin produced by ETBF known as bacteroides fragilis toxin, acted as a metalloprotease cleaving E-cadherin, a major constituent of the zonula adherens, which is responsible for cell adhesion[46]. This toxin can trigger an inflammatory, pro-tumoral signaling caspase in colonic epithelial cells that cause the recruitment of polymorphonuclear immature myeloid cells to promote colon cancers[44].
There is a consensus that dysbiosis is present in both IBD and CRC, and that dysbiosis could lead to a disruption of the mucosal barrier with perpetuation of inflammation and carcinogenesis. Dysbiosis with a consequent increase in bacteria, such as E. coli and ETBF, is believed to lead to a breakdown of the intestinal mucosal barrier, allowing the translocation of more bacteria from the lumen to the interior of the tissue. This condition leads to chronic tissue inflammation, with the release of inflammatory and pro-carcinogenic mediators increasing the risk of developing CRC. This positive feedback loop of dysbiosis could be the basis for the inflammation-dysplasia-cancer sequence (Figure 1).
Further studies should be carried out to identify which bacteria or which set of bacteria may be responsible for this feedback cycle. Understanding the mechanism behind dysbiosis cycles may be the basis for preventing or treating IBD-associated CRC and CRC. Future research should evaluate the advantages of modulating the intestinal microbiota as a protective factor for the development of IBD-associated CRC; thus, the use of prebiotics, probiotics, or diet-based treatment can be used as preventive measures in CRC high-risk patients, directly affecting the prognosis of the disease and the quality of life of patients living with IBD.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Budin C, Romania; Houston KV, United States S-Editor: Chen YL L-Editor: A P-Editor: Chen YL
| 1. | Michaudel C, Sokol H. The Gut Microbiota at the Service of Immunometabolism. Cell Metab. 2020;32:514-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 189] [Article Influence: 37.8] [Reference Citation Analysis (0)] |
| 2. | Quigley EM. Gut bacteria in health and disease. Gastroenterol Hepatol (N Y). 2013;9:560-569. [PubMed] |
| 3. | Kc D, Sumner R, Lippmann S. Gut microbiota and health. Postgrad Med. 2020;132:274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 4. | Gomaa EZ. Human gut microbiota/microbiome in health and diseases: a review. Antonie Van Leeuwenhoek. 2020;113:2019-2040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 701] [Article Influence: 140.2] [Reference Citation Analysis (4)] |
| 5. | Sekirov I, Russell SL, Antunes LC, Finlay BB. Gut microbiota in health and disease. Physiol Rev. 2010;90:859-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2501] [Cited by in RCA: 2749] [Article Influence: 183.3] [Reference Citation Analysis (1)] |
| 6. | Eckburg PB, Bik EM, Bernstein CN, Purdom E, Dethlefsen L, Sargent M, Gill SR, Nelson KE, Relman DA. Diversity of the human intestinal microbial flora. Science. 2005;308:1635-1638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5700] [Cited by in RCA: 5592] [Article Influence: 279.6] [Reference Citation Analysis (2)] |
| 7. | Nishida A, Inoue R, Inatomi O, Bamba S, Naito Y, Andoh A. Gut microbiota in the pathogenesis of inflammatory bowel disease. Clin J Gastroenterol. 2018;11:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 533] [Cited by in RCA: 905] [Article Influence: 113.1] [Reference Citation Analysis (3)] |
| 8. | Roy Sarkar S, Banerjee S. Gut microbiota in neurodegenerative disorders. J Neuroimmunol. 2019;328:98-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 212] [Article Influence: 35.3] [Reference Citation Analysis (1)] |
| 9. | Almeida-Junior LD, Curimbaba TFS, Chagas AS, Quaglio AEV, Di Stasi LC. Dietary intervention with green dwarf banana flour (Musa sp. AAA) modulates oxidative stress and colonic SCFAs production in the TNBS model of intestinal inflammation. J Funct Foods. 2017;38:497-504. |
| 10. | Curimbaba TFS, Almeida-Junior LD, Chagas AS, Quaglio AEV, Herculano AM, Di Stasi LC. Prebiotic, antioxidant and anti-inflammatory properties of edible Amazon fruits. Food Biosci. 2020;100599. |
| 11. | Mills S, Stanton C, Lane JA, Smith GJ, Ross RP. Precision Nutrition and the Microbiome, Part I: Current State of the Science. Nutrients. 2019;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 131] [Cited by in RCA: 206] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 12. | Matsuoka K, Kanai T. The gut microbiota and inflammatory bowel disease. Semin Immunopathol. 2015;37:47-55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 407] [Cited by in RCA: 573] [Article Influence: 52.1] [Reference Citation Analysis (1)] |
| 13. | Ghouri YA, Tahan V, Shen B. Secondary causes of inflammatory bowel diseases. World J Gastroenterol. 2020;26:3998-4017. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 54] [Cited by in RCA: 49] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 14. | Ryma T, Samer A, Soufli I, Rafa H, Touil-Boukoffa C. Role of Probiotics and Their Metabolites in Inflammatory Bowel Diseases (IBDs). Gastroenterol Insights. 2021;12:56-66. [RCA] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (2)] |
| 15. | Humphreys C. Intestinal Permeability. 5th ed. Pizzorno JE, Murray, MT, editors. Textbook of Natural Medicine, 2020: 166-177. [DOI] [Full Text] |
| 16. | Zuo T, Ng SC. The Gut Microbiota in the Pathogenesis and Therapeutics of Inflammatory Bowel Disease. Front Microbiol. 2018;9:2247. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 380] [Cited by in RCA: 403] [Article Influence: 57.6] [Reference Citation Analysis (0)] |
| 17. | Varela E, Manichanh C, Gallart M, Torrejón A, Borruel N, Casellas F, Guarner F, Antolin M. Colonisation by Faecalibacterium prausnitzii and maintenance of clinical remission in patients with ulcerative colitis. Aliment Pharmacol Ther. 2013;38:151-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 187] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 18. | Machiels K, Joossens M, Sabino J, De Preter V, Arijs I, Eeckhaut V, Ballet V, Claes K, Van Immerseel F, Verbeke K, Ferrante M, Verhaegen J, Rutgeerts P, Vermeire S. A decrease of the butyrate-producing species Roseburia hominis and Faecalibacterium prausnitzii defines dysbiosis in patients with ulcerative colitis. Gut. 2014;63:1275-1283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1036] [Cited by in RCA: 1337] [Article Influence: 121.5] [Reference Citation Analysis (3)] |
| 19. | Luo W, Shen Z, Deng M, Li X, Tan B, Xiao M, Wu S, Yang Z, Zhu C, Tian L, Wu X, Meng X, Quan Y, Wang X. Roseburia intestinalis supernatant ameliorates colitis induced in mice by regulating the immune response. Mol Med Rep. 2019;20:1007-1016. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 20. | Rizzatti G, Lopetuso LR, Gibiino G, Binda C, Gasbarrini A. Proteobacteria: A Common Factor in Human Diseases. Biomed Res Int. 2017;2017:9351507. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 388] [Cited by in RCA: 796] [Article Influence: 99.5] [Reference Citation Analysis (0)] |
| 21. | Nishino K, Nishida A, Inoue R, Kawada Y, Ohno M, Sakai S, Inatomi O, Bamba S, Sugimoto M, Kawahara M, Naito Y, Andoh A. Analysis of endoscopic brush samples identified mucosa-associated dysbiosis in inflammatory bowel disease. J Gastroenterol. 2018;53:95-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 344] [Cited by in RCA: 312] [Article Influence: 44.6] [Reference Citation Analysis (0)] |
| 22. | Vester-Andersen MK, Mirsepasi-Lauridsen HC, Prosberg MV, Mortensen CO, Träger C, Skovsen K, Thorkilgaard T, Nøjgaard C, Vind I, Krogfelt KA, Sørensen N, Bendtsen F, Petersen AM. Increased abundance of proteobacteria in aggressive Crohn's disease seven years after diagnosis. Sci Rep. 2019;9:13473. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 98] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 23. | Rivera-Chávez F, Lopez CA, Bäumler AJ. Oxygen as a driver of gut dysbiosis. Free Radic Biol Med. 2017;105:93-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 213] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 24. | Hughes ER, Winter MG, Duerkop BA, Spiga L, Furtado de Carvalho T, Zhu W, Gillis CC, Büttner L, Smoot MP, Behrendt CL, Cherry S, Santos RL, Hooper LV, Winter SE. Microbial Respiration and Formate Oxidation as Metabolic Signatures of Inflammation-Associated Dysbiosis. Cell Host Microbe. 2017;21:208-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 253] [Article Influence: 31.6] [Reference Citation Analysis (0)] |
| 25. | Winter SE, Winter MG, Xavier MN, Thiennimitr P, Poon V, Keestra AM, Laughlin RC, Gomez G, Wu J, Lawhon SD, Popova IE, Parikh SJ, Adams LG, Tsolis RM, Stewart VJ, Bäumler AJ. Host-derived nitrate boosts growth of E. coli in the inflamed gut. Science. 2013;339:708-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 602] [Cited by in RCA: 749] [Article Influence: 62.4] [Reference Citation Analysis (1)] |
| 26. | Atarashi K, Tanoue T, Oshima K, Suda W, Nagano Y, Nishikawa H, Fukuda S, Saito T, Narushima S, Hase K, Kim S, Fritz JV, Wilmes P, Ueha S, Matsushima K, Ohno H, Olle B, Sakaguchi S, Taniguchi T, Morita H, Hattori M, Honda K. Treg induction by a rationally selected mixture of Clostridia strains from the human microbiota. Nature. 2013;500:232-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1875] [Cited by in RCA: 2142] [Article Influence: 178.5] [Reference Citation Analysis (2)] |
| 27. | Weitz J, Koch M, Debus J, Höhler T, Galle PR, Büchler MW. Colorectal cancer. Lancet. 2005;365:153-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 862] [Cited by in RCA: 948] [Article Influence: 47.4] [Reference Citation Analysis (0)] |
| 28. | Olovo CV, Huang X, Zheng X, Xu M. Faecal microbial biomarkers in early diagnosis of colorectal cancer. J Cell Mol Med. 2021;25:10783-10797. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 29. | Kehm RD, Lima SM, Swett K, Mueller L, Yang W, Gonsalves L, Terry MB. Age-specific Trends in Colorectal Cancer Incidence for Women and Men, 1935-2017. Gastroenterology. 2021;161:1060-1062.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 30. | Zhang W, An Y, Qin X, Wu X, Wang X, Hou H, Song X, Liu T, Wang B, Huang X, Cao H. Gut Microbiota-Derived Metabolites in Colorectal Cancer: The Bad and the Challenges. Front Oncol. 2021;11:739648. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 53] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 31. | Silva M, Brunner V, Tschurtschenthaler M. Microbiota and Colorectal Cancer: From Gut to Bedside. Front Pharmacol. 2021;12:760280. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (1)] |
| 32. | Liu K, Yang X, Zeng M, Yuan Y, Sun J, He P, Xie Q, Chang X, Zhang S, Chen X, Cai L, Xie Y, Jiao X. The Role of Fecal Fusobacterium nucleatum and pks+ Escherichia coli as Early Diagnostic Markers of Colorectal Cancer. Dis Markers. 2021;2021:1171239. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (2)] |
| 33. | Brennan CA, Garrett WS. Fusobacterium nucleatum - symbiont, opportunist and oncobacterium. Nat Rev Microbiol. 2019;17:156-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 359] [Cited by in RCA: 734] [Article Influence: 146.8] [Reference Citation Analysis (0)] |
| 34. | Jin M, Shang F, Wu J, Fan Q, Chen C, Fan J, Liu L, Nie X, Zhang T, Cai K, Ogino S, Liu H. Tumor-Associated Microbiota in Proximal and Distal Colorectal Cancer and Their Relationships With Clinical Outcomes. Front Microbiol. 2021;12:727937. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 35. | Kumar R, Herold JL, Schady D, Davis J, Kopetz S, Martinez-Moczygemba M, Murray BE, Han F, Li Y, Callaway E, Chapkin RS, Dashwood WM, Dashwood RH, Berry T, Mackenzie C, Xu Y. Streptococcus gallolyticus subsp. gallolyticus promotes colorectal tumor development. PLoS Pathog. 2017;13:e1006440. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 107] [Cited by in RCA: 156] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 36. | Kumar R, Herold JL, Taylor J, Xu J, Xu Y. Variations among Streptococcus gallolyticus subsp. gallolyticus strains in connection with colorectal cancer. Sci Rep. 2018;8:1514. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 37. | Oehmcke-Hecht S, Mandl V, Naatz LT, Dühring L, Köhler J, Kreikemeyer B, Maletzki C. Streptococcus gallolyticus abrogates anti-carcinogenic properties of tannic acid on low-passage colorectal carcinomas. Sci Rep. 2020;10:4714. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 38. | Haghi F, Goli E, Mirzaei B, Zeighami H. The association between fecal enterotoxigenic B. fragilis with colorectal cancer. BMC Cancer. 2019;19:879. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 136] [Article Influence: 22.7] [Reference Citation Analysis (1)] |
| 39. | Appunni S, Rubens M, Ramamoorthy V, Tonse R, Saxena A, McGranaghan P, Kaiser A, Kotecha R. Emerging Evidence on the Effects of Dietary Factors on the Gut Microbiome in Colorectal Cancer. Front Nutr. 2021;8:718389. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 40. | Keller DS, Windsor A, Cohen R, Chand M. Colorectal cancer in inflammatory bowel disease: review of the evidence. Tech Coloproctol. 2019;23:3-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 174] [Article Influence: 29.0] [Reference Citation Analysis (0)] |
| 41. | Olén O, Erichsen R, Sachs MC, Pedersen L, Halfvarson J, Askling J, Ekbom A, Sørensen HT, Ludvigsson JF. Colorectal cancer in ulcerative colitis: a Scandinavian population-based cohort study. Lancet. 2020;395:123-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 312] [Article Influence: 62.4] [Reference Citation Analysis (0)] |
| 42. | Lucafò M, Curci D, Franzin M, Decorti G, Stocco G. Inflammatory Bowel Disease and Risk of Colorectal Cancer: An Overview From Pathophysiology to Pharmacological Prevention. Front Pharmacol. 2021;12:772101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 75] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 43. | Popov J, Caputi V, Nandeesha N, Rodriguez DA, Pai N. Microbiota-Immune Interactions in Ulcerative Colitis and Colitis Associated Cancer and Emerging Microbiota-Based Therapies. Int J Mol Sci. 2021;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 51] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 44. | Yu LC. Microbiota dysbiosis and barrier dysfunction in inflammatory bowel disease and colorectal cancers: exploring a common ground hypothesis. J Biomed Sci. 2018;25:79. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 167] [Cited by in RCA: 280] [Article Influence: 40.0] [Reference Citation Analysis (1)] |
| 45. | Yang Y, Gharaibeh RZ, Newsome RC, Jobin C. Amending microbiota by targeting intestinal inflammation with TNF blockade attenuates development of colorectal cancer. Nat Cancer. 2020;1:723-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 46. | Zamani S, Taslimi R, Sarabi A, Jasemi S, Sechi LA, Feizabadi MM. Enterotoxigenic Bacteroides fragilis: A Possible Etiological Candidate for Bacterially-Induced Colorectal Precancerous and Cancerous Lesions. Front Cell Infect Microbiol. 2019;9:449. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 105] [Cited by in RCA: 102] [Article Influence: 20.4] [Reference Citation Analysis (0)] |