Published online Aug 7, 2022. doi: 10.3748/wjg.v28.i29.3814
Peer-review started: April 9, 2022
First decision: May 9, 2022
Revised: June 7, 2022
Accepted: July 5, 2022
Article in press: July 5, 2022
Published online: August 7, 2022
Processing time: 116 Days and 3.7 Hours
Early detection of pancreatic cancer has long eluded clinicians because of its insidious nature and onset. Often metastatic or locally invasive when symp
Core Tip: Several reviews have evaluated the use of contrast-enhanced endoscopic ultrasound (CE-EUS), EUS-elastography (EUS-E), and artificial intelligence in separation. Not many have reviewed all three modalities' strengths in a single article. This article elaborates on current methods and outcomes of CE-EUS and EUS-E while reviewing the impact of artificial intelligence on the field of EUS imaging.
- Citation: Spadaccini M, Koleth G, Emmanuel J, Khalaf K, Facciorusso A, Grizzi F, Hassan C, Colombo M, Mangiavillano B, Fugazza A, Anderloni A, Carrara S, Repici A. Enhanced endoscopic ultrasound imaging for pancreatic lesions: The road to artificial intelligence. World J Gastroenterol 2022; 28(29): 3814-3824
- URL: https://www.wjgnet.com/1007-9327/full/v28/i29/3814.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i29.3814
Pancreatic ductal adenocarcinoma (PDAC) is the 5th most fatal cancer globally, and those receiving a diagnosis have only a 6% 5-year survival rate[1]. Fortunately, early detection of a PDAC, especially when smaller than 1 cm, along with timely resection can aggrandize 5-year survival rates by up to 80.4%[2]. This disease's increasing incidence and mortality trend have brought different specialists (i.e. radiologists and gastroenterologists) together to create a framework to enhance early detection. Computed tomography (CT), magnetic resonance imaging (MRI), and endoscopic ultrasound (EUS) have all emerged as essentials in the multidisciplinary diagnostic approach of PDAC. EUS images of the pancreas are distinct from all modalities above because of their increased spatial resolution, making it 94% sensitive for PDAC detection[3]. Successive generations of EUS imaging transducers and post-processing software have markedly improved the spatial resolution of conventional B-mode EUS images. When used alone, it boasts a superior diagnostic accuracy over multidetector CT and MRI, singularly for solid pancreatic lesions (SPLs), but a meager specificity when differentiating pancreatic cancer from other pathologies[3,4]. However, with the advent of image-enhancing technologies such as contrast-enhanced EUS (CE-EUS) and EUS-elastography (EUS-E), there is evidence to suggest that even smaller SPLs are now detectable with good sensitivity and specificity[5-7]. Although promising, these advances' overarching impact in the face of early pancreatic cancer detection and diagnosing benign pancreatic diseases is still largely underwhelming. Pancreatic cancer remains a leading cause of death in industrialized populations, and the new case burden is estimated to grow steadily for the next 20 years[8]. Thus far, we know that the diagnostic accuracy of EUS, when coupled with EUS-guided tissue sampling, holds good outcomes, but reproducing its performance with ease remains a global challenge. The learning curve to master and competently perform an EUS examination is steep[9,10]. In this context, the introduction of artificial intelligence (AI), alone or in combination with existing enhanced EUS imaging technologies, may contribute to filling the gaps in accurately and consistently diagnosing pancreatic diseases[11]. This commentary highlights existing enhanced EUS imaging technologies while paving the way for AI, postulating its possible role in this arena.
Elastography is an ultrasonographic tool to measure the stiffness of the desired study area. The desired study area for a suspicious pancreatic lesion is also known as a region of interest (ROI). Akin to the clinical aspect of palpating a mass by hand and describing its characteristics, elastography does this similarly, but instead for deeper structures[12]. The two types of elastography include strain elastography (SE) and sheer wave elastography (SWE). However, SWE is still unstable in its use to measure the elasticity of SPLs and will not be discussed further in this article[13].
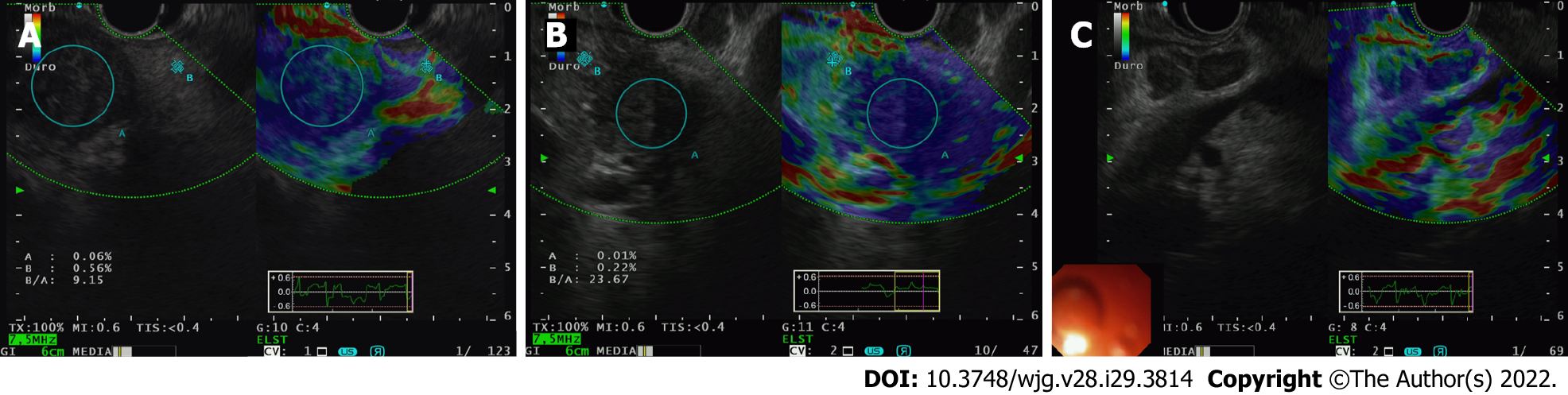
The type of elastography used in EUS is quasi-static or SE. It measures tissue displacement from a compressive force generated internally by the patient’s physiology like breathing and vascular pulsations or externally by the tip of the echoendoscope pressing against the GI wall[14]. The compressive force deforms the tissue momentarily. The amount the tissue deforms or the degree to which it gets displaced is known as strain. Softer or more elastic tissue, i.e. more benign, will have more displacement while stiffer, inelastic, and generally more malignant tissue, will have less strain[15]. The images can be seen side by side on the EUS display, with the EUS-E overlayed on the B mode image.
We present examples for PDAC (Figure 1A and B) and for a metastatic lymph node (Figure 1C). The color spectrum represents a qualitative measurement, blue being the hardest and red being the softest. Quantitative measurements are seen on the strain histogram or valued as the strain ratio (SR; the strain of the larger round-shaped ROI area A divided by the strain of smaller round-shaped region of surrounding normal tissue area B). Suggested surrounding normal homogenous tissue to be used as reference include either healthy surrounding pancreatic parenchyma (pSR) or healthy GI tract wall (wSR). Suggested elastography SR values are automatically computed and estimated using the built-in software found in the Olympus EU-ME2 processor and the Hitachi United States machines. However, the reference areas have yet to be standardized.
One of the earliest prospective multicenter studies by Giovannini[16] evaluated the elastography of pancreatic masses from 121 patients on initial EUS referenced against final histological diagnoses. Elastography successfully demonstrated “intense blue” on qualitative measurement for all PDAC, endocrine tumors, pancreatic metastasis, and pancreatic sarcomas. According to his scoring system of 1 through 5 (5 being the stiffest and most intense blue), scores 1 and 2 had a negative predictive value (NPV) of 77.4%, whilst scores 3 and 4 had a positive predictive value (PPV) for malignancy of 92.8%[16].
In the interest of detecting smaller ductal adenocarcinomas (< 15 mm), which if resected earlier, have shown a 5-year survival mark in PDAC survivors to exceed 30%-60%, Ignee et al[7] evaluated SRs for SPLs of < 15 mm from 218 patients across 13 international centers. They found that EUS-E patterns of a small lesion (average size 11 ± 3 mm), if found to be soft, could confidently rule out malignancy (NPV 98%). Although PDAC was diagnosed in these small lesions with a sensitivity of 96%, elevated stiffness in a detected lesion had a specificity of only 67% with a PPV of 56% when diagnosing malignancy[7]. These small lesions’ final etiological percentage breakdown was 66% benign, while 52% were neuroendocrine tumors (NETs). Notably, 36% of the NETs were stiff lesions, while 64% were soft compared to surrounding tissue. The remaining 23% were PDAC, 17% other entities, and 8% metastasis (which showed stiffness only 59% of the time)[7].
In 2012, Pei et al[17] and in 2013, Ying et al[18], the Asian groups conducted separate metanalyses, but with additions to pooled data on the subject matter of EUS-E’s diagnostic accuracy, a more recent meta-analysis of 17 studies analyzing 1544 lesions from 1537 patients was conducted in 2017. From their pooled results, EUS-E reported an accumulated sensitivity of 97% (95%CI: 95%-99%) and a sensitivity of 67% (95%CI: 59%-74%) for qualitative methods; 97% sensitivity (95%CI: 95%-98%) and 67% specificity (95%CI: 61%-73%) for Strain Histograms, and lastly, 98% specificity (95%CI: 96%-99%) and 62% sensitivity (95%CI: 56%-68%) for strain ratios, suggesting its value as a complement to EUS-guided tissue sampling, i.e. EUS-FNA[19].
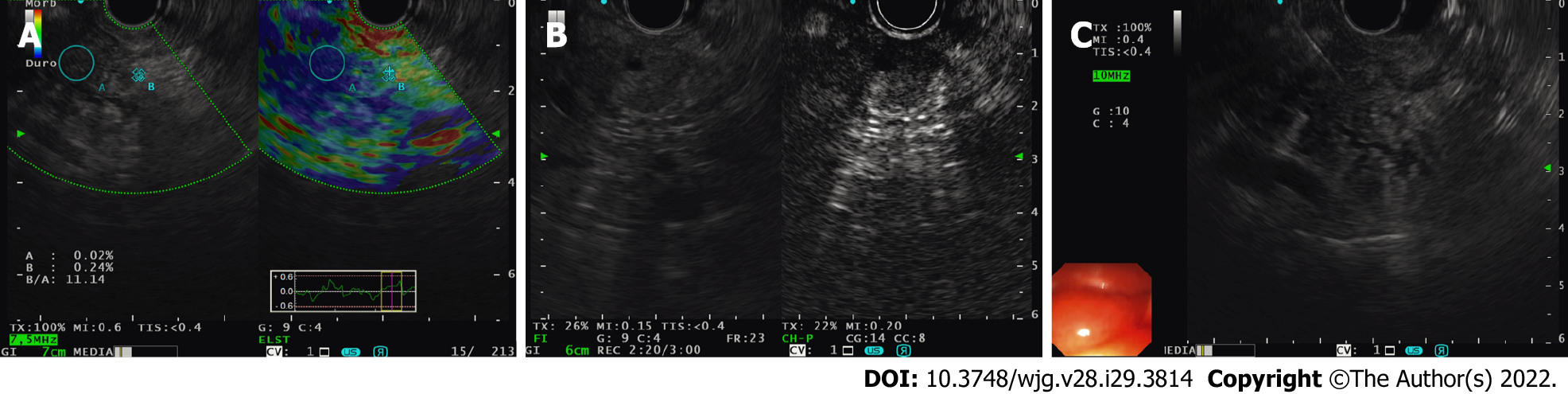
Similarly, guidelines proposed by the European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) advocate using elastography as a complementary tool for focal pancreatic lesion characterization[20]. When a EUS-FNA sample is negative, but the index of suspicion for malignancy remains, the EFSUMB recommends using elastography and CE-EUS for repeat tissue sampling or referring the patient directly to the surgeons for operative intervention without further delay[20]. We demonstrate the clinical application of EUS-E (with CE-EUS) to target FNB sampling in a patient with a degenerated intraductal papillary mucinous neoplasm (IPMN) under our surveillance (Figure 2). This patient had positive cytology, warranting early surgery. Although documented to be helpful in the diagnosis of early autoimmune pancreatitis due to an idiosyncratic distribution of tissue stiffness, the guidelines cannot recommend the use of elastography in differentiating advanced chronic pancreatitis from pancreatic cancer[20].
One of EUS-E’s many inherent limitations is evident here: Its low specificity and inability to consistently distinguish between pancreatic diseases (inflammatory vs neoplastic) or even types of pancreatic malignancies.
Inbuilt elastography software reduces intra-observer variability by overcoming the selection bias of images by providing the operator with a real-time movie of all recorded frames. However, there remains significant inter-observer variability when differentiating NETs from normal pancreatic parenchyma, as both may appear green i.e. soft.
Here are a few other scenarios where misdiagnoses occur: (1) If the endoscopist places too much compressive pressure between the probe and the examined tissue; and (2) False image reconstruction due to the heterogeneity of the examined tissue i.e. in the case of pancreatic cancer where some areas within the lesion are either necrotic, fibrous from desmoplasia, or have become inhomogeneous from vessel infiltration.
Other pitfalls include: (1) A lack of standardization for cut-off values for strain ratios, although some experts propose using parenchyma-to-lesion SR of > 9.10 (PPV 89.7%; NPV 76.9%) or the gastric wall-to-lesion SR of > 16.2 (PPV 86.5%; NPV 80%)[21]; (2) Border delineation once the lesion becomes larger[22]; (3) Inability to measure strain if the lesion is too far away from the probe, and lastly; and (4) Image acquisition when fluid is present, i.e. with cysts[22].
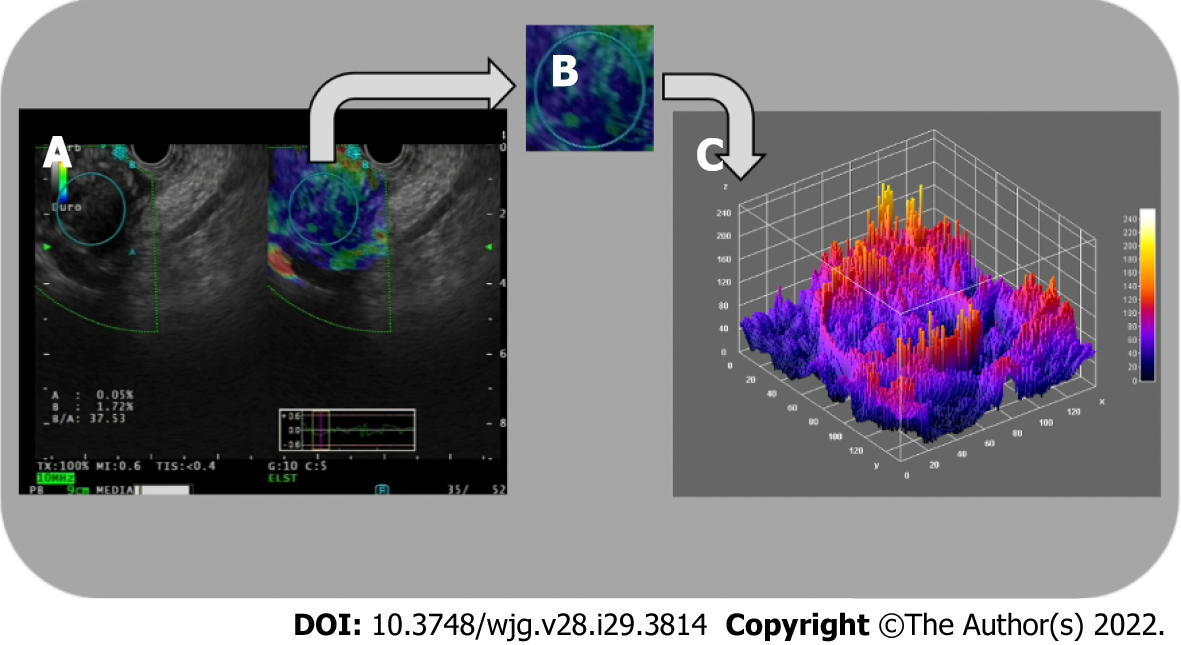
Carrara et al[21] demonstrated the use of fractal geometry analysis (Figure 3) to quantify the surface roughness of 2 tissues that share the same mechanical properties on elastography, and in doing so, overcome a significant limitation of EUS-E, but further trials are required[21]. Studies are also underway to evaluate the use of EUS-E in differentiating actual vessel wall infiltration by tumor tissue from that caused by an inflammatory reaction. The European Elastography Group, amongst others, is also designing and training deep learning platforms for future use in reducing inter-operator variability.
CE-EUS imaging is a non-invasive technique that utilizes a contrast agent during a EUS examination to improve diagnostic imaging. Contrast use in ultrasound imaging was first pioneered in 1986 by Matsuda and Yabuuchi with the infusion of CO2 as a medium. Kato heralded its subsequent application into EUS in 1991, confined only to angiographic examinations[23]. In the mid-1990s, the use of Doppler function and sonicated serum albumin expanded the application of CE-EUS beyond the premise of angiographic studies[24].
In CE-EUS, the mechanical index (MI) alludes to the reaction of microbubbles in response to a stimulus in the form of an acoustic wave[25]. From this response, CE-EUS is typed into two: (1) Contrast-enhanced high-MI EUS (CEHMI-EUS), not requiring specific interpretive software; and (2) Contrast-enhanced low-MI EUS (CELMI-EUS), requiring a contrast-specific software mode.
A significant advantage of CELMI-EUS over CEHMI-EUS is its higher resolution and visibility of the contrast enhancer bubbles. In contrast, CEHMI-EUS's ability to display pancreatic macro-vessels (vessels with a diameter of approximately 0.2 mm and higher) comes at the expense of microbubble destruction and, as a result, CEHMI-EUS's use for Doppler enhancement is preferred[26].
In collaboration with European experts in a recently issued guideline, the Asian Federation of Societies for Ultrasound in Medicine and Biology (AFSUMB) concluded that the MI should be between 0.2 and 0.4. They added that the 0.1 to 0.4 range used in published reports was influenced by several factors, including EUS probe type (radial or linear), image processing hardware, and software, phase-inversion harmonics, amplitude modulations, and focal points[27].
Tissue harmonic imaging (THI) is an ultrasonographic technique, first introduced in 1997, that utilizes nonlinear propagation of ultrasound (US) waves to generate images that are superior in quality to the fundamental B-mode imaging mode[28]. This tool was incorporated into the EUS imaging arsenal approximately a decade later[29].
The two image processing techniques developed to generate harmonic images were the band filtering method and phase inversion method. The ability of harmonic imaging to improve signal-to-noise ratio and reduce artifacts produced by side lobes, grating lobes, and reverberation allowed it to outperform earlier imaging applications, such as Color Doppler and power Doppler, which were susceptible to motion artifacts[30]. Furthermore, this modality allowed for visualization of parenchymal perfusion and microvasculature of the pancreas[31].
AFSUMB, in their summary recommendations, alluded to the benefit of contrast-enhanced harmonic EUS (CH-EUS) for characterization of solid pancreatic masses, pancreatic cancer staging in patients with suspected major vessel involvement, identification of mural nodules in cystic pancreatic lesions, and detection of subtle pancreatic lesions[27].
Nevertheless, THI is saddled with certain intrinsic technical limitations. The narrow bandwidth decreases axial resolution when applying the band filtering method. This limitation gave rise to the conception of the phase inversion method. However, the latter method necessitates the transmission of two US pulses, thus decreasing the frame rate and raising the possibility of motion artifacts[30].
The first reported use of intravenous ultrasound contrast agents (UCAs) in ultrasonography was for image enhancement during echocardiography. Its adoption followed this in transabdominal ultrasonography before it was eventually introduced in EUS[32]. EFSUMB’s recommendation on contrast for CE-EUS in non-liver applications highlighted its similarity to its use in transabdominal CEUS[33]. Worth noting is that the modalities, as mentioned earlier, represent the only imaging techniques that allow a dynamic observation of the CE phases[34]. UCAs are used to augment their ability in lesion characterization and intervention guidance.
During the evolutionary phase of CE-EUS, various agents were explored to advance the diagnostic performance of this modality. To render stability and durability, all commercially available agents are composed of gas-filled microbubbles encapsulated by a phospholipid or albumin shell. Each agent is aptly categorized based on its half-life and ability for transpulmonary passage[32].
The AFSUMB working group strongly recommends the following for use as UCAs: SonoVue (Lumason, sulfur hexafluoride micro-bubbles; Bracco, Milan, Italy; available in Europe, China, India, Korea, Hong Kong, New Zealand, Singapore, and Brazil); Definity (octafluoropropane microbubbles; Bristol- Myers Squibb Medical Imaging, New York, NY, United States; available in the United States, Canada, and Australia), and Sonazoid (perfluorobutane microbubbles; GE Healthcare, Chicago, IL, United States; Daiichi Sankyo, Tokyo, Japan; available in Japan, South Korea, Taiwan and Norway). They further stated that neither of the agents had a superior diagnostic ability over the other[27].
A significant emphasis has been placed on researching the adjunctive role of CE-EUS in evaluating solid pancreatic masses. The result is a wealth of data that supports its use in assessing the pancreas and related pathologies[33]. Mei et al[35] affirmed this in a recent meta-analysis (n = 1497) to evaluate the accuracy of CE-EUS in discriminating between benign and malignant pancreatic masses with a reported pooled sensitivity, specificity, and diagnostic odds ratio of 0.91, 0.86, and 69.50, respectively[35].
Another meta-analysis that included 1139 patients across 12 studies highlighted that both high and low MI techniques had a 94% sensitivity and 89% specificity in differentiating pancreatic adenocarcinoma from other pathologies, with an area under the receiver operating characteristic curve of 0.9732. Subgroup analysis by excluding the outliers provided a sensitivity and specificity of 93%[36].
Săftoiu et al[37] analyzed the diagnostic accuracy of combining CE-EUS and elastography to differentiate focal pancreatic masses and highlighted its influence in decision making when confronted with a negative EUS-FNB result with a strong clinical suspicion of malignancy. A similar study by the same authors assessed the "synergistic" performance of CE-EUS with EUS-EG in 50 patients with a negative FNA of pancreatic masses. The results determined 19 to be pancreatic adenocarcinoma and 31 to be pseudo-tumoral chronic pancreatitis. CE-EUS reported a specificity of 100% and an accuracy of 93% in the cohort of 25 patients where EUS-EG demonstrated high lesion stiffness, diagnosing malignancy[38].
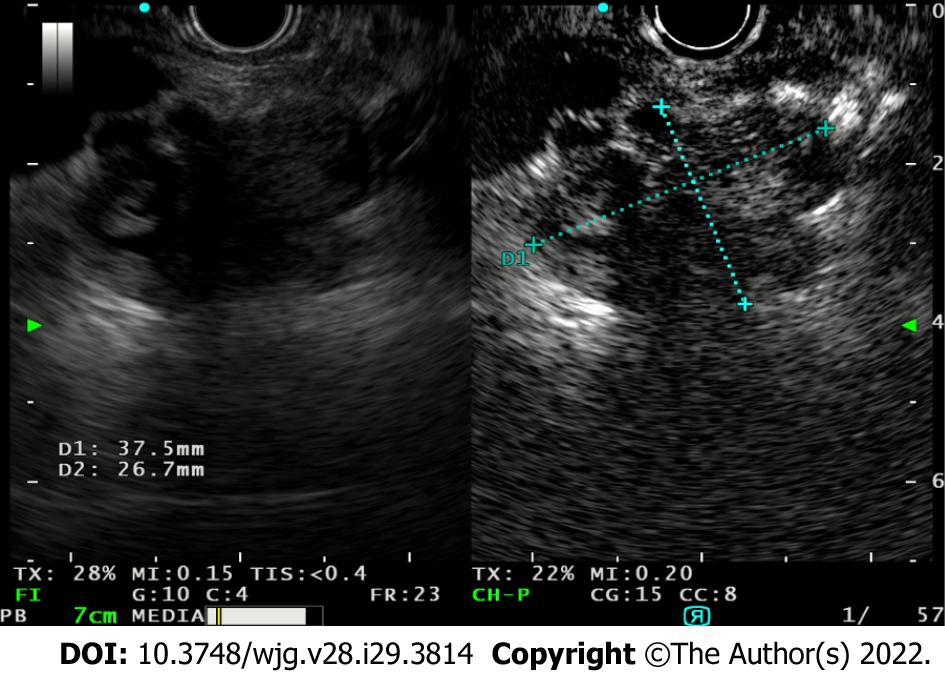
Buxbaum et al[39], in a prospective tandem-controlled trial involving 101 cases of focal pancreatic lesions, concluded that CE-EUS increased the diagnostic yield compared to conventional B-mode EUS with an odds ratio of 7.8 (95%CI: 2.7-30.2). Ninety-one percent of lesions were correctly characterized in the validation cohort, with an improved yield compared to unenhanced EUS[39]. In a real-life clinical setting, we demonstrate its use in a case of a degenerated IPMN showing how its use allows differentiation of tumor vegetation from mucus within a cyst (Figure 4).
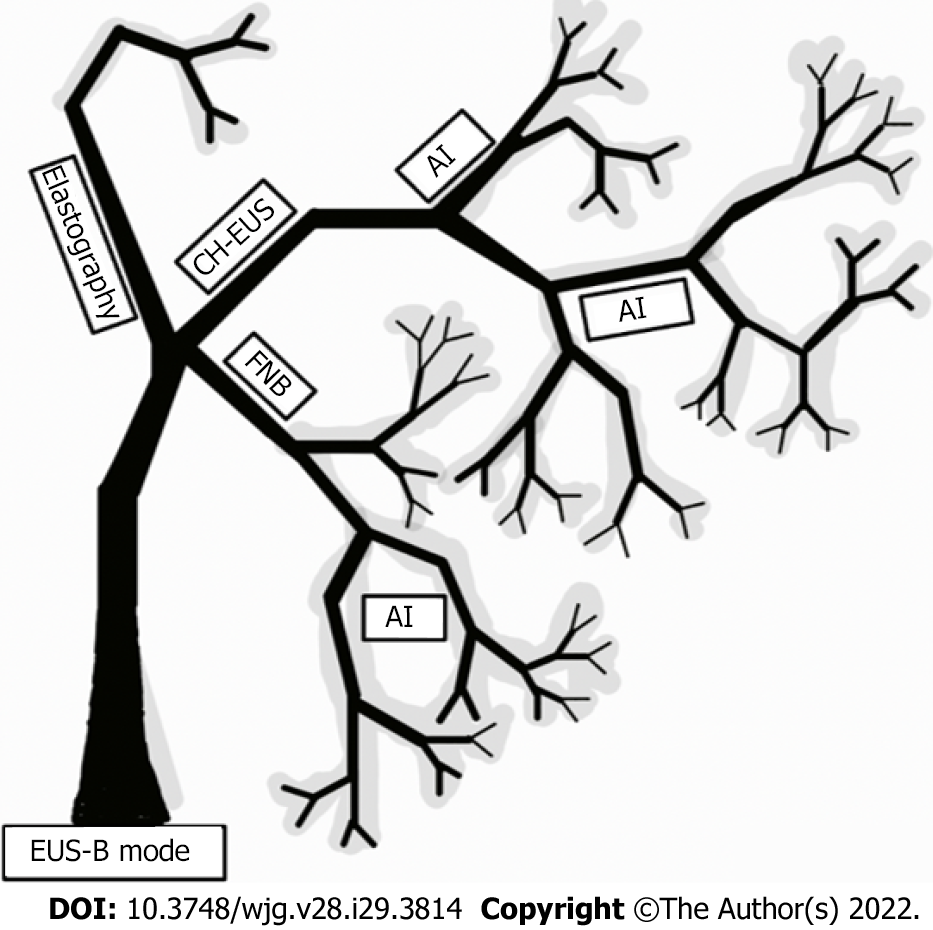
AI can level the playing field for endoscopists globally by making this highly sensitive and specific, but technically challenging, diagnostic tool we know as EUS more user-friendly and quicker to master.
The existing image enhancing techniques, CH-EUS and EUS-E, are available to the endoscopist currently as stand-alone software plug-ins. They require prior training before use with a low to moderate learning curve to master given that the user is already proficient with an echoendoscope.
The potential of AI is seen here in its ability to harness the diagnostic power of EUS while unifying all existing and future image-enhancing techniques “under one roof.” This unifying software can aid the endoscopist by highlighting areas of concern while prompting suitable image-enhancing methods.
This added edge of diagnostic confidence can help overcome lesion ambiguity and improve lesion specificity, regardless of the years of prior endosonographic training.
AI is a divaricate under the broader umbrella of computing methodology and information sciences. It utilizes autonomous properties from rapidly advancing technological developments in deep learning as a segue to mimic human behavior ultimately. Over the last decade, AI applications have quickly matured. Their iterations in the daily practice of various fields within medicine are expanding with success.
The development and training of computer-aided diagnosis (CAD) systems revolve around the aim of autonomously distinguishing features that the human eye and mind may unintentionally miss. Identifying and interpreting changes of varying subtleties, particularly in medical images, has been the high point of AI. The objectivity of a trained CAD system could potentially seek to overcome one of the most significant limitations of any physician or endoscopist: The lack of an intra- and inter-observer agreement. Suppose an AI system can distinguish between neoplastic and non-neoplastic lesions with near perfection after training, it would seem reasonable to imagine that the burden from pathological examinations may be considerably relieved very soon. Thus far, colonic adenoma detection and differentiation have gained tremendous attention from several CAD systems utilizing deep learning and Artificial Neural networks. Due to their promising results, these systems have gained popularity in day-to-day endoscopy usage[40-43].
The most common application of AI in EUS is creating machine learning architectures that extract EUS images and analyze them for their textures (boasting accuracy of up to 93%-94%) to create an artificial neural network that can ultimately serve as a clinical decision support tool. It can do one of 2 things: (1) Using the station approach to familiarize the endoscopist with normal anatomy, as demonstrated by Kanno et al[44]; and (2) Non-invasively differentiating pancreatic parenchymal pathologies when EUS-FNB may not be clinically feasible or have a poor diagnostic yield in the case of cysts or AIP[40].
In 2008, two studies emerged providing the diagnostic ability of AI integrated EUS in reporting pancreatic diseases. Săftoiu et al[45] reported 68 cases in a prospective study using a neural network EUS to compare PDAC and chronic pancreatitis. The authors reported 95% accuracy in the system’s diagnostic ability. In the second study, Das et al[46] reviewed 319 images with a neural network system and performed a principal component analysis to compare acute and chronic pancreatitis, from pancreatic carcinoma. The study reported the area under the curve indicating the systems’ diagnostic ability to be 93%. In 2013, Zhu et al[47] studied 288 cases retrospectively with a support vector machine and reached an accuracy of 94%.
Additionally, Săftoiu et al[48], in a prospective multicenter study, reported 167 cases using a neural network system, reaching a diagnostic accuracy of 94%. Ozkan et al[49] reported an accuracy of 93% in reviewing 332 images in retrospect using a neural network. A deep learning architecture specific to EUS noteworthy of mentioning is one used to differentiate high-grade dysplasia vs malignancy for IPMN with an accuracy of 94%[42]. In a single-center retrospective study that trained a deep learning algorithm using 3970 still images, deep learning was superior to human ability in its diagnostic accuracy (95% vs 56%), proving an objective method such as is this is more accurate in diagnosing malignancies of IPMN origin in comparison to conventional EUS features[42].
AI demonstrates its usefulness again in increasing diagnostic specificity using occlusion heatmap analysis to differentiate AIP from PDAC. The result is overcoming a delay in diagnosis, initiating immunosuppressive or chemoradiotherapy early, and preventing unwarranted resections (90% sensitive, 85% specific)[50]. It is worth mentioning that these studies use a cross-validation method with an internal control check, thus inflating the actuality of the diagnostic accuracy. In its applications to actual EUS fine-needle biopsy histopathological samples, AI was able to bring diagnostic clarity to difficult-to-analyze samples with an accuracy of 94.1% despite cellular paucity and contamination.
In centers with a lack of dedicated GI pathologists, AI software can quickly close this gap of diagnostic delay and eliminate repeat sampling at second or third centers[11]. One setback of AI is the black-box phenomenon, which can cause judgment errors without an explanatory basis. That said, a trained convolutional neural network model with extracted visual features from various pancreatic diseases, namely chronic pseudo-tumoral pancreatitis, NET, and PDAC, can accurately produce a real-time diagnosis[51].
For a suspected pancreatic mass, we propose utilizing both EUS-E and CE-EUS to augment conventional B-mode imaging (Figure 5).
Their advantages in defining nodules and ambiguous ROIs allow FNA/FNB sampling precision, making them crucial adjuncts in day-to-day practice, whether for first encounters or follow-up visits.
Validation studies are still underway to evaluate promising non-contrast-based high-definition imaging modalities. The modalities are in-built into the echo processor for ease of microvasculature study. They carry great potential in supplementing and possibly surrogating UCAs in conditions, such as pregnancy or compromised cardiopulmonary status[52]. However, until then, EUS-E and CE-EUS coupled with B-mode imaging will remain the choice stratagem in improving the early detection of pancreatic cancer.
In the EUS world of greys, colors emerged from elastography and patterns from contrast use, improving the overall accuracy of pancreatic mass differentiation. AI could be the rainbow that bridges us to a more precise diagnosis.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Pausawasdi N, Thailand; Tsoulfas G, Greece S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR
| 1. | McGuigan A, Kelly P, Turkington RC, Jones C, Coleman HG, McCain RS. Pancreatic cancer: A review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol. 2018;24:4846-4861. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1338] [Cited by in RCA: 1261] [Article Influence: 180.1] [Reference Citation Analysis (39)] |
| 2. | Egawa S, Toma H, Ohigashi H, Okusaka T, Nakao A, Hatori T, Maguchi H, Yanagisawa A, Tanaka M. Japan Pancreatic Cancer Registry; 30th year anniversary: Japan Pancreas Society. Pancreas. 2012;41:985-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 306] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 3. | Kitano M, Yoshida T, Itonaga M, Tamura T, Hatamaru K, Yamashita Y. Impact of endoscopic ultrasonography on diagnosis of pancreatic cancer. J Gastroenterol. 2019;54:19-32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 170] [Cited by in RCA: 216] [Article Influence: 36.0] [Reference Citation Analysis (0)] |
| 4. | Müller MF, Meyenberger C, Bertschinger P, Schaer R, Marincek B. Pancreatic tumors: evaluation with endoscopic US, CT, and MR imaging. Radiology. 1994;190:745-751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 357] [Cited by in RCA: 304] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 5. | Dietrich CF, Ignee A, Frey H. Contrast-enhanced endoscopic ultrasound with low mechanical index: a new technique. Z Gastroenterol. 2005;43:1219-1223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 73] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 6. | Dietrich CF, Sahai AV, D'Onofrio M, Will U, Arcidiacono PG, Petrone MC, Hocke M, Braden B, Burmester E, Möller K, Săftoiu A, Ignee A, Cui XW, Iordache S, Potthoff A, Iglesias-Garcia J, Fusaroli P, Dong Y, Jenssen C. Differential diagnosis of small solid pancreatic lesions. Gastrointest Endosc. 2016;84:933-940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 80] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 7. | Ignee A, Jenssen C, Arcidiacono PG, Hocke M, Möller K, Saftoiu A, Will U, Fusaroli P, Iglesias-Garcia J, Ponnudurai R, Petrone MC, Braden B, Burmester E, Dong Y, Atkinson NS, Dietrich CF. Endoscopic ultrasound elastography of small solid pancreatic lesions: a multicenter study. Endoscopy. 2018;50:1071-1079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 59] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 8. | Rawla P, Sunkara T, Gaduputi V. Epidemiology of Pancreatic Cancer: Global Trends, Etiology and Risk Factors. World J Oncol. 2019;10:10-27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 893] [Cited by in RCA: 1518] [Article Influence: 253.0] [Reference Citation Analysis (1)] |
| 9. | Elfanagely Y, Tse CS, Rich H, Hyder SM. Learning curves for EUS: single operators, endoscopy teams, and institutions. Gastrointest Endosc. 2021;93:989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Gonzalez JM, Cohen J, Gromski MA, Saito K, Loundou A, Matthes K. Learning curve for endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) of pancreatic lesions in a novel ex-vivo simulation model. Endosc Int Open. 2016;4:E1286-E1291. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Tonozuka R, Mukai S, Itoi T. The Role of Artificial Intelligence in Endoscopic Ultrasound for Pancreatic Disorders. Diagnostics (Basel). 2020;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 12. | Faruk T, Islam MK, Arefin S, Haq MZ. The Journey of Elastography: Background, Current Status, and Future Possibilities in Breast Cancer Diagnosis. Clin Breast Cancer. 2015;15:313-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 13. | Ohno E, Kawashima H, Ishikawa T, Iida T, Suzuki H, Uetsuki K, Yashika J, Yamada K, Yoshikawa M, Gibo N, Aoki T, Kataoka K, Mori H, Yamamura T, Furukawa K, Nakamura M, Hirooka Y, Fujishiro M. Diagnostic performance of endoscopic ultrasonography-guided elastography for solid pancreatic lesions: Shear-wave measurements vs strain elastography with histogram analysis. Dig Endosc. 2021;33:629-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 14. | Sigrist RMS, Liau J, Kaffas AE, Chammas MC, Willmann JK. Ultrasound Elastography: Review of Techniques and Clinical Applications. Theranostics. 2017;7:1303-1329. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 954] [Cited by in RCA: 1093] [Article Influence: 136.6] [Reference Citation Analysis (0)] |
| 15. | Giovannini M. Endoscopic ultrasound elastography. Pancreatology. 2011;11 Suppl 2:34-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Giovannini M. Contrast-enhanced endoscopic ultrasound and elastosonoendoscopy. Best Pract Res Clin Gastroenterol. 2009;23:767-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Pei Q, Zou X, Zhang X, Chen M, Guo Y, Luo H. Diagnostic value of EUS elastography in differentiation of benign and malignant solid pancreatic masses: a meta-analysis. Pancreatology. 2012;12:402-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 18. | Ying L, Lin X, Xie ZL, Hu YP, Tang KF, Shi KQ. Clinical utility of endoscopic ultrasound elastography for identification of malignant pancreatic masses: a meta-analysis. J Gastroenterol Hepatol. 2013;28:1434-1443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 81] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 19. | Lu Y, Chen L, Li C, Chen H, Chen J. Diagnostic utility of endoscopic ultrasonography-elastography in the evaluation of solid pancreatic masses: a meta-analysis and systematic review. Med Ultrason. 2017;19:150-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (1)] |
| 20. | Cosgrove D, Piscaglia F, Bamber J, Bojunga J, Correas JM, Gilja OH, Klauser AS, Sporea I, Calliada F, Cantisani V, D'Onofrio M, Drakonaki EE, Fink M, Friedrich-Rust M, Fromageau J, Havre RF, Jenssen C, Ohlinger R, Săftoiu A, Schaefer F, Dietrich CF; EFSUMB. EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 2: Clinical applications. Ultraschall Med. 2013;34:238-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 681] [Cited by in RCA: 623] [Article Influence: 51.9] [Reference Citation Analysis (0)] |
| 21. | Carrara S, Di Leo M, Grizzi F, Correale L, Rahal D, Anderloni A, Auriemma F, Fugazza A, Preatoni P, Maselli R, Hassan C, Finati E, Mangiavillano B, Repici A. EUS elastography (strain ratio) and fractal-based quantitative analysis for the diagnosis of solid pancreatic lesions. Gastrointest Endosc. 2018;87:1464-1473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 22. | Hirche TO, Ignee A, Barreiros AP, Schreiber-Dietrich D, Jungblut S, Ott M, Hirche H, Dietrich CF. Indications and limitations of endoscopic ultrasound elastography for evaluation of focal pancreatic lesions. Endoscopy. 2008;40:910-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 100] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 23. | Kato T, Tsukamoto Y, Naitoh Y, Hirooka Y, Furukawa T, Hayakawa T. Ultrasonographic and endoscopic ultrasonographic angiography in pancreatic mass lesions. Acta Radiol. 1995;36:381-387. [PubMed] |
| 24. | Hirooka Y, Naitoh Y, Goto H, Ito A, Taki T, Hayakawa T. Usefulness of contrast-enhanced endoscopic ultrasonography with intravenous injection of sonicated serum albumin. Gastrointest Endosc. 1997;46:166-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Mohamed RM, Yan BM. Contrast enhanced endoscopic ultrasound: More than just a fancy Doppler. World J Gastrointest Endosc. 2010;2:237-243. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Hocke M, Dietrich CF. Advanced EUS Imaging for Pancreatic Diseases: CE-EUS (Low-MI, High-MI) and Real-Time Elastography, 3D. Video J Encyc GI Endos. 2013;1:537-539. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 27. | Kitano M, Yamashita Y, Kamata K, Ang TL, Imazu H, Ohno E, Hirooka Y, Fusaroli P, Seo DW, Napoléon B, Teoh AYB, Kim TH, Dietrich CF, Wang HP, Kudo M; Working group for the International Consensus Guidelines for Contrast-Enhanced Harmonic Endoscopic Ultrasound. The Asian Federation of Societies for Ultrasound in Medicine and Biology (AFSUMB) Guidelines for Contrast-Enhanced Endoscopic Ultrasound. Ultrasound Med Biol. 2021;47:1433-1447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 28. | Anvari A, Forsberg F, Samir AE. A Primer on the Physical Principles of Tissue Harmonic Imaging. Radiographics. 2015;35:1955-1964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 29. | Alvarez-Sánchez MV, Napoléon B. Contrast-enhanced harmonic endoscopic ultrasound imaging: basic principles, present situation and future perspectives. World J Gastroenterol. 2014;20:15549-15563. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 30] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 30. | Ohno E, Kawashima H, Hashimoto S, Goto H, Hirooka Y. Current status of tissue harmonic imaging in endoscopic ultrasonography (EUS) and EUS-elastography in pancreatobiliary diseases. Dig Endosc. 2015;27 Suppl 1:68-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 31. | Kitano M, Sakamoto H, Matsui U, Ito Y, Maekawa K, von Schrenck T, Kudo M. A novel perfusion imaging technique of the pancreas: contrast-enhanced harmonic EUS (with video). Gastrointest Endosc. 2008;67:141-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 140] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 32. | Reddy NK, Ioncică AM, Săftoiu A, Vilmann P, Bhutani MS. Contrast-enhanced endoscopic ultrasonography. World J Gastroenterol. 2011;17:42-48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 47] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 33. | Saftoiu A, Vilmann P, Bhutani MS. The role of contrast-enhanced endoscopic ultrasound in pancreatic adenocarcinoma. Endosc Ultrasound. 2016;5:368-372. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 34. | D'Onofrio M, Biagioli E, Gerardi C, Canestrini S, Rulli E, Crosara S, De Robertis R, Floriani I. Diagnostic performance of contrast-enhanced ultrasound (CEUS) and contrast-enhanced endoscopic ultrasound (ECEUS) for the differentiation of pancreatic lesions: a systematic review and meta-analysis. Ultraschall Med. 2014;35:515-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 35. | Mei S, Wang M, Sun L. Contrast-Enhanced EUS for Differential Diagnosis of Pancreatic Masses: A Meta-Analysis. Gastroenterol Res Pract. 2019;2019:1670183. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 36. | Gong TT, Hu DM, Zhu Q. Contrast-enhanced EUS for differential diagnosis of pancreatic mass lesions: a meta-analysis. Gastrointest Endosc. 2012;76:301-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 99] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 37. | Săftoiu A, Iordache SA, Gheonea DI, Popescu C, Maloş A, Gorunescu F, Ciurea T, Iordache A, Popescu GL, Manea CT. Combined contrast-enhanced power Doppler and real-time sonoelastography performed during EUS, used in the differential diagnosis of focal pancreatic masses (with videos). Gastrointest Endosc. 2010;72:739-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 75] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 38. | Iordache S, Costache MI, Popescu CF, Streba CT, Cazacu S, Săftoiu A. Clinical impact of EUS elastography followed by contrast-enhanced EUS in patients with focal pancreatic masses and negative EUS-guided FNA. Med Ultrason. 2016;18:18-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 39. | Buxbaum J, Ko C, Varghese N, Lee A, Sahakian A, King K, Serna J, Lee H, Tchelepi H, Van Dam J, Duddalwar V. Qualitative and Quantitative Contrast-enhanced Endoscopic Ultrasound Improves Evaluation of Focal Pancreatic Lesions. Clin Gastroenterol Hepatol. 2020;18:917-925.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 40. | Kuwahara T, Hara K, Mizuno N, Haba S, Okuno N, Koda H, Miyano A, Fumihara D. Current status of artificial intelligence analysis for endoscopic ultrasonography. Dig Endosc. 2021;33:298-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 41. | Murakami D, Yamato M, Arai M, Nishino T. Artificial intelligence in colonoscopy. Lancet Gastroenterol Hepatol. 2021;6:984-985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 42. | Marya NB, Powers PD, Chari ST, Gleeson FC, Leggett CL, Abu Dayyeh BK, Chandrasekhara V, Iyer PG, Majumder S, Pearson RK, Petersen BT, Rajan E, Sawas T, Storm AC, Vege SS, Chen S, Long Z, Hough DM, Mara K, Levy MJ. Utilisation of artificial intelligence for the development of an EUS-convolutional neural network model trained to enhance the diagnosis of autoimmune pancreatitis. Gut. 2021;70:1335-1344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 86] [Article Influence: 21.5] [Reference Citation Analysis (1)] |
| 43. | Zhang J, Zhu L, Yao L, Ding X, Chen D, Wu H, Lu Z, Zhou W, Zhang L, An P, Xu B, Tan W, Hu S, Cheng F, Yu H. Deep learning-based pancreas segmentation and station recognition system in EUS: development and validation of a useful training tool (with video). Gastrointest Endosc. 2020;92:874-885.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 69] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 44. | Kanno A, Masamune A, Fujishima F, Iwashita T, Kodama Y, Katanuma A, Ohara H, Kitano M, Inoue H, Itoi T, Mizuno N, Miyakawa H, Mikata R, Irisawa A, Sato S, Notohara K, Shimosegawa T. Diagnosis of autoimmune pancreatitis by EUS-guided FNA using a 22-gauge needle: a prospective multicenter study. Gastrointest Endosc. 2016;84:797-804.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 91] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 45. | Săftoiu A, Vilmann P, Gorunescu F, Gheonea DI, Gorunescu M, Ciurea T, Popescu GL, Iordache A, Hassan H, Iordache S. Neural network analysis of dynamic sequences of EUS elastography used for the differential diagnosis of chronic pancreatitis and pancreatic cancer. Gastrointest Endosc. 2008;68:1086-1094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 173] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 46. | Das A, Nguyen CC, Li F, Li B. Digital image analysis of EUS images accurately differentiates pancreatic cancer from chronic pancreatitis and normal tissue. Gastrointest Endosc. 2008;67:861-867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 81] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 47. | Zhu M, Xu C, Yu J, Wu Y, Li C, Zhang M, Jin Z, Li Z. Differentiation of pancreatic cancer and chronic pancreatitis using computer-aided diagnosis of endoscopic ultrasound (EUS) images: a diagnostic test. PLoS One. 2013;8:e63820. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 73] [Article Influence: 6.1] [Reference Citation Analysis (2)] |
| 48. | Săftoiu A, Vilmann P, Dietrich CF, Iglesias-Garcia J, Hocke M, Seicean A, Ignee A, Hassan H, Streba CT, Ioncică AM, Gheonea DI, Ciurea T. Quantitative contrast-enhanced harmonic EUS in differential diagnosis of focal pancreatic masses (with videos). Gastrointest Endosc. 2015;82:59-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 112] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 49. | Ozkan M, Cakiroglu M, Kocaman O, Kurt M, Yilmaz B, Can G, Korkmaz U, Dandil E, Eksi Z. Age-based computer-aided diagnosis approach for pancreatic cancer on endoscopic ultrasound images. Endosc Ultrasound. 2016;5:101-107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 66] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 50. | Naito Y, Tsuneki M, Fukushima N, Koga Y, Higashi M, Notohara K, Aishima S, Ohike N, Tajiri T, Yamaguchi H, Fukumura Y, Kojima M, Hirabayashi K, Hamada Y, Norose T, Kai K, Omori Y, Sukeda A, Noguchi H, Uchino K, Itakura J, Okabe Y, Yamada Y, Akiba J, Kanavati F, Oda Y, Furukawa T, Yano H. A deep learning model to detect pancreatic ductal adenocarcinoma on endoscopic ultrasound-guided fine-needle biopsy. Sci Rep. 2021;11:8454. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 44] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 51. | Udriștoiu AL, Cazacu IM, Gruionu LG, Gruionu G, Iacob AV, Burtea DE, Ungureanu BS, Costache MI, Constantin A, Popescu CF, Udriștoiu Ș, Săftoiu A. Real-time computer-aided diagnosis of focal pancreatic masses from endoscopic ultrasound imaging based on a hybrid convolutional and long short-term memory neural network model. PLoS One. 2021;16:e0251701. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 52. | Hwang JS, Seo DW, So H, Ko SW, Joo HD, Oh D, Song TJ, Park DH, Lee SS, Lee SK, Kim MH. Clinical utility of directional eFLOW compared with contrast-enhanced harmonic endoscopic ultrasound for assessing the vascularity of pancreatic and peripancreatic masses. Pancreatology. 2022;22:130-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |