Published online Mar 28, 2022. doi: 10.3748/wjg.v28.i12.1284
Peer-review started: September 2, 2021
First decision: September 29, 2021
Revised: March 28, 2022
Accepted: February 23, 2022
Article in press: February 23, 2022
Published online: March 28, 2022
Processing time: 203 Days and 20.9 Hours
Near infrared fluorescence using indocyanine green is beneficial for visual assessment of blood vessels, blood flow, and tissue perfusion, sentinel lymph node biopsy, lymph node road mapping, identification of the vascular system round the major vessels, and the detection of ureters in order to reduce the risk of iatrogenic ureteral lesions in colorectal surgery.
Core Tip: Near infrared fluorescence technique using indocyanine green can be used in estimation of intestinal vascularization to detect areas of poor perfusion for preventing anastomotic leakage, the visualization of sentinel lymphatic drainage and peritoneal metastases, and the detection of ureters in order to reduce the risk of iatrogenic ureteral lesions in colorectal surgery. Additionally, this technique can be used in identifying suspected lymph nodes and preventing their incomplete dissection during lateral pelvic lymph node dissection and D3 Lymphadenectomy for rectal cancer and right-sided colon cancer, respectively, and in identification of the vascular system round the major vessels.
- Citation: Bae SU. Near-infrared fluorescence imaging guided surgery in colorectal surgery. World J Gastroenterol 2022; 28(12): 1284-1287
- URL: https://www.wjgnet.com/1007-9327/full/v28/i12/1284.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i12.1284
Indocyanine green (ICG) emits an infrared signal when excited by laser light in situ, which can be detected with near infrared fluorescence (NIF) camera. NIF imaging uses laser technology to activate an intravenously delivered agent, ICG, which rapidly binds to plasma proteins. This allows ICG to remain predominantly in visual assessment of blood vessels, blood flow, and tissue perfusion, sentinel lymph node biopsy and lymph node road mapping[1,2].
In this issue of World Journal of World Journal of Gastroenterology, the review article by Zocola et al[3] highlights the role of NIF in colorectal surgery. They reviewed the literature regarding NIF for three main indications including the estimation of intestinal vascularization to detect areas of poor perfusion for preventing anastomotic leakage, the visualization of sentinel lymphatic drainage and peritoneal metastases, and the detection of ureters in order to reduce the risk of iatrogenic ureteral lesions in colorectal surgery.
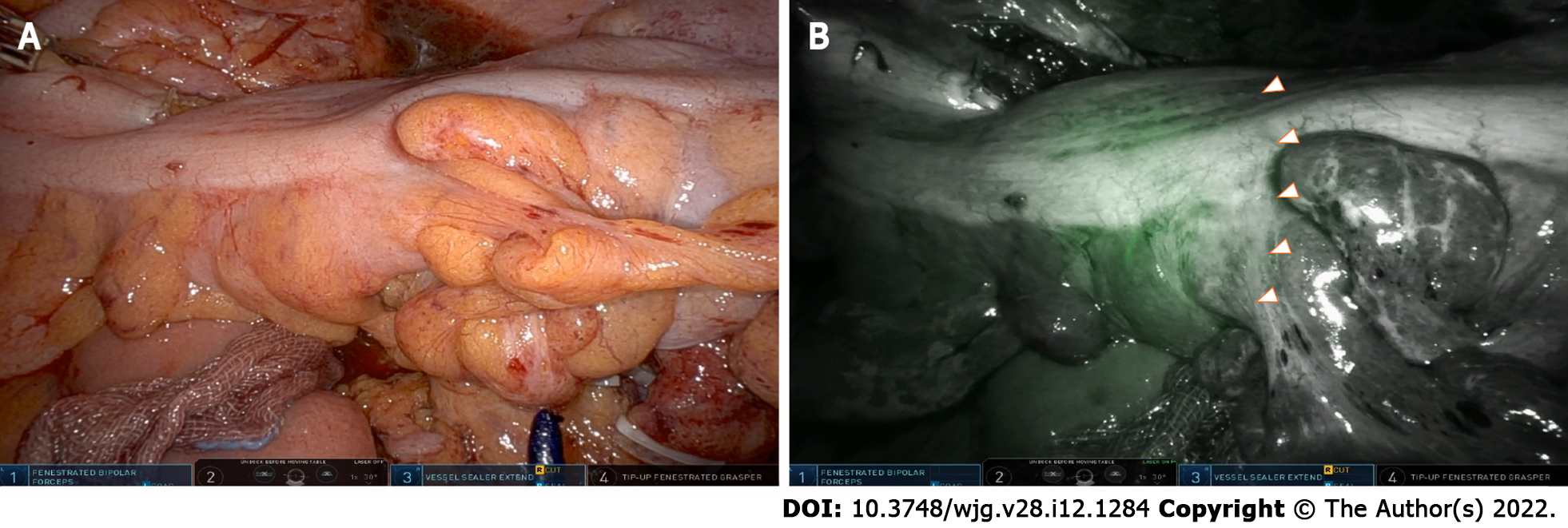
NIF in conjunction with ICG allows for visualization of the microcirculation before formation of the anastomosis, thereby allowing the surgeon to choose the point of transaction at an optimally perfused area (Figure 1). Zocola et al[3] intensively reviewed the role of NIF in the intraoperative bowel viability assessment to prevent anastomotic leaks. They divided the retrospective cohort study and prospective randomized controlled study and reviewed the effectiveness of NIF in reducing anastomotic leakage.
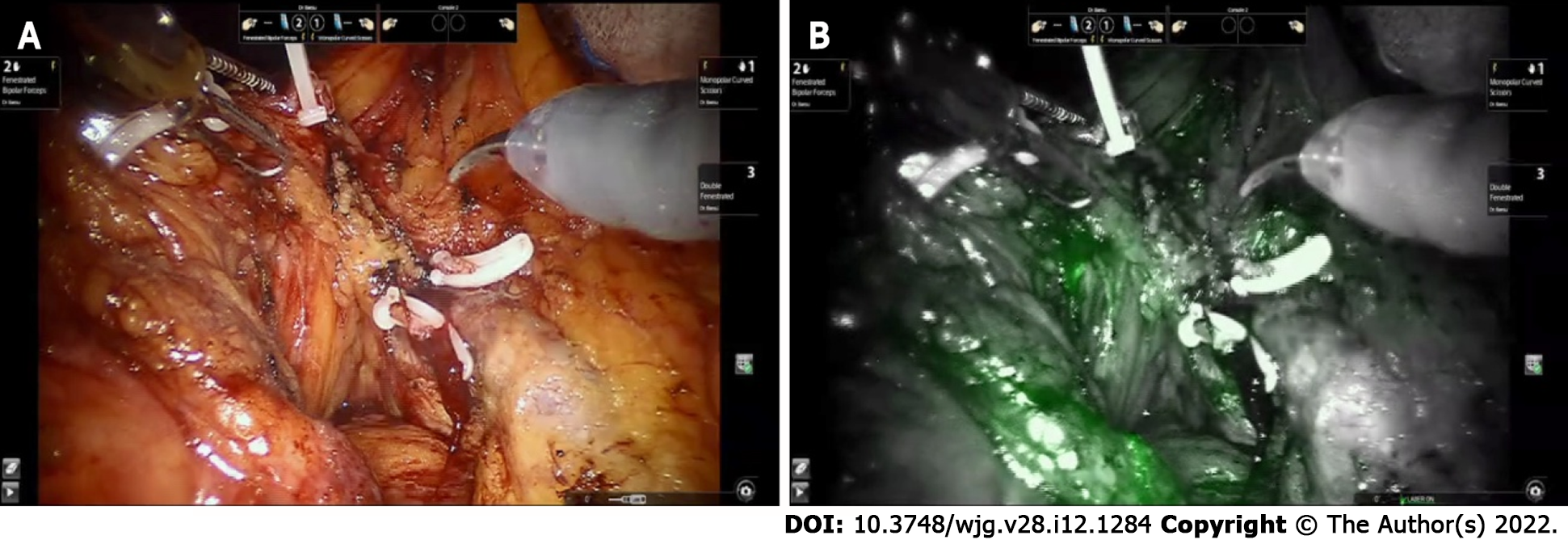
Regarding the role of NIF with ICG to detect metastatic lymph node, Zocola et al[3] reviewed studies on the identification of sentinel lymph node and mapping additional lymph nodes outside of the proposed resection margins to achieve radical lymphadenectomy for curative surgery (Figure 2). In addition to the studies mentioned by Zocola et al[3], I would like to mention some recent studies related to this issue. One of the issues related to radical lymphadenectomy in colorectal cancer is lateral pelvic node dissection (LPND), and recent introductions and data on this procedure using NIF have been reported. Kim et al[4] demonstrated a novel application of NIF using ICG during robotic total mesorectal excision (TME) with LPND to identify suspected lateral pelvic lymph nodes and prevent their incomplete dissection. They injected ICG at a dose of 2.5 mg around the tumor transanally before surgery and NIF imaging–guided robotic TME with lateral pelvic lymphadenectomy allowed the surgeon to identify lymph nodes and lymphatic flow of rectal cance. Zhou et al[5] compared patients who underwent TME and LPND with NIF technique (n = 12) and patients who received conventional TME and LPND without NIF-guided imaging (n = 30). They reported that the NIF group had significantly lower intraoperative blood loss (55.8 ± 37.5 mL vs 108.0 ± 52.7 mL, P = 0.003) and a significantly larger number of lateral pelvic nodes harvested (11.5 ± 5.9 vs 7.1 ± 4.8, P = 0.017), and lateral pelvic lymph nodes from two patients in the NIF group remained during LPND. Additionally, Park et al[6] and Bae et al[7] used NIF technique for colorectal cancer surgery is D3 Lymphadenectomy, especially in right-sided colon cancer. Park et al[6] injected ICG around the tumor for visualization of lymphatic flow and lymph nodes and demonstrated the numbers of apical lymph nodes (14 vs 7, P < 0.001) and total harvested lymph nodes (39 vs 30, P = 0.003) were significantly higher in the NIF group than in the conventional group.
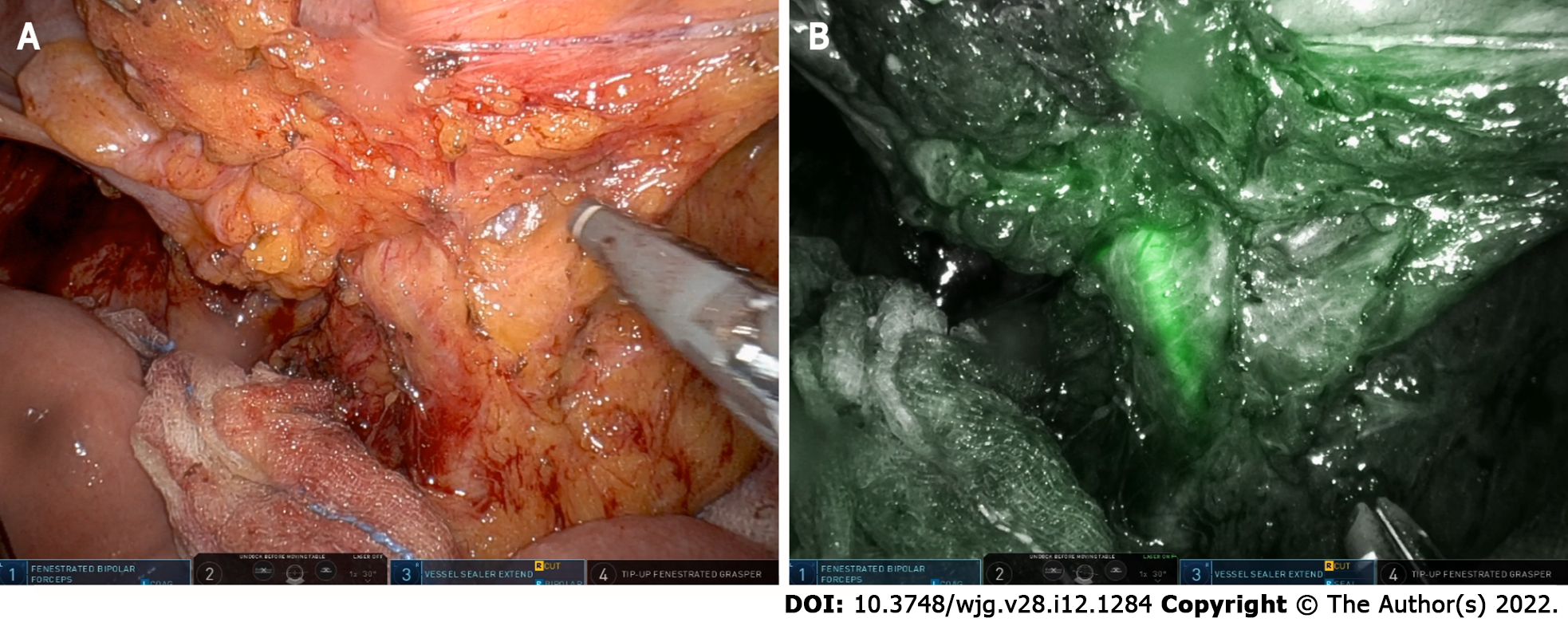
When injected intravenously, ICG rapidly binds to plasma proteins and remains predominantly in the vasculature. Although there was no mention in the review article, NIF angiography can be used in identification of the vascular system (Figure 3). ICG can be easily injected into the blood circulation during surgery, when the blood vessels are exposed, to allow direct visual observation. Bae et al[8,9] included 11 patients who underwent a robotic TME with preservation of the left colic artery for rectal cancer using NIF technique. The optimal point of division was then chosen by the surgeon under NIF imaging that facilitated the identification of the left colic branch of the inferior mesenteric artery (IMA). In addition, NIF imaging was used for the identification of the collateral vessels (Arc of Riolan) around the inferior mesenteric vein in their study. The left colic artery branches mainly at the Griffith point (watershed), which is located in the splenic bend where the left branch of the middle colic and the ascending branch of the left colic join. This area is vulnerable to injury and ischemia during surgery due to poor blood supply. For this reason, great care must be taken not to interfere with the bifurcation of the left colic artery. Real-time identification of collateral vessels using NIF technology can help implement safe low ligation of the IMA while preventing damage to these vessels. For now, it remains a linear graded outcome that requires subjective interpretation of the demarcation point between sufficient and insufficient perfusion and perfusion is assessed is based on a subjective qualitative impression of the surgeon. Quantitative analysis of NIF images is desirable but not currently available in robotic or laparoscopic systems. Son et al[10] performed quantitative evaluation of colon perfusion patterns using NIF angiography to find the most reliable predictive factor of anastomotic complications after laparoscopic colorectal surgery. They found that the fluorescence slope, T1/2MAX, and time ratio were related with anastomotic complications and those complications were significantly correlated with the novel factor time ratio (> 0.6) as the most reliable predictor of perfusion and anastomotic complications. Recently, Han et al[11] compared the changes in perfusion status between high tie and low tie through quantitative evaluation of ICG using NIF technique. They demonstrated that T_max increased and Slope_max decreased significantly in the high tie group after IMA ligation, whereas the intensity of perfusion status (F_max), which indicates the intensity of perfusion, did not change according to the level of IMA ligation. They suggested that the speed of blood perfusion could be more delayed after high tie than low tie, but the intensity of perfusion was similar between high and low ligation of IMA. There are still a lot of questions and debates to be discussed, but we believe that the NIF technique will play an important role in improving the clinical and oncologic outcomes of colorectal surgery.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Li M, Luo ZW S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Bae SU, Baek SJ, Hur H, Baik SH, Kim NK, Min BS. Intraoperative near infrared fluorescence imaging in robotic low anterior resection: three case reports. Yonsei Med J. 2013;54:1066-1069. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Son GM, Ahn HM, Lee IY, Ha GW. Multifunctional Indocyanine Green Applications for Fluorescence-Guided Laparoscopic Colorectal Surgery. Ann Coloproctol. 2021;37:133-140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 3. | Zocola E, Meyer J, Christou N, Liot E, Toso C, Buchs NC, Ris F. Role of near-infrared fluorescence in colorectal surgery. World J Gastroenterol. 2021;27:5189-5200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Kim HJ, Park JS, Choi GS, Park SY, Lee HJ. Fluorescence-guided Robotic Total Mesorectal Excision with Lateral Pelvic Lymph Node Dissection in Locally Advanced Rectal Cancer: A Video Presentation. Dis Colon Rectum. 2017;60:1332-1333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Zhou SC, Tian YT, Wang XW, Zhao CD, Ma S, Jiang J, Li EN, Zhou HT, Liu Q, Liang JW, Zhou ZX, Wang XS. Application of indocyanine green-enhanced near-infrared fluorescence-guided imaging in laparoscopic lateral pelvic lymph node dissection for middle-low rectal cancer. World J Gastroenterol. 2019;25:4502-4511. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 63] [Cited by in RCA: 47] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 6. | Park SY, Park JS, Kim HJ, Woo IT, Park IK, Choi GS. Indocyanine Green Fluorescence Imaging-Guided Laparoscopic Surgery Could Achieve Radical D3 Dissection in Patients With Advanced Right-Sided Colon Cancer. Dis Colon Rectum. 2020;63:441-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 7. | Bae SU, Jeong WK, Baek SK. Intra-operative near-infrared fluorescence imaging for robotic complete mesocolic excision and central vascular ligation in right-sided colon cancer - a video vignette. Colorectal Dis. 2019;21:1459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Bae SU, Min BS, Kim NK. Robotic Low Ligation of the Inferior Mesenteric Artery for Rectal Cancer Using the Firefly Technique. Yonsei Med J. 2015;56:1028-1035. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Bae SU, Min BS, Kim NK. Near infrared fluorescence imaging for real-time assessment of blood flow during totally robotic total mesorectal excision for rectal cancer--a video vignette. Colorectal Dis. 2016;18:313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Son GM, Kwon MS, Kim Y, Kim J, Kim SH, Lee JW. Quantitative analysis of colon perfusion pattern using indocyanine green (ICG) angiography in laparoscopic colorectal surgery. Surg Endosc. 2019;33:1640-1649. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 141] [Article Influence: 20.1] [Reference Citation Analysis (1)] |
| 11. | Han SR, Lee CS, Bae JH, Lee HJ, Yoon MR, Al-Sawat A, Lee DS, Lee IK, Lee YS. Quantitative evaluation of colon perfusion after high versus low ligation in rectal surgery by indocyanine green: a pilot study. Surg Endosc. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |