Published online Mar 28, 2022. doi: 10.3748/wjg.v28.i12.1220
Peer-review started: March 20, 2021
First decision: June 14, 2021
Revised: July 29, 2021
Accepted: February 23, 2022
Article in press: February 23, 2022
Published online: March 28, 2022
Processing time: 369 Days and 11.4 Hours
Colonoscopy is currently the gold standard for diagnosis of inflammatory bowel disease (IBD) and colorectal cancer (CRC). This has the obvious drawback of being invasive as well as carrying a small risk. The most widely used non-invasive approaches include the use of faecal calprotectin in the case of IBD and fecal immunochemical test in the case of CRC. However, the necessity of stool collection limits their acceptability for some patients. Over the recent years, there has been emerging data looking at the role of non-invasively obtained colorectal mucus as a screening and diagnostic tool in IBD and CRC. It has been shown that the mucus rich material obtained by self-sampling of anal surface following defecation, can be used to measure various biomarkers that can aid in diagnosis of these conditions.
Core Tip: We now know that non-invasively collected colorectal mucus contains diagnostically informative cells that can be analysed to look for various biomarkers. The presence of some of these biomarkers have the potential role in diagnosis of inflammatory bowel disease and colorectal cancer. This is an exciting field that we believe is worth exploring further.
- Citation: Nooredinvand HA, Poullis A. Emerging role of colorectal mucus in gastroenterology diagnostics. World J Gastroenterol 2022; 28(12): 1220-1225
- URL: https://www.wjgnet.com/1007-9327/full/v28/i12/1220.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i12.1220
The current gold standard for the diagnosis of inflammatory bowel disease (IBD) and colorectal cancer (CRC) is ileocolonoscopy. This however is time consuming, expensive and carries a small risk. Unnecessary colonoscopies could be avoided if reliable non-invasive tests were available to diagnose these conditions.
Non-invasive approaches to measurement of inflammation include serum biomarkers such as C-reactive protein (CRP) although this is not bowel specific. Stool calprotectin is bowel specific and is the best studied test[1] however necessity of collecting stool makes this unpopular with some patients[2-4].
In adults, a faecal calprotectin of > 50 μg/g has a sensitivity and specificity of 93% and 94% respectively for distinguishing between irritable bowel syndrome (IBS) and IBD[1]. While faecal calprotectin has an established position in helping to guide the need for ileocolonoscopy in those with bowel symptoms and the follow up of established IBD, it is not in itself a specific diagnostic test.
For CRC, fecal immunochemical test (FIT) is the most widely used non-invasive screening tool with a sensitivity and specificity of 79% and 94% respectively[5]. Similar to faecal calprotectin, an abnormal FIT prompts further investigations and assessment but is not a diagnostic test.
Over the recent years there has been emerging data looking at the use of non-invasive colorectal mucus sampling as a screening and diagnostic tool for IBD as well as CRC.
Colorectal mucus acts as an interface between colonic mucosa and gut content and is a recipient of cells released from the mucosal surface[6]. Some of these cells embedded in the colorectal mucus are excreted with faeces. This cell containing colorectal mucus can therefore be used for specific cell and biomarker detection[7-9]. There is increasing understanding of the complex roles of the colorectal mucus. The mucus itself is a dilute, aqueous and viscoelastic secretion with specific proteins, the mucins, being the major component[10]. The role, composition, physiology and pathophysiology are outside the scope of this review and have recently been reviewed elsewhere[11]. This review will focus on the emerging role of colorectal mucus in diagnostics.
Colorectal mucus can be obtained during proctoscopy[7,8,12] however this has the obvious drawback of being invasive and therefore unfavorable as a screening tool. Up until recently there was no reliable non-invasive method for colorectal mucus sampling. Over the past few years, a novel technique has been developed based on self-sampling of mucus-rich material from the anal surface immediately following defecation.
The use of colorectal mucus as a source of biomarkers has been evaluated in several studies. In the setting of IBD diagnostics and monitoring and CRC diagnostics colorectal mucus has been shown to be a novel and useful medium.
The first study assessing non-invasively collected colorectal mucus compared 141 patients (58 patients with IBD, 50 patients with IBS and 33 healthy volunteers). The study participants were instructed to swab the external anal area immediately following defecation and samples were collected for cytological and Mucin 2 (MUC2) analysis. This was the first study ever to describe non-invasively collected cytology demonstrating large numbers of preserved inflammatory cells in IBD. Significant differences in MUC2 levels were identified in IBD vs non-IBD groups raising the possibility that colorectal mucus was a useful diagnostic medium[9].
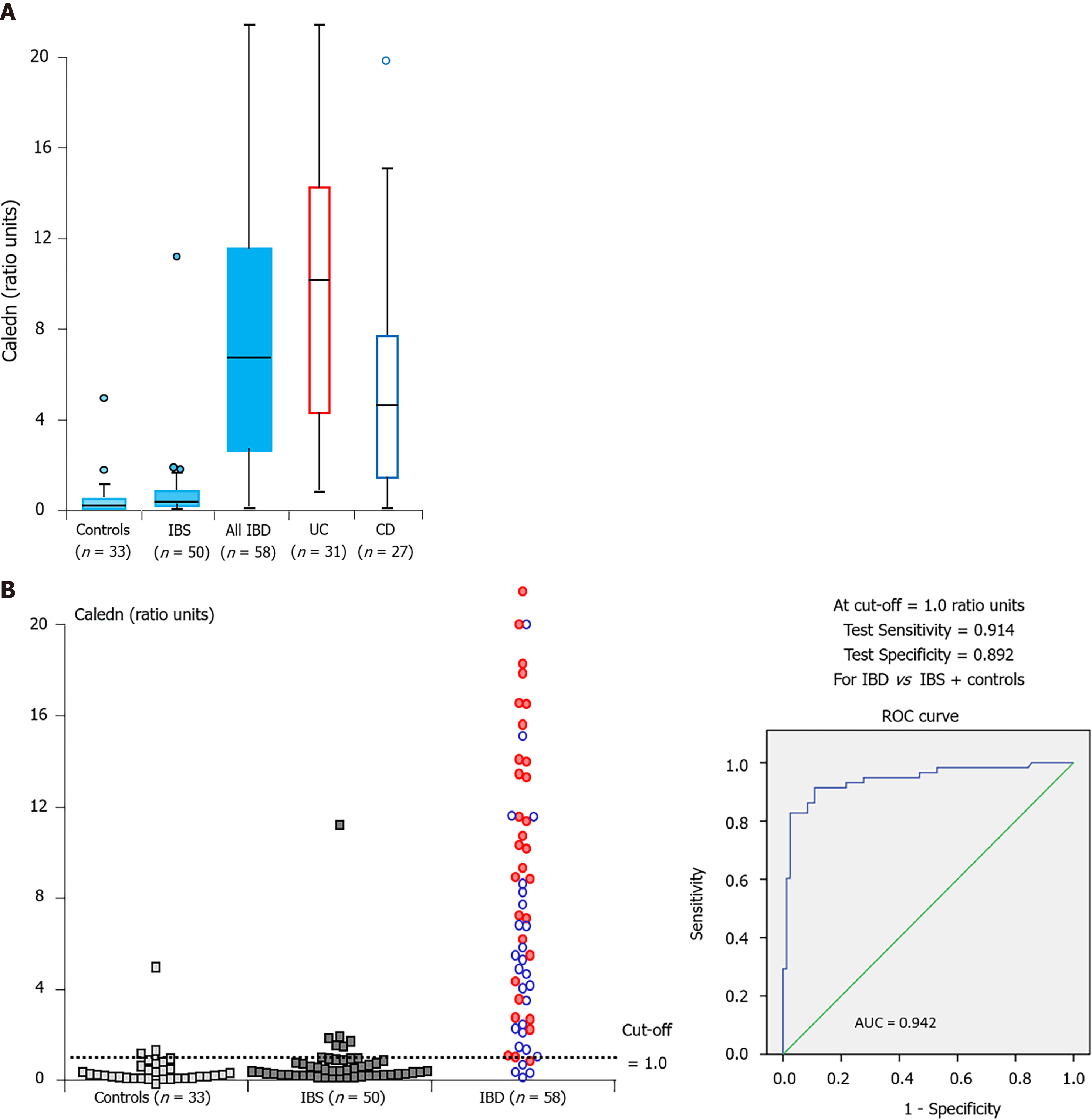
In a follow on study the performance of several biomarkers including calprotectin, eosinophil-derived neurotoxin (EDN) and protein S100A12 was evaluated in active IBD[13]. EDN is a major secretory protein of eosinophils and elevated levels of EDN have previously been detected in faeces of IBD patients[8]. S100A12 is another granulocyte protein and it has previously been proposed that measurement of the level of S100A12 in the faeces can help differentiate IBD from IBS[14,15].
The authors found that the medium concentration of all of these biomarkers were significantly higher in IBD patients compared to inflammation free individuals with calprotectin and EDN being more sensitive than S100A12 in detecting patients with IBD. Using a combined test taking into account the result of calprotectin and EDN (designated as CALEDN) resulted in sensitivity and specificity of 91% and 89% respectively in detecting patients with IBD (Figure 1). The concentration of all of these biomarkers was significantly higher in ulcerative colitis (UC) patients than those with Crohn’s disease (CD) with the most pronounced difference seen for EDN. Over a follow up period of 30 d following treatment there was a steady decrease of all biomarker levels among patients who demonstrated clinical improvement however correlation was easier to detect in UC patients[13].
Further to the description of inflammatory cells in the colorectal mucus of IBD patients an additional follow on cytology study demonstrated that true diagnostic cytology could be carried out on non-invasively collected colorectal mucus. Using cytology and immunocytochemistry a number of different cell types were identified (neutrophils, plasma cells and erythrophagocytes). Blinded cytological analysis enabled an accurate diagnosis to be made in 61.8% of cases[16].
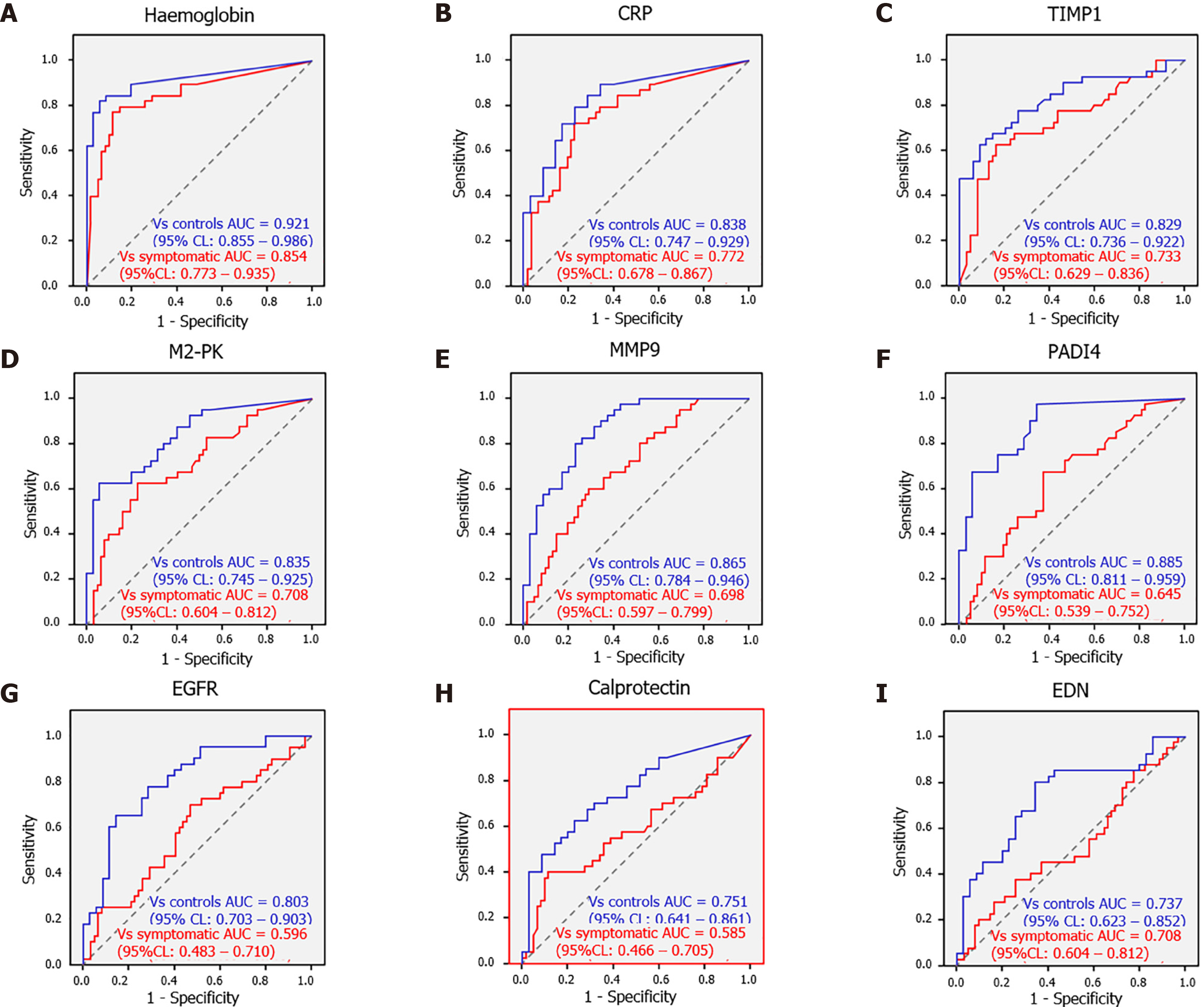
Given the success of this new medium in the diagnosis and monitoring of IBD attention has turned to CRC diagnostics. A pilot study was performed looking at whether various biomarkers detected in the colorectal mucus can be reliably used to aid detection of CRC. The diagnostic performance of 24 biomarkers were evaluated. 17 CRC and 35 healthy controls were used to assess these biomarkers. Quantification of haemoglobin, tissue inhibitor of metalloproteinase 1 (TIMP1), M2-pyruvate kinase (M2-PK), peptidyl arginine deiminase-4 (PADI4), CRP, matrix metalloproteinase 9 (MMP9), epidermal growth factor receptor (EGFR), EDN and calprotectin all showed good diagnostic potential[17].
A larger follow on study with 35 healthy volunteers, 62 CRC-free symptomatic patients and 40 CRC patients was conducted to assess the utility of these biomarkers collected in colorectal mucus[18].
The sensitivity and specificity of each of these biomarkers was analyzed in two different scenarios. For assessment of these markers in bowel cancer screening (BCS) comparison was made between the CRC group and healthy controls “screening” arm. A “triage” arm to the study was set up to reflect non-BCS clinical practice and a comparison between CRC cases and symptomatic CRC free patients. Hemoglobin was the best performer with overall sensitivity of 80% and specificity of 94% and 85.5% in the ‘screening’ and the ‘triage’ group respectively. These values are comparable to those reported for CRC screening by FIT test[19]. All other biomarkers had a lower sensitivity and specificity especially in the triage group. Of note proximal CRC was associated with higher numbers of false-negative results. EGFR, calprotectin and EDN were worst performing and could not be recommended as reliable diagnostic markers (Table 1 and Figure 2).
| Biomarker | Optimal cut-off level | Sensitivity (%) | AUC vs Sympt. Pat-s (95%CI) | Specificity vs Sympt. Pat-s (%) | AUC vs Control (95%CI) | Specificity vs Control (%) | Median biomarker level (CRC) | Median biomarker level (Sympt. Pat-s) | Median biomarker level (Control) |
| Haemoglobin | 109.27 ng/mL | 80.00 | 0.85 (0.77-0.93) | 88.55 | 0.92 (0.85-0.99) | 94.29 | 1708.74 ng/mLa,b | 0.00 ng/mLa,c | 0.00 ng/mLb,c |
| CRP | 8.90 ng/mL | 72.50 | 0.77 (0.68-0.87) | 75.81 | 0.84 (0.75-0.93) | 80.00 | 22.09 ng/mLd,e | 1.41 ng/mLd | 0.00 ng/mLe |
| TIMP1 | 3.25 ng/mL | 67.50 | 0.73 (0.63-0.84) | 75.81 | 0.83 (0.74-0.92) | 85.71 | 8.26 ng/mLf,g | 1.42 ng/mLf,h | 0.71 ng/mLg,h |
| M2-PK | 9.00 U/mL | 62.50 | 0.71 (0.60-0.81) | 77.42 | 0.83 (0.74-0.92) | 91.43 | 11.98 U/mLi,j | 2.97 U/mLi,k | 0.57 U/mLj,k |
| MMP9 | 10.38 ng/mL | 65.00 | 0.70 (0.60-0.80) | 64.52 | 0.86 (0.78-0.95) | 82.86 | 20.93 ng/mLl,m | 6.37 ng/mLl,n | 0.44 ng/mLm,n |
| PADI4 | 1.16 ng/mL | 67.50 | 0.64 (0.54-0.75) | 62.90 | 0.88 (0.81-0.96) | 94.29 | 1.51 ng/mLo,p | 0.88 ng/mLo,q | 0.00 ng/mLp,q |
| EGFR | 305.52 pg/mL | 60.00 | 0.60 (0.48-0.71) | 58.06 | 0.80 (0.70-0.90) | 88.57 | 342.72 pg/mLr | 187.01 pg/mLs | 67.72 pg/mLr,s |
| Calprotectin | 3.38 μg/mL | 57.50 | 0.58 (0.47-0.70) | 56.45 | 0.75 (0.64-0.86) | 80.00 | 4.01 μg/mLt | 2.94 μg/mLu | 0.59 μg/mLt,u |
| EDN | 12.83 ng/mL | 45.00 | 0.52 (0.40-0.64) | 62.90 | 0.74 (0.62-0.85) | 88.57 | 8.04 ng/mLv | 10.10 ng/mLw | 2.85 ng/mLv,w |
Through the use of a questionnaire we found that the method of colorectal mucus sampling was generally very well accepted by the patients arguing that non-invasive testing of colorectal samples for haemoglobin can present an attractive alternative to FIT. The average time taken for carrying out the sampling was about six minutes. Given the immunochemical colorectal mucus sample testing for haemoglobin differs very little from faecal sample testing and the cost being similar to that of FIT, this alternative may boost participation rates.
These studies demonstrate that diagnostically informative cells can be obtained from colorectal mucus which can be non-invasively obtained by simply swabbing the external anal area immediately following defecation. The proposed method of colorectal mucus sample collection eliminates the necessity of stool collection and appeared to be very well accepted by the study participants with the vast majority of samples being suitable for biomarker and cytological analysis.
Future work however needs to focus on direct head-to-head comparison between stool calprotectin and colorectal mucus calprotectin in the case of IBD and colorectal mucus haemoglobin concentration and FIT test for colonic cancer screening.
The non-invasive collection of colorectal mucus is a novel and exciting area of gastrointestinal diagnostics and may dramatically change our approach to the investigation and diagnosis of colorectal diseases.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: British Society of Gastroenterology.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zhang C S-Editor: Fan JR L-Editor: A P-Editor: Yu HG
| 1. | Waugh N, Cummins E, Royle P, Kandala NB, Shyangdan D, Arasaradnam R, Clar C, Johnston R. Faecal calprotectin testing for differentiating amongst inflammatory and non-inflammatory bowel diseases: systematic review and economic evaluation. Health Technol Assess. 2013;17:xv-xix, 1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 166] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 2. | Lecky DM, Hawking MK, McNulty CA; ESBL steering group. Patients' perspectives on providing a stool sample to their GP: a qualitative study. Br J Gen Pract. 2014;64:e684-e693. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 54] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 3. | Schultze A, Akmatov MK, Andrzejak M, Karras N, Kemmling Y, Maulhardt A, Wieghold S, Ahrens W, Günther K, Schlenz H, Krause G, Pessler F. Comparison of stool collection on site vs at home in a population-based study : feasibility and participants' preference in Pretest 2 of the German National Cohort. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2014;57:1264-1269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Feigelson HS, Bischoff K, Ardini MA, Ravel J, Gail MH, Flores R, Goedert JJ. Feasibility of self-collection of fecal specimens by randomly sampled women for health-related studies of the gut microbiome. BMC Res Notes. 2014;7:204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Lee JK, Liles EG, Bent S, Levin TR, Corley DA. Accuracy of fecal immunochemical tests for colorectal cancer: systematic review and meta-analysis. Ann Intern Med. 2014;160:171. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 530] [Cited by in RCA: 490] [Article Influence: 44.5] [Reference Citation Analysis (0)] |
| 6. | Loktionov A. Cell exfoliation in the human colon: myth, reality and implications for colorectal cancer screening. Int J Cancer. 2007;120:2281-2289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 72] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | Loktionov A, Ferrett CG, Gibson JJS, Bandaletova T, Dion C, Llewelyn AH, Lywood HGG, Lywood RCG, George BD, Mortensen NJ. A case-control study of colorectal cancer detection by quantification of DNA isolated from directly collected exfoliated colonocytes. Int J Cancer. 2010;126:1910-1919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Anderson N, Suliman I, Bandaletova T, Obichere A, Lywood R, Loktionov A. Protein biomarkers in exfoliated cells collected from the human rectal mucosa: implications for colorectal disease detection and monitoring. Int J Colorectal Dis. 2011;26:1287-1297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Loktionov A, Chhaya V, Bandaletova T, Poullis A. Assessment of cytology and mucin 2 in colorectal mucus collected from patients with inflammatory bowel disease: Results of a pilot trial. J Gastroenterol Hepatol. 2016;31:326-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Bansil R, Turner BS. The biology of mucus: Composition, synthesis and organization. Adv Drug Deliv Rev. 2018;124:3-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 429] [Cited by in RCA: 415] [Article Influence: 59.3] [Reference Citation Analysis (0)] |
| 11. | Paone P, Cani PD. Mucus barrier, mucins and gut microbiota: the expected slimy partners? Gut. 2020;69:2232-2243. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 693] [Cited by in RCA: 948] [Article Influence: 189.6] [Reference Citation Analysis (0)] |
| 12. | Loktionov A, Bandaletova T, Llewelyn AH, Dion C, Lywood HG, Lywood RC, Rockall TA, Stebbing JF, Broughton M, Caffarey S, Marks CG. Colorectal cancer detection by measuring DNA from exfoliated colonocytes obtained by direct contact with rectal mucosa. Int J Oncol. 2009;34:301-311. [PubMed] |
| 13. | Loktionov A, Chhaya V, Bandaletova T, Poullis A. Inflammatory bowel disease detection and monitoring by measuring biomarkers in non-invasively collected colorectal mucus. J Gastroenterol Hepatol. 2017;32:992-1002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Foell D, Wittkowski H, Roth J. Monitoring disease activity by stool analyses: from occult blood to molecular markers of intestinal inflammation and damage. Gut. 2009;58:859-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 160] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 15. | Kaiser T, Langhorst J, Wittkowski H, Becker K, Friedrich AW, Rueffer A, Dobos GJ, Roth J, Foell D. Faecal S100A12 as a non-invasive marker distinguishing inflammatory bowel disease from irritable bowel syndrome. Gut. 2007;56:1706-1713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 163] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 16. | Bandaletova T, Chhaya V, Poullis A, Loktionov A. Colorectal mucus non-invasively collected from patients with inflammatory bowel disease and its suitability for diagnostic cytology. APMIS. 2016;124:160-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Loktionov A, Soubieres A, Bandaletova T, Mathur J, Poullis A. Colorectal cancer detection by biomarker quantification in noninvasively collected colorectal mucus: preliminary comparison of 24 protein biomarkers. Eur J Gastroenterol Hepatol. 2019;31:1220-1227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Loktionov A, Soubieres A, Bandaletova T, Francis N, Allison J, Sturt J, Mathur J, Poullis A. Biomarker measurement in non-invasively sampled colorectal mucus as a novel approach to colorectal cancer detection: screening and triage implications. Br J Cancer. 2020;123:252-260. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Gies A, Bhardwaj M, Stock C, Schrotz-King P, Brenner H. Quantitative fecal immunochemical tests for colorectal cancer screening. Int J Cancer. 2018;143:234-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (2)] |